Abstract
Background
Pregnant women form a specially vulnerable group due to unique changes in pregnancy, leading to a higher risk of getting a severe infection. As severe COVID-19 increases the risk of preeclampsia, preterm delivery, gestational diabetes, and low birth weight in pregnancy, there is a need to enhance pregnant women’s knowledge, attitudes, and practices to prevent these complications. This systematic review and meta-analysis aimed to determine their levels of knowledge, attitudes, and practice (KAP) regarding COVID-19 at the global level.
Methods
The systematic literature search was conducted in the English language, including Google Scholar, Scopus, PubMed/MEDLINE, Science Direct, Web of Science, EMBASE, Springer, and ProQuest, from the occurrence of the pandemic until September 2022. We used The Newcastle Ottawa scale for cross-sectional studies checklist to evaluate the risk of bias in the studies. Data were extracted by a Microsoft Excel spreadsheet and analyzed by STATA software version 14. We also employed Cochran Q statistics to assess the heterogeneity of studies and utilized Inverse variance random-effects models to estimate the pooled level of pregnant women’s KAP towards COVID-19 infection prevention.
Results
Based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) and inclusion criteria, 53 qualified studies were acquired from several countries. In total, 51 articles (17,319 participants) for knowledge, 15 articles (6,509 participants) for attitudes, and 24 articles (11,032 participants) for practice were included in this meta-analysis. The pooled good knowledge, positive attitude, and appropriate practice in pregnant women were estimated at 59%(95%CI: 52–66%), 57%(95%CI: 42–72%), and 53%(95%CI: 41–65%), respectively. According to subgroup analysis, the level of knowledge, attitude, and practice were 61%(95%CI: 49–72), 52%(95%CI: 30–74), and 50%(95%CI: 39–60), respectively, in Africa, and 58.8%(95%CI: 49.2–68.4), 60%(95%CI: 41–80) and 60% (95%CI: 41–78), respectively, in Asia.
Conclusion
The Knowledge, attitude, and practice towards COVID-19 infection prevention in pregnant women were low. It is suggested that health education programs and empowerment of communities, especially pregnant women, about COVID-19 continue with better planning. For future studies, we propose to investigate the KAP of COVID-19 in pregnant women in countries of other continents and geographical regions.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-023-05560-2.
Keywords: COVID-19, Knowledge, Attitudes, Practice, Pregnant
Background
The WHO declared the pandemic caused by COVID-19 as a public health emergency of international concern in January 2020 [1]. As of 02 October 2022, it has resulted in 623,268,353 confirmed cases of COVID-19 and 6,549,980 deaths globally [2]. Over time, new aspects of the effect of this virus on different body organs were identified and reported. Studies showed its impact on the digestive system, nervous system, skin, smell, cardiovascular system, liver, kidney, and eyes [3–6]. In addition to physical symptoms, the psychological burden of COVID-19 patients was heavy and persistent. So, the ongoing psychological trauma of the survivors of COVID-19 was highlighted in health care [7]. As of March 2021, there were 80 reported maternal deaths due to COVID-19 in the United States, and as of October 6, 2021, 1,637 COVID-19 infections and 15 deaths were reported in Mississippi [8].
On the other hand, pregnant women are more vulnerable, especially in the case of emerging infections, due to physiological and immunological changes [9, 10]. They are at risk of contracting the disease because of the weakness of the immune system and being in general society [11]. Changes caused by disasters and crises harm women's health [12]. Moreover, the level of anxiety and stress during the COVID-19 pandemic is high, so women are worried about their babies getting infected and seeking prenatal care [13, 14]. The most common complications in pregnancy include acute respiratory distress, disseminated intravascular coagulation, renal failure, bacterial infection, sepsis, need for mechanical ventilation, fetal death, and preterm delivery [15, 16]. The type of delivery in affected pregnant women depends on the conditions of the fetus, mother, and cervix. Thus, infection with COVID-19 alone does not determine the type of delivery [17]. Furthermore, COVID-19 can also affect children and cause systemic disease with several internal organ involvements [18].
In a systematic review study, Turan et al. showed that increasing age, obesity, diabetes, D-dimer levels, and interleukin-6 were effective in predicting pregnancy outcomes at the time of COVID-19, leading to a rise in premature birth and cesarean section. Also, vertical transmission may be possible, although it has not been proven [19]. In another study, Simsek et al. reported that COVID-19 has a harmful effect on pregnancy [20]. The association of severe COVID-19 during pregnancy with preeclampsia, premature birth, gestational diabetes, and low birth weight was reported [21].
Considering the vulnerability of pregnant women, the availability of fully effective vaccines in preventing infection, and the lack of definitive treatment, it is suggested that prevention is possible by increasing the knowledge of society to apply the correct health principles and physical distance to prevent its prevalence. According to a study in Ethiopia, maternal age, educational levels, husband educational levels, underlying disease, and sociocultural and demographic features had an influence on the KAP of COVID-19 in pregnant women [22]. Although there are numerous studies about the KAP of pregnant women in the prevention of COVID-19, their findings are not consistent with each other in some cases. Therefore, an overall understanding of KAP on the prevention behaviors of COVID-19 in pregnant women is essential for health system policymakers and stakeholders to design prevention programs. As a result, this study aims to determine the level of knowledge, attitudes, and preventive actions of pregnant women regarding COVID-19 at the global level.
Methods
This study was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [23, 24]. In addition, its executive protocol was registered in the international prospective register of systematic reviews (PROSPERO) with code [CRD42022351552],(https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=351552).
Search strategy
We searched all articles published in the English language, including Google Scholar, Scopus, PubMed/MEDLINE, Science Direct, Web of Science, EMBASE, Springer, and ProQuest, from the occurrence of the pandemic until September 2022.
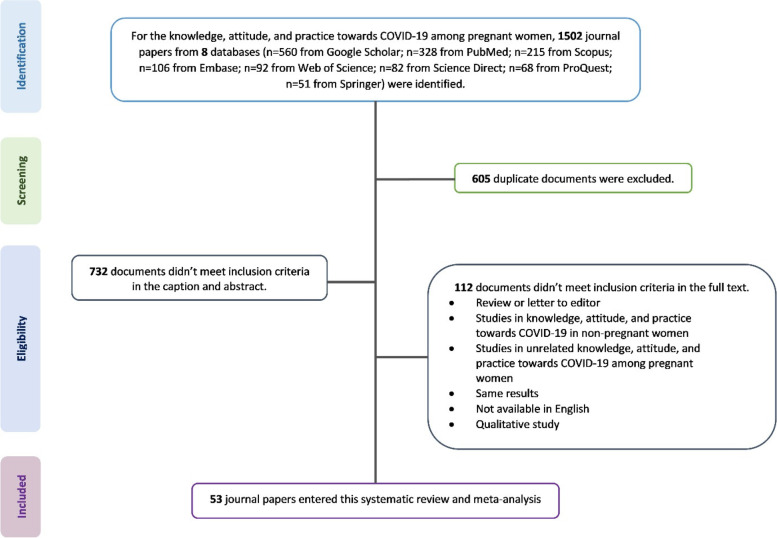
The search method was performed using MeSH terms in combination or separately using “AND” and “OR” functions (supplementary Table 1). The references of the found articles were also examined to increase the sensitivity. The processes of searching and selecting related articles are shown in the PRISMA flowchart (Fig. 1).
Fig. 1.
PRISMA flowchart presenting the selection of articles analyzed in this systematic review and meta-analysis
Eligibility criteria
Databases were searched based on the mentioned strategy. Then, the collected articles were carefully reviewed in terms of the desired epidemiological parameters and the inclusion criteria:
All Cross-sectional studies that reported data on COVID-19 knowledge and attitudes and practices, as well as studies on KAP in COVID-19 in pregnant women.
All articles published in the English language from the occurrence of the pandemic until September 2022.
All articles whose full text was accessible.
Articles in which the subjects were selected based on random sampling or census.
Exclusion criteria.
Articles whose population was other than pregnant women (such as the general population, health care workers, and students).
Articles published in languages other than English.
Studies except for observational studies, such as reviews, case series, and short communication.
Quality assessment (Risk of bias)
In this study, we used the modified Newcastle Ottawa scale for cross-sectional studies checklist to evaluate the risk of bias (internal validity) of the studies. The Newcastle–Ottawa Scale (NOS) is an ongoing collaboration between the Australian universities of Newcastle and Ottawa, Canada. This scale has been developed to evaluate the quality of non-randomized studies with its design, content, and ease of use to combine quality assessments in the interpretation of meta-analytic results. In this scale, studies are evaluated and graded based on three points of view, each of which includes subsections: a) Selection of study groups (including representativeness of the sample, sample size, ascertainment of exposure, and non-respondents), b) Ability to compare groups (the subjects in different outcome groups are comparable, based on the study design or analysis, and confounding factors), and c) determining the exposure or outcome of interest (assessment of the outcome and statistical test). The goal of the Newcastle–Ottawa Scale (NOS) is to develop a simple and convenient tool to assess the quality of non-randomized studies used in a systematic review.
The title of the journal and the names of the authors is apparent for the reviewers to measure the quality assessment of included studies. First, the full text of the article was read carefully by the first referee, and then the quality assessment checklist was completed and scored. The same steps were done independently by the second referee. Disagreements were discussed in a group discussion session. The range of scores is 0–10, calculated based on the checklist for each study. So, we determine the risk of bias for articles divided into three categories with low risk (8–10), medium risk (5–7), and high risk (0–5) [25].
Data extraction
At first, all selected articles were entered into EndNote X8 software (Thomson Reuters, New York, USA), and duplicate articles were removed. Then, two team members (MJ and VR) reviewed the selected titles and abstracts and excluded irrelevant articles from the study.
We tried to select articles related to the research topic and compatible with descriptive and cross-sectional studies based on working methods. After choosing the appropriate ones according to the study objectives, the final selection was made through group discussion. Then, the articles were entered into the next processes for qualitative evaluation and information extraction.
