Abstract
Purpose
To evaluate the impact of preoperative anemia on postoperative complications after hip fracture surgery.
Patients and Methods
We conducted a retrospective study including hip fracture patients at a teaching hospital between 2005 and 2022. We defined preoperative anemia as the last hemoglobin measurement level before surgery < 130 g/L for men and < 120 g/L for women. The primary outcome was a composite of in-hospital major complications, including pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, arrhythmia, myocardial infarction, heart failure, stroke, and death. Secondary outcomes were cardiovascular events, infection, pneumonia, and death. We used multivariate negative binomial or logistic regression to evaluate the impact of anemia and its severity, categorized as mild (90–130 g/L for men, 90–120 g/L for women) or moderate-to-severe (< 90 g/L for both) anemia on outcomes.
Results
Of the 3540 included patients, 1960 had preoperative anemia. 188 anemic patients experienced 324 major complications, while 63 non-anemic patients had 94 major complications. The risk of major complications was 165.3 (95% CI, 149.5–182.4) and 59.5 (95% CI, 48.9–72.3) per 1000 persons in anemic and non-anemic patients, respectively. Anemic patients were more likely to have major complications than non-anemic patients (adjusted incidence rate ratio (aIRR), 1.87; 95% CI, 1.30–2.72), which was consistent in mild (aIRR, 1.77; 95% CI, 1.22–2.59) and moderate-to-severe (aIRR, 2.97; 95% CI, 1.65–5.38) anemia. Preoperative anemia also increased the risk of cardiovascular events (aIRR, 1.96; 95% CI, 1.29–3.01), infection (aIRR, 1.68; 95% CI, 1.01–2.86), pneumonia (adjusted odds ratio (aOR), 1.91; 95% CI, 1.06–3.57), and death (aOR, 3.17; 95% CI, 1.06–11.89).
Conclusion
Our findings suggest that even mild preoperative anemia is associated with major postoperative complications in hip fracture patients. This finding highlights considering preoperative anemia as a risk factor in surgical decision-making for high-risk patients.
Keywords: anemia, hip fracture, postoperative complications, risk factor
Introduction
Hip fracture is a major public health concern, particularly due to the increasing proportion of elderly individuals in the population.1 Postoperative complications resulting from hip fracture surgery can prolong hospital stays and increase the overall cost of care.2 Additionally, preliminary data suggest postoperative complications may lead to poor long-term outcomes for these patients.3 Identifying and addressing the factors that contribute to postoperative complications can help improve the overall outcome of patients undergoing hip fracture surgery.
Preoperative anemia, which affects around 40% of hip fracture patients, is a potentially modifiable risk factor.4,5 There is strong evidence that preoperative anemia is associated with adverse outcomes in the general surgical population. A meta-analysis of patients undergoing major surgery found that preoperative anemia was associated with an increased risk of in-hospital mortality, myocardial infarction, stroke, and infection.6 However, the impact of preoperative anemia on postoperative complications in hip fracture populations is not well understood.
Previous studies on hip fracture patients have mainly focused on the association between preoperative anemia and long-term mortality, while research on the association between preoperative anemia and in-hospital postoperative complications is limited.7 Early studies suggested preoperative anemia was associated with length of hospital stay, in-hospital mortality, and readmission, but did not examine other clinically important postoperative complications such as cardiovascular events, infection, and pneumonia.8 Only one study, which included 395 hip fracture patients, reported these endpoints, but due to the limited statistical power, it did not demonstrate a significant difference in the incidence of postoperative complications between anemic and non-anemic patients.9 Another pilot study with 51 hip fracture patients also failed to establish a meaningful association between preoperative anemia and in-hospital postoperative complications.10 However, the sample sizes of these previous studies were too small to draw a definitive conclusion. Additionally, it is unclear whether the severity of anemia and important patient characteristics such as advanced age, sex, and fracture type could modify such an association.
Therefore, we performed an observational cohort study to assess the relationship between preoperative anemia and postoperative complications after hip fracture surgery.
Materials and Methods
Data Source and Study Population
This is a retrospective cohort study using data from the Chinese PLA General Hospital Hip Fracture Cohort (PLAGH Hip Fracture Cohort) which is a tertiary teaching hospital-based cohort study that evaluates the prognosis of hip fracture patients in Beijing, China. The PLAGH Hip Fracture Cohort comprises over 4000 patients with hip fracture from 1991 to 2022.11 This study was approved by the Institutional Review Board of the Chinese PLA General Hospital (#S2023-059-01) and conducted in accordance with the Declaration of Helsinki. Patient consent was waived due to the retrospective nature of the study, which involves minimal risk to the patients. Appropriate measures were taken to ensure patient confidentiality and protection of their personal information.
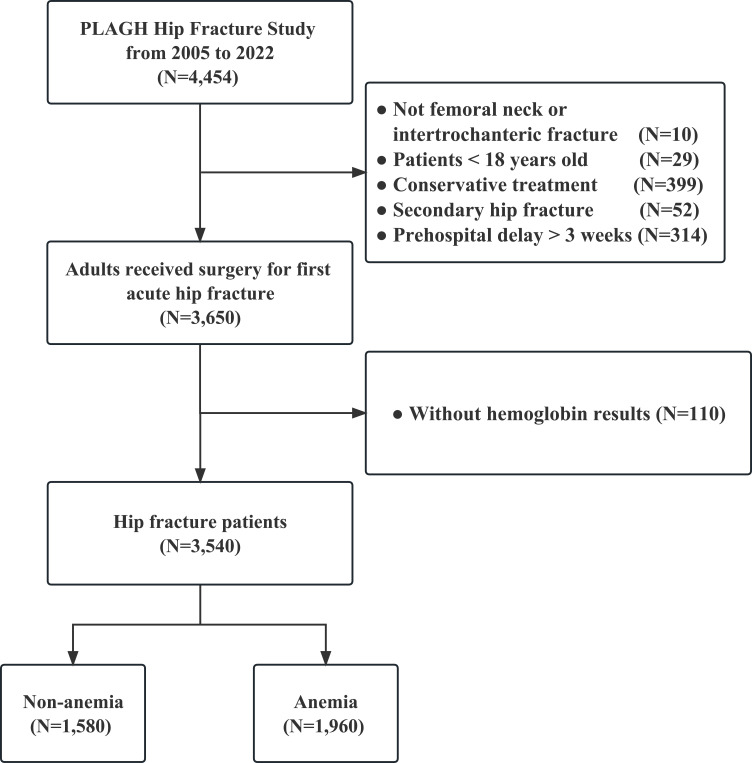
We included adult patients who had femoral neck fracture or intertrochanteric fracture and received surgery between 2005 to 2022, and whose preoperative hemoglobin (Hb) test results were available. We excluded patients with secondary hip fracture and non-fresh fracture, which were defined as more than 3 weeks from injury to admission according to a previous study (Figure 1).12
Figure 1.
Selection process of the study population.
Data Collection
We collected data on demographics such as age, sex, fracture type, body mass index (BMI), and year of admission. We also collected preexisting comorbidities, including pneumonia within three months before admission, chronic obstructive pulmonary disease, hypertension, type 2 diabetes, coronary heart disease, myocardial infarction, arrhythmia, heart failure, chronic kidney disease, stroke, liver disease, Alzheimer’s disease, Parkinson’s disease, and tumor. Additionally, we collected patients’ preoperative peripheral blood Hb level, type of surgery (internal fixation, hemiarthroplasty, total hip arthroplasty, and external fixation), type of anesthesia (general anesthesia, spinal anesthesia, peripheral nerve block, and local infiltration anesthesia), duration of surgery, and postoperative complications (postoperative pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, stroke, and death). We defined incision infection (also named as superficial surgical site infection) as a clinically reported infection of the surgical site. To describe the comorbidity burdens of each patient, we calculated the age-adjusted Charlson Comorbidity Index (aCCI) based on a previous study.13
Exposure
We defined preoperative anemia as the last Hb measurement level before the operation less than 130 g/L for men and less than 120 g/L for women according to a previous study and the World Health Organization criteria.14,15 Patients were classified into two mutually exclusive exposure groups: non-anemic and anemic groups. To further explore the impact of anemia severity on the risk of postoperative complications, we classified anemic patients into mild anemia (Hb levels between 90–130 g/L for men and 90–120 g/L for women) and moderate-to-severe anemia (Hb levels below 90 g/L for both men and women).
Outcomes
We defined the primary outcome as the total number of serious in-hospital major complications, a composite of postoperative pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, arrhythmia, myocardial infarction, heart failure, stroke, and death. To accurately reflect the clinical situation, we expressed the postoperative complications as count data, that is, we summed up the event of each complication and allowed one patient to have multiple events. All these diagnoses were adjudicated by medical specialists, such as cardiologists, neurologists, or internists from the intensive care unit, based on clinical symptoms, postoperative lab tests, electrocardiograms, or imaging examinations.
The secondary outcomes were as follows: (1) cardiovascular events, defined as a composite of deep venous thrombosis, pulmonary embolism, angina pectoris, arrhythmia, myocardial infarction, heart failure, and stroke, (2) infection, defined as a composite of postoperative pneumonia, urinary tract infection, and incision infection, (3) postoperative pneumonia, and (4) in-hospital death.
Statistical Analysis
To describe the baseline characteristics of the study population, we used frequencies and proportions for categorical variables, and mean and standard deviation for continuous variables. We compared baseline characteristics between groups using Chi-square or Fisher’s exact test for categorical variables, t-test for continuous variables, and row means score difference test for ordinal variables.
To account for the fact that patients could develop multiple complications, we treated the composite endpoints such as major complications, cardiovascular events, infection as count data. We preferred this approach over using binary data because collapsing multiple complication events into binary data would underestimate the outcome. We used negative binomial regression to analyze count data (major complications, cardiovascular events, and infection) due to overdispersion of the variance relative to the mean, and we adjusted for potential confounders according to a previous study.16 We included all variables listed in Table 1 except for aCCI after multi-collinearity examination among covariates on the basis of variance inflation factor (the variance inflation factor of aCCI was 9.19).17 We calculated the incidence rate ratio (IRR) and corresponding 95% confidence intervals (CI). Additionally, we assessed the potential bias caused by unmeasured confounders (eg, other comorbidities and severity of fracture) using the E-value.18 A large E-value implies that considerable unmeasured confounders were needed to explain the effect estimate while a small one implies little unmeasured confounders. We also performed a sensitivity analysis using logistic regression to assess the robustness of our primary outcome (major complications). In addition, we used multivariate logistic regression to analyze binary data such as pneumonia and death, adjusting for potential confounders. Finally, to examine whether important patient characteristics have modifying effects, we performed subgroup analyses stratified by age, sex, fracture type, and aCCI.
Table 1.
Baseline Characteristics of Patients Following Hip Fracture Surgery
| Non-anemia (N=1580) | Anemia (N=1960)a | P | |
|---|---|---|---|
| Year of admission | <0.001 | ||
| 2005–2010 | 481 (30.4) | 434 (22.1) | |
| 2011–2016 | 678 (42.9) | 862 (44.0) | |
| 2017–2022 | 421 (26.6) | 664 (33.9) | |
| Age | 68.1 ± 15.3 | 76.9 ± 12.8 | <0.01 |
| Sex | 0.16 | ||
| Male | 592 (37.5) | 688 (35.1) | |
| Female | 988 (62.5) | 1272 (64.9) | |
| Fracture type | <0.01 | ||
| Femoral neck fracture | 1140 (72.2) | 827 (42.2) | |
| Intertrochanteric fracture | 440 (27.8) | 1133 (57.8) | |
| Body mass index | 23.4 ± 3.4 | 22.3 ± 3.8 | <0.01 |
| Comorbidity | |||
| Pneumonia | 32 (2.0) | 94 (4.8) | <0.01 |
| COPD | 44 (2.8) | 94 (4.8) | <0.01 |
| Hypertension | 685 (43.4) | 939 (47.9) | 0.01 |
| Type 2 diabetes | 327 (20.7) | 464 (23.7) | 0.04 |
| Coronary heart disease | 219 (13.9) | 396 (20.2) | <0.01 |
| Myocardial infarction | 71 (4.5) | 111 (5.7) | 0.14 |
| Arrhythmia | 127 (8.0) | 243 (12.4) | <0.01 |
| Heart failure | 10 (0.6) | 21 (1.1) | 0.23 |
| Chronic kidney disease | 120 (7.6) | 461 (23.5) | <0.01 |
| Stroke | 232 (14.7) | 342 (17.4) | 0.03 |
| Liver disease | 31 (2.0) | 59 (3.0) | 0.06 |
| Alzheimer’s disease | 46 (2.9) | 75 (3.8) | 0.16 |
| Parkinson’s disease | 25 (1.6) | 46 (2.3) | 0.14 |
| Tumor | 121 (7.7) | 176 (9.0) | 0.18 |
| aCCI | <0.01 | ||
| 0 | 175 (11.1) | 76 (3.9) | |
| 1 | 150 (9.5) | 54 (2.8) | |
| 2 | 230 (14.6) | 104 (5.3) | |
| 3 | 289 (18.3) | 288 (14.7) | |
| 4 | 330 (20.9) | 489 (24.9) | |
| 5 | 178 (11.3) | 334 (17.0) | |
| ≥ 6 | 228 (14.4) | 615 (31.4) | |
| Surgery type | <0.01 | ||
| Internal fixation | 737 (46.6) | 1148 (58.6) | |
| Hemiarthroplasty | 580 (36.7) | 620 (31.6) | |
| Total hip arthroplasty | 258 (16.3) | 179 (9.1) | |
| External fixation | 5 (0.3) | 13 (0.7) | |
| Anesthesia type | <0.01 | ||
| General anesthesia | 682 (43.2) | 698 (35.6) | |
| Spinal anesthesia | 504 (31.9) | 487 (24.8) | |
| Peripheral nerve block | 385 (24.4) | 771 (39.3) | |
| Local infiltration anesthesia | 9 (0.6) | 4 (0.2) | |
| Duration of surgery | 0.01 | ||
| < 90 min | 447 (28.7) | 626 (32.2) | |
| 90–119 min | 517 (33.2) | 607 (31.3) | |
| 120–150 min | 327 (21.0) | 345 (17.8) | |
| > 150 min | 265 (17.0) | 364 (18.7) |
Notes: aWe defined anemia as hemoglobin (Hb) < 130 g/L in men and < 120 g/L in women.
Abbreviations: aCCI, age-adjusted Charlson comorbidity index; COPD, chronic obstructive pulmonary disease.
All tests were two-sided, and a p value < 0.05 was considered statistically significant. We conducted all analyses using R-3.1.4 (The Comprehensive R Archive Network; https://cran.rproject.org).
Results
Baseline Characteristics
Among the 3540 patients included in this study, 1960 (55.4%) had preoperative anemia. Anemic patients had a mean age of 76.9 ± 12.8 years, 64.9% were women, and intertrochanteric fracture (57.8%) was the most common type in these patients. Compared with non-anemic patients, those with anemia had a lower BMI (22.3 ± 3.8 vs 23.4 ± 3.4) and a higher frequency of pneumonia within 3 months before admission (4.8% vs 2.0%), chronic obstructive pulmonary disease (4.8% vs 2.8%), hypertension (47.9% vs 43.4%), type 2 diabetes (23.7% vs 20.7%), coronary heart disease (20.2% vs 13.9%), arrhythmia (12.4% vs 8.0%), chronic kidney disease (23.5% vs 7.6%), and stroke (17.4% vs 14.7%). The proportion of patients with aCCI ≥ 3 was also higher in anemic patients than those without anemia (88.0% vs 64.8%). There were significant differences between the two groups in the proportions of type of surgery and anesthesia applied and duration of surgery. (all p < 0.05) (Table 1).
Risk of Postoperative Complications
The incidence of major complications was higher in anemic patients. Out of 1960 anemic patients, 188 (9.6%) anemic patients experienced a total of 324 major complications. Among them, 124 had 1 complication, 30 had 2 complications, and 34 had at least 3 complications. In contrast, out of 1580 non-anemic patients, 63 (4.0%) experienced 94 major complications, with 48 patients having 1 complication, 5 having 2 complications, and 10 having at least 3 complications (Table 2 and Figure 2).
Table 2.
Postoperative Complications of Patients with Hip Fracture
| Non-anemia (N=1580) | Anemia (N=1960)a | P | |
|---|---|---|---|
| Major complicationsb | 63 (4.0) | 188 (9.6) | <0.01 |
| Pneumonia | 21 (1.3) | 72 (3.7) | <0.01 |
| Respiratory failure | 7 (0.4) | 28 (1.4) | 0.01 |
| Gastrointestinal bleeding | 3 (0.2) | 14 (0.7) | 0.05 |
| Urinary tract infection | 2 (0.1) | 13 (0.7) | 0.03 |
| Incision infection | 6 (0.4) | 9 (0.5) | 0.92 |
| Deep venous thrombosis | 16 (1.0) | 52 (2.7) | <0.01 |
| Pulmonary embolism | 1 (0.1) | 8 (0.4) | 0.09 |
| Angina pectoris | 3 (0.2) | 17 (0.9) | 0.01 |
| Myocardial infarction | 3 (0.2) | 6 (0.3) | 0.73 |
| Arrhythmia | 24 (1.5) | 87 (4.4) | <0.01 |
| Heart failure | 5 (0.3) | 31 (1.6) | <0.01 |
| Stroke | 15 (0.9) | 25 (1.3) | 0.45 |
| Death | 5 (0.3) | 22 (1.1) | 0.01 |
| Counts of major complications | <0.01 | ||
| 1 | 48 (3.0) | 124 (6.3) | |
| 2 | 5 (0.3) | 30 (1.5) | |
| 3 | 7 (0.4) | 14 (0.7) | |
| 4 | 0 (0.0) | 9 (0.5) | |
| 5 | 3 (0.2) | 6 (0.3) | |
| 6 | 0 (0.0) | 3 (0.2) | |
| 7 | 0 (0.0) | 2 (0.1) |
Notes: aWe defined anemia as hemoglobin (Hb) < 130 g/L in men and < 120 g/L in women. bMajor complications include pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, stroke, and death.
Figure 2.
Frequency of major complications in anemic and non-anemic patients after hip fracture surgery.
The incidence of major complications was higher in anemic patients, with a risk of 165.3 (95% CI, 149.5–182.4) per 1000 persons compared to 59.5 (95% CI, 48.9–72.3) per 1000 persons in non-anemic patients (Figure 3). After multiple adjustments, anemic patients were still more likely to have major complications compared to non-anemic patients, with an adjusted incidence rate ratio (aIRR) of 1.87 (95% CI, 1.30–2.72) (Table 3). To evaluate the potential impact of unmeasured confounders, we calculated the E-value, which was 3.15 for the IRR estimates in the anemic group with a lower confidence limit of 1.92. This suggests that substantial unmeasured confounders would be needed to explain away the association between preoperative anemia and major complications to the null.
Figure 3.
Risk (per 1000 persons) of major complications in anemic and non-anemic patients after hip fracture surgery, stratified by the frequency of complications.
Table 3.
Risk of Postoperative Complications in Hip Fracture Patients
| Non-anemia (N=1580) | Anemia (N=1960)a | P | |
|---|---|---|---|
| Primary outcome | |||
| Major complicationsb | |||
| Number of patients | 63 | 188 | - |
| Events | 94 | 324 | - |
| Risk/1000 persons (95% CI) | 59.5 (48.9–72.3) | 165.3 (149.5–182.4) | - |
| Crude IRR | Reference | 2.78 (2.03–3.81) | <0.01 |
| Adjusted IRR* | Reference | 1.87 (1.30–2.72) | <0.01 |
| Crude OR | Reference | 2.55 (1.92–3.45) | <0.01 |
| Adjusted OR* | Reference | 1.76 (1.22–2.57) | <0.01 |
| Secondary outcomes | |||
| Cardiovascular eventsc | |||
| Events | 50 | 166 | - |
| Risk/1000 persons (95% CI) | 31.6 (24.0–41.4) | 84.7 (73.2–97.9) | - |
| Crude IRR | Reference | 2.68 (1.88–3.86) | <0.01 |
| Adjusted IRR* | Reference | 1.96 (1.29–3.01) | <0.01 |
| Infectiond | |||
| Events | 29 | 94 | - |
| Risk/1000 persons (95% CI) | 18.4 (12.8–26.3) | 48.0 (39.4–58.4) | - |
| Crude IRR | Reference | 2.61 (1.70–4.13) | <0.01 |
| Adjusted IRR* | Reference | 1.68 (1.01–2.86) | <0.01 |
| Pneumonia | |||
| Number of patients | 21 | 72 | - |
| Risk/1000 persons (95% CI) | 13.3 (8.7–20.2) | 36.7 (29.2–46.0) | - |
| Crude OR | Reference | 2.83 (1.77–4.74) | <0.01 |
| Adjusted OR* | Reference | 1.91 (1.06–3.57) | <0.01 |
| Death | |||
| Number of patients | 5 | 22 | - |
| Risk/1000 persons (95% CI) | 3.2 (1.4–7.4) | 11.2 (7.4–16.9) | - |
| Crude OR | Reference | 3.58 (1.46–10.70) | 0.01 |
| Adjusted OR* | Reference | 3.17 (1.06–11.89) | 0.05 |
Notes: aWe defined anemia as hemoglobin (Hb) < 130 g/L in men and < 120 g/L in women. bMajor complications include pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, stroke, and death. cCardiovascular events include deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, and stroke. dInfection include postoperative pneumonia, urinary tract infection, and incision infection. *We adjusted all baseline variables except aCCI in Table 1 using a negative binomial model or a logistic regression model.
Abbreviations: IRR, incidence rate ratio; OR, odds ratio; CI, confidence interval.
For secondary outcomes, preoperative anemia was also significantly associated with a higher risk of cardiovascular events, infection, pneumonia, and in-hospital death. Anemic patients had a 2.68-fold higher risk of cardiovascular events (84.7; 95% CI, 73.2–97.9 per 1000 persons) than non-anemic patients (31.6; 95% CI, 24.0–41.4 per 1000 persons). After multiple adjustments, anemia was independently associated with cardiovascular events, with an aIRR of 1.96 (95% CI, 1.29–3.01). Similar results were found for infection, pneumonia, and in-hospital death between groups, with an aIRR of 1.68 (95% CI, 1.01–2.86), an adjusted odds ratio (aOR) of 1.91 (95% CI, 1.06–3.57) and 3.17 (95% CI, 1.06–11.89), respectively (Table 3).
Severity of Anemia on the Risk of Postoperative Complications
Analysis of the severity dose-response relationship suggested that the risk of postoperative complications increased with the severity of anemia. Among the anemic patients, 1737 (88.6%) had mild anemia while the remaining 223 (11.4%) had moderate-to-severe anemia. Patients with moderate-to-severe anemia were at a higher risk of developing major complications (aIRR, 2.97; 95% CI, 1.65–5.38), cardiovascular events (aIRR, 2.49; 95% CI, 1.27–4.78), infection (aIRR, 2.69; 95% CI, 1.27–5.64), pneumonia (aOR, 3.59; 95% CI, 1.51–8.46), and in-hospital death (aOR, 10.53; 95% CI, 2.12–55.18) following hip fracture surgery. Patients with mