Abstract
Introduction:
Despite bronchopulmonary dysplasia (BPD) being a common morbidity of preterm birth, there is no validated objective tool to assess outpatient respiratory symptom control for clinical and research purposes.
Methods:
Data were obtained from 1049 preterm infants and children seen in outpatient BPD clinics of 13 U.S. tertiary care centers from 2018-2022. A new standardized instrument was modified from an asthma control test questionnaire and administered at the time of clinic visits. External measures of acute care use were also collected. The questionnaire for BPD control was validated in the entire population and selected subgroups using standard methodology for internal reliability, construct validity, and discriminative properties.
Results:
Based on the scores from BPD control questionnaire, the majority of caregivers (86.2%) felt their child’s symptoms were under control, which did not differ by BPD severity (p=0.30) or a history of pulmonary hypertension (p=0.42). Across the entire population and selected subgroups, the BPD control questionnaire was internally reliable, suggestive of construct validity (albeit correlation coefficients were −0.2 to −0.4.), and discriminated control well. Control categories (controlled, partially controlled, and uncontrolled) were also predictive of sick visits, emergency department visits, and hospital readmissions.
Conclusion:
Our study provides a tool for assessing respiratory control in children with BPD for clinical care and research studies. Further work is needed to identify modifiable predictors of disease control and link scores from the BPD control questionnaire to other measures of respiratory health such as lung function testing.
Keywords: bronchopulmonary dysplasia, outpatient, symptoms, validation, questionnaire
INTRODUCTION
Preterm births account for approximately 10% of live births in the U.S. every year and over 15 million preterm births annually worldwide.1,2 One of the most common complications of preterm birth is bronchopulmonary dysplasia (BPD), a respiratory disease which affects the developing airways, alveoli, and pulmonary vasculature.3,4 Despite advances in neonatal care, rates of BPD remain unchanged,5 perhaps due to improved survival of infants born at earlier gestational ages. Preterm survivors with BPD frequently require respiratory support in the home setting, multiple daily medications, and frequent provider visits with a higher risk for rehospitalization.6
Despite these morbidities and high incidence of BPD, there is limited knowledge for best practices for outpatient care. Published guidelines lack high quality evidence on key issues such as the use of respiratory support and medications including identifying which patients would benefit, assessing effect, and deciding when to wean.7,8 One of the contributing factors is a paucity of objective tools to measure outcomes in young children. Typically, BPD can be diagnosed (and severity established) by a number of classification schema at 36 weeks post menstrual age,9–11 but there are few objective tools available to assess BPD symptom control during early childhood. The only objective, standardized, measure of respiratory disease available is lung function measured by spirometry, which cannot be obtained until approximately 5-7 years of age and assumes cooperation with maximal effort maneuvers, which limits applicability in those with neurodevelopmental impairment.12 Newer methods of obtaining lung function without sedation for children less than 6 years of age, such as oscillometry,13 are being gradually employed, they are not currently widely available and lack well established reference values for a diverse population.14 Respiratory disease symptom control has provided an essential tool in asthma clinical management and research. However, in BPD there is no standardized questionnaire-based data instrument to assess respiratory health and symptom control,15 which is especially essential for disease assessment in younger children and those with neurodevelopmental impairment.
This study aims to assess and validated a questionnaire for BPD control based on a respiratory disease symptom questionnaire. To achieve this, we examined responses from a modified version of a commonly used asthma control test (ACT) questionnaire16 and validated it with disease-specific external measures of control using data obtained from a multicenter outpatient registry of subjects with BPD in the Unites States.17 The BPD control questionnaire assessed and validated in this study provides an objective, quantitative tool to assess respiratory symptoms and disease control in BPD that will improve clinical decision making and facilitate the design of clinical trials, including potential randomized control trials in this population.
METHODS
Study Population:
Subjects were enrolled in the BPD Collaborative Outpatient Registry between September 2018 and June 2022 on the basis of a diagnosis of BPD by the 2001 NHLBI workshop definition and at least one complete control questionnaire as described below.10,17 Thirteen tertiary care centers recruited subjects through outpatient BPD clinics and contributed data to the registry, including Phoenix Children’s Hospital, Arkansas Children’s Hospital, Lucille Packard Children’s Hospital Stanford, Children’s Hospital of Los Angeles, Johns Hopkins Children’s Center, Boston Children’s Hospital, University of Massachusetts Memorial Children’s Medical Center, C.S. Mott Children’s Hospital, Children’s Mercy Hospital Kansas City, Nationwide Children’s Hospital, Children’s Hospital of Philadelphia, Monroe Carell Jr. Children’s Hospital at Vanderbilt, and Intermountain Primary Children’s Hospital at the University of Utah. All centers obtained approval through local institutional boards; data use agreements were signed between institutions for compiling anonymized data. Parents or legal guardians gave informed consent in accordance with local review board policies.
