Abstract
Takotsubo syndrome (TTS) is an acute myocardial disease characterized by reversible left ventricular dysfunction, in the absence of obstructive coronary artery disease, caused by adrenergic overactivity and associated with non-negligible morbidity and mortality. Takotsubo syndrome, by far more frequent in women, who account for 9 out of 10 cases, is generally triggered by intense psychoemotional stress. In men, TTS has different, though not yet fully defined, characteristics and clinical course. In fact, men have a higher prevalence of a physical trigger and comorbidities, such as bronchopulmonary or cerebral pathologies, diabetes mellitus, and malignant neoplasms. The hospital course is burdened by a higher rate of cardiogenic shock and mortality. The long-term prognosis is also less favourable in men. Takotsubo syndrome in men characterizes a higher-risk phenotype, which requires close monitoring during hospitalization and careful surveillance during follow-up.
Keywords: Takotsubo cardiomyopathy, Treatment outcomes, Gender differences
Over the last few years, takotsubo syndrome (TTS) has emerged as an important cause of acute reversible myocardial injury caused by transient left ventricular dysfunction with a segmental distribution. This syndrome derives its name from the Japanese word which literally means ‘polyp trap’, as the characteristic shape assumed by the left ventricle in end systole recalls the amphorae used in Japan to trap polyps. It has been described under different names in the literature over the years, including ‘broken heart syndrome’, ‘stress cardiomyopathy’, and ‘apical balloon syndrome’; however, no term accurately describes the heterogeneous ventricular appearance with which this syndrome can manifest.1 To date, consensus on nomenclature has not been reached, but the term ‘takotsubo’ is widely used in recognition of Japanese physicians who first described it.2 Its prevalence is currently estimated at 1–3% of all acute coronary syndromes (ACS) with which it shares common characteristics such as initial presenting symptoms, electrocardiographic changes, and elevation of myocardionecrosis enzymes. Unlike ACS and cardiomyopathies, TTS is generally characterized by a temporary impairment of left ventricular systolic function with complete recovery within 3 weeks.
Adrenergic hyperactivation plays a central role in the pathophysiology of TTS. The interaction between the hypothalamic–pituitary–adrenal axis, which can release large quantities of adrenaline and noradrenaline following stress, and the response of the cardiovascular system to the peak of catecholamines is crucial. From literature data, about 90% of affected patients are women, and 80% are over 50 years of age. Women over the age of 55 have a 10 times higher risk of developing TTS than men.3 Nonetheless, TTS should not be considered a gender disease, so much so that in recent years, there has been an increase in cases in males, in which the onset is more often associated with a physical trigger.3 In fact, a hallmark of TTS is its association with a previous stressful event. Initially, most of the triggers reported involved emotional trauma; later, an association with physical stress also emerged (especially in men), while in a third of cases, it occurs in the absence of a recognizable stressor. The triggers are mostly represented by traumatic emotional events, including mourning, interpersonal conflicts, fear, and panic. Sometimes, however, the triggering emotions may depend on happy events. Physical stressors can be related to medical conditions, such as acute respiratory failure, subarachnoid haemorrhage, stroke, pancreatitis, cholecystitis, pheochromocytoma, thyrotoxicosis, neoplasms, or related therapies (chemotherapy and radiotherapy). The use of sympathomimetic drugs such as dobutamine in provocative tests or isoproterenol in electrophysiological alterations can be a trigger.
It should not be underestimated that even the acute occlusion of a coronary artery can have a causal role in the development of TTS.4 In this regard, TTS can be divided into a primary form in which acute cardiac symptoms are the main reason for medical consultation and a secondary form in which the pathological event occurs in patients hospitalized for other medical, surgical, or psychiatric conditions. In the first case, the comorbidities can coexist, but they are not the cause of the catecholaminergic storm; in the second case, the sudden activation of the sympathetic nervous system and/or the increase of circulating catecholamines is the consequence of the primary pathologies or their treatment, determining the development of TTS.5,6 In this regard, it has been reported that patients with secondary TTS are more frequently males and have a higher prevalence of in-hospital death than patients with primary TTS.4 The most common symptoms of TTS are acute chest pain, dyspnoea, or syncope and therefore are difficult to distinguish from ACS. In patients with hospital-onset takotsubo, it may be diagnosed incidentally by new electrocardiogram (ECG) changes or increased markers of myocardionecrosis.
In relation to the above, men usually have atypical symptoms (tachycardia, hypotension), hidden by the underlying morbid condition.7 The ECG changes typical of this syndrome, such as ST-segment elevation (44% of cases), ST-segment depression (8%), left bundle branch block (5%), or T-wave inversion (41%), do not show different distributions in both sexes.3,7 As in ACS, the ECG shows a temporal evolution with resolution of the initial ST-segment elevation (if present), followed by progressive T-wave inversion and QT interval prolongation. Within days or weeks, the ECG should return to normal.7 Biomarkers also play an important role for diagnostic purposes; in fact troponin is generally elevated, but its increase is low in relation to the extent of left ventricular dysfunction; on the contrary, the values of brain natriuretic peptide (BNP) and NT-proBNP are disproportionately elevated, and the peak is observed 24–48 h after the acute presentation with normalization over months. These alterations do not show significant differences in relation to gender or age at clinical presentation, although a lower troponin value at onset may indicate a more favourable prognosis.
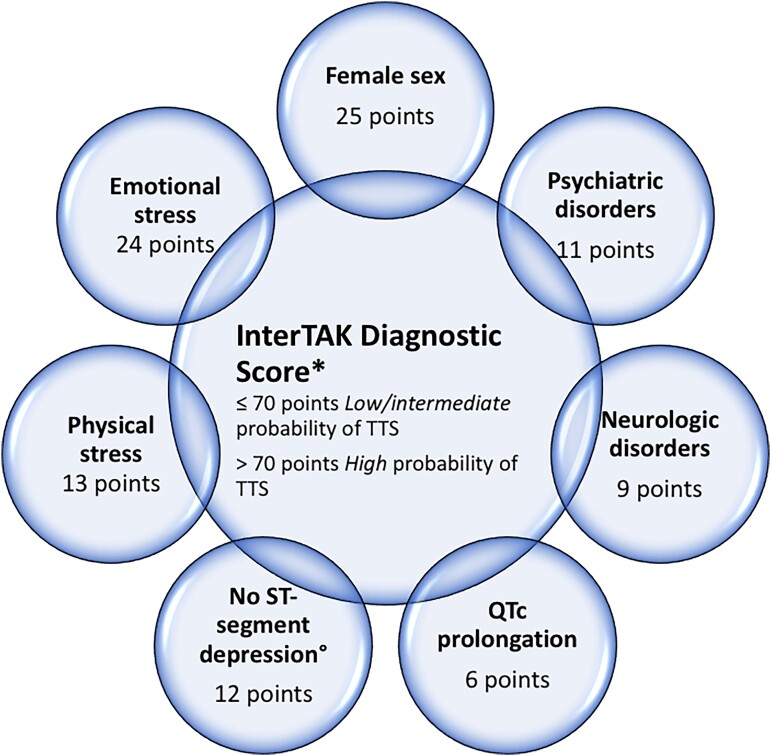
Regarding the echocardiographic features, the prevalence described in the literature of the four commonly encountered subtypes does not change between the two sexes. Indeed, the apical form with a-dyskinesia of the mid-apical segments and basal hypercontractility remains the most frequent (80% of cases); the mid-ventricular variant has a prevalence of 15% that, with basal akinesia, remains an exceptional finding (<5%). Forms of TTS with focal involvement, mostly of the anterolateral wall, are also described, making it difficult to differentiate TTS from ACS and myocarditis without resorting to cardiac magnetic resonance imaging. In about one third of patients, the dysfunction is biventricular with involvement of the right ventricle as well. In most variants, left ventricular dysfunction affects more than one territory of distribution of a coronary vessel, generally with a circumferential trend in the absence of ‘culprit’ lesions on angiography.7 The operative model proposed in the international consensus document on TTS7 states that patients with ST-segment elevation should undergo urgent coronary angiography with left ventriculography to rule out acute myocardial infarction (AMI). In patients without ST-segment elevation, the use of the InterTAK diagnostic score may be considered (Figure 1).
Figure 1.
Diagnostic algorithm of takotsubo syndrome. *The InterTAK Diagnostic Score did not include patients with pheochromocytoma induced takotsubo syndrome in which atypical pattern are more frequently noted. °Except in lead aVR.
The InterTAK diagnostic score was developed from the international takotsubo registry, and since the female gender is prevalent, this is the component of the ‘score’ that gives the highest score of all (25 points).3,8 An InterTAK score <70 points suggests a low to intermediate probability of TTS, while a score >70 indicates a high probability of TTS. Patients with low probability should undergo coronary angiography with left ventriculography, while in patients with high probability, a decision should be made according to the result of transthoracic echocardiography. In the absence of the apical circumferential pattern on the echocardiogram, coronary angiography is still recommended. In general, in stable patients with an apical pattern, coronary computed tomography is preferable to rule out coronary artery disease. In unstable patients, the typical complications of TTS, such as left ventricular outflow tract obstruction, must be investigated, and both echocardiography and coronary angiography are essential to rule out AMI with certainty. The association between undamaged coronary arteries and apical pattern, in the absence of markers suggestive of acute myocarditis (signs or symptoms of viral infection, increased C-reactive protein or erythrocyte sedimentation rate, or presence of pericardial effusion), indicates TTS as the most likely diagnosis; kinetic recovery on echocardiographic follow-up will confirm the diagnosis. In the presence of markers of acute myocarditis, cardiac magnetic resonance imaging is recommended to confirm or exclude the diagnosis.7
Although TTS is a reversible condition with a benign medium- and long-term prognosis, the in-hospital acute phase is associated, in a fifth of cases, with major even fatal complications such as acute heart failure, left ventricular outflow obstruction, cardiogenic shock, ventricular tachycardias, and left intraventricular thrombosis. Therefore, early risk stratification at the time of diagnosis is important, allowing for adequate clinical management of the patient. Parameters that predict an unfavourable outcome are physical trigger, acute neurological or psychiatric illness, initial troponin >10 times the upper reference limit, and left ventricular ejection fraction at diagnosis <45%.3 In addition, men have up to three times higher rates of death and major adverse cardiac and cerebrovascular events than women (8.4% vs. 3.6%, P < 0.0001) and more often have an underlying critical illness that contributes to the increased mortality.9 From a prospective study that enrolled 82 patients hospitalized for TTS from January 2008 to December 2015, male gender and physical trigger as the underlying causes were independent risk factors for in-hospital mortality.10 Gender may also play a role in the follow-up; in fact in the study by Stiermaier et al.,11 male gender, Killip Class 3 or 4 at admission, and diabetes mellitus were identified as independent predictors of long-term mortality in patients with TTS. In this regard, from the analysis of patients enrolled in the German Italian Spanish Takotsubo international multicentre registry, men with TTS were younger but with a higher prevalence of comorbidities (diabetes mellitus 25% vs. 19%; P = 0.01; pulmonary disease 21% vs. 15%; P = 0.006; malignancies 25% vs. 13%; P < 0.001) and physical triggers (55 vs. 32% P < 0.01), compared with women (Table 1). Furthermore, survival analysis showed a higher mortality rate in men, both during the acute phase and after 60 days.12
Table 1.
Comparison of different variables between males and females in takotsubo syndrome
| Gender difference in takotsubo syndrome | ||
|---|---|---|
| Variable | Males | Females |
| Age | Younger | Older |
| Comorbidity | More | Less |
| Prevalent trigger | Physical | Emotional |
| Cardiogenic shock | Higher | Lower |
| In-hospital mortality | Higher | Lower |
| Long-term mortality | Higher | Lower |
Amongst patients who survive the initial event, the recurrence of TTS has been reported in approximately 5% of cases; the second event can mostly occur between 3 weeks and 3.8 years after the first.5,7,13,14 Recurrent TTS affects both men and women and can occur in any age group. Although TTS recurrences in several variants are reported, a detailed review of published cases and clinical experience suggest that generally TTS recurrences occur in the apical pattern.7
Regarding therapy, there are no randomized clinical trials supporting a specific treatment of TTS, either in the acute phase or in the follow-up. The therapeutic strategies are based on clinical experience and on the management of possible complications such as heart failure, arrhythmias, and cardiogenic shock. In the presence of ventricular dysfunction, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) and beta blockers should be indicated. In the most severe cases with cardiogenic shock, the use of catecholamines should be avoided, but levosimendan and possibly mechanical aids can be used.7,15
In conclusion, early risk stratification remains the main tool for promptly choosing the appropriate treatments and for managing any complications. Although TTS is more common in women, it is characterized by a distinct high-risk phenotype in men that requires close hospital monitoring and close long-term follow-up.
Contributor Information
Enrico Natale, UOC Cardiology, Cardio-Thoraco-Vascular Department, S. Camillo Forlanini Hospital, Rome, Italy.
Raffaella Mistrulli, Department of Cardiology, Sapienza University of Rome, S. Andrea University Hospital, Rome, Italy.
Funding
None declared.
Data availability
No new data were generated or analysed in support of this research.
References
- 1. Sharkey SW, Lesser JR, Maron MS, Maron BJ. Why not just call it tako-tsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol 2011;57:1496–1497. [DOI] [PubMed] [Google Scholar]
- 2. Sato H. Tako-tsubo-like left ventricular dysfunction due to multivessel coronary spasm. In: Kodama K, Haze K, Hori M, eds. Clinical Aspect of Myocardial Injury: From Ischemia to Heart Failure. Tokyo: Kagakuhyoronsha Publishing Co; 1990. p56–64. [Google Scholar]
- 3. Templin C, Ghadri JR, Diekmann Jet al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med 2015;373:929–938. [DOI] [PubMed] [Google Scholar]
- 4. Ghadri JR, Wittstein IS, Prasad Aet al. International expert consensus document on takotsubo syndrome (part I): clinical characteristics, diagnostic criteria, and pathophysiology. Eur Heart J 2018;39:2032–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lyon AR, Bossone E, Schneider Bet al. Current state of knowledge on takotsubo syndrome: a position statement from the task force on takotsubo syndrome of the heart failure association of the European society of cardiology. Eur J Heart Fail 2016;18:8–27. [DOI] [PubMed] [Google Scholar]
- 6. Isogai T, Yasunaga H, Matsui Het al. Out-of-hospital versus in-hospital takotsubo cardiomyopathy: analysis of 3719 patients in the diagnosis procedure combination database in Japan. Int J Cardiol 2014;176:413–417. [DOI] [PubMed] [Google Scholar]
- 7. Ghadri JR, Cammann VL, Jurisic Set al. A novel clinical score (InterTAK diagnostic score) to differentiate takotsubo syndrome from acute coronary syndrome: results from the International Takotsubo Registry. Eur J Heart Fail 2017;19:1036–1042. [DOI] [PubMed] [Google Scholar]
- 8. Ghadri JR, Wittstein IS, Prasad Aet al. International expert consensus document on takotsubo syndrome (part II): diagnostic workup, outcome, and management. Eur Heart J 2018;39:2047–2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the national inpatient sample 2008 to 2009. Am Heart J 2012;164:215–221. [DOI] [PubMed] [Google Scholar]
- 10. Sobue Y, Watanabe E, Ichikawa Tet al. Physically triggered takotsubo cardiomyopathy has a higher in-hospital mortality rate. Int J Cardiol 2017;235:87–93. [DOI] [PubMed] [Google Scholar]
- 11. Stiermaier T, Moeller C, Oehler Ket al. Long-term excess mortality in takotsubo cardiomyopathy: predictors, causes and clinical consequences. Eur J Heart Fail 2016;18:650–656. [DOI] [PubMed] [Google Scholar]
- 12. Arcari L, Núñez Gil IJ, Stiermaier Tet al. Gender differences in takotsubo syndrome. J Am Coll Cardiol 2022;79:2085–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sharkey SW, Windenburg DC, Lesser JRet al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol 2010;55:333–341. [DOI] [PubMed] [Google Scholar]
- 14. Cattaneo M, Moccetti M, Pasotti Eet al. Three recurrent episodes of apical-ballooning takotsubo cardiomyopathy in a man. Circulation 2015;132:e377–e379. [DOI] [PubMed] [Google Scholar]
- 15. Singh T, Khan H, Gamble DT, Scally C, David E, Newby DEet al. Takotsubo syndrome: pathophysiology, emerging concepts, and clinical implications. Circulation 2022;145:1002–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.