Abstract
Background:
Tai Chi is emerging as a promising treatment for a variety of pain conditions, including chronic nonspecific neck pain. Given this trend, it is important to better understand the dose–response relationship and how pain, anxiety, and depression impact this relationship.
Method:
This secondary analysis used data from the Tai Chi arm (age = 52.03 ± 10.92 years; 73.68% female; n = 38) of a randomized controlled trial for chronic nonspecific neck pain. The authors tested whether (1) greater home practice time or cumulative practice time during the intervention predicted greater post-treatment reductions in neck pain intensity and (2) reporting greater neck pain intensity during the current week relative to other weeks was associated with lower home practice time during the current week. Post hoc analyses were conducted to evaluate whether baseline anxiety and depression levels moderated the association between weekly pain intensity and weekly home practice time.
Results:
While cumulative Tai Chi practice time (i.e., home practice + class time) was associated with post-treatment reductions in neck pain intensity, home practice time alone was not associated with post-treatment reductions in neck pain. Participants with low and moderate baseline anxiety were found to practice less than usual on weeks when pain intensity was worse, while participants with high baseline anxiety were found to practice more than usual on weeks when pain intensity was worse. Baseline depression levels did not moderate the effect of weekly pain intensity on weekly home practice time.
Conclusions:
Combined class and at-home exposure to Tai Chi appears to be critical to reductions in chronic nonspecific neck pain. In addition, anxiety may be an important characteristic that partially governs the dose–response relationship in participants with chronic nonspecific neck pain.
Clinical Trial Registration:
Keywords: Tai Chi, home practice time, neck pain, anxiety, depression
Introduction
With an annual prevalence rate greater than 30%, chronic neck pain is ranked fourth globally on the years lived with disability index and 21st in overall global burden.1,2 Given such a consequential societal impact, considerable research attention has been directed toward noninvasive and nonpharmacologic treatments for chronic neck pain, such as exercise and manual therapy.3 However, despite this attention, these interventions show only modest effect sizes in reducing neck pain.3 To offer patients a wider range of interventions, a number of studies have examined the use of mind–body interventions for chronic neck pain.
Commonly used evidence-based mind–body approaches for chronic neck pain include meditation, yoga, clinical and relaxation massage, progressive muscle relaxation, and biofeedback,3 with meditation and movement-based awareness practices receiving increasingly greater attention in recent years.4–7 While results on the effects of meditation on chronic neck pain are mixed, movement- and breath-based awareness practices, such as yoga, Tai Chi, and Qigong, are emerging as promising economical treatment alternatives for chronic neck pain.6,8–13 An important next step in advancing this research is to assess the impact of factors that may directly and indirectly impact the benefits of these interventions.
Increased compliance with home practice is one way to possible improvements in outcomes. To date, no studies have examined the influence of Tai Chi home practice time on pain intensity. However, doing so is critically important as dose–response effects in mind–body movement interventions appear to be inconsistent, with two studies finding null effects, a separate study reporting clinically significant effects and a few studies demonstrating clinically significant day-to-day effects at the within-person level but no improvements at the between-person level.14–18 Furthermore, a literature review of Tai Chi clinical trials found large variations in recommended home practice time across studies and infrequent reporting of home practice time.19
On the contrary, cumulative Tai Chi practice time (i.e., home practice + class time) appears to be a prominent marker of treatment response. For example, a randomized trial of a Tai Chi intervention of 86 postmenopausal osteopenic women reported greater improvements in femoral neck bone mineral density, bone formation markers, and physical quality of life only for participants who completed at least 75% of the training requirements, totaling 74.63 h of practice time.20 In a separate study of 60 Tai Chi novice adults and 27 Tai Chi experts, findings demonstrated that (1) treatment-related gains in postural sway among novice participants was positively associated with number of practice hours and (2) greater exposure to Tai Chi in both novice and expert participants was linked to better physical function.21 Last, another study reported a strong dose–response relationship in pain and function among participants enrolled in a Tai Chi and physical therapy intervention for symptomatic knee osteoarthritis.22