Data Collection:
The BPD Collaborative uses standardized instruments to collect demographic and clinical data, as previously described.17 The BPD control questionnaire was modified from the ACT questionnaire for asthma control, which has been validated and is in widespread use as both a clinical and research measure (Figure 1).16 Specifically, the modifications made by expert opinion include: the timeframe for the question for rescue inhaler use was modified from 4 weeks to 3 months, and the question on asthma control was replaced with a question assessing systemic steroid use over the past 12 months, excluding initial NICU admission. Demographic and clinical characteristics (summarized in Table 1) were collected at the first outpatient clinical encounter. The BPD control questionnaire and external measures of acute care use were collected at recruitment (summarized in Table 2). and repeatedly collected at subsequent visits, which were scheduled per clinical practice at each site. Acute care use measures, all for respiratory concerns, included number of sick visits, emergency department visits, hospital readmissions, antibiotic use, and systemic steroid use since either NICU discharge or the last clinic visit, whichever occurred last. Only subjects with complete demographic and clinical data as well as known BPD severity were retained for analyses.
Figure 1.
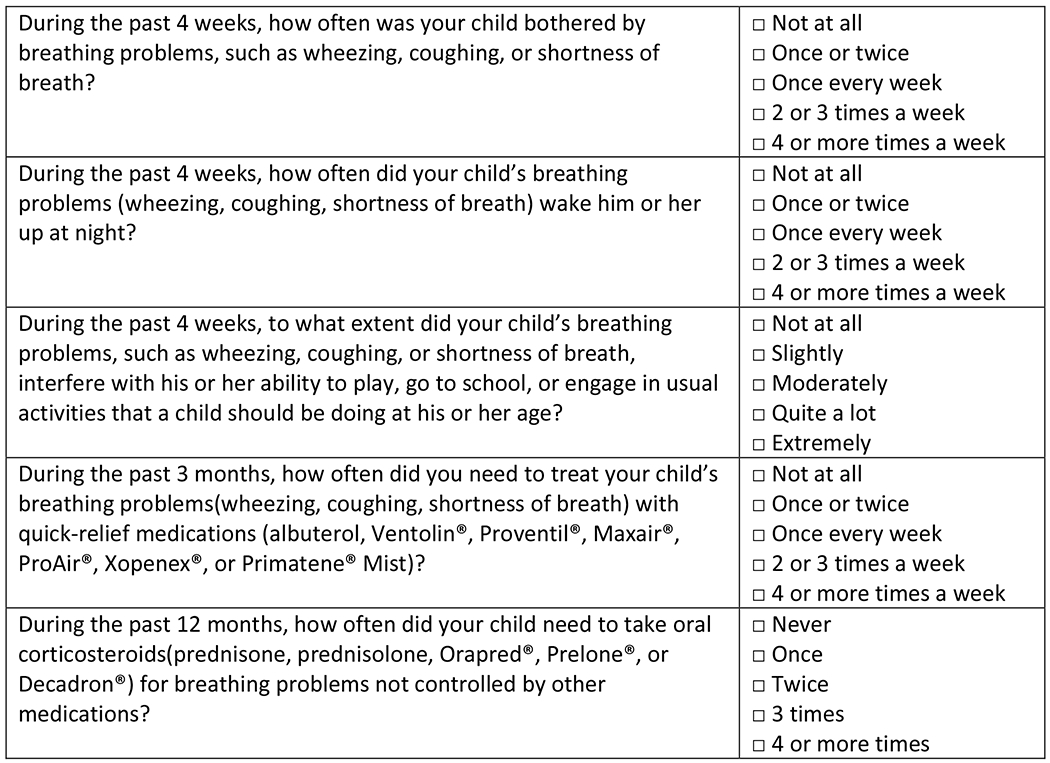
Bronchopulmonary Control Questionnaire
This questionnaire is scored by adding responses for each question (1 point for “4 or more times [a week]” to 5 points for “not at all” or “never”) to yield a score from 5-25 points (sum score) with higher values suggesting better disease control.
Table 1.
Demographic and Clinical Characteristics
| Mean ± S.D. [Range] | ||
|---|---|---|
| Study population (N) | 1049 | |
| Sex (% female) | 45.3% (n = 1044) |
|
| Race (% Non-white) | 43.5% (n = 1025) |
|
| Ethnicity (% Hispanic) | 11.6% (n = 1027) |
|
| Gestational age (weeks) | 26.8 ± 2.6 [22.0, 36.6] (n = 1048) |
|
| Birth weight (grams) | 902 ± 400 [280, 4500] (n = 1040) |
|
| Age at initial discharge from NICU (months) | 4.8 ± 3.1 [0.3, 28.0] (n = 1017) |
|
| Bronchopulmonary dysplasia severity (%) | Mild | 8.0% |
| Moderate | 21.9% | |
| Severe | 66.9% | |
| Unknown severity | 3.2% | |
| Pulmonary hypertension (% yes) | 23.1% (n = 1024) |
|
| Congenital cyanotic heart disease (% yes) | 1.2% (n = 1044) |
|
| Syndrome (% yes) | 10.1% (n = 1036) |
Table 2.
Data at Time of First BPD Control Questionnaire (Surveyed at Recruitment)
| Mean ± S.D. [Range] | ||
|---|---|---|
| Study population (N) | 1049 | |
| Age at first questionnaire (recruitment) (years) | 1.9 ± 2.4 [0.08, 16.7] |
|
| Sum score at first questionnaire (recruitment) | 22.8 ± 3.4 [6, 25] |
|
| Score Category at first questionnaire (recruitment) | Controlled (Sum score: 20-25) | 86.2% |
| Partially controlled (Sum score: 15-19) | 9.9% | |
| Not controlled (Sum score: 5-14) | 3.9% | |
| Number of acute respiratory events at first questionnaire | Sick visits | 0.5 ± 1.5 [0, 30] (n = 1033) |
| Emergency department visits | 0.3 ± 0.9 [0, 8] (n = 1035) |
|
| Hospital readmissions | 0.2 ± 0.7 [0, 10] (n = 1031) |
|
| Antibiotic use | 0.3 ± 1.0 [ 0, 15] (n = 1019) |
|
| Systemic steroid | 0.2 ± 0.8 [0, 10] (n = 1012) |
Measures:
BPD severity was defined in three categories (mild, moderate, and severe) per 2001 NHLBI definition.18 Pulmonary hypertension was defined as present or absent on or after 36 weeks PMA by clinical report at the local institution. Acute care use was captured by count of episodes, unless otherwise stated. The BPD control questionnaire consisted of 5 Likert scale (five-level) questions and was scored similar to the ACT questionnaire by adding the responses for each question (1 point for “4 or more times a week” to 5 points for “not at all”) to yield a score from 5-25 points (sum score) with higher values suggesting better disease control. Score categories were derived from the original ACT asthma questionnaire categories (Controlled BPD: 20-25; Partially controlled BPD: 15-19; Uncontrolled BPD: 5-14).16
Validation Analysis:
For validation, both reliability (internal reliability and test-retest reliability) and validity (construct validity and discriminative properties) were assessed. Content validity was not assessed as this is a modified form and not a new questionnaire. Except for test-retest reliability, the earliest BPD control questionnaire for each subject was utilized to avoid biasing results towards subjects with more than one collected questionnaire. Factors associated with Sum Score: To determine if demographic or clinical factors were associated with sum score, generalized estimating equations (GEE; clustered linear regression) were used with sum score as the dependent variable and the listed demographic variable as the independent variable (Table 3), and adjusted for age at questionnaire completion a priori.19 In this analysis, all BPD control questionnaires for each eligible subject were analyzed, using generalized estimating equations to account for the correlation arising from the possibility of more than one questionnaire per subject. A robust empirical “sandwich” variance estimator with independent covariance structure was used. Internal Reliability: Consistency in responses between individual items in the scale was assessed via Cronbach’s alpha values using the first available BPD control questionnaire for each subject, and also compared between demographic subgroups of race, ethnicity, BPD severity, and age group. Cronbach’s alpha values between 0.70-0.95 were interpreted as acceptable.20 Test-Retest Differences: For subjects with two or more BPD control questionnaires, a paired t-test was used to determine if sum scores differed between the first and second questionnaire. Linear regression was used to test whether time elapsed predicted the difference in sum scores between the first and second questionnaires while adjusting for the sum score and age at the first questionnaire. Construct Validity and Discriminative Properties: Spearman’s correlations between the scores from the first BPD control questionnaire were examined with external measures of acute care obtained at the same time (Table 4). Subgroup analyses were also performed. Kruskal-Wallis tests were used to compare the distribution of external acute care events across three sum score categories from the first BPD control questionnaire (Table 5). Sum Score Categories as Predictors: To assess whether sum score categories were predictive of emergency department visits and hospital readmissions, generalized estimating equations (clustered logistic regression) with robust “sandwich” variance estimators was used with sum score categories as the independent dummy variable and sick visit (Y/N), emergency department visit (Y/N) or hospital readmission (Y/N) as the dependent variable (E-Table 1). As all questionnaires for each eligible subject were used, regressions were clustered by subject and adjusted for age. Regressions were not adjusted for demographic or clinical variables similar to Table 3. P-values of less than 0.05 were considered to be of statistical significance.
Table 3.
Demographic and Clinical Factors Associated with Sum Score for BPD Control
| Coefficient [95% C.I.] (n = 1852 questionnaires for 920 subjects) |
Adjusted Model Coefficient* | P Value | |
|---|---|---|---|
| Sex (Female) | 0.1 [−0.3, 0.5] |
0.60 | |
| Race (Non-white) | 0.2 [−0.2, 0.6] |
0.38 | |
| Ethnicity (Hispanic) | −0.4 [−1.1, 0.2] |
0.21 | |
| Gestational age (weeks) | −0.004 [−0.07, 0.06] |
0.90 | |
| Birth weight (grams) | <−0.001 [−0.001, <0.001] |
0.33 | |
| Age at initial discharge (months) | −0.1 [−0.2, 0.0] |
0.11 | |
| Bronchopulmonary dysplasia severity (versus mild) | Moderate | 0.2 [−0.6, 1.0] |
0.57 |
| Severe | −0.1 [−0.9, 0.6] |
0.76 | |
| Pulmonary hypertension (yes versus no) | −0.2 [−0.6, 0.3] |
0.51 | |
| Congenital cyanotic heart disease (yes versus no) | −0.3 [−2.2, 1.5] |
0.72 | |
| Syndrome (yes versus no) | 0.1 [−0.5, 0.7] |
0.70 |
Coefficients and associated p values were generated through general estimating equations (GEE) clustered by subject to account for the possibility of more than one questionnaire per subject with sum score as the dependent variable and the listed demographic variable as the independent variable, and adjusted for age at the time of questionnaire completion.
Table 4.
Construct Validity: Correlation between BPD control sum score and acute care use for overall and by subgroups
| Acute Care Events | Subgroups | Subjects (N) |
Spearman Correlation Coefficient (Sum Score) |
P Value |
|---|---|---|---|---|
| Number of outpatient visits for respiratory illnesses (sick visits) | Overall | 1033 | −0.407 | <0.001 |
| Non-white | 440 | −0.420 | <0.001 | |
| Hispanic | 117 | −0.459 | <0.001 | |
| Mild/Moderate BPD | 308 | −0.381 | <0.001 | |
| Severe BPD | 692 | −0.423 | <0.001 | |
| <3 years old | 831 | −0.383 | <0.001 | |
| 3-5 years old | 150 | −0.429 | <0.001 | |
| ≥6 years old | 93 | −0.447 | <0.001 | |
| Number of emergency department visits | Overall | 1035 | −0.306 | <0.001 |
| Non-white | 439 | −0.323 | <0.001 | |
| Hispanic | 118 | −0.460 | <0.001 | |
| Mild/Moderate BPD | 310 | −0.290 | <0.001 | |
| Severe BPD | 692 | −0.304 | <0.001 | |
| <3 years old | 832 | −0.319 | <0.001 | |
| 3-5 years old | 151 | −0.314 | <0.001 | |
| ≥6 years old | 94 | −0.217 | 0.036 | |
| Number of hospital readmissions | Overall | 1031 | −0.274 | <0.001 |
| Non-white | 438 | −0.282 | <0.001 | |
| Hispanic | 119 | −0.206 | 0.025 | |
| Mild/Moderate BPD | 308 | −0.264 | <0.001 | |
| Severe BPD | 690 | −0.268 | <0.001 | |
| <3 years old | 828 | −0.315 | <0.001 | |
| 3-5 years old | 150 | −0.193 | 0.018 | |
| ≥6 years old | 94 | −0.105 | 0.31 | |
| Number of antibiotic courses | Overall | 1019 | −0.248 | <0.001 |
| Non-white | 439 | −0.276 | <0.001 | |
| Hispanic | 119 | −0.185 | 0.046 | |
| Mild/Moderate BPD | 302 | −0.211 | <0.001 | |
| Severe BPD | 684 | −0.247 | <0.001 | |
| <3 years old | 820 | −0.214 | <0.001 | |
| 3-5 years old | 147 | −0.336 | <0.001 | |
| ≥6 years old | 93 | −0.363 | <0.001 | |
| Number of systemic steroid courses | Overall | 1012 | −0.351 | <0.001 |
| Non-white | 436 | −0.413 | <0.001 | |
| Hispanic | 111 | −0.282 | 0.003 | |
| Mild/Moderate BPD | 305 | −0.348 | <0.001 | |
| Severe BPD | 675 | −0.330 | <0.001 | |
| <3 years old | 811 | −0.311 | <0.001 | |
| 3-5 years old | 149 | −0.409 | <0.001 | |
| ≥6 years old | 93 | −0.370 | <0.001 |
Table 5.
