Summary
Background
The suicide mortality rate in the Region of the Americas has been increasing, while decreasing in all other World Health Organization regions; highlighting the urgent need for enhanced prevention efforts. Gaining a better understanding of population-level contextual factors associated with suicide may aid such efforts. We aimed to evaluate the contextual factors associated with country-level, sex-specific suicide mortality rates in the Region of the Americas for 2000–2019.
Methods
Annual sex-specific age-standardized suicide mortality estimates were obtained from the World Health Organization (WHO) Global Health Estimates database. To investigate the sex-specific suicide mortality rate trend over time in the region, we performed joinpoint regression analysis. We then applied a linear mixed model to estimate the effects of specific contextual factors on the suicide mortality rate across countries in the region over time. All potentially relevant contextual factors, obtained from the Global Burden of Disease Study 2019 covariates and The World Bank, were selected in a step-wise manner.
Findings
We found that the mean country-level suicide mortality rate among males in the region decreased as health expenditure per capita and the proportion of the country with a moderate population density increased; and increased as the death rate due to homicide, prevalence of intravenous drug use, risk-weighted prevalence of alcohol use, and unemployment rate increased. The mean country-level suicide mortality rate among females in the region decreased as the number of employed medical doctors per 10,000 population and the proportion of the country with a moderate population density increased; and increased when relative education inequality and unemployment rate increased.
Interpretation
Although there was some overlap, the contextual factors that significantly impacted the suicide mortality rate among males and females were largely different, which mirrors the current literature on individual-level risk factors for suicide. Taken together, our data supports that sex should be considered when adapting and testing suicide risk reduction interventions, and when developing national suicide prevention strategies.
Funding
This work received no funding.
Keywords: Contextual factors, Suicide, Self-harm, Region of the Americas, Ecological study
Research in context.
Evidence before this study
Despite other World Health Organization regions experiencing a decline in their suicide mortality rate in recent years, the Region of the Americas has been experiencing an increase. However, there are notable between-country differences in the region. Yet, no study on the effect of specific contextual factors (i.e., factors which reflect particular characteristics of a particular group, community, or society) on the suicide mortality rate exists for the region. We searched the PubMed database with no date or language restrictions up to April 15, 2022, for published between-country comparisons of contextual factors associated with suicide mortality rate. The search terms used were: “suicide” (MeSH) AND (“ecological observations” OR “ecological study” OR “ecological analysis”). Although a handful of published studies were identified, they were largely limited to single social or economic factors. Further, those studies that restricted their analyses to a certain geographic sub-region were for European countries only.
Added value of this study
Our findings provide evidence that certain contextual factors are associated with country-level suicide mortality rates in the Region of the Americas. Specifically, using 20-years of data, we identified the following contextual factors as having contributed to the suicide mortality rates in the region, namely: alcohol use, education inequality, health expenditure, homicide rate, intravenous drug use, number of employed medical doctors, population density, and unemployment rate. To the best of our knowledge, this is the first study to estimate the impact of specific contextual factors on country-level suicide mortality rates in the region.
Implications of all the available evidence
This study adds to the growing evidence that certain country-level contextual factors may be worth exploring as potential indirect suicide prevention mechanisms. Multisectoral measures targeting health and social well-being in society, which are informed and developed using evidence on local contextual factors, should be emphasized in suicide prevention initiatives.
Introduction
Suicide is a major public health problem, particularly in the Region of the Americas, where the suicide mortality rate increased between 2000 and 2019,1 despite national and international efforts to reduce its occurrence.2,3 In 2019, there were over 97 thousand suicides in the Region of the Americas, resulting in a suicide mortality rate of 9.0 per 100,000 population (14.2 per 100,000 males and 4.1 per 100,000 females).4 Within the region, however, the suicide mortality rate varied considerably by sub-region, with the North America region having the highest rate (14.1 per 100,000 population) and the Andean Area region having the lowest rate (3.9 per 100,000 population); likely due to notable sociocultural differences between regions (e.g.,5). Further, there were stark differences in the suicide mortality rate between countries, for example, ranging from 0.3 per 100,000 population (Barbados) up to 65.0 per 100,000 population (Guyana).4 Although, such between-country variation is noted throughout the literature, studies on the effects of specific contextual factors (i.e., factors which reflect particular characteristics of a particular group, community, or society) on the suicide mortality rate across countries are scarce,6, 7, 8, 9 and no study focusing on the Region of the Americas exists. This represents a significant gap in knowledge, given that understanding population-level contextual factors associated with suicide can inform targeted suicide prevention efforts.10 In fact, the uniqueness of the Americas and the need for between country comparisons to better understand what political, social, cultural and economic factors may be contributing to country-level suicide mortality rates has been noted in the literature.10
With that being said, it is imperative that an investigation into the contextual factors associated with suicide take sex into consideration, as the suicide mortality rate ratio for males-to-females differs quite notably across countries.4 The sex difference in suicide mortality is a culture-bound phenomenon, meaning that cultural expectations about gender and suicide strongly determine both its existence and magnitude.11,12 As such, it is also likely that the contextual factors associated with suicide will be different for males and females. Sex-specific contextual factor analyses have the potential to identify the conditions that may be influencing the suicide mortality rate of one sex more than the other and thus, can further inform suicide prevention strategies. On the individual-level, the identification of risk/protective factors for suicide is helpful in identifying those most at risk. However, prevention efforts must not only target vulnerable populations, but also target the contextual factors contributing to the suicide mortality burden in a given country. In fact, population-level approaches to suicide prevention have been called for.13
The impact of population-level contextual factors on mental health has been highlighted by Lund et al.,14 who developed an evidence-informed conceptual framework for the social determinants of mental disorders. The framework is comprised of demographic, economic, neighborhood, environmental events, and social and cultural domains; and the association between their macro-level indicators and suicide is grounded in the literature–for example, for economic measures see,15,16 substance use measures see,17,18 and health care measures see.18,19
Therefore, in the current study, we aimed to evaluate the contextual factors associated with country-level sex-specific suicide mortality rates in the Region of the Americas for 2000–2019. By doing so, we hope to help health authorities determine their focus for public health strategies targeting suicide prevention; aid in the development and tailoring of national suicide prevention efforts to maximize benefits; and inform the development and implementation of national suicide prevention strategies.
Methods
A cross-sectional ecological study design was used to evaluate the population-level contextual factors associated with country-level sex-specific suicide mortality rates in the Region of the Americas.
Data
Annual sex-specific age-standardized suicide mortality estimates were obtained from the World Health Organization (WHO) Global Health Estimates database (https://www.who.int) for a total of 33 countries of the Region of the Americas for 2000–2019: Antigua and Barbuda, Argentina, Bahamas, Barbados, Belize, Bolivia (Plurinational State of), Brazil, Canada, Chile, Colombia, Costa Rica, Cuba, Dominican Republic, Ecuador, El Salvador, Grenada, Guatemala, Guyana, Haiti, Honduras, Jamaica, Mexico, Nicaragua, Panama, Paraguay, Peru, Saint Lucia, Saint Vincent and the Grenadines, Suriname, Trinidad and Tobago, United States of America, Uruguay, and Venezuela (Bolivarian Republic of). The suicide mortality rate estimates are derived from primary data, and when absent, estimates are derived from statistical modeling. In brief, total deaths by 5-year age groups and sex were estimated by the WHO for each country by applying the WHO life table death rates20 to the estimated resident populations prepared by the UN Population Division in its 2019 revision.21 In order to facilitate international comparability, age-standardized suicide mortality rates were computed using the WHO standard population,22 which assumes one standard age distribution of the population in all countries. Additional details of the methods used by the WHO to compute the suicide mortality rate estimates used here, as well as data sources can be found elsewhere.23
For the selection of the population-level contextual factors to be included in the modeling, we first identified all potentially relevant contextual factors from the Global Burden of Disease (GBD) Study 2019 covariates (http://ghdx.healthdata.org) and The World Bank (https://data.worldbank.org), based on the current literature (see Table 1 for a complete list). All covariates were year- and country-specific; some were also sex-specific and age-standardized, as indicated in Table 1.
Table 1.
Covariates considered for inclusion.
| Covariate | Sex-specific | Age-standardized |
|---|---|---|
| Education Absolute Inequality (AAID) | X | X |
| Education Relative Inequality (GINI) | X | X |
| Health expenditure per capita, in 2018 USD | ||
| Gross domestic product based on purchasing power parity (GDP-PPP) | ||
| Healthcare access and quality (HAQ) index | ||
| Hospital beds per 1000 people | ||
| Level of educational attainment per capita | X | X |
| Mean alcohol consumption, measured in grams per day | X | X |
| Mean mortality rate in the previous ten years due to military operations and terrorism, disasters, and famines (protein-energy malnutrition deaths) measured from year's end | ||
| Mortality rate due to homicide | X | X |
| Mortality rate due to protein-energy malnutrition | ||
| Number of cigarettes or cigarette equivalents consumed per adult aged 15+ years per year | ||
| Number of employed health workers (of any specialty) per 10,000 population | ||
| Number of employed medical doctors per 10,000 population | ||
| Percent of population with access to improved toilet types as defined by the Joint Monitoring Program | ||
| Prevalence of diabetes | X | X |
| Proportion of a population that abstain from alcohol | X | X |
| Proportion of a population that binge drink | X | X |
| Proportion of a population using intravenous drugs | X | X |
| Proportion of the country with population density between 150 and 300 people per km2 | ||
| Proportion of the country with population density between 300 and 500 people per km2 | ||
| Proportion of the country with population density between 500 and 1000 people per km2 | ||
| Proportion of the country with population density over 1000 people per km2 | ||
| Proportion of the country with population density under 150 people per km2 | ||
| Proportion of the employed population ages 15–69 working as professionals (according to ISCO classifications) | ||
| Proportion of the population living in urban areas | ||
| Proportion of the population that has consumed alcohol in the past year | X | X |
| Proportion of the population that smoke | X | X |
| Proportion of the population with 0 years of education | X | X |
| Proportion of the population with at least 12 years of education | X | X |
| Proportion of the population with at least 6 years of education | X | X |
| Socio-demographic index | ||
| Summary exposure valuea for alcohol use | X | |
| Summary exposure valuea for childhood sexual abuse | X | |
| Summary exposure valuea for drug use | X | |
| Summary exposure valuea for intimate partner violence | X | |
| Summary exposure valuea for low physical activity | X | |
| Summary exposure valuea for no access to handwashing facility | X | |
| Summary exposure valuea for second-hand smoke | X | |
| Summary exposure valuea for smoking | X | |
| Summary exposure valuea for unsafe sanitation | X | |
| Summary exposure valuea for unsafe water source | X | |
| Total fertility rate | ||
| Unemployment rateb | X |
Summary exposure value (SEV) - a measure of a population's exposure to a risk factor that considers the extent of exposure by risk level and the severity of that risk's contribution to disease burden. SEV takes the value zero when no excess risk for a population exists and the value one when the population is at the highest level of risk; we report SEV on a scale from 0% to 100% to emphasize that it is risk-weighted prevalence.
Not available for Antigua and Barbuda and Grenada.
Statistical analysis
Trend analysis
In order to identify trends in the sex-specific age-standardized suicide mortality rate in the Region of the Americas over time, joinpoint regression analyses were performed,24 using the Joinpoint Regression Program, version 4.8.0.1.25 Based on the maximum number of joinpoints specified (i.e., three24), linear segments were fitted to the data. Using a Monte Carlo Permutation method, the fewest number of linear segments such that an additional joinpoint does not add a statistically significant linear trend was selected.24 Lastly, the slope coefficient for each individual linear segment was transformed to an annual percent change (APC), and the parametric method was used to estimate the 95% CI for the APC of each linear segment. The average annual percent change (AAPC), a weighted average of the APCs to summarize the trend over a predetermined fixed interval, was also computed as a summary measure of the trend over the past 20 years.26
Analysis of contextual factors
A linear mixed model was used to analyze the effects of specific contextual factors on the suicide mortality rate across countries over time. The linear mixed model offers a number of advantages when there are missing data points and a hierarchical data structure. With multiple correlated data points for each country, the linear mixed model allowed us to systematically account for country-level variability (between countries) and subject-level variability (within countries). The Hausman test was used to confirm the choice of a random effects model over a fixed effect model (p = 0.990 for males and p = 0.980 for females).27 We assumed the suicide mortality rate and its growth rate (i.e., the intercept and slope) may depend on the countries, and thus, a normally distributed random intercept and a random slope were included in all linear mixed models. More specifically, the random intercept and slope pairs followed a bivariate normal distribution centered at the origin with variance-covariance matrix, which allowed the correlation between random intercepts and slopes. Univariate analyses were performed to identify those covariates significantly associated with the sex-specific suicide mortality rate. Pearson's correlation coefficient was then used to measure linear correlation between covariates considered to be potentially redundant (Supplementary Table S1). When covariates were identified to be highly correlated (i.e., r = +/−0.6 to +/−1.0) with one another, the covariate with the largest effect size and lowest p-value was retained (Supplementary Table S2). Likelihood ratio test was used to measure the significance of all remaining covariates. When a covariate was identified to be statistically significant (i.e., p < 0.05), the covariate was retained. Then a full model was fit (for a list of variables included in the full models see Supplementary Table S3). Akaike information criterion (AIC) was used to assist with selecting the most appropriate model. A lower AIC value indicates a better fit; as such, the model with the lowest AIC was selected. The final model was further optimized by removing non-significant covariates if their inclusion did not improve model fit (as per the AIC). In order to account for the temporal trend of the suicide mortality rate, “year” was included as a covariate in all models. Significance was set at α ≤ 0.05. All analyses were performed using R version 4.1.2.28
Ethical statement
Institutional review board approval and informed consent were not required, as the current study utilized aggregated data obtained from public domain databases.
Role of the funding source
This research received no funding.
Results
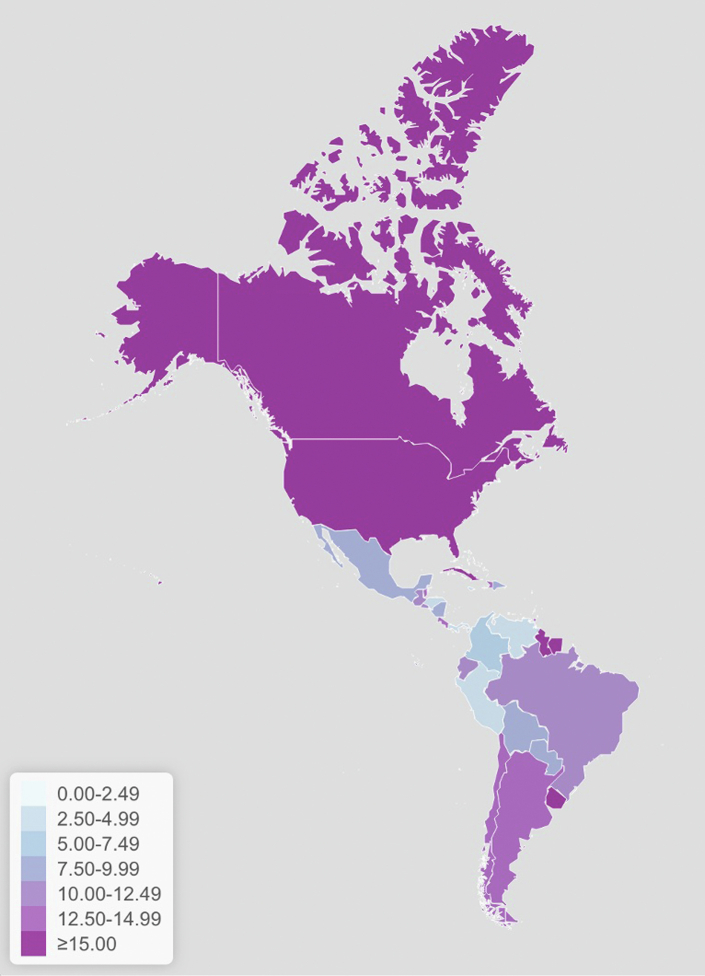
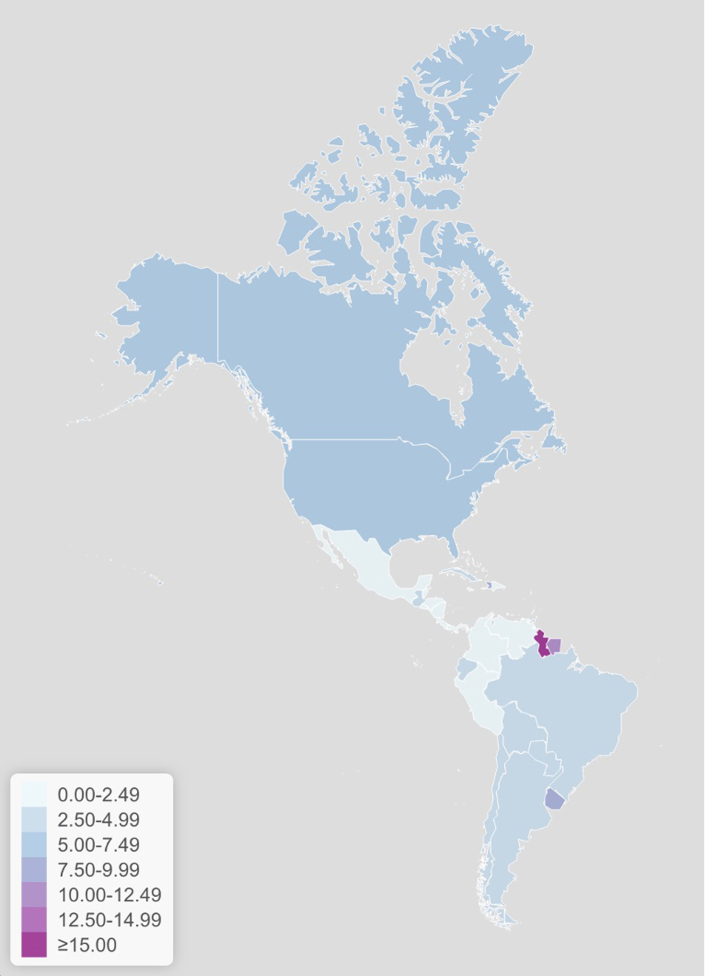
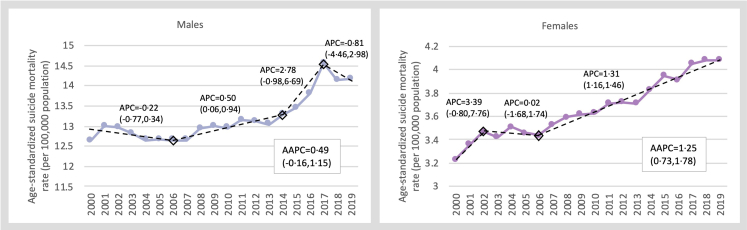
For the age-standardized suicide mortality rates per 100,000 population among males and females in the Region of the Americas by country for 2019, see Figs. 1 and 2, respectively. As depicted, the suicide mortality rate in the vast majority of countries in the region is notably higher among males than females. While the suicide mortality rate among males in the Region of the Americas showed an overall upward trend between 2000 and 2019, the AAPC was not statistically significant. However, the suicide mortality rate among females significantly increased annually, on average, by 1.25% (95% CI: 0.73%, 1.78%) between 2000 and 2019 (Fig. 3). See Supplementary Figs. S1 and S2 for the suicide mortality rate over time in the region by country for males and females, respectively.