Studies examining dose–response effects in mindfulness-based practices have also reported divergent results, rendering it unclear whether formal daily mindfulness practice is the primary mechanism of change in mindfulness-based interventions for novice practitioners.23,24 Be that as it may, in a 12-week yoga program for stress reduction, where participants were randomized to low, medium, or high home practice time conditions, only participants in the high practice time condition demonstrated significant reductions in stress.14–18,23,24 Together, the inconclusive nature of these findings warrants further investigation into quantifying dose–response effects in mind–body interventions. One explanation worthy of attention draws from the common factors in psychotherapy literature. The common factors model suggests that nonspecific treatment components, such as group and instructor characteristics, may hold similar weight to treatment-specific components, such as home practice time, in improving outcomes.23
In addition to assessing dose–response effects in Tai Chi interventions, another particularly compelling line of inquiry is to elucidate the correspondence between weekly fluctuation in neck pain intensity and weekly fluctuation in home practice time. Extant literature on mind–body interventions for chronic pain has yet to evaluate whether week-to-week variation in pain intensity adversely impacts weekly home practice time. Furthermore, it is possible that the effect of weekly neck pain intensity on weekly home practice time depends on baseline anxiety and depression levels. Uncovering how anxiety and depression may differentially influence the association between pain intensity and home practice time will aid mind–body instructors in providing individualized home practice recommendations.
Aims
The authors' first aim was to test whether greater home practice time or cumulative practice time (i.e., home practice + class time) during the intervention predicted greater reductions in neck pain intensity at post-treatment. Their second aim was to examine whether reporting greater neck pain intensity during the current week relative to other weeks was associated with lower home practice time during the current week. In a post hoc analysis, the authors aimed to evaluate whether baseline anxiety and depression levels moderated the association between weekly pain intensity and weekly home practice time.
Materials and Methods
Design
This is a secondary analysis of a randomized controlled trial conducted at the Department of Internal and Integrative Medicine, Evang. Kliniken Essen-Mitte in Essen, Germany from 2014 to 2015.9 The trial aimed to examine the efficacy and safety of Tai Chi compared with exercise and usual care in adults with chronic nonspecific neck pain. The study was approved by the University Hospital Essen Human Research Ethics Committee (Approval No. 13-5672-BO), and was registered with ClinicalTrials.gov
Participants
Only participants allocated to the Tai Chi arm were included (n = 38, age range 26–74 years, mean 52.03, standard deviation [SD] 10.92, 73.68% female). Inclusion criteria were moderate or greater chronic nonspecific neck pain, no Tai Chi, Qigong, or yoga practice for the preceding 6 months and no recent invasive treatments, major medical conditions or comorbidities. Seven participants did not report Tai Chi at-home practice time for any of the 13 weeks and were thus excluded from the present analyses.
Interventions
Participants were allocated to groups of 10–15 participants and met weekly for 75–90 min for 12 consecutive weeks. The Mantak Chia manual comprising 13 forms derived from the Yang style was used for the Tai Chi intervention. During each session, the Tai Chi form practice was preceded by 5–10 min of warm-up exercises and was followed by 5–10 min of relaxation. Breathing exercises, psychoeducation, and relaxing music were also incorporated into each session. For each sequence of movements, participants were instructed to use handouts to guide them through 15 min of daily home practice.
Outcome measures
Home practice time
To assess home practice time, participants were asked to keep a daily practice log, where they noted their total daily practice time in minutes. Total daily practice time during the intervention was summed and used as a predictor variable in hypothesis 1. Total practice time ranged from 0 to 3530 min, with a mean of 447 min, a median of 240 min and a SD of 694 min. Of the participants who provided at-home practice logs, 12 reported 0 min of total home practice time.
Pain intensity
The intensity item from the German Pain Questionnaire was used to measure pain intensity.25,26 The item uses a 0–100 mm visual analog scale (VAS) to measure pain intensity, which ranges from “no neck pain at all” to “worst neck pain imaginable.” Participants provided neck pain intensity ratings in a daily log. Weekly pain intensity was derived as the average of daily pain intensity for each of the 12 weeks.
Anxiety and depression
The Hospital and Depression Scale was used to assess baseline anxiety and depression.27 The measure has both good internal consistency and concurrent validity.28 Total scores for the anxiety and depression subscales, comprising seven items each, were used in the present analyses. Higher scores reflected higher baseline anxiety and depression levels.
Covariates
Baseline participant expectation that Tai Chi would reduce neck pain was assessed on an 11-point Likert-type scale, with 10 labeled as, “highest possible expectation.” Class attendance was collected during each class.
Statistical analyses
The authors used the tidyverse R libraries, the nlme R library, and the sjPlot R library to structure the data, perform the ordinary least squares regressions and mixed modeling analyses, and generate the tables and figures.29–32 To test the authors' first hypothesis, the authors regressed post-treatment pain intensity scores on pretreatment pain intensity scores and total home practice time and cumulative practice time (i.e., home practice + class time) in separate models. Participant expectancy was not included in the model because it was not independently associated with post-treatment pain intensity (p > 0.05). Assumption plots did not demonstrate aberrant departures from normality, independence, homoscedasticity, or linearity.
Given that the second hypothesis involved assessing longitudinal effects, the authors used linear mixed models to examine the time-varying effect of weekly pain intensity on weekly home practice time (see Appendix A1 for analytic procedure).33 In the full model, Tai Chi weekly home practice time in minutes was entered as the dependent variable and the within-person variable for pain intensity was included as the independent variable. In post hoc analyses, anxiety, depression, and their interaction with within-person pain intensity were included in two separate models.
Anxiety and depression were centered at their means to aid in the interpretation of coefficients. Participant expectation and class attendance were not independently associated with weekly home practice time and were, therefore, not included in the final model (p's > 0.05). As shown by examination of model assumption plots, a random linear time model estimated with restricted maximum likelihood and a heterogeneous error variance term fit the data adequately and precluded the need to use a Poisson function.34
Results
Effect of Tai Chi practice time on post-treatment neck pain intensity
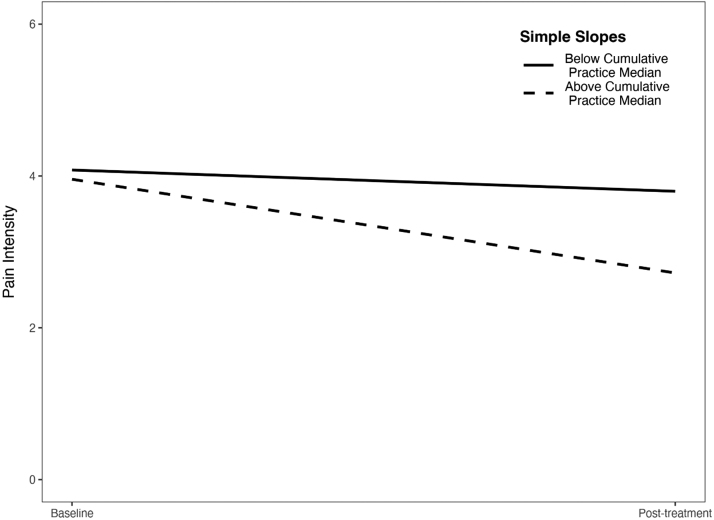
Participant baseline expectancy was not independently associated with post-treatment neck pain intensity and was thus not included as a covariate in the full model (b = 0.07, standard error [SE] = 0.25, t = 0.26, p = 0.79). Although greater total home practice time was not associated with lower post-treatment pain intensity scores (b = −0.00, SE = 0.00, t = −1.30, p = 0.20), greater cumulative practice time was associated with lower post-treatment pain intensity (b = −0.001, SE = 0.00, t = −3.97, p < 0.001; Fig. 1).
FIG. 1.
The effect of cumulative practice time on pain intensity. Median cumulative practice time (home practice + class time) was 720 min.
Association between weekly fluctuation in pain intensity and weekly home practice time
Results showed a significant effect of within-person weekly fluctuation in pain intensity on weekly home practice time, with weekly home practice time decreasing by 4.49 min for every unit increase in weekly pain intensity (b = −4.49, SE = 2.14, t = −2.10, p = 0.037). Post hoc analyses showed that baseline depression levels did not moderate the effect of within-person weekly fluctuation in pain intensity on weekly home practice time (b = 0.38, SE = 0.86, t = 0.44, p = 0.659).
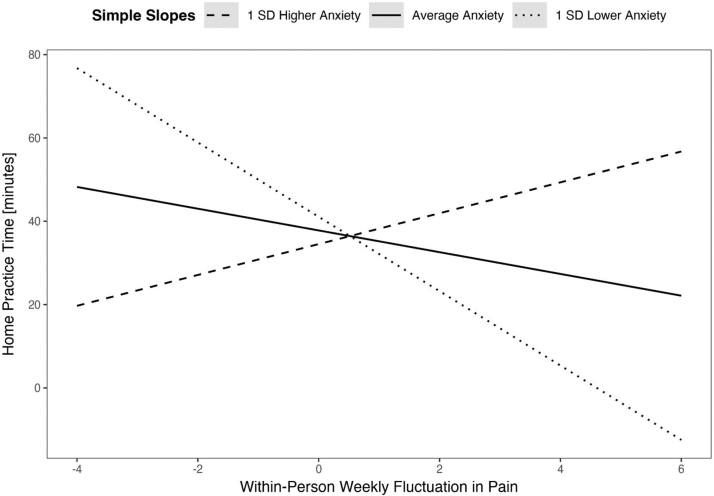
However, post hoc analyses demonstrated a crossed interaction between baseline anxiety levels and within-person weekly fluctuation in pain intensity (Table 1 and Fig. 2). Participants with low and average anxiety levels demonstrated a decrease in weekly home practice time on weeks when pain intensity was greater than usual (i.e., than on other weeks), with a greater effect for those with low anxiety levels (Table 1 and Fig. 2). In contrast, on weeks when pain intensity was greater than usual, participants with greater baseline anxiety levels showed evidence of an increase in weekly home practice time (Table 1 and Fig. 2).
Table 1.
Longitudinal Outcomes in Home Practice Time
| Predictors | Home practice time |
|||||
|---|---|---|---|---|---|---|
| b | SE | CI | t | df | p | |
| Within-person pain | −3.63 | 1.62 | −6.83 to −0.44 | −2.23 | 28 | 0.026 |
| Baseline anxiety | −0.90 | 2.39 | −5.79 to 4.00 | −0.37 | 28 | 0.711 |
| Between-person pain | 1.23 | 5.80 | −10.65 to 13.11 | 0.21 | 358 | 0.833 |
| Within-person pain × Baseline anxiety | 1.64 | 0.58 | 0.51 to 2.78 | 2.84 | 358 | 0.005 |
Within-person pain = weekly fluctuation in pain intensity (VAS) or experiencing greater pain intensity than on other weeks; baseline anxiety = anxiety measured before the Tai Chi intervention with the hospital and depression scale; between-person pain = cross-sectional pain intensity (VAS) or experiencing greater pain than other participants. Bold p-values indicate statistical significance.
CI, confidence interval; SE, standard error; VAS, visual analog scale.
FIG. 2.
Impact of weekly pain intensity on weekly home practice time by baseline anxiety. Average baseline anxiety was 6.95 and the SD was 3.83. SD, standard deviation.
Discussion
The present findings demonstrate that Tai Chi cumulative practice time (home practice + class time), but not home practice time alone, is an important predictor of post-treatment reductions in chronic nonspecific neck pain. The authors also found that on weeks when pain intensity is worse than usual (i.e., than on other weeks), individuals with low and moderate baseline anxiety levels are likely to practice less than usual, while individuals with high baseline anxiety levels are likely to practice more than usual. Contrary to the effect of baseline anxiety levels, the authors did not find that the association between weekly pain intensity and home practice time depends on baseline depression levels. Last, the study failed to show effects of baseline expectation and class attendance on post-treatment pain intensity.
In light of the divergent results on home practice time and outcomes in integrative medicine interventions, it is not especially surprising that cumulative practice time, but not home practice time, predicted post-treatment reductions in pain intensity. Taking a common factors approach, it may be that the total sum of all specific and nonspecific treatment components, rather than of any one treatment-specific component alone (e.g., home practice time), is what drives pain reductions in Tai Chi interventions and in related integrative medicine interventions.
For example, Tai Chi is traditionally practiced in a group setting, where participants provide verbal and nonverbal support to one another, which may function to augment pain intensity. Additional symbols of healing in Tai Chi courses, such as a revered instructor, the location in which participants gather, the ambience of the practice room, the clothing worn by the instructor and participants and the novelty of the intervention itself, may also explain a significant amount of variance in symptom improvement.35,36 The literature on Tai Chi for chronic pain would benefit from designing dismantling studies to elucidate the unique influence of treatment-specific and nonspecific factors on primary outcome measures.
This is the first study to examine the moderating effects of depression and anxiety on the association between pain intensity and Tai Chi home practice time. A study that evaluated the association between depression and home practice time in mindfulness-based cognitive therapy found that greater depression was associated with less at-home mindfulness practice.37 The discrepant result on the link between home practice time and depression may be due to low variability in the depression variable, with only a small number of participants endorsing depressive symptoms at baseline.
Although no studies have examined the association between home practice time and anxiety in integrative medicine interventions, a few studies have examined the role of neuroticism in integrative medicine interventions. Neuroticism, a personality trait characterized by a predisposition for negative states of mind such as anxiety, has been associated with greater class attendance in a yoga and meditation intervention for breast cancer survivors38 and with better outcomes in a mindfulness intervention for police officers.39 In so far that anxiety is construed as a response to a perceived threat marked by motivation and mobilization,40 it may be that participants with greater anxiety interpret greater pain intensity as a threat and are mobilized to reduce the pain (i.e., threat) by increasing Tai Chi home practice. Future studies should investigate whether greater anxiety- and pain-related home practice time is associated with greater symptom improvement in Tai Chi interventions for chronic pain.
From an embodied cognition perspective (or enactive cognitive science), whereby the construct of feedback loops is utilized to study the mind/body as a monistic phenomenon rather than as a dualistic problem, it may be that the bidirectional nature of pain catastrophizing and physiological arousal is integral to understanding inter- and intraindividual differences in Tai Chi home practice.41 For example, the ruminative thought, “I'm really worried that the pain will never go away,” in response to neck pain may further exacerbate the physiological pain response and result in increased, possibly maladaptively effortful, Tai Chi home practice. This potential interpretation is empirically corroborated by the finding that reduced pain catastrophizing explains approximately one-third of the variance in Tai Chi-related improvements in low back pain.42
It is also supported by observations that changes in body posture and affect, including anxiety and depression, are associated over the course of mind–body training for chronic pain.43 While speculative, future research may benefit from designing lead-lag studies to better understand the temporal dynamics of how pain and anxiety impact Tai Chi home practice. Such efforts would be consistent with prior literature demonstrating that mind–body practices reduce chronic pain by targeting both bottom-up and top-down self-regulatory processes.44,45 In addition to quantitative approaches, the inclusion of semistructured qualitative interviews would deepen the authors' phenomenological understanding of how anxiety and the instructor–participant relationship motivate practitioners to develop a consistent Tai Chi practice.
Limitations
The limitations of this study highlight important considerations for future research. Although the results showed an association between within-person weekly fluctuation in pain intensity and Tai Chi home practice time, it is unclear whether increased pain intensity causes a reduction in home practice time or vice versa. Future studies should seek to identify whether increases in weekly pain intensity cause a reduction in weekly home practice time or whether less home practice causes greater weekly pain intensity. In conjunction with a small sample size, the VAS pain intensity scale may be susceptible to capturing random fluctuation in pain symptoms. Future studies examining the effect of Tai Chi home practice time on pain intensity may benefit from considering alternative composite measures of chronic pain. Last, it may be important for future studies to assess Tai Chi treatment expectations over time to better assess whether treatment expectations impact chronic pain outcomes.
Conclusions
Total class and at-home Tai Chi practice time is an important mechanism by which chronic nonspecific neck pain improves. Furthermore, baseline anxiety may help to explain dose–response effects in Tai Chi interventions for chronic nonspecific neck pain.
Appendix
Appendix A1
By virtue of maximum likelihood estimation, linear mixed models are advantageous to least-squares models in their handling of data that are missing at random. To derive an estimate of within-person weekly fluctuation in pain intensity, the authors first detrended variance due to the reduction of pain over time by regressing time, centered at week 6, on pain intensity.A1 They then used level 1 residuals as the within-person effect of pain intensity (i.e., reporting greater pain intensity than on other weeks) and used level 2 random intercepts as the between-person effect of pain intensity (i.e., reporting greater pain intensity than other participants).A1
Appendix Reference
- A1.Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol 2011;62:583–619; doi: 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
Authors' Contributions
All authors contributed substantially to the article and approved the final article.
Author Disclosure Statement
P.W. is the founder and sole owner of the Tree of Life Tai Chi Center. P.W.'s interests were reviewed and managed by the Brigham and Women's Hospital and Partner's HealthCare in accordance with their conflict of interest policies. H.C., R.L., and S.A. do not have any conflicts of interest to disclose.
Funding Information
This study was supported by grants to P.W. from the National Center for Complementary and Integrative Health/National Institutes of Health (K24AT009282).
References
- 1. Haldeman S, Carroll L, Cassidy JD. Findings from the bone and joint decade 2000 to 2010 task force on neck pain and its associated disorders. J Occup Environ Med 2010;52(4):424–427; doi: 10.1097/JOM.0b013e3181d44f3b [DOI] [PubMed] [Google Scholar]
- 2. Hoy D, March L, Woolf A, et al. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73(7):1309–1315; doi: 10.1136/annrheumdis-2013-204431 [DOI] [PubMed] [Google Scholar]
- 3. Chou R, Côté P, Randhawa K, et al. The Global Spine Care Initiative: Applying evidence-based guidelines on the non-invasive management of Back and Neck Pain to Low- and Middle-Income Communities. Eur Spine J 2018;27(S6):851–860; doi: 10.1007/s00586-017-5433-8 [DOI] [PubMed] [Google Scholar]
- 4. Rosenzweig S, Greeson JM, Reibel DK, et al. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res 2010;68(1):29–36; doi: 10.1016/j.jpsychores.2009.03.010 [DOI] [PubMed] [Google Scholar]
- 5. Jeitler M, Brunnhuber S, Meier L, et al. Effectiveness of Jyoti meditation for patients with chronic neck pain and psychological distress—A randomized controlled clinical trial. J Pain 2015;16(1):77–86; doi: 10.1016/j.jpain.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 6. Cramer H, Klose P, Brinkhaus B, et al. Effects of yoga on chronic neck pain: A systematic review and meta-analysis. Clin Rehabil 2017;31(11):1457–1465; doi: 10.1177/0269215517698735 [DOI] [PubMed] [Google Scholar]
- 7. Koch AK, Cramer H. Complementary medicine use in patients with low back or neck pain: Results of the 2017 National Health Interview Survey. Pain Med 2021;22(10):2393–2400; doi: 10.1093/pm/pnab169 [DOI] [PubMed] [Google Scholar]
- 8. Fernandez MM, Maldonado Fernandez M, Rubio Rodriguez L, et al. Evidence-based mindfulness. Eur Psychiatry 2016;33(S1):S635–S635; doi: 10.1016/j.eurpsy.2016.01.2389 [DOI] [Google Scholar]
- 9. Lauche R, Stumpe C, Fehr J, et al. The effects of Tai Chi and neck exercises in the treatment of chronic nonspecific neck pain: A randomized controlled trial. J Pain 2016;17(9):1013–1027; doi: 10.1016/j.jpain.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 10. Lauche R, Wayne PM, Fehr J, et al. Does postural awareness contribute to exercise-induced improvements in neck pain intensity? A secondary analysis of a randomized controlled trial evaluating Tai Chi and neck exercises. Spine 2017;42(16):1195–1200; doi: 10.1097/brs.0000000000002078 [DOI] [PubMed] [Google Scholar]
- 11. Xie Y-H, Liao M-X, Wang M-Y, et al. Traditional Chinese mind and body exercises for neck pain: A meta-analysis of randomized controlled trials. Pain Res Manag 2021;2021:5426595; doi: 10.1155/2021/5426595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kong L, Ren J, Fang S, et al. Traditional Chinese exercises on pain and disability in middle-aged and elderly patients with neck pain: A systematic review and meta-analysis of randomized controlled trials. Front Aging Neurosci 2022;14:912945; doi: 10.3389/fnagi.2022.912945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Girard J, Girard A. The effects of qigong on neck pain: A systematic review. Complement Ther Clin Pract 2019;34:23–29; doi: 10.1016/j.ctcp.2018.10.013 [DOI] [PubMed] [Google Scholar]
- 14. Carson JW, Carson KM, Porter LS, et al. Yoga for women with metastatic breast cancer: Results from a pilot study. J Pain Symptom Manage 2007;33(3):331–341; doi: 10.1016/j.jpainsymman.2006.08.009 [DOI] [PubMed] [Google Scholar]
- 15. Groessl EJ, Weingart KR, Aschbacher K, et al. Yoga for veterans with chronic low-back pain. J Altern Complement Med 2008;14(9):1123–1129; doi: 10.1089/acm.2008.0020 [DOI] [PubMed] [Google Scholar]
- 16. Greenberg J, Braun TD, Schneider ML, et al. Is less more? A randomized comparison of home practice time in a mind-body program. Behav Res Ther 2018;111:52–56; doi: 10.1016/j.brat.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carson JW, Carson KM, Olsen M, et al. Yoga practice predicts improvements in day-to-day pain in women with metastatic breast cancer. J Pain Symptom Manage 2021;61(6):1227–1233; doi: 10.1016/j.jpainsymman.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chen M-L, Wotiz SB, Banks SM, et al. Dose-response association of Tai Chi and cognition among community-dwelling older adults: A systematic review and meta-analysis. Int J Environ Res Public Health 2021;18(6):3179; doi: 10.3390/ijerph18063179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sannes TS, Mansky PJ, Chesney MA. The need for attention to dose in mind–body interventions: Lessons from T'ai Chi Clinical Trials. J Altern Complement Med 2008;14(6):645–653; doi: 10.1089/acm.2007.0680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wayne PM, Kiel DP, Buring JE, et al. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: A pilot pragmatic, randomized trial. BMC Complement Altern Med 2012;12:7; doi: 10.1186/1472-6882-12-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wayne PM, Gow BJ, Costa MD, et al. Complexity-based measures inform effects of Tai Chi training on standing postural control: Cross-sectional and randomized trial studies. PLoS One 2014;9(12):e114731; doi: 10.1371/journal.pone.0114731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee AC, Harvey WF, Price LL, et al. Dose-response effects of Tai Chi and physical therapy exercise interventions in symptomatic knee osteoarthritis. PM R 2018;10(7):712–723; doi: 10.1016/j.pmrj.2018.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Canby NK, Eichel K, Lindahl J, et al. The contribution of common and specific therapeutic factors to mindfulness-based intervention outcomes. Front Psychol 2020;11:603394; doi: 10.3389/fpsyg.2020.603394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goldberg SB, Knoeppel C, Davidson RJ, et al. Does practice quality mediate the relationship between practice time and outcome in mindfulness-based stress reduction? J Couns Psychol 2020;67(1):115–122; doi: 10.1037/cou0000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Korb J, Pfingsten M. Der deutsche Schmerzfragebogen—Implementierte Psychometrie. Schmerz 2003;17:S47. [Google Scholar]
- 26. Pfingsten M, Nagel B, Emrich O, et al. Deutscher Schmerz-Fragebogen. Handbuch ed, Deutsche Schmerzgesellschaft e.V.; 2012. Available from: https://www.dgss.org/fileadmin/pdf/12_DSF_ Manual_2012.2.pdf
- 27. Herrmann-Lingen C, Buss U, Philip Snaith R. Hospital Anxiety and Depression Scale: HADS-D; Deutsche Version. Huber: Germany; 2011. [Google Scholar]
- 28. Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 1997;27(2):363–370; doi: 10.1017/s0033291796004382 [DOI] [PubMed] [Google Scholar]
- 29. Wickham H. tidyverse: Easily Install and Load the “Tidyverse.” R Package Version 1.2. 1; 2017. [Google Scholar]
- 30. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria; 2017. [Google Scholar]
- 31. Lüdecke D. sjPlot: Data Visualization for Statistics in Social Science. R Package Version 2.6. 3; 2018; doi: 10.5281/zenodo.1308157 [DOI] [Google Scholar]
- 32. Pinheiro J, Pinheiro J́C, Bates D. Mixed-Effects Models in S and S-PLUS. Springer Science & Business Media: United States; 2000. [Google Scholar]
- 33. Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol 2011;62:583–619; doi: 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Knief U, Forstmeier W. Violating the normality assumption may be the lesser of two evils. Behav Res Methods 2021;53(6):2576–2590; doi: 10.3758/s13428-021-01587-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wayne PM, Kaptchuk TJ. Challenges inherent to t'ai chi research: Part II-defining the intervention and optimal study design. J Altern Complement Med 2008;14(2):191–197; doi: 10.1089/acm.2007.7170b [DOI] [PubMed] [Google Scholar]
- 36. Wayne PM, Kaptchuk TJ. Challenges inherent to T'ai Chi Research: Part I—T'ai Chi as a complex multicomponent intervention. J Altern Complement Med 2008;14(1):95–102; doi: 10.1089/acm.2007.7170a [DOI] [PubMed] [Google Scholar]
- 37. Avest MJT, ter Avest MJ, Greven CU, et al. Prospective associations between home practice and depressive symptoms in mindfulness-based cognitive therapy for recurrent depression: A 15 months follow-up study. Cogn Ther Res 2021;45(2):250–261; doi: 10.1007/s10608-020-10108-1 [DOI] [Google Scholar]
- 38. Tamagawa R, Speca M, Stephen J, et al. Predictors and effects of class attendance and home practice of yoga and meditation among breast cancer survivors in a Mindfulness-Based Cancer Recovery (MBCR) Program. Mindfulness 2015;6(5):1201–1210; doi: 10.1007/s12671-014-0381-4 [DOI] [Google Scholar]
- 39. Krick A, Felfe J. Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. J Occup Health Psychol 2020;25(2):99–112; doi: 10.1037/ocp0000159 [DOI] [PubMed] [Google Scholar]
- 40. Benjamin LS. Interpersonal Reconstructive Therapy for Anger, Anxiety, and Depression: Healing Broken Hearts, Not Broken Minds. American Psychological Association: Washington, DC; 2018. [Google Scholar]
- 41. Varela FJ, Thompson E, Rosch E. The Embodied Mind, Revised Edition: Cognitive Science and Human Experience. MIT Press: United States; 2017. [Google Scholar]
- 42. Hall AM, Kamper SJ, Emsley R, et al. Does pain-catastrophising mediate the effect of tai chi on treatment outcomes for people with low back pain? Complement Ther Med 2016;25:61–66; doi: 10.1016/j.ctim.2015.12.013 [DOI] [PubMed] [Google Scholar]
- 43. Quixadá AP, Miranda JGV, Osypiuk K, et al. Qigong training positively impacts both posture and mood in breast cancer survivors with persistent post-surgical pain: Support for an Embodied Cognition Paradigm. Front Psychol 2022;13:800727; doi: 10.3389/fpsyg.2022.800727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cramer H, Mehling WE, Saha FJ, et al. Postural awareness and its relation to pain: Validation of an innovative instrument measuring awareness of body posture in patients with chronic pain. BMC Musculoskelet Disord 2018;19(1):109; doi: 10.1186/s12891-018-2031-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Osypiuk K, Thompson E, Wayne PM. Can Tai Chi and Qigong postures shape our mood? Toward an embodied cognition framework for mind-body research. Front Hum Neurosci 2018;12:174; doi: 10.3389/fnhum.2018.00174 [DOI] [PMC free article] [PubMed] [Google Scholar]