Discriminant Properties of Sum Score Categories for BPD control: the distribution of acute care events by three sum score categories for overall sample and subgroups
| Acute Care Events | Subgroups | Subjects (N) |
Controlled (Sum Score: 20-25) Mean ± S.D. |
Partially Controlled (Sum Score: 15-19) Mean ± S.D. |
Uncontrolled (Sum Score: 5-14) Mean ± S.D. |
Kruskal Wallis P Value |
|---|---|---|---|---|---|---|
| Number of outpatient visits for respiratory illnesses (sick visits) | Overall | 1033 | 0.3 ± 1.4 | 1.2 ± 1.9 | 1.5 ± 1.6 | <0.001 |
| Non-white | 440 | 0.3 ± 0.8 | 1.0 ± 1.5 | 1.1 ± 1.5 | <0.001 | |
| Hispanic | 117 | 0.4 ± 1.0 | 1.7 ± 2.3 | 2.2 ± 1.9 | <0.001 | |
| Mild/Moderate BPD | 308 | 0.4 ± 2.0 | 1.4 ± 2.3 | 1.3 ± 1.4 | <0.001 | |
| Severe BPD | 692 | 0.3 ± 0.8 | 1.2 ± 1.7 | 1.6 ± 1.7 | <0.001 | |
| <3 years old | 831 | 0.3 ± 0.8 | 0.9 ± 1.6 | 1.6 ± 1.7 | <0.001 | |
| 3-5 years old | 150 | 1.0 ± 3.2 | 2.1 ± 2.5 | 2.0 ± 2.8 | <0.001 | |
| ≥6 years old | 93 | 0.3 ± 1.2 | 1.1 ± 1.5 | 1.5 ± 1.7 | <0.001 | |
| Number of emergency department visits | Overall | 1035 | 0.2 ± 0.6 | 0.9 ± 1.5 | 0.7 ± 1.5 | <0.001 |
| Non-white | 439 | 0.3 ± 0.8 | 0.8 ± 1.3 | 0.5 ± 0.7 | <0.001 | |
| Hispanic | 118 | 0.3 ± 0.7 | 1.5 ± 2.0 | 2.0 ± 2.6 | 0.001 | |
| Mild/Moderate BPD | 310 | 0.2 ± 0.7 | 0.8 ± 1.4 | 0.6 ± 1.1 | 0.002 | |
| Severe BPD | 692 | 0.2 ± 0.6 | 0.9 ± 1.6 | 0.8 ± 1.7 | <0.001 | |
| <3 years old | 832 | 0.2 ± 0.6 | 0.9 ± 1.4 | 1.1 ± 2.0 | <0.001 | |
| 3-5 years old | 151 | 0.3 ± 0.9 | 1.2 ± 2.0 | 1.0 ± 1.4 | 0.005 | |
| ≥6 years old | 94 | 0.1 ± 0.3 | 0.3 ± 0.6 | 0.2 ± 0.4 | 0.08 | |
| Number of hospital readmissions | Overall | 1031 | 0.2 ± 0.6 | 0.6 ± 1.4 | 0.7 ± 1.5 | <0.001 |
| Non-white | 438 | 0.2 ± 0.6 | 0.6 ± 1.1 | 0.2 ± 0.4 | 0.001 | |
| Hispanic | 119 | 0.2 ± 0.7 | 0.2 ± 0.4 | 1.3 ± 2.8 | 0.19 | |
| Mild/Moderate BPD | 308 | 0.2 ± 0.6 | 0.4 ± 0.8 | 0.4 ± 1.1 | 0.014 | |
| Severe BPD | 690 | 0.1 ± 0.5 | 0.7 ± 1.5 | 0.6 ± 1.6 | <0.001 | |
| <3 years old | 828 | 0.1 ± 0.5 | 0.6 ± 1.0 | 0.7 ± 1.7 | <0.001 | |
| 3-5 years old | 150 | 0.2 ± 0.7 | 1.0 ± 2.2 | 0.8 ± 1.4 | 0.013 | |
| ≥6 years old | 94 | 0.2 ± 0.8 | 0.1 ± 0.2 | 0.1 ± 0.3 | 0.94 | |
| Number of antibiotic courses | Overall | 1019 | 0.3 ± 0.9 | 1.0 ± 1.7 | 0.7 ± 1.0 | <0.001 |
| Non-white | 439 | 0.3 ± 0.7 | 0.7 ± 1.2 | 0.7 ± 0.8 | <0.001 | |
| Hispanic | 119 | 0.2 ± 0.6 | 1.1 ± 2.0 | 0.3 ± 0.5 | 0.08 | |
| Mild/Moderate BPD | 302 | 0.3 ± 1.1 | 0.7 ± 1.1 | 0.6 ± 1.1 | <0.001 | |
| Severe BPD | 684 | 0.3 ± 0.7 | 1.0 ± 1.9 | 0.7 ± 1.0 | <0.001 | |
| <3 years old | 820 | 0.2 ± 0.6 | 0.7 ± 1.2 | 0.6 ± 1.1 | <0.001 | |
| 3-5 years old | 147 | 0.5 ± 1.6 | 1.7 ± 2.3 | 0.8 ± 1.2 | <0.001 | |
| ≥6 years old | 93 | 0.4 ± 1.3 | 1.2 ± 1.7 | 1.1 ± 0.9 | 0.001 | |
| Number of systemic steroid courses | Overall | 1012 | 0.1 ± 0.6 | 0.9 ± 1.5 | 1.0 ± 1.4 | <0.001 |
| Non-white | 436 | 0.1 ± 0.6 | 0.8 ± 1.0 | 1.1 ± 1.4 | <0.001 | |
| Hispanic | 111 | 0.1 ± 0.3 | 0.6 ± 0.9 | 0.6 ± 0.9 | 0.002 | |
| Mild/Moderate BPD | 305 | 0.2 ± 0.9 | 0.9 ± 1.3 | 0.6 ± 1.1 | <0.001 | |
| Severe BPD | 675 | 0.1 ± 0.4 | 0.8 ± 1.6 | 1.0 ± 1.5 | <0.001 | |
| <3 years old | 811 | 0.1 ± 0.4 | 0.6 ± 1.1 | 0.8 ± 1.3 | <0.001 | |
| 3-5 years old | 149 | 0.3 ± 1.2 | 1.4 ± 2.4 | 0.8 ± 0.9 | <0.001 | |
| ≥6 years old | 93 | 0.2 ± 0.6 | 0.9 ± 1.2 | 1.3 ± 1.8 | 0.001 |
RESULTS
Demographic and Clinical Characteristics:
The study population consisted of 1049 preterm individuals from 13 tertiary care centers with a mean (± S.D.) number of 2.1±1.8 (Range: 1, 15; total number of questionnaires: 2155) BPD control questionnaires per subject (Table 1). The study population was 45.3% female with 43.5% and 11.6% self-identifying as non-white and Hispanic, respectively. The mean gestational age at birth was 26.8±2.6 weeks and the mean birth weight was 902±400 grams. Many subjects had a prolonged initial hospital stay with mean duration of 4.8±3.1 months reflecting the high proportion of participants with severe BPD (66.9%) and pulmonary hypertension (23.1%).