The data from the articles include the name of the author(s), year of study, type of study, sample size, geographical region of the study, and a good level of knowledge, good attitude, and appropriate practice towards COVID-19, which were extracted.
In this study, the knowledge, attitude, and practice about Covid-19 were as follows:
Knowledge
Containing disease symptoms, route of transmission, incubation period and isolation period, and ways to prevent COVID-19 were used to assess knowledge. A good level of knowledge means an above-average score.
Attitude
It included the individual's agreement or desire to participate in the fight against the epidemic of COVID-19, as well as the trust in the government and her companions in winning the battle against the COVID-19 pandemic. A score above the average level is recognized as a good attitude in the control and management of COVID-19.
Practice
It was defined as preventing infection and implementing prevention recommendations, such as maintaining physical distance, hand hygiene, wearing a mask, avoiding crowded places or social events, and isolation and quarantine to prevent the spread of COVID-19. Those whose score is average or higher are considered to be appropriate practices.
Statistical analysis
In this meta-analysis study, we performed statistical analyzes employing the STATA software (version 14.). We also used Inverse variance and Cochran Q statistics to evaluate the heterogeneity of studies. Low, medium, or high heterogeneity was considered as I2 test statistics. Values < 50%, 50%-80%, and > 80% were defined as low, moderate, and high heterogeneity, respectively [26]. Due to heterogeneity, the Dersimonian and Liard random-effects models were used in the current paper [27].
To evaluate the source of heterogeneity, univariate and multivariable meta-regression methods were used, as well as subgroup analysis [24]. In the analysis of the subgroups, the level of appropriate knowledge, positive attitude, and appropriate practice regarding preventive behaviors toward COVID-19 were estimated based on geographical areas.
We used the Funnel plots and Egger's regression test to check the existence of publication bias. On a condition of confirmation of publication bias, the trim-and-fill method was used to estimate the number of censored studies and correct the final estimate [28].
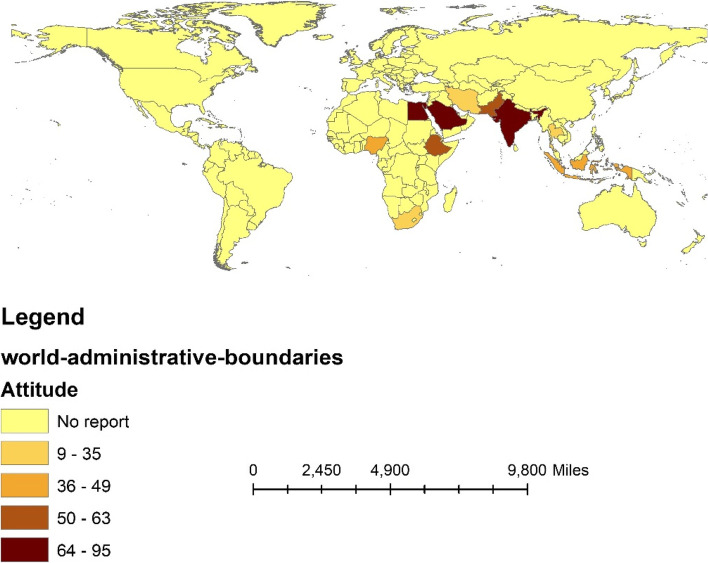
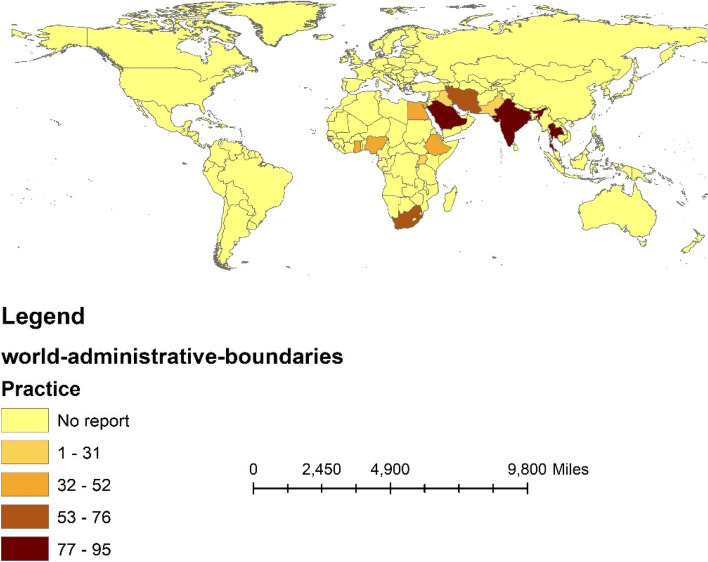
In addition, we used Arc GIS 10.3 software to visualize the geographic distribution of appropriate knowledge, positive attitudes, and appropriate practice according to continents and countries.
Results
Search results and eligibility studies
A total of 1,502 articles were reviewed by searching the seven mentioned databases based on the inclusion criteria. In the next step, 605 articles were excluded due to duplicates and 732 articles due to a lack of inclusion criteria in the abstract and title. Furthermore, 112 studies were excluded based on the exclusion criteria, such as the type of study, non-pregnant target group, and lack of access to the full text of the article. Finally, 53 studies, including 52 studies for knowledge [29–80], 15 studies for attitude [32, 36, 46–48, 50, 51, 55, 57, 66, 71, 73, 74, 77, 79], and 24 studies for practice [32, 40, 46, 48, 50, 52, 55, 57, 58, 62, 64, 65, 67–69, 71, 73–79, 81] were included in this systematic review and meta-analysis (Fig. 1).
Characteristics of the eligible studies
Total eligible studies include 53 journal articles. In terms of evaluating the quality assessment of included studies, 44 studies with low risk of bias and nine studies with moderate risk of bias were scored based on the NOS quality scale, and no one was included in the high risk of bias category (Table 1). Based on the continent, 30 studies were conducted in Asia, 21 in Africa, and one in North America (Tables 1 and 2). In terms of the type of study, all studies were conducted in a cross-sectional design (Table 1).
Table 1.
The article met the eligibility criteria of this systematic review and meta-analysis
| Authors Name | Year | Country | Total number | Study type | Good knowledge % | Good Attitude % |
Appropriate practice% |
QA |
|---|---|---|---|---|---|---|---|---|
| Ahlers-Schmidt, C.R [29] | 2020 | USA | 114 | CS | 35.9 | NA | NA | 9 |
| Kiftia, M [30] | 2022 | Indonesia | 138 | CS | 65.9 | NA | NA | 8 |
| Lee, TY [31] | 2020 | China | 161 | CS | 77.5 | NA | NA | 8 |
| Sukontrakoon, S [32] | 2022 | Thailand | 283 | CS | 75.62 | 8.48 | 88.34 | 8 |
| Septiasari, RT [33] | 2021 | Indonesia | 53 | CS | 24.5 | NA | NA | 4 |
| Tindaon, RL [34] | 2022 | Indonesia | 39 | CS | 97.4 | NA | NA | 4 |
| Novelia, S [35] | 2021 | Indonesia | 112 | CS | 58 | NA | NA | 5 |
| Oktaviani, M [36] | 2022 | Indonesia | 100 | CS | 55 | 57 | NA | 6 |
| Rahmawati, VE [37] | 2021 | Indonesia | 72 | CS | 87.5 | NA | NA | 5 |
| Sajid, A [38] | 2020 | Pakistan | 600 | CS | 85.69 | NA | NA | 9 |
| Sultana, R [39] | 2021 | Pakistan | 400 | CS | 33.3 | NA | NA | 8 |
| Abdulla, TN [40] | 2021 | Iraq | 400 | CS | 72 | NA | 32.75 | 9 |
| Hakiki, M [41] | 2022 | Indonesia | 35 | CS | 11 | NA | NA | 4 |
| Tamtiana, NK [42] | 2021 | Indonesia | 110 | CS | 49.1 | NA | NA | 5 |
| Aghababae, S [43] | 2020 | Iran | 225 | CS | 93.8 | NA | NA | 6 |
| Indumathi, P [44] | 2022 | India | 325 | CS | 50.5 | NA | NA | 7 |
| El Taha, L [45] | 2021 | Lebanon | 163 | CS | 81.5 | NA | NA | 5 |
| Izhar, R [46] | 2021 | Pakistan | 376 | CS | 39.4 | 62.8 | 30.9 | 8 |
| Kundaryanti, R [47] | 2021 | Indonesia | 73 | CS | 54.8 | 41.1 | NA | 5 |
| Alsafi, R [48] | 2022 | Saudi Arabia | 1574 | CS | 48.5 | 77.4 | 94.7 | 9 |
| Jhirwal, M( 49) | 2022 | India | 109 | CS | 94.4 | NA | NA | 7 |
| Deep Kamal [50], SC | 2022 | India | 506 | CS | 75.3 | 73.9 | 92.7 | 8 |
| MM, K [51] | 2021 | India | 505 | CS | 97.2 | 92.7 | NA | 8 |
| Kaream, AK [52] | 2021 | Iraq | 150 | CS | 28.7 | NA | 28 | 6 |
| Rahayuningsih, FB [53] | 2021 | Indonesia | 40 | CS | 15 | NA | NA | 4 |
| Bahrum,SW [54] | 2021 | Indonesia | 30 | CS | 46.7 | NA | NA | 4 |
| Hamzehgardeshi, Z [55] | 2021 | Iran | 318 | CS | 46.9 | 34.9 | 66.7 | 6 |
| Maharlouei, N [56] | 2020 | Iran | 540 | CS | 44.8 | NA | NA | 8 |
| Ali, HA [57] | 2022 | Egypt | 415 | CS | 75.4 | 95 | 43.6 | 8 |
| Temesgan, WZ [58] | 2022 | Ethiopia | 678 | CS | 62.2 | NA | 44.8 | 9 |
| Aboma, D [59] | 2021 | Ethiopia | 232 | CS | 63 | NA | NA | 8 |
| Elhameed E, [60] | 2022 | Egypt | 290 | CS | 15 | NA | NA | 7 |
| Abdus-Salam, RA [61] | 2021 | Nigeria | 380 | CS | 15 | NA | NA | 9 |
| Burodo A [62] | 2022 | Nigeria | 394 | CS | 98.7 | NA | 19.1 | 9 |
| Metwally, HM [63] | 2020 | Egypt | 370 | CS | 57.6 | NA | NA | 7 |
| Omozuwa [64] | 2021 | Nigeria | 420 | CS | 46.9 | NA | 77.1 | 8 |
| Ayele, A [65] | 2020 | Ethiopia | 405 | CS | 46.8 | NA | 47.6 | 8 |
| Degu [66] | 2021 | Ethiopia | 403 | CS | 52.1 | 52.6 | NA | 8 |
| Kassie BA, [67] | 2021 | Ethiopia | 422 | CS | 55 | NA | 47.4 | 9 |
| Kumbeni, M [68] | 2021 | Ghana | 527 | CS | 85.6 | NA | 46.6 | 9 |
| Fikadu, Y [69] | 2021 | Ethiopia | 403 | CS | 54.8 | NA | 76.2 | 8 |
| Adegoke, J [70] | 2020 | Nigeria | 382 | CS | 86.65 | NA | NA | 8 |
| Aduloju, O [71] | 2021 | Nigeria | 423 | CS | 87.2 | 74.5 | 79.2 | 8 |
| Omoronyia, E [72] | 2021 | Nigeria | 284 | CS | 43.3 | NA | NA | 7 |
| West, B [73] | 2021 | Nigeria | 253 | CS | 81.4 | 20.2 | 26.5 | 7 |
| Hoque, A [74] | 2021 | South Africa | 346 | CS | 43.5 | 30 | 76 | 8 |
| Theuring, S [75] | 2021 | Uganda | 648 | CS | 32.8 | NA | 21.4 | 8 |
| Besho, M [76] | 2021 | Ethiopia | 415 | CS | 75.4 | NA | 43.6 | 8 |
| Silesh, M [22] | 2021 | Ethiopia | 396 | CS | 70.5 | 87.6 | 56.1 | 8 |
| Nwafor, J [78] | 2020 | Nigeria | 284 | CS | 60.9 | NA | 30.3 | 7 |
| Zeleke, A [79] | 2022 | Ethiopia | 538 | CS | 67.3 | 46.7 | 51.1 | 9 |
| Anikwe [80] | 2021 | Nigeria | 460 | CS | 43.5 | NA | NA | 8 |
| Belayneh, M [81] | 2021 | Ethiopia | 458 | CS | NA | 53 | 8 |
CS Cross-Sectional, QA Quality assessment, NA Not applicable
Table 2.