Fig. 1.
Age-standardized suicide mortality rates per 100,000 population among males in the Region of the Americas, 2019.
Fig. 2.
Age-standardized suicide mortality rates per 100,000 population among females in the Region of the Americas, 2019.
Fig. 3.
Age-standardized suicide mortality rate among males and females and the trend over time in the Region of the Americas, 2000–2019. Diamonds indicate identified points of inflection. AAPC: Average annual percent change; APC: Annual percent change.
Contextual factors for the suicide mortality rate among male individualss
The final model for the suicide mortality rate among males in the Region of the Americas included the following significant covariates: a risk-weighted prevalence of alcohol use (in %), health expenditure per capita in 2018 USD (in $), death rate due to homicide (per 100,000 population), age-standardized proportion of a population using intravenous drugs (per 1000 population), proportion of the country with population density between 500 and 1000 people per km2 (in %), and unemployment rate (in %) (Table 2).
Table 2.
Final linear mixed model for contextual factors associated with county-level suicide mortality rate among male individuals in the Region of the Americas.
| Covariates | Estimate | 95% CI |
p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Intercept | 2.75 | −3.21 | 8.70 | 0.366 |
| Year | −0.12 | −0.24 | 0.00 | 0.057 |
| Alcohol use, a risk-weighted prevalence (%) | 0.48 | 0.17 | 0.79 | 0.002 |
| Health expenditure per capita, in 2018 USD ($) | −0.002 | −0.003 | −0.0003 | 0.019 |
| Death rate due to homicide, per 100,000 population | 0.002 | 0.0006 | 0.003 | 0.004 |
| Intravenous drug use, age-standardized proportion (per 1000 population) | 2.12 | 0.87 | 3.37 | 0.001 |
| Proportion of the country with a population density between 500 and 1000 people per km2 (%) | −0.03 | −0.06 | −0.002 | 0.035 |
| Unemployment rate (%) | 0.15 | 0.06 | 0.23 | 0.001 |
While holding all other covariates in the model constant, the mean suicide mortality rate among males in the region increased by 0.48 per 100,000 population (95% CI: 0.17, 0.79 per 100,000 population) for every 1-unit increase in the risk-weighted prevalence of alcohol use; 0.002 per 100,000 population (95% CI: 0.0006, 0.003 per 100,000 population) for every 1-unit increase in the death rate due to homicide; 2.12 per 100,000 population (95% CI: 0.87, 3.37 per 100,000 population) for every 1-unit increase in the prevalence of intravenous drug use; and by 0.15 per 100,000 population (95% CI: 0.06, 0.23 per 100,000 population) for every 1-unit increase in the unemployment rate. The mean suicide mortality rate among males in the region decreased by −0.002 per 100,000 population (95% CI: −0.003, −0.0003 per 100,000 population) for every 1-unit increase in health expenditure per capita; and by −0.03 per 100,000 population (95% CI: −0.06, −0.002 per 100,000 population) for every 1-unit increase in the proportion of the country with population density between 500 and 1000 people per km2, while holding all other covariates in the model constant.
Contextual factors for the suicide mortality rate among female individuals
The final model for the suicide mortality rate among females in the Region of the Americas included the following significant covariates: education relative inequality (a standard measure of education inequality that ranges from 0 [no inequality] to 1 [high inequality]), number of employed medical doctors per 10,000 population, proportion of the country with population density between 500 and 1000 people per km2 (in %), and unemployment rate (in %) (Table 3).
Table 3.
Final linear mixed model for contextual factors associated with county-level suicide mortality rate among female individuals in the Region of the Americas.
| Covariates | Estimate | 95% CI |
p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Intercept | 1.17 | −1.90 | 4.24 | 0.455 |
| Year | 0.06 | 0.02 | 0.10 | 0.002 |
| Education relative inequalitya | 10.98 | 3.45 | 18.51 | 0.004 |
| Number of employed medical doctors per 10,000 population | −0.09 | −0.14 | −0.04 | 0.001 |
| Proportion of the country with a population density between 500 and 1000 people per km2 (%) | −0.01 | −0.02 | −0.002 | 0.015 |
| Unemployment rate (%) | 0.04 | 0.02 | 0.06 | 0.000 |
Ranges from 0 (no inequality) to 1 (high inequality).
While holding all other covariates in the model constant, the mean suicide mortality rate among females in the region increased by 10.98 per 100,000 population (95% CI: 3.45, 18.51 per 100,000 population) for every 1-unit increase in education inequality; and by 0.04 per 100,000 population (95% CI: 0.02, 0.06 per 100,000 population) for every 1-unit increase in the unemployment rate. The mean suicide mortality rate among females in the region decreased by −0.09 per 100,000 population (95% CI: −0.14, −0.04 per 100,000 population) for every 1-unit increase in the number of employed medical doctors per 10,000 population; and by −0.01 per 100,000 population (95% CI: −0.02, −0.002 per 100,000 population) for every 1-unit increase in the proportion of the country with population density between 500 and 1000 people per km2, while holding all other covariates in the model constant.
Discussion
In the current paper, we have identified a set of contextual factors that contribute to the suicide mortality rates in the Region of the Americas. Specifically, it can be deduced that as health expenditure per capita and the proportion of the country with a moderate population density increase, the suicide mortality rate among males tends to decrease; and that when the death rate due to homicide, prevalence of intravenous drug use, risk-weighted prevalence of alcohol use, and unemployment rate increase, the suicide mortality rate among males tends to increase. Among females, the suicide mortality rate tends to decrease as the number of employed medical doctors per 10,000 population and the proportion of the country with a moderate population density increase; and tends to increase when relative education inequality and unemployment rate increase.
Although most of the contextual factors identified seem relatively intuitive and are supported by the current literature (for example, for the relationship between suicide mortality rate and homicide rate see,29 unemployment rate see,30 alcohol and drug use see,31 and health expenditure see32,33), the proportion of the country with a moderate population density is less so at first glance. However, recently, Steelesmith et al.34 found that between 1999 and 2016, suicide rates were higher and increased more rapidly in rural than in large metropolitan US counties; suggesting that rural areas may be more sensitive to the impact of social deprivation than more metropolitan counties. Although increasing the population density of a country is not a realistic public health strategy for reducing the suicide mortality rate, improving social connectedness, and civic opportunities may be worth exploring as potential suicide prevention strategies.
As per the current literature, despite there being some similarities in the individual-level risk factors for suicidal behavior across sexes, there is also evidence of sex-specific risk factors.35 With the current investigation, we extend these findings, by showing that the contextual factors that are associated with the suicide mortality rate among males are not necessarily the same as those that are associated with the suicide mortality rate among females. There were only two contextual factors that were significantly associated with the suicide mortality rate among both males and females (for which the magnitude of the effect was different): population density and unemployment rate. The difference in the contextual factors associated with the suicide mortality rate among males and females was expected, given that there are important differences in suicidal behavior across sexes, in terms of aetiology and epidemiology.36,37 Although there is much to be learnt about such sex differences in suicide, differences in norms, practices and behaviors, as well as exposures and vulnerabilities are likely part of the story. For instance, males are less likely to engage in health-seeking behavior, and more likely to participate in risky behaviors such as heavy alcohol use.38,39 In addition to impacting the existence and magnitude of the sex difference in the suicide mortality rate, gender norms and expectations are also likely to influence the factors that increase the risk of suicide for each sex, and the strength of their effect. Although an in-depth review of each risk factor and their sex-specific mechanism is beyond the scope of this paper, the current study is intended to evoke hypotheses and spark further investigation into sex-specific risk relationships for suicide mortality, and their aetiology.
Our findings, coupled with the current literature, highlight that it is of vital importance that sex is considered when developing, adapting and testing suicide risk reduction interventions, and when developing national suicide prevention strategies. They also support the World Health Organization Live Life Approach to suicide prevention, which outlines six core pillars, including the need for situation analyses and multisectoral collaboration.23 As the contextual factors correlated with suicide mortality will vary by population group, among them different sexes, a situation analysis, which provides disaggregated data on local rates of suicide and self-harm, means of suicide, and available services and resources, among other information, is crucial to informing the planning and implementation of suicide prevention initiatives that are not one-size-fits-all. Additionally, key contextual factors linked to suicide, including alcohol and substance use, health expenditure per capita, homicide, unemployment and education inequality go beyond the purview of the health sector, necessitating whole-of-society collaboration and action that bring together diverse representatives from sectors such as Social Affairs and Welfare, Planning and Development, Education, and Labor/Employment, and people with lived experience of mental health issues and suicide, among others. These factors, and their unique impact on males and females, must also be integrated into multisectoral suicide prevention strategies and plans. Further, we would like to acknowledge that the association between the identified contextual factors and the suicide mortality rate could vary by age-group. This should be explored in the future, as such work could have important prevention implications.
Strengths and limitations
There are a few limitations of the current study that we must acknowledge. First, the country-level contextual factor measures are only a proxy based on the average in the population. Second, although gender is likely to be playing a role in the sex-differences observed, the data used were sex-specific. Third, it is possible, that both country-level suicide mortality rates and the effects estimated here are being influenced by additional confounding variables that were not controlled for. Fourth, due to low power, we chose a data-driven variable selection strategy, which may have resulted in the exclusion of factors that are in fact related to country-level suicide mortality rate. Fifth, the covariates obtained from the GBD study, although useful and informative, are largely estimations derived from statistical models. Lastly, our ability to determine causality is precluded by the ecological study design and the data-driven variable selection strategy. However, there are some notable strengths as well. First, the study design allowed us to investigate exposure data that is only available on a country-level. Second, the use of GBD study and The World Bank covariates and WHO Global Health Estimates for suicide mortality rates provides some reassurance against the potential for systematic differences between countries in recording suicide mortality and in the measurement of contextual factors. Lastly, to the best of our knowledge this is the first study to examine contextual factors associated with country-level suicide mortality rates in the Region of the Americas using 20-years of collected data.
Conclusion
In conclusion, by quantifying the association between population-level contextual factors and country-level suicide mortality rates in the region, we strive to improve scientific knowledge and provide decision-makers with the evidence needed to inform national suicide prevention strategies, by identifying areas of need for targeted prevention effort. Study findings suggest that increasing employment programs and services, access to and capacity of health services including treatment services for substance use, to name a few, may have the potential to reduce suicide mortality rates in the respective country. Overall, our results indicate that multisectoral measures targeting health and social well-being in society, which are informed and developed using evidence on local contextual factors, should be emphasized in suicide prevention initiatives.
Contributors
S.L.: Conceptualization, Methodology, Visualization, Writing – original draft. C.C.: Conceptualization, Writing – review & editing. H.J.: Formal analysis, Methodology. A.T.: Writing – review & editing. R.O.S.: Conceptualization, Supervision, Writing – review & editing. S.L. and H.J. had access to all data independently.
Data sharing statement
Data from the World Health Organization Global Health Estimates database and all other databases used in this study are publicly available. Our analysis code is available upon request to the corresponding author.
Editor's note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
S.L. received compensation from the Pan American Health Organization for carrying-out this investigation.
Footnotes
The author is a staff member of the Pan American Health Organization. The author alone is responsible for the views expressed in this publication, and they do not necessarily represent the decisions or policies of the Pan American Health Organization.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100450.
Appendix A. Supplementary data
References
- 1.World Health Organization . World Health Organization; Geneva, Switzerland: 2021. Suicide worldwide in 2019: global health estimates. [Google Scholar]
- 2.United Nations . United Nations; 2017. The sustainable development goals report. [Google Scholar]
- 3.World Health Organization . WHO; Geneva, Switzerland: 2013. Metal health action plan 2013-2020. [Google Scholar]
- 4.Pan American Health Organization (PAHO) Pan American Health Organization; Washington, D.C.: 2021. Suicide mortality in the Americas – regional report 2015-2019. [Google Scholar]
- 5.Mascayano F., Irrazabal M., Emilia W.D., et al. Suicide in Latin America: a growing public health issue. Rev Fac Cien Med Univ Nac Cordoba. 2015;72(4):295–303. [PubMed] [Google Scholar]
- 6.Burgess P., Pirkis J., Jolley D., Whiteford H., Saxena S. Do nations' mental health policies, programs and legislation influence their suicide rates? An ecological study of 100 countries. Aust N Z J Psychiatry. 2004;38(11-12):933–939. doi: 10.1080/j.1440-1614.2004.01484.x. [DOI] [PubMed] [Google Scholar]
- 7.Alothman D., Fogarty A. Global differences in geography, religion and other societal factors are associated with sex differences in mortality from suicide: an ecological study of 182 countries. J Affect Disord. 2020;260:67–72. doi: 10.1016/j.jad.2019.08.093. [DOI] [PubMed] [Google Scholar]
- 8.Kelly B.D., Davoren M., Mhaoláin Á.N., Breen E.G., Casey P. Social capital and suicide in 11 European countries: an ecological analysis. Soc Psychiatry Psychiatr Epidemiol. 2009;44(11):971. doi: 10.1007/s00127-009-0018-4. [DOI] [PubMed] [Google Scholar]
- 9.Rodríguez Ruzafa M., Carrasco Picazo J.P., Junquera Fernández G., Aguilar García-Iturrospe E.J. EUROLD: preliminary results of the ecological study on suicide and its associated socioeconomic variables in people over 85 in Europe. Int Psychogeriatr. 2022:1–3. doi: 10.1017/S1041610222000072. [DOI] [PubMed] [Google Scholar]
- 10.Stack S. Contributing factors to suicide: political, social, cultural and economic. Prev Med. 2021;152(Pt 1):106498. doi: 10.1016/j.ypmed.2021.106498. [DOI] [PubMed] [Google Scholar]
- 11.Canetto S.S., Sakinofsky I. The gender paradox in suicide. Suicide Life Threat Behav. 1998;28(1):1–23. [PubMed] [Google Scholar]
- 12.Canetto S.S. Women and suicidal behavior: a cultural analysis. Am J Orthopsychiatry. 2008;78(2):259–266. doi: 10.1037/a0013973. [DOI] [PubMed] [Google Scholar]
- 13.Blanco C., Wall M.M., Olfson M. A population-level approach to suicide prevention. JAMA. 2021;325(23):2339–2340. doi: 10.1001/jama.2021.6678. [DOI] [PubMed] [Google Scholar]
- 14.Lund C., Brooke-Sumner C., Baingana F., et al. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5(4):357–369. doi: 10.1016/S2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- 15.Catalano R., Goldman-Mellor S., Saxton K., et al. The health effects of economic decline. Annu Rev Public Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iemmi V., Bantjes J., Coast E., et al. Suicide and poverty in low-income and middle-income countries: a systematic review. Lancet Psychiatry. 2016;3(8):774–783. doi: 10.1016/S2215-0366(16)30066-9. [DOI] [PubMed] [Google Scholar]