External Measures and Sum Score:
The mean age at the time of the first BPD control questionnaire was 1.9±2.4 years with 56.2% under 1 year of age (Table 2). The score on the BPD control questionnaire was 22.8±3.4, and by score category, the majority of caregivers (86.2%) felt their child’s symptoms were under control with 50.0% reporting a maximal score of 25. Of note, the percentages of caregivers indicating good control were similar among those with mild BPD (83.3%), moderate BPD (87.4%), and severe BPD (86.8%)(p=0.30) as well as pulmonary hypertension (84.4%) versus no pulmonary hypertension (87.7%)(p=0.42). There were a low number of acute respiratory events per subject, less than one for each of the following: sick visits, emergency department visits, hospital readmissions, antibiotic use, and systemic steroid use.
Demographic and Clinical Predictors of Sum Score:
Generalized estimating equations demonstrated that none of the assessed demographic factors, including gestational age or BPD severity, were associated with sum scores from outpatient clinic visits (Table 3).
Internal Reliability:
Internal reliability for the BPD control questionnaire for each subject was acceptable as assessed by Cronbach α (0.74; n=1049). Subgroup internal reliability was similar for non-white subjects (0.72; n=446), Hispanic subjects (0.78; n=119), mild BPD (0.69; n=84), moderate BPD (0.66; n=230), and severe BPD (0.76; n=702). Reliability was also similar by age groups, including those less than 3 years old (0.69; n=841), 3 to 5 years (0.80; n=128), and 6 years and older (0.78; n=80).
Test-Retest Differences:
For the 443 subjects who had at least 2 BPD control questionnaires, the mean scores between the first and second questionnaires were not different (First: 23.2±3.1; second: 23.0±3.4; p=0.24). The mean time elapsed between questionnaires was 4.3±6.4 months. A regression model did not identify an association between difference in scores and time elapsed (p=0.23).
Construct Validity:
The sum score from the BPD control questionnaire demonstrated construct validity with all five external measures of respiratory acute care use (sick visits, emergency department visits, hospital readmissions, antibiotic use, and systemic steroid use)(Table 4). The negative Spearman correlation coefficients reflect that higher sum scores represent better control and higher frequencies of respiratory care use suggest poorer control. While validity was demonstrated by p values for all demographic subgroups except for hospital readmissions for subjects 6 years of age and older, it should be noted that most correlation coefficients ranged between −0.2 and −0.4.
Discriminant Properties:
To assess whether the sum scores discriminated by external measures of respiratory disease severity, Kruskal Wallis tests were used to compare sum score categories of control (controlled, partially controlled, uncontrolled) to external measures of care use (Table 5). The distribution of acute care events differed for at least one category of sum score for the entire study population and almost all demographic subgroups except emergency department visits and hospital readmissions for subjects 6 years of age and older, and hospital readmissions for subjects self-identifying as Hispanic.
Predictive Nature of Sum Score Categories:
GEE models adjusted by visit age and clustered by subject were used to determine whether categories of sum scores (controlled, partially controlled, and uncontrolled) were predictive of sick visits, emergency department visits, or hospital readmissions (E-Table 1). Compared to individuals with sum scores categorized as controlled, partially controlled and uncontrolled individuals had a 5.6 and 9.9 times higher likelihood of a sick visit, respectively. Uncontrolled individuals had a 1.8 times higher likelihood of sick visits compared to partially controlled individuals (p=0.031). Similarly, compared to individuals with sum scores categorized as controlled, partially controlled and uncontrolled individuals had a 3.9 and 5.3 times higher likelihood of an emergency department visit, respectively. Lastly, compared to individuals with sum scores categorized as controlled, partially controlled and uncontrolled individuals had a 4.3 and 5.7 times higher likelihood of a hospital readmission, respectively. However, there were no differences in likelihood for emergency department visits (p=0.26) or admissions (p=0.29) between partially controlled and uncontrolled individuals.