The results of subgroup analysis based on country and continent for knowledge, attitude, and practice for COVID-19 in pregnant women
| type | grouping | No. studies | Sample size | Overall frequency (95%CI) |
Heterogeneity | |||
|---|---|---|---|---|---|---|---|---|
| χ2 | P-value | I2 (%) | ||||||
| Knowledge | Continent | Africa | 21 | 9353 | 61(49–72) | 4479.4 | < 0.001 | 99.6% |
| Asia | 30 | 7852 | 58.8(49.2–68.4) | 4036.7 | < 0.001 | 99.3% | ||
| North America | 1 | 114 | 36(27–45) | NA | NA | NA | ||
| Country | China | 1 | 161 | 77.5(71–84) | NA | NA | NA | |
| Egypt | 3 | 2520 | 49.3(12–86.6) | 429.6 | < 0.001 | 99.5% | ||
| Ethiopia | 9 | 4177 | 60.8(54.7–67) | 131.0 | < 0.001 | 93.9% | ||
| Ghana | 1 | 527 | 85.6(82.6–88.6) | NA | NA | NA | ||
| India | 4 | 1445 | 79.5(61.2–97.7) | 351.1 | < 0.001 | 99.1% | ||
| Indonesia | 11 | 802 | 51.6(33.3–69.8) | 449.2 | < 0.001 | 97.8% | ||
| Iran | 3 | 1083 | 61.9(26.7–97) | 425.1 | < 0.001 | 99.5% | ||
| Iraq | 2 | 550 | 50.4(8–92.2) | 100.3 | < 0.001 | 99.0% | ||
| Lebanon | 1 | 163 | 81.5(75.5–87.5) | NA | NA | NA | ||
| Nigeria | 9 | 5605 | 62.6(41.6–83.7) | 2879.2 | < 0.001 | 99.7% | ||
| Pakistan | 3 | 1376 | 52.8(16.1–89.6) | 493.4 | < 0.001 | 99.6% | ||
| Saudi Arabia | 1 | 1574 | 48.5(46–51) | NA | NA | NA | ||
| South Africa | 1 | 346 | 43.5(38–48.7) | NA | NA | NA | ||
| Thailand | 1 | 283 | 75.6(70.6–80.6) | NA | NA | NA | ||
| Uganda | 1 | 648 | 32.8(29.2–36.4) | NA | NA | NA | ||
| USA | 1 | 114 | 35.9(27.1–44.7) | NA | NA | NA | ||
| Attitude | Continent | Africa | 6 | 2359 | 52(30–74) | 765.4 | < 0.001 | 99.3% |
| Asia | 9 | 4150 | 60(41–80) | 2498.9 | < 0.001 | 99.7% | ||
| Country | Thailand | 1 | 283 | 8.5(5.2–11.7) | NA | NA | NA | |
| Indonesia | 2 | 173 | 49.3(33.7–64.9) | 4.38 | 0.036 | 77.2% | ||
| Pakistan | 1 | 376 | 62.8(58.9–67.8) | NA | NA | NA | ||
| Saudi Arabia | 1 | 1574 | 77.4(75.3–79.5) | NA | NA | NA | ||
| India | 2 | 1011 | 83.4(64.9–98.01) | 68.6 | < 0.001 | 98.5% | ||
| Iran | 1 | 318 | 34.9(29.7–40.1) | NA | NA | NA | ||
| Egypt | 1 | 415 | 95(92.9–97.1) | NA | NA | NA | ||
| Ethiopia | 3 | 1337 | 62.3(34.7–89.9) | 276.4 | < 0.001 | 99.3% | ||
| Nigeria | 2 | 676 | 47.4(5.08–99.01) | 271.4 | < 0.001 | 99.6% | ||
| South Africa | 1 | 346 | 30(25.2–34.8) | NA | NA | NA | ||
| Practice | Continent | Africa | 16 | 7010 | 50(39–60) | 1382.2 | < 0.001 | 98.9% |
| Asia | 8 | 4022 | 60(41–78) | 1928.9 | < 0.001 | 99.6% | ||
| Country | Thailand | 1 | 283 | 88.3(84.6–92.1) | NA | NA | NA | |
| Iraq | 2 | 550 | 31.2(26.9–35.6) | 1.2 | 0.275 | 16.0% | ||
| Pakistan | 1 | 376 | 30.9(26.2–35.6) | NA | NA | NA | ||
| Iran | 1 | 318 | 66.7(61.5–71.9) | NA | NA | NA | ||
| Egypt | 1 | 415 | 43.6(38.8–48.4) | NA | NA | NA | ||
| Ethiopia | 8 | 3715 | 52.5(44.8–60.1) | 165.2 | < 0.001 | 95.8% | ||
| Nigeria | 5 | 1774 | 46.5(19.3–73.6) | 760.9 | < 0.001 | 99.5% | ||
| Ghana | 1 | 527 | 46.6(42.3–50.9) | NA | NA | NA | ||
| South Africa | 1 | 346 | 76(71.5–80.5) | NA | NA | NA | ||
| Uganda | 1 | 648 | 21.4(18.2–24.6) | NA | NA | NA | ||
| India | 1 | 506 | 92.7(90.4–95) | NA | NA | NA | ||
| Saudi Arabia | 1 | 1574 | 94.7(93.6–95.8) | NA | NA | NA | ||
NA Not applicable
Pooled good knowledge about COVID-19
A total of 17,319 pregnant women were examined to estimate the level of good knowledge of COVID-19, which included 30 studies in Asia (7852 people), 21 studies in Africa (9353 people), and one study in America (114 people).
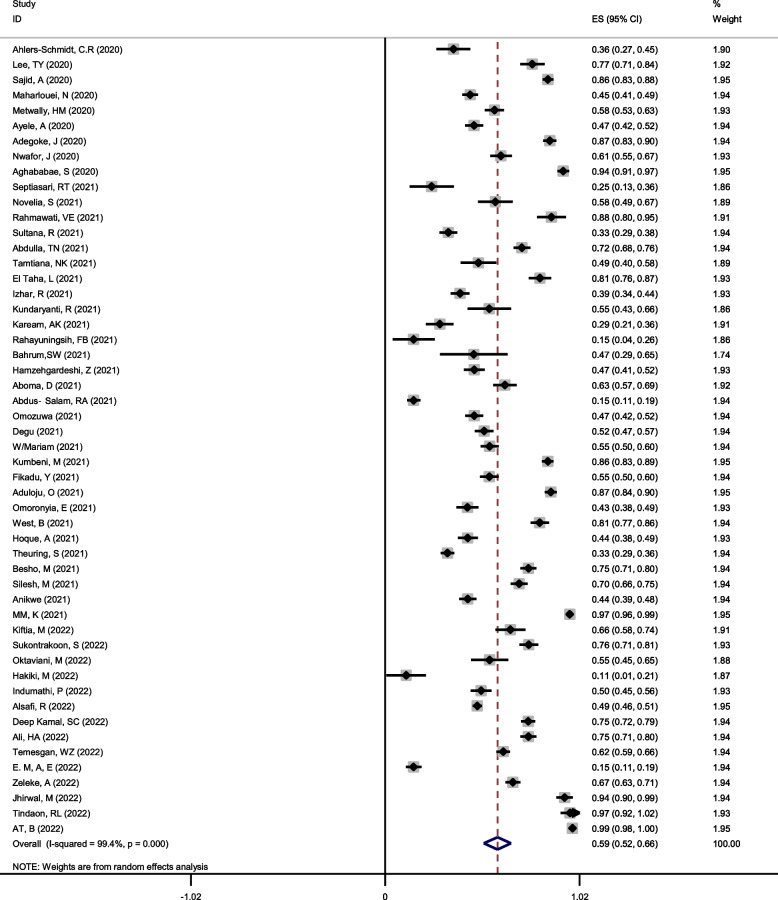
The overall good knowledge among pregnant women, using the random effect model with Mantel-Hanenszel heterogeneity, was estimated at 59% (95%CI: 52–66%) (Q statistic = 8632.71, d.f. = 51, p < 0.0001, I2 = 99.4%), as shown in Fig. 2.