- 17.Ramstedt M. Alcohol and suicide in 14 European countries. Addiction. 2001;96 Suppl 1:S59–S75. doi: 10.1080/09652140020021189. [DOI] [PubMed] [Google Scholar]
- 18.Rockett I.R.H., Jia H., Ali B., et al. Association of state social and environmental factors with rates of self-injury mortality and suicide in the United States. JAMA Netw Open. 2022;5(2):e2146591. doi: 10.1001/jamanetworkopen.2021.46591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tondo L., Albert M.J., Baldessarini R.J. Suicide rates in relation to health care access in the United States: an ecological study. J Clin Psychiatry. 2006;67(4):517–523. doi: 10.4088/jcp.v67n0402. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization Life tables by country. Geneva, Switzerland: Global Health Observatory Data Repository, World Health Organization. 2020. https://apps.who.int/gho/data/node.main.LIFECOUNTRY?lang=en Available from:
- 21.United Nations DoEaSA, Population Division World population prospects 2019, online edition. Rev. 1. New York, NY: United Nations. 2019. https://population.un.org/wpp/ Available from:
- 22.Ahmad O.B., Boschi-Pinto C., Lopez A.D., Murray C.J.L., Lozano R., Inoue M. World Health Organization; Geneva, Switzerland: 2001. Age standardization of rates: a new WHO standard. GPE discussion paper series: No. 31. [Google Scholar]
- 23.World Health Organization WHO methods and data sources for country-level causes of death 2000-2019. Geneva, Switzerland: Department of Data and Analytics, World Health Organization. 2020. https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_cod_methods.pdf?sfvrsn=37bcfacc_5 Available from:
- 24.Kim H.J., Fay M.P., Feuer E.J., Midthune D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 25.National Cancer Institute (NCI) Joinpoint trend analysis software. 4.8.0.1 ed. Maryland, USA: Statistical Research and Applications Branch, NCI. 2020. https://surveillance.cancer.gov/joinpoint Available from:
- 26.Clegg L.X., Hankey B.F., Tiwari R., Feuer E.J., Edwards B.K. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–3682. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amini S., Delgado M.S., Henderson D.J., Parmeter C.F. In: Essays in Honor of Jerry Hausman (Advances in Econometrics, Vol. 29) Baltagi B.H., Carter Hill R., Newey W.K., White H.L., editors. Emerald Group Publishing Limited; Bingley, UK: 2012. Fixed vs random: the Hausman test four decades later; pp. 479–513. [Google Scholar]
- 28.R Development Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2021. R: a language and environment for statistical computing. Version 4.1.2. [Google Scholar]
- 29.Machado D.B., McDonald K., Castro-de-Araujo L.F.S., et al. Association between homicide rates and suicide rates: a countrywide longitudinal analysis of 5507 Brazilian municipalities. BMJ Open. 2020;10(11) doi: 10.1136/bmjopen-2020-040069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stuckler D., Basu S., Suhrcke M., Coutts A., McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. 2009;374(9686):315–323. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- 31.Wilcox H.C., Conner K.R., Caine E.D. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76 Suppl:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 32.Milner A., McClure R., De Leo D. Socio-economic determinants of suicide: an ecological analysis of 35 countries. Soc Psychiatry Psychiatr Epidemiol. 2012;47(1):19–27. doi: 10.1007/s00127-010-0316-x. [DOI] [PubMed] [Google Scholar]
- 33.Minoiu C., Rodriguez Andres A. The effect of public spending on suicide: evidence from U.S. state data. J Soc Econ. 2008;37:237–261. [Google Scholar]
- 34.Steelesmith D.L., Fontanella C.A., Campo J.V., Bridge J.A., Warren K.L., Root E.D. Contextual factors associated with county-level suicide rates in the United States, 1999 to 2016. JAMA Netw Open. 2019;2(9) doi: 10.1001/jamanetworkopen.2019.10936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miranda-Mendizabal A., Castellví P., Parés-Badell O., et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health. 2019;64(2):265–283. doi: 10.1007/s00038-018-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qin P., Agerbo E., Westergård-Nielsen N., Eriksson T., Mortensen P.B. Gender differences in risk factors for suicide in Denmark. Br J Psychiatry. 2000;177(6):546–550. doi: 10.1192/bjp.177.6.546. [DOI] [PubMed] [Google Scholar]
- 37.Schrijvers D.L., Bollen J., Sabbe B.G. The gender paradox in suicidal behavior and its impact on the suicidal process. J Affect Disord. 2012;138(1-2):19–26. doi: 10.1016/j.jad.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 38.Galdas P.M., Cheater F., Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005;49(6):616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 39.Kanny D., Naimi T.S., Liu Y., Lu H., Brewer R.D. Annual total binge drinks consumed by U.S. adults, 2015. Am J Prev Med. 2018;54(4):486–496. doi: 10.1016/j.amepre.2017.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.