DISCUSSION
Clinical research into outcomes of respiratory disease secondary to prematurity is hampered by a paucity of validated tools to objectively assess disease severity in young children. In this study, we provide a new measure of respiratory control in children with a diagnosis of BPD. Our tool, which is a modification of an existing validated instrument for pediatric asthma control,16 demonstrates reliability and the ability to discriminate disease severity when compared to external measures of disease severity in a real world population of over 1000 preterm infants and children recruited from tertiary care centers across the U.S. The brevity of our tool (5 Likert scale questions) makes it feasible to deploy in a variety of clinical and research situations.
In general, the majority of BPD control questionnaires obtained (86.8%) reflected good control of respiratory symptoms. However, disease that was partially or not controlled based on sum scores was not associated with any of the demographic factors assessed; this may potentially suggest that other outpatient factors, such as daycare attendance,21,22 secondhand smoke exposure,23,24 or exposure to air pollution,25,26 could play a larger role in disease control than the demographic or clinical characteristics assessed. Conversely, BPD control could also be influenced by genetic factors, such as a family history of asthma.27 Further work is needed to assess the outpatient influences on preterm respiratory disease.
In addition to demonstrating reliability and the ability to discriminate between controlled individuals versus others in the entire study population, we were able to demonstrate the vast majority of these findings in several key demographic groups. Specifically, our instrument demonstrates the generalizability of these findings in non-white and Hispanic groups, mild/moderate versus severe BPD, and in several age categories. We would note that with regards to construct validity, we did observe significant correlations, albeit of small magnitude. While we did observe validity in older ages (≥6 years of age), we acknowledge that we have less data in their age group with a potential recruitment bias. Nevertheless, our questionnaire may have some utility in this older age group when spirometry is not available. Additionally, neurodevelopmental issues, which are more common in preterm individuals28 may preclude performing spirometry. Lastly, our questionnaire can also be used to identify patients who may be at higher risk of sick visits, emergency department visits, or hospital readmissions. We observed a four to five-fold increased risk of these acute care visits in subjects who had partial or no control of respiratory symptoms on the BPD control questionnaire. Patients identified to be at risk could be prioritized for antiviral measures, potentially the prescription of inhaled corticosteroids, and counseling to avoid situations, such as daycare, which have a higher potential for contracting respiratory infections.
Limitations:
One limitation for our study is a population weighted towards severe BPD and those less than 3 years of age, which reflects the patient populations seen at our tertiary care centers for respiratory follow-up. However, we observed similar reliability and discriminative properties in subjects with mild/moderate BPD compared to severe BPD, and across age groups, although we did have smaller numbers of subjects with less well controlled disease. We would also note that we observed small correlations, albeit significant, in our construct validity analysis. Additionally, score categories were based on the ACT, and it is possible that different ranges may perform better for individuals with BPD. Also, our instrument assesses measures of respiratory symptoms as control and does not include other important features of severe BPD, including hypoxia, chronic respiratory medication use (e.g., scheduled use of beta-agonists, diuretics, and inhaled corticosteroids), and/or poor growth. Our study may also be weighted towards more urban populations given the locations of our outpatient clinics. Another limitation is that we were unable to adjust for the time periods between when external measures were assessed owing to IRB restrictions on obtaining dates; there is also a potential for periods of time where external measures were not assessed. However, we would suspect that this would bias our results towards the null; while subjects with more severe disease are more likely to have more frequent follow-up (shorter time periods between external event assessment), they are also more likely to have external events, perhaps making them appear more similar to their mild/moderate disease counterparts in terms of rates of events. Our instrument is also subject to reporting bias as it is based on caregiver report; however, our data were collected in real-world settings, so we would expect the instrument in practice to function similarly to how it did in the study. Lastly, as no test-retest differences were observed (which may be a function of most subjects having good control), future work is needed to determine if the questionnaire is appropriate for assessing clinical responsiveness longitudinally.
Conclusions:
Our study provides a tool for assessing respiratory control in children with BPD that is reliable, has discriminant properties, and is suggestive of validity. Most children with BPD assessed at our tertiary centers had good control of disease by questionnaire. We hope our tool can provide standardized data for clinical care and research studies. Further work is needed to identify modifiable predictors of disease control and link scores from our BPD control questionnaire to other measures of respiratory health such as lung function testing, especially for infants and younger children.
Supplementary Material
Funding:
Children’s Hospital of Philadelphia (JMC), NIH/NHLBI K23 HL136851 (LP Hayden).
Footnotes
Conflicts of Interest: No conflict of interest declared.
Data Availability Statement:
Data available on request from the authors.