Fig. 2.
Forest plot of Mantel –Hanenszel random effect meta-analysis for good knowledge of COVID-19 among pregnant women
Since the heterogeneity between studies was high, univariate and multivariable meta-regression methods were employed to investigate the cause and source of heterogeneity. In this regard, univariate meta-regression indicated that the country with a coefficient of 0.02281 might be its cause, which means that the percentage of good knowledge for COVID-19 can increase by 0.02281 with the change of the country, as demonstrated in Table 3.
Table 3.
Univariate and multivariable meta-regression to find possible causes of heterogeneity between studies included in the meta-analysis
| Type | Possible cause of heterogeneity | Univariate | Multivariable | ||
|---|---|---|---|---|---|
| Coefficient (95%CI) | P-value | Coefficient (95%CI) | P-value | ||
| Knowledge | Continent | -0.040(-0.162, 0.082) | 0.510 | -0.124(-0.283, 0.034) | 0.123 |
| Country | 0.022(0.016, 0.061) | 0.041 | 0.010(-0.013, 0.0341) | 0.123 | |
| Risk of bias | -.075(-0.243, 0.092) | 0.372 | -0.086(-0.317, 0.143) | 0.453 | |
| Year | 0.003(-0.096,0.103) | 0.942 | -0.007(-0.112, 0.097) | 0.885 | |
| Sample size | 0.0005(-0.0002, 0.0003) | 0.710 | -0.0001(-0.0004, 0.0002) | 0.497 | |
| Attitude | Continent | -0.085(-0.397, 0.226) | 0.565 | -0.410(-1.04, 0.225) | 0.178 |
| Country | 0.008(-0.046, 0.063) | 0.748 | 0.052(-0.056, 0.160) | 0.306 | |
| Risk of bias | 0.079(-0.056, 0.215) | 0.229 | 0.082(-0.155, 0.319) | 0.453 | |
| Year | 0.045(-0.270, 0.360) | 0.762 | -0.077(-0.493, 0.338) | 0.685 | |
| Sample size | 0.0002(-0.0001, 0.0007) | 0.167 | 0.00008(-0.0005, 0.0007) | 0.776 | |
| Practice | Continent | -0.100(-0.309, 0.107) | 0.325 | -0.129(-0.592, 0.333) | 0.563 |
| Country | -0.011(-0.049, 0.026) | 0.541 | 0.007(-0.075,0.089) | 0.859 | |
| Risk of bias | -0.072(-0.437, 0.292) | 0.683 | -0.06113(-0.535, 0.413) | 0.789 | |
| Year | 0.114(-0.051, 0.281) | 0.167 | 0.05616(-0.173, 0.285) | 0.614 | |
| Sample size | 0.0003(-0.00005, 0.0006) | 0.091 | 0.0002(-0.0002, 0.0006) | 0.296 | |
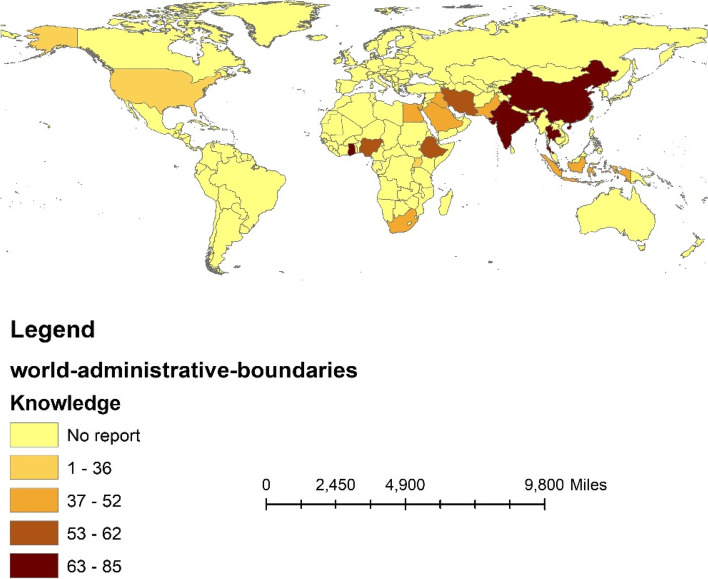
Based on the results of the subgroup analysis, the level of good knowledge about COVID-19 in pregnant women in Africa and Asia was estimated to be 61% (95%CI: 49–72) and 58.8% (95%CI: 49.2–68.4) (between-group p-value = 0.024), respectively. In regard to country, this level of knowledge was reported in Uganda at 32.8% (95%CI: 29.2–36.4) and Ghana at 85.6% (95%CI: 82.6–88.6) (between-group p-value < 0.001), as displayed in Table 3 and Fig. 3.
Fig. 3.
The percentage of good knowledge of COVID-19 among pregnant women based on countries
Pooled good attitudes toward COVID-19
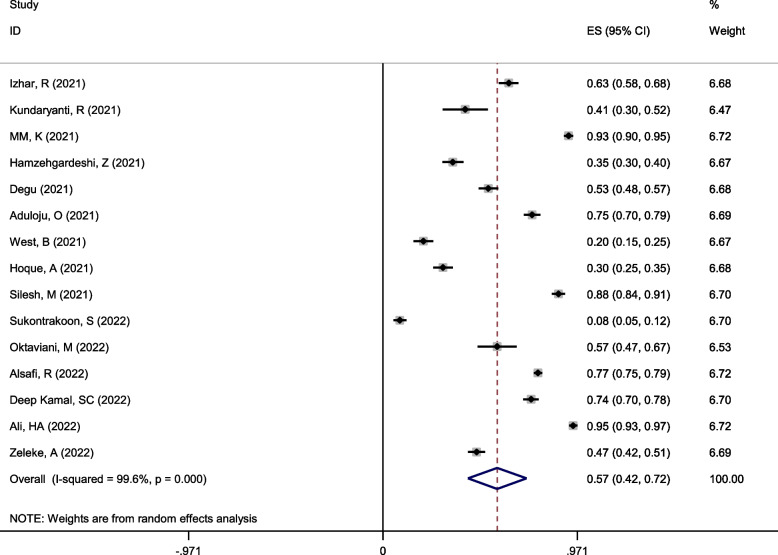
A total of 15 studies with 6509 people, including nine studies in Asia (4150 people) and six studies in Africa (2359 people), were included for attitude analysis.
Using the random effect model with Mantel-Hanenszel heterogeneity, the overall good attitude among pregnant women was estimated at 57% (95%CI: 42–72%) (Q statistic = 3512.77, d.f. = 14, p < 0.0001, I2 = 99.6% %), as depicted in Fig. 4.
Fig. 4.
Forest plot of Mantel –Hanenszel random effect meta-analysis for good attitude towards COVID-19 among pregnant women
The results of univariate and multivariable meta-regression analysis showed that none of the variables of the continent, country, quality of studies, year of study, and sample size were possible causes of heterogeneity (p > 0.05), as shown in Table 3.
Based on subgroup analysis, the level of positive attitude in Asia and Africa was estimated to be 60% (95%CI: 41–80) and 52%(95%CI: 30–74) (between-group p-value < 0.001), respectively, as demonstrated in Table 2 and Fig. 5.
Fig. 5.
The percentage of positive attitudes towards COVID-19 among pregnant women based on the continent
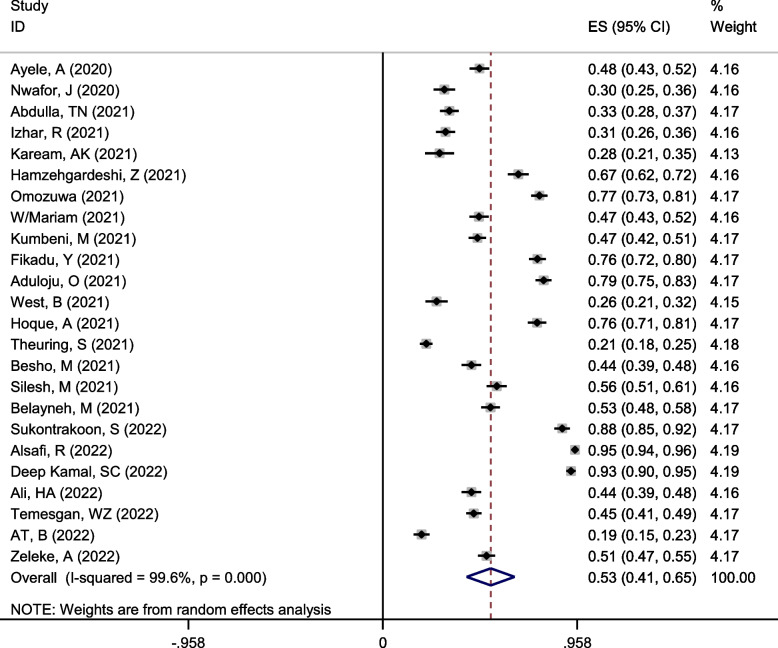
Pooled appropriate practice toward COVID-19
A total of 24 studies contained 11,032 pregnant women, including 16 studies in Africa (7010 people) and eight studies in Asia (4022 people).
Employing a random effect model with Mantel-Hanenszel heterogeneity, the pooled appropriate practice was estimated at 53% (95%CI: 41–65%) (Q statistic = 5968.39, d.f. = 23, p < 0.0001, I2 = 99.6% %), as presented in Fig. 6.
Fig. 6.
Forest plot of Mantel –Hanenszel random effect meta-analysis for appropriate practice towards COVID-19 among pregnant women
Univariate and multivariable meta-regression analysis was performed to find the source of heterogeneity. Table 3 shows that none of the variables of the continent, country, quality of studies, year of study, and sample size are possible causes of heterogeneity (p > 0.05).
Subgroup analysis showed that appropriate practice towards COVID-19 in pregnant women in Asia and Africa was estimated to be 60% (95%CI: 41–78) and 50%(95%CI: 39–60) (between-group p-value < 0.001), respectively (Table 3 and Fig. 7).
Fig. 7.
The percentage of appropriate practice towards COVID-19 among pregnant women based on the continent
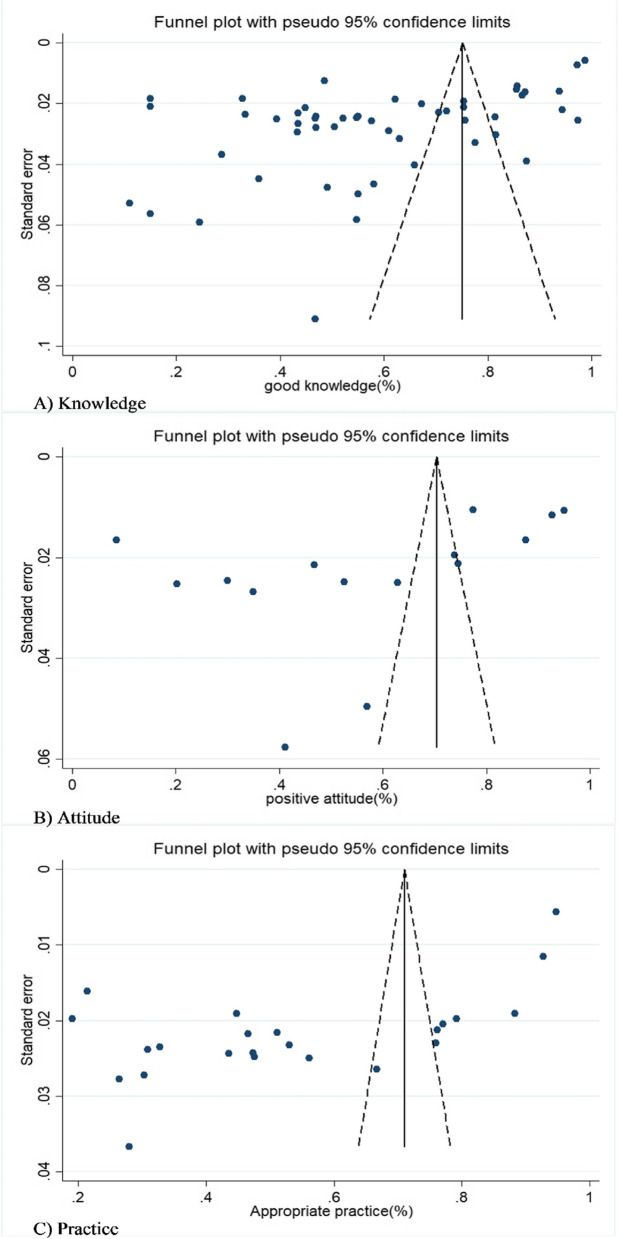
Publication bias
We employed Egger's regression test and funnel plots to check publication bias. On a condition of confirmation of publication bias, the trim-and-fill method was used to estimate the number of censored studies and finally to correct the overall estimate of the meta-analysis.
The funnel plots and Egger's test showed that there is a significant publication bias for the level of knowledge (bias = -15.8941, 95%CI: -21.322, -10.466, P < 0.001), as depicted in Fig. 8, A. Based on the results of trim- and -fill, two studies were censored. Thus, the approximation of the corrected good knowledge level was 58.5%(95%CI: 49.5–67.5%).
Fig. 8.
Funnel plot with pseudo 95% confidence limits for detection of publication bias among included studies
Egger's test was significant for good attitude (bias = -21.29213, 95%CI: -39.929, -2.654, P = 0.028). Also, Fig. 8, B displayed that the asymmetric distribution of studies in the funnel plot confirmed the publication bias. Based on the non-parametric method, the trim-and-fill test estimated three censored studies. Consequently, the corrected positive attitude was estimated as 55.6%(95%CI:38.9–72.3%).
For appropriate practice, the funnel plot was asymmetric, and Egger's test was significant (bias = -25.4246, 95%CI: -34.458, -16.39, P < 0.001), as shown in Fig. 8, C. Based on Trim-and-fill and non-parametric methods, the expected values of two censored studies were calculated, and the overall appropriate practice corrected by the random effects model in pregnant women was estimated to be 49.4% (95%CI: 33.5–65.3%).
Discussion
This comprehensive systematic review and meta-analysis study assessed the overall good knowledge, positive attitude, and appropriate practice towards COVID-19 in pregnant women. The study demonstrated that these parameters for COVID-19 infection prevention in pregnant women were low. According to the results, good knowledge was 59%, which was in line with the results of several studies [82–84]. However, this finding is significantly lower than that of research conducted on sub-Saharan Africans [85]. In a systematic review and meta-analysis, Mose et al. estimated that pooled knowledge of COVID-19 infection prevention among pregnant women in Ethiopia was 60.24% [86].
In the present paper, information about knowledge was extracted from 30 studies in Asia (7852 people), 21 studies in Africa (9353 people), and one study in America (114 people). At first glance, it seems that considering that the majority of the study population was conducted from developing countries. The current study's estimate of people's level of knowledge was lower than the real values of the global average, or at least these results cannot be generalized for developed countries.
While taking a closer look at the separate results of different articles, it is revealed that these results have shown the highest knowledge among pregnant women about COVID-19 in African countries (61%), followed by Asian countries (58.8%) and the lowest in the United States of America (35.9%) [29]. Interestingly, the highest knowledge was for an African country (Ghana 85.6%) [68], and the lowest one is for an African country as well (Uganda 32.8%) [75]. Also, Asian countries, such as India (79.5%) (53- 54- 55) and Lebanon (81.5%) [45], showed a high level of knowledge.
In addition, maternal age, educational levels, husband educational levels, underlying disease, and socio-cultural and demographic features were associated with KAP of COVID-19 in pregnant women [22]. Furthermore, a study conducted in China on pregnant women represented that a level of knowledge of COVID-19 prevention related to high education through the media, especially at the beginning of the epidemic, previous experiences of exposure to other coronavirus epidemics, and the local government-imposed strict restrictions on immediate infection control after the outbreak began [31].
The other results of this study demonstrated that the overall positive attitude among pregnant women toward COVID-19 was 57%, which was in line with the results of several studies [82, 83, 87]. A systematic review and meta-analysis estimated that the attitude towards COVID-19 infection prevention among pregnant women in Ethiopia was 62.46%% [86]. In this study, good knowledge of COVID-19 had a better status than a positive attitude. Generally, it is expected that people's knowledge is at a higher level than their attitude. Also, Asia (60%) had a better situation than Africa (52%). However, the highest values of a positive attitude were for Egypt (95%) [57], which has a better socioeconomic status and literacy level than other African countries.
The majority of the studies were online surveys, and literature support, age, and education level affected the behaviors of online surveys [88] since information sources, the Internet, and social networks played an important role in creating knowledge and attitude [89]. Furthermore, the difference in time in terms of the status of the epidemic curve during the study period, as well as the trust in the local government to manage the epidemic, especially the experience of controlling and managing previous epidemics, affected the attitude of the community [22].
Furthermore, our findings showed that the positive practice towards COVID-19 was 53%, which was in line with previous studies [83, 85, 87] and lower than a review conducted around the globe [90]. A systematic review and meta-analysis estimated that the practice among pregnant women in Ethiopia was 52.29% [86]. This study revealed that pregnant women who resided in urban areas were 2.23 times more likely to have good preventive practices for COVID-19 infection compared with those who resided in rural areas. One of the possible reasons may be that urban pregnant women have better access to basic healthcare services and media. They also can read texts related to Covid-19 from newspapers or social media. Moreover, findings showed that pregnant women with a secondary education level perform 3.36 times more preventive behaviors against Covid-19 compared to those with no formal education [86].
On the other hand, it should be mentioned that the present study focused on pregnant women, while the global study conducted worldwide included all people in society. The positive practice towards COVID-19 in pregnant women in the Asian continent was (60%) better compared to the African continent (50%), which seems logical. The level of positive practice of people was lower in knowledge and attitude. Achieving positive practice requires improving knowledge and attitude, yet their improvement does not lead to positive practice in all cases [91]. In a meta-analysis study, Mose et al. showed that pregnant women with good knowledge were 2.73 times more likely to have good preventive practices for COVID-19 than those with poor practice [86].
The level of risk perception of society to understand the risk of infection, cultural norms, such as shaking hands and participating in family, social and religious gatherings, continuity of water sources and easy washing of hands, access to the health care facility and living conditions may be effective in carrying out prevention behaviors for COVID-19 in communities [90, 92].
Furthermore, the harm caused by the pandemic may be different in the uninfected pregnant population. In this regard, Zheng et al., in a systematic review and qualitative meta-synthesis study, reported that the COVID‐19 pandemic disrupted the conceiving plan and the routine care of pregnant women. Since the availability and quality of maternal care have played a decisive role in maternal and fetal outcomes, it is suggested that the government or healthcare providers balance the restrictions and access to maternity care during future pandemics [93].
Strengths and limitations
One of the limitations of the current paper was the lack of studies regarding the KAP components of pregnant women in preventive behaviors against COVID-19, especially in developed countries, which to some extent limited the global estimate of the KAP rate for pregnant women leading to encountering the problem on the comparison of countries and continents. In addition, despite performing meta-regression analysis to find the source of heterogeneity and subgroup analysis to reduce its impact on the estimates, the heterogeneity rate between studies was still high. The reason for this is probably other variables, such as the difference in tools, questionnaires used to measure KAP components, and the difference in the studied societies in terms of basic demographic variables, such as age, literacy level, socioeconomic status, cultural difference, ethnicity, type of health system, and the different policies of the governing systems of the societies to deal with the COVID-19 pandemic in each region and country, which was not investigated in this study. The small sample size of many studies conducted in most countries, which probably cannot be generalized to the population of those countries, is worth considering. In addition, the publication bias among included studies was significant. Despite its correction with statistical methods and the estimation of the number of censored studies, it can still influence the estimates of this study.
However, considering the global estimation of the level of KAP components in pregnant women for COVID-19, we believe that in this study, all the available and accessible information and the appropriate statistical methods have been used for the most appropriate estimation of the KAP components at the global level. Also, by creating scientific evidence, its findings can be used in health policies and prevention programs, especially for possible future epidemics.
Conclusion
Our results showed that knowledge, attitude, and practice toward COVID-19 infection prevention in pregnant women were low. Considering that several years have passed since the beginning of this pandemic and taking into account the global effects of the disease in terms of health, social, economic, and political, it was expected that the knowledge, attitude, and practice of pregnant women, who are one of the high-risk groups regarding this disease, would be in a better condition. It is proposed that health education programs and empowerment of communities, especially pregnant women, about COVID-19 continue with better planning. For future studies, it is suggested to investigate the KAP of COVID-19 in pregnant women in countries of other continents and geographical regions.
Supplementary Information
Additional file 1: S1 Table. strategy search for the KAP towards COVID-19 among pregnant women.
Acknowledgements
Not applicable.
Abbreviations
- KAP
Knowledge, attitudes, and practice
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- WHO
World Health Organization
- PROSPERO
International prospective register of systematic reviews
- MeSH
Medical Subject Headings
- NOS
Newcastle–Ottawa Scale
- d.f
Degree of freedom
Authors’ contributions
ASJ and VR considered and planned the study. MJ and VR were responsible for the literature search and screening. MJ and BO were responsible for data collection. VR participated in the statistical analysis. MJ, NSH, and VR contributed to data interpretation. ASJ, VR, and NSH drafted the manuscript, and VR critically revised the manuscript. All authors read the final manuscript and approved it for publication, [VR] had full access to all of the data in this study and take complete responsibility for the integrity of the data and the accuracy of the data analysis.”
Funding
None.
Availability of data and materials
The authors acknowledge that data supporting the findings of this study are available in the article [and/or] its supplementary material.
Declarations
Ethics approval and consent to participate
In this study, we adhered to all ethical principles in the systematic review and meta-analysis studies. The Research Ethics Committee of Jahrom University of Medical Sciences approved the study protocol (ID IR.JUMS.REC.1401.057.).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abdolreza Sotoodeh Jahromi, Email: sotoodehj2002@yahoo.com.
Mohammad Jokar, Email: rakoj1375@gmail.com.
Nader Sharifi, Email: nadersharifi81@yahoo.com.
Vahid Rahmanian, Email: vahid.rahmani1392@gmail.com.
References
- 1.Rahmanian V, Rabiee MH, Sharifi H. Case fatality rate of coronavirus disease 2019 (COVID-19) in Iran-a term of caution. Asian Pac J Trop Med. 2020;13(7):328. doi: 10.4103/1995-7645.281617. [DOI] [Google Scholar]
- 2.WHO. Coronavirus (COVID-19) Dashboard 2022 [updated 2 October; cited 2022 3 October]. Available from: https://covid19.who.int/.
- 3.Annweiler C, Sacco G, Salles N, Aquino J-P, Gautier J, Berrut G, et al. National French Survey of Coronavirus Disease (COVID-19) symptoms in people aged 70 and over. Clin Infect Dis. 2021;72(3):490–494. doi: 10.1093/cid/ciaa792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma P, Uppal NN, Wanchoo R, Shah HH, Yang Y, Parikh R, et al. COVID-19–associated kidney injury: a case series of kidney biopsy findings. J Am Soc Nephrol. 2020;31(9):1948–1958. doi: 10.1681/ASN.2020050699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, et al. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1–6. doi: 10.1016/j.ejim.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 6.SeyedAlinaghi S, Karimi A, Barzegary A, Pashaei Z, Afsahi AM, Alilou S, et al. Mucormycosis infection in patients with COVID-19: A systematic review. Health Sci Rep. 2022;5(2):e529. doi: 10.1002/hsr2.529. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7.Zheng X, Qian M, Ye X, Zhang M, Zhan C, Li H, et al. Implications for long COVID: A systematic review and meta‐aggregation of experience of patients diagnosed with COVID‐19. J Clin Nurs. 2022. 10.1111/jocn.16537. [DOI] [PMC free article] [PubMed]
- 8.Kasehagen L, Byers P, Taylor K, Kittle T, Roberts C, Collier C, et al. COVID-19–associated deaths after SARS-CoV-2 infection during pregnancy—Mississippi, March 1, 2020–October 6, 2021. Morb Mortal Wkly Rep. 2021;70(47):1646. doi: 10.15585/mmwr.mm7047e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jahromi AS, Shojaei M, Ghobadifar MA. Insulin resistance and serum levels of interleukin-17 and interleukin-18 in normal pregnancy. Immune network. 2014;14(3):149–155. doi: 10.4110/in.2014.14.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415–426. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rahmani Bilandi R, Khalajabadi Farahamni F, Ahmadi F, Kazemnejad A, Mohammadi R. Exploring the perception of women about menstrual health in earthquake stricken areas. J Mazandaran Univ Med Sci. 2015;25(125):49–60. [Google Scholar]
- 13.Abedzadeh-Kalahroudi M, Karimian Z, Nasiri S, Khorshidifard MS. Anxiety and perceived stress of pregnant women towards Covid-19 disease and its related factors in Kashan (2020) Iranian J Obstet Gynecol Infertility. 2021;24(5):8–18. [Google Scholar]
- 14.Rasekh Jahromi A, Daroneh E, Jamali S, Ranjbar A, Rahmanian V. Impact of COVID-19 pandemic on depression and hopelessness in infertile women. J Psychosom Obstet Gynaecol. 2022;43(4):495–501. doi: 10.1080/0167482X.2022.2082279. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz DA, Graham AL. Potential maternal and infant outcomes from coronavirus 2019-nCoV (SARS-CoV-2) infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12(2):194. doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith LH, Dollinger CY, VanderWeele TJ, Wyszynski DF, Hernández-Díaz S. Timing and severity of COVID-19 during pregnancy and risk of preterm birth in the International Registry of Coronavirus Exposure in Pregnancy. BMC Pregnancy Childbirth. 2022;22(1):775. doi: 10.1186/s12884-022-05101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: What clinical recommendations to follow? 2020. [DOI] [PubMed]
- 18.Mehraeen E, Oliaei S, SeyedAlinaghi S, Karimi A, Mirzapour P, Afsahi AM, et al. COVID-19 in pediatrics: a systematic review of current knowledge and practice. Infect Disord Drug Targets. 2022;22(5):47–57. doi: 10.2174/1871526521666210929121705. [DOI] [PubMed] [Google Scholar]
- 19.Turan O, Hakim A, Dashraath P, Jeslyn WJL, Wright A, Abdul-Kadir R. Clinical characteristics, prognostic factors, and maternal and neonatal outcomes of SARS-CoV-2 infection among hospitalized pregnant women: a systematic review. Int J Gynecol Obstet. 2020;151(1):7–16. doi: 10.1002/ijgo.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simsek Y, Ciplak B, Songur S, Kara M, Karahocagil M. Maternal and fetal outcomes of COVID-19, SARS, and MERS: a narrative review on the current knowledge. Eur Rev Med Pharmacol Sci. 2020;24(18):9748–9752. doi: 10.26355/eurrev_202009_23068. [DOI] [PubMed] [Google Scholar]
- 21.Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193(16):E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silesh M, Demisse TL, Taye BT, Desta K, Kitaw TM, Mekuria AD, et al. Compliance with COVID-19 preventive measures and associated factors among women attending antenatal care at public health facilities of Debre Berhan Town, Ethiopia. Risk Manage Healthcare Policy. 2021;14:4561. doi: 10.2147/RMHP.S330932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jokar M, Bokaie S, Rahmanian V, Zahedi R, Sharifi N, Khoubfekr H. Neospora caninum infection in cattle and dogs in iran: A systematic review and meta-analysis. Am J Anim Vet Sci. 2021;16(1):23–38. doi: 10.3844/ajavsp.2021.23.38. [DOI] [Google Scholar]
- 24.Jokar M, Rahmanian V, Farhoodi M, Abdous A, Shams F, Karami N. Seroprevalence of bovine viral diarrhea virus (BVDV) infection in cattle population in Iran: a systematic review and meta-analysis. Trop Anim Health Prod. 2021;53(5):1–12. doi: 10.1007/s11250-021-02918-6. [DOI] [PubMed] [Google Scholar]
- 25.Jokar M, Shams F, Rahmanian V, Farhoodi M, Nadali B, Raziee Y. The global seroprevalence of Neospora caninum infection in deer: a systematic review and meta-analysis study. Small Ruminant Res. 2022;214:1–10. doi: 10.1016/j.smallrumres.2022.106745. [DOI] [Google Scholar]
- 26.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 27.Jokar M, Rabiee M, Bokaie S, Rahmanian V, Dehesh P, Hasannejad H, et al. Prevalence of cryptosporidiosis in animals in Iran: A systematic review and metaanalysis. Asian Pac J Trop Med. 2021;14(3):99–112. doi: 10.4103/1995-7645.307532. [DOI] [Google Scholar]
- 28.Rahmanian V, Rahmanian K, Sotoodeh-Jahromi A, Bokaie S. Systematic review and meta-analysis of human visceral leishmaniasis in Iran. Acta facultatis medicae Naissensis. 2019;36(4):279–293. doi: 10.5937/afmnai1904279R. [DOI] [Google Scholar]
- 29.Ahlers-Schmidt CR, Hervey AM, Neil T, Kuhlmann S, Kuhlmann Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Educ Couns. 2020;103(12):2578–2582. doi: 10.1016/j.pec.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kiftia M, Rizkia M, Ardhia D. The correlation among pregnant woman's education level with knowledge and behaviour on readiness toward COVID-19 pandemic. Enferm Clin. 2022;32:S35–S38. doi: 10.1016/j.enfcli.2022.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee T-Y, Zhong Y, Zhou J, He X, Kong R, Ji J. The outbreak of coronavirus disease in China: risk perceptions, knowledge, and information sources among prenatal and postnatal women. Women and Birth. 2021;34(3):212–218. doi: 10.1016/j.wombi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sukontrakoon P, Phumonsakul S, Prohm S, Sawatpanich A. Associations among Knowledge, Attitudes, Health Behaviors, and Stress of Pregnant Women in Thailand during the New Coronavirus-2019. Ramathibodi Nurs J. 2022;28(2):170–82.