REFERENCES
- 1.Martin JA, Hamilton BE, Osterman MJ. Births in the United States, 2021. NCHS Data Brief 2022:1–8. [PubMed] [Google Scholar]
- 2.Cao G, Liu J, Liu M. Global, Regional, and National Incidence and Mortality of Neonatal Preterm Birth, 1990-2019. JAMA pediatrics 2022;176:787–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Northway WH Jr., Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. The New England journal of medicine 1967;276:357–68. [DOI] [PubMed] [Google Scholar]
- 4.Baraldi E, Filippone M. Chronic lung disease after premature birth. The New England journal of medicine 2007;357:1946–55. [DOI] [PubMed] [Google Scholar]
- 5.Villosis MFB, Barseghyan K, Ambat MT, Rezaie KK, Braun D. Rates of Bronchopulmonary Dysplasia Following Implementation of a Novel Prevention Bundle. JAMA Netw Open 2021;4:e2114140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abman SH, Collaco JM, Shepherd EG, et al. Interdisciplinary Care of Children with Severe Bronchopulmonary Dysplasia. The Journal of pediatrics 2017;181:12–28 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duijts L, van Meel ER, Moschino L, et al. European Respiratory Society guideline on long-term management of children with bronchopulmonary dysplasia. The European respiratory journal 2020;55. [DOI] [PubMed] [Google Scholar]
- 8.Cristea AI, Ren CL, Amin R, et al. Outpatient Respiratory Management of Infants, Children, and Adolescents with Post-Prematurity Respiratory Disease: An Official American Thoracic Society Clinical Practice Guideline. American journal of respiratory and critical care medicine 2021;204:e115–e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary Dysplasia: Executive Summary of a Workshop. The Journal of pediatrics 2018;197:300–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jobe AH, Bancalari E. Bronchopulmonary dysplasia. American journal of respiratory and critical care medicine 2001;163:1723–9. [DOI] [PubMed] [Google Scholar]
- 11.Jensen EA, Dysart K, Gantz MG, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. American journal of respiratory and critical care medicine 2019;200:751–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aoyama BC, Collaco JM, McGrath-Morrow SA. Predictors of pulmonary function at 6 years of age in infants with bronchopulmonary dysplasia. Pediatric pulmonology 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manti S, Galdo F, Parisi GF, et al. Long-term effects of bronchopulmonary dysplasia on lung function: a pilot study in preschool children’s cohort. J Asthma 2021;58:1186–93. [DOI] [PubMed] [Google Scholar]
- 14.Ducharme FM, Smyrnova A, Lawson CC, Miles LM. Reference values for respiratory sinusoidal oscillometry in children aged 3 to 17 years. Pediatric pulmonology 2022;57:2092–102. [DOI] [PubMed] [Google Scholar]
- 15.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. The American review of respiratory disease 1992;145:1321–7. [DOI] [PubMed] [Google Scholar]
- 16.Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113:59–65. [DOI] [PubMed] [Google Scholar]
- 17.Collaco JM, Agarwal A, Austin ED, et al. Characteristics of infants or children presenting to outpatient bronchopulmonary dysplasia clinics in the United States. Pediatric pulmonology 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jobe AH, Bancalari E. Bronchopulmonary dysplasia. American Journal of Respiratory and Critical Care Medicine 2001:1723–9. [DOI] [PubMed] [Google Scholar]
- 19.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986;42:121–30. [PubMed] [Google Scholar]
- 20.Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ 2011;2:53–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGrath-Morrow SA, Agarwal A, Alexiou S, et al. Daycare Attendance is Linked to Increased Risk of Respiratory Morbidities in Children Born Preterm with Bronchopulmonary Dysplasia. The Journal of pediatrics 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGrath-Morrow SA, Lee G, Stewart BH, et al. Day care increases the risk of respiratory morbidity in chronic lung disease of prematurity. Pediatrics 2010;126:632–7. [DOI] [PubMed] [Google Scholar]
- 23.Collaco JM, Aherrera AD, Breysse PN, Winickoff JP, Klein JD, McGrath-Morrow SA. Hair nicotine levels in children with bronchopulmonary dysplasia. Pediatrics 2015;135:e678–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collaco JM, Aherrera AD, Ryan T, McGrath-Morrow SA. Secondhand smoke exposure in preterm infants with bronchopulmonary dysplasia. Pediatric pulmonology 2014;49:173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collaco JM, Morrow M, Rice JL, McGrath-Morrow SA. Impact of road proximity on infants and children with bronchopulmonary dysplasia. Pediatric pulmonology 2020;55:369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rice JL, McGrath-Morrow SA, Collaco JM. Indoor Air Pollution Sources and Respiratory Symptoms in Bronchopulmonary Dysplasia. The Journal of pediatrics 2020;222:85–90 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGlynn JR, Aoyama BC, Collaco JM, McGrath-Morrow SA. Family history of asthma influences outpatient respiratory outcomes in children with BPD. Pediatric pulmonology 2021;56:3265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell EF, Hintz SR, Hansen NI, et al. Mortality, In-Hospital Morbidity, Care Practices, and 2-Year Outcomes for Extremely Preterm Infants in the US, 2013-2018. JAMA : the journal of the American Medical Association 2022;327:248–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request from the authors.