- 33.Septiasari RM, Viandika N. The correlation between covid-19 knowledge and anxiety of pregnant women during covid-19 pandemic. anxiety. 2021;17:32.
- 34.Tindaon RL, Halawa M. The relationship of pregnant women's knowledge of COVID-19 prevention with ante natal care (ANC) visits. Eur J Clin Biomed Sci. 2022;8(2):23–26. doi: 10.11648/j.ejcbs.20220802.13. [DOI] [Google Scholar]
- 35.Novelia S, Lubis R, Apriyanti R. Determinant of Anxiety Levels among Pregnant Women during Covid-19 Pandemic. Asian Community Health Nurs Res. 2021;3(2):1–6.
- 36.Oktaviani M, Kundaryanti R, Novelia S. Factors Related to Prevention Behavior of COVID-19 Transmission among Pregnant Women. Nurs Health Sci J (NHSJ) 2022;2(1):24–28. doi: 10.53713/nhs.v2i2.67. [DOI] [Google Scholar]
- 37.Rahmawati VE, Prihartini SD, Annuchasari H, editors. The Level of Knowledge of Pregnant Women About COVID-19 Pandemic in Ngumpul District, Jogoroto, Jombang. Indonesia: The 3rd Joint International Conference; 2021.
- 38.Sajid A, Sajid A, Sajid A, Hanif A, Wazir A, Cheema S. Knowledge Attitude and Practices towards COVID-19 among Pregnant Patients Coming in Lady Aitchison Hospital, Lahore. Journal of The Society of Obstetricians and Gynaecologists of Pakistan. 2020;10(3):153–158. [Google Scholar]
- 39.Sultana R, Yasin I. Awareness about breastfeeding practices among pregnant and postnatal women during COVID-19 pandemic. Annals of PIMS-Shaheed Zulfiqar Ali Bhutto Medical University. 2021;17(1):12–16. [Google Scholar]
- 40.Abdulla TN, Akram W, MardanAbullah T. Knowledge and practice of pregnant Iraqi women about COVID-19 preventive measures. Medico Legal Update. 2021;21(1):1217–1223. [Google Scholar]
- 41.Hakiki M, Widiyastuti NE. Knowledge about Covid-19 and pregnant women’s anxiety during the pandemic. Jurnal Kebidanan Malahayati. 2021;8(1):173–179. [Google Scholar]
- 42.Tamtiana NK, Purnami N, Frety EE. Knowledge of pregnant women in the third trimester about congenital deafness and frequency of antenatal care during the covid-19 pandemic. Knowledge of pregnant women in the third trimester about congenital deafness and frequency of antenatal care during the COVID-19 pandemic. 2021;88(1):6.
- 43.Aghababaei S, Bashirian S, Soltanian A, Refaei M, Omidi T, Ghelichkhani S, et al. Perceived risk and protective behaviors regarding COVID-19 among Iranian pregnant women. Middle East Fertility Society Journal. 2020;25(1):1–9. doi: 10.1186/s43043-020-00038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Indumathi P, Swain D, Priyadarshini T, Jacob J, Tigga R. Knowledge, perceived threats and protective behaviour related to COVID 19 among pregnant women. Asian J Psychiatr. 2022;72:103091. doi: 10.1016/j.ajp.2022.103091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.El Taha L, Beyrouthy C, Tamim H, Ghazeeri G. Knowledge and attitudes among Lebanese pregnant women and women seeking fertility treatment during the COVID-19 outbreak: a cross-sectional survey. BMJ Open. 2022;12(3):e057873. doi: 10.1136/bmjopen-2021-057873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Izhar R, Husain S, Tahir MA, Husain S, Hussain S. Pregnant during the COVID-19 pandemic: Knowledge, concerns, attitudes and practices of Pakistani women. Eur J Midwifery. 2021;5(54):1–9. [DOI] [PMC free article] [PubMed]
- 47.Kundaryanti R, Karningsih K, Astri H, Syafrudin S. The relationship between knowledge and attitude towards the preventive behaviors for the Covid-19 transmission in pregnant mothers at “Rini K” independent midwifery practice (PMB), Jagakarsa, South Jakarta, 2021. STRADA Jurnal Ilmiah Kesehatan. 2021;10(2):1480–1486. doi: 10.30994/sjik.v10i2.851. [DOI] [Google Scholar]
- 48.Alsafi R, Farsi LZ, Alharbi A, Minshawi F, Alsafi H, Qashqari F, et al. Knowledge, Attitudes, and Practices among Pregnant Saudi Women during the COVID-19 Pandemic: A Cross-Sectional Analysis. Int J Pharmaceutical Res Allied Sci. 2022;11(2):100–09.
- 49.Jhirwal M, Singh P, Sharma C, Kathuria P, Shekhar S, Meena SP. Awareness and understanding of COVID-19 among pregnant woman in Northern India. J Educ Health Promotion. 2022;11(191):1–7. [DOI] [PMC free article] [PubMed]
- 50.Kamal D, Thakur VD, Swain SK, Vikneshram C. Knowledge, attitude, and practice toward COVID-19 among pregnant women in a tertiary care hospital during the COVID-19 outbreak. J Marine Med Soc. 2020;22(3):66. [Google Scholar]
- 51.Kalpana M, Sreenivas S, Santhosh S, Sabeena S. Knowledge, Attitude, and Practice regarding Health Effects of COVID-19 Pandemic and Preventive Measures including Vaccination among Pregnant Women from South India. 2021.
- 52.Kaream A, Ali R. Assessment of pregnant women’s knowledge and health behaviors concerning corona virus disease precaution measures at primary health care centers in Baghdad City-Iraq. Kufa J Nurs Sci. 2021;11(2):146–153. [Google Scholar]
- 53.Rahayuningsih FB, Fitriani N, Dewi E, Sudaryanto A, Sulastri S, Jihan AF. Knowledge about care of pregnant mothers during the Covid-19 pandemic. Open Access Macedonian J Med Sci. 2021;9(G):266–72. doi: 10.3889/oamjms.2021.6845. [DOI] [Google Scholar]
- 54.Bahrum SW, Rejeki IS, Fajri F, Nurnainah N, Atika R, Kayacilar C. Knowledge analysis of pregnant women on prevention the transmission COVID 19. International Journal of Health and Pharmaceutical (IJHP) 2021;1(1):1–4. doi: 10.51601/ijhp.v1i1.2. [DOI] [Google Scholar]
- 55.Hamzehgardeshi Z, Omidvar S, Amoli AA, Firouzbakht M. Pregnancy-related anxiety and its associated factors during COVID-19 pandemic in Iranian pregnant women: a web-based cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):1–9. doi: 10.1186/s12884-021-03694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maharlouei N, Asadi N, Bazrafshan K, Roozmeh S, Rezaianzadeh A, Zahed-Roozegar M-H, et al. Knowledge and attitude regarding COVID-19 among pregnant women in Southwestern Iran in the early period of its outbreak: a cross-sectional study. Am J Trop Med Hyg. 2020;103(6):2368. doi: 10.4269/ajtmh.20-0608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ali HA, Ramadan S, Ahmed NH. Knowledge, attitude, and practice toward corona virus infection among pregnant women attending antenatal care clinics at Kafrelsheikh, Egypt. Int Egyptian J Nurs Sci Res. 2022;2(2):241–252. doi: 10.21608/ejnsr.2022.212455. [DOI] [Google Scholar]
- 58.Temesgan WZ, Aklil MB, Yacob HS, Mekonnen ET, Tegegne ED, Tesfa EB, et al. Adherence to COVID-19 preventive practice and associated factors among pregnant women in Gondar city, northwest Ethiopia, 2021: Community-based cross-sectional study. PLoS ONE. 2022;17(3):e0264237. doi: 10.1371/journal.pone.0264237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aboma D, Gurmu S. Level of Knowledge and Preventive Practices against Covid-19 Pandemic Infection among Pregnant Women Visiting Serbo Health Center, Jimma Town South West Ethiopia. J Women's Health Care. 2021;10(510):2167–0420.21. [Google Scholar]
- 60.Elhameed E, El-Rahman A, El-Razek AA, Ayoub GG. Knowledge assessment of pregnant women and maternity nurses regarding coronavirus (COVID-19) Menoufia Nurs J. 2022;7(1):267–282. doi: 10.21608/menj.2022.245473. [DOI] [Google Scholar]
- 61.Abdus-Salam RA, Lawal TV, Lawal OO, Akinlusi FM, Bello OO, Morhason-Bello IO. Determinants of correct knowledge of coronavirus infection and COVID-19 disease pandemic among pregnant women in South-West Nigeria. Nigerian Postgraduate Medical Journal. 2021;28(4):240. doi: 10.4103/npmj.npmj_650_21. [DOI] [PubMed] [Google Scholar]
- 62.Burodo A. Awareness and practice of COVID-19 preventive measures among pregnant women attending antenatal care clinic in a tertiary health centre in North-Western Nigeria. Sch Int J Obstet Gynec. 2021;5(1):14–20. [Google Scholar]
- 63.Metwally HMS, MMAEM D. Knowledge, practice and attitudes of preventive measures against coronavirus infection among pregnant women in Egypt. Saudi J Nurs Health Care. 2020;(3):156–66. 10.36348/sjnhc.2020.v03i06.001.
- 64.Omozuwa SE, Uwaibi NE. Level of awareness, knowledge and perception on COVID-19 among pregnant women attending antenatal clinics in Central Hospital Benin City, Edo state. Ann Clin Biomed Res. 2021;2(1):1–7.
- 65.Ayele AD, Mihretie GN, Belay HG, Teffera AG, Kassa BG, Amsalu BT. Knowledge and Practice to Prevent Against Corona Virus Disease (COVID-19) and Its Associated Factors Among Pregnant Women in Debre Tabor Town Northwest Ethiopia: a Community Based Cross-Sectional Study. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Degu A, Nibret G, Gebrehana H, Getie A, Getnet B. Knowledge and attitude towards the current pandemic corona virus disease and associated factors among pregnant women attending antenatal care in debre tabor general hospital northwest ethiopia: an institutional-based cross-sectional study. Int J Women's Health. 2021;13:61. doi: 10.2147/IJWH.S285552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kassie BA, Asratie MH, Abate AT. The effects of fear and knowledge of COVID-19 on preventive practice among pregnant women who attend antenatal care in northwest Ethiopia, 2020: institution-based cross-sectional study. Int J Women's Health. 2021;13:95. doi: 10.2147/IJWH.S286088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kumbeni MT, Apanga PA, Yeboah EO, Lettor IBK. Knowledge and preventive practices towards COVID-19 among pregnant women seeking antenatal services in Northern Ghana. PLoS ONE. 2021;16(6):e0253446. doi: 10.1371/journal.pone.0253446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fikadu Y, Yeshaneh A, Melis T, Mesele M, Anmut W, Argaw M. Covid-19 preventive measure practices and knowledge of pregnant women in guraghe zone hospitals. Int J Women's Health. 2021;13:39. doi: 10.2147/IJWH.S291507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Adegoke J, Ajibade B, Rhoda D. Knowledge, attitude and practice of preventive measures towards COVID-19 among pregnant women attending selected primary health centre’s in Osogbo, Osun state. Int J Nursing Midwife Heal Relat Cases. 2020;6(2):29–45. [Google Scholar]
- 71.Aduloju OP, Okunola TO, Adefisan A, Aduloju T. Knowledge, attitude and practice of preventive measures against coronavirus disease 2019 among pregnant women in a tertiary health facility in southwest Nigeria. Int J Clin Obstet Gynaecol. 2021;5(3):101–107. doi: 10.33545/gynae.2021.v5.i3b.911. [DOI] [Google Scholar]
- 72.Omoronyia EE, Eyong E, Omoronyia OE, Akpan U, Arogundade K, Ekanem EI. Knowledge, attitude, and practice of preventive measures against COVID-19 among pregnant women receiving antenatal care in Calabar, Nigeria. Niger J Med. 2021;30(5):548. doi: 10.4103/NJM.NJM_16_21. [DOI] [Google Scholar]
- 73.West B, Aitafo J, Genesis D, Kalio B. Knowledge, attitudes and practices of pregnant women attending the antenatal clinic of rivers state university teaching hospital, Nigeria towards the coronavirus (COVID-19) pandemic. Int J Health Sci Res. 2021;11:21–33. doi: 10.52403/ijhsr.20210403. [DOI] [Google Scholar]
- 74.Hoque A, Alam A, Hoque M, Hoque M, Van Hal G. Knowledge, attitudes, and practices towards COVID-19 of pregnant women at a primary health care facility in South Africa. Eur J Med Health Sci. 2021;3(1):50–55. doi: 10.24018/ejmed.2021.3.1.654. [DOI] [Google Scholar]
- 75.Theuring S, Kengonzi A, Hafermann L, Herrmann C, Kabwama SN, Rubaihayo J. Repercussions of the COVID-19 response in pregnant women in western Uganda: Knowledge, behavior, and emotional state after the first lockdown in 2020. Int J Environ Res Public Health. 2021;18(15):7817. doi: 10.3390/ijerph18157817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Besho M, Tsegaye R, Yilma MT, Kasaye HK, Tolossa T, Hiko N, et al. Knowledge, attitude and practice toward corona virus infection among pregnant women attending antenatal care at public hospitals in three wollega zones, ethiopia. Int J Gen Med. 2021;14:3563. doi: 10.2147/IJGM.S295490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Silesh M, Demisse TL, Taye BT, Desta K, Kitaw TM, Mekuria AD, et al. Compliance with COVID-19 preventive measures and associated factors among women attending antenatal care at public health facilities of Debre Berhan Town, Ethiopia. Risk Manage Healthc Policy. 2021;14:4561–9. [DOI] [PMC free article] [PubMed]
- 78.Nwafor JI, Aniukwu JK, Anozie BO, Ikeotuonye AC, Okedo-Alex IN. Pregnant women’s knowledge and practice of preventive measures against COVID-19 in a low-resource African setting. Int J Gynaecol Obstet. 2020;150(1):121–123. doi: 10.1002/ijgo.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zeleke AM, Bayeh GM. Knowledge, attitude and practice towards COVID-19 and associated factors among pregnant women at Debark Town Northwest Ethiopia: An institutional-based cross-sectional study. 2022. [Google Scholar]
- 80.Anikwe CC, Ogah CO, Anikwe IH, Ewah RL, Onwe OE, Ikeoha1c CC. Coronavirus 2019 pandemic: assessment of the level of knowledge, attitude, and anxiety among pregnant women in Ebonyi State, Nigeria. Ann Med Health Sci Res. 2021;11(2):1267–73.
- 81.Belayneh M, Agumas Y, Engidaw D. Factors influencing knowledge, attitude and practice of COVID-19 preventive measures among pregnant women attending antenatal care in Adiarkay District, Northwest Ethiopia. 2021. [Google Scholar]
- 82.Yazew BG, Abate HK, Mekonnen CK. Knowledge, attitude and practice towards COVID-19 in Ethiopia: a systematic review; 2020. Patient Prefer Adherence. 2021;15:337. doi: 10.2147/PPA.S288186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Azene AG, Workie MS, Aragaw AM. Knowledge, attitude, and prevention practices toward coronavirus disease 2019 in Ethiopia: a systematic review and meta-analysis. Curr Ther Res. 2021;94:100633. doi: 10.1016/j.curtheres.2021.100633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bekele F, Sheleme T, Fekadu G, Bekele K. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: a systematic review. SAGE open medicine. 2020;8:2050312120970721. doi: 10.1177/2050312120970721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Obi CG, Fozeu LF, Ezaka EI, Ochonma C, Kamwela R. Knowledge, Attitudes, Practices, and Misconceptions towards COVID-19 among Sub-Sahara Africans. Eur J Environ Public Health. 2022;6(1):em0101. doi: 10.21601/ejeph/11559. [DOI] [Google Scholar]
- 86.Mose A, Zewdie A, Sahle T. Pregnant women’s knowledge, attitude, and practice towards COVID-19 infection prevention in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2022;17(10):e0276692. doi: 10.1371/journal.pone.0276692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lake EA, Demissie BW, Gebeyehu NA, Wassie AY, Gelaw KA, Azeze GA. Knowledge, attitude and practice towards COVID-19 among health professionals in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2021;16(2):e0247204. doi: 10.1371/journal.pone.0247204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Alahdal H, Basingab F, Alotaibi R. An analytical study on the awareness, attitude and practice during the COVID-19 pandemic in Riyadh, Saudi Arabia. J Infect Public Health. 2020;13(10):1446–1452. doi: 10.1016/j.jiph.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jokar M, Rahmanian V. Potential use of Google Search Trend analysis for risk communication during the mpox (formerly monkeypox) outbreak in Iran. Health Sci Rep. 2023;6(1):1–4. [DOI] [PMC free article] [PubMed]
- 90.Siddiquea BN, Shetty A, Bhattacharya O, Afroz A, Billah B. Global epidemiology of COVID-19 knowledge, attitude and practice: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e051447. doi: 10.1136/bmjopen-2021-051447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Marzban A, Ramezani-Siakhulak F, Rahmanian V, Dolatabadi M, Ansari A, Aghda MA. The Effect of Education on the Knowledge, Attitude, and Practice of Breastfeeding Mothers towards Heavy Metals Transferred from Breast Milk. J Nutr Food Secur. 2022;7(4):437–44.
- 92.Azlan AA, Hamzah MR, Sern TJ, Ayub SH, Mohamad E. Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study in Malaysia. PLoS ONE. 2020;15(5):e0233668. doi: 10.1371/journal.pone.0233668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zheng X, Zhang J, Ye X, Lin X, Liu H, Qin Z, et al. Navigating through motherhood in pregnancy and postpartum periods during the COVID‐19 pandemic: a systematic review and qualitative meta‐synthesis. J Nurs Manage. 2022. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: S1 Table. strategy search for the KAP towards COVID-19 among pregnant women.
Data Availability Statement
The authors acknowledge that data supporting the findings of this study are available in the article [and/or] its supplementary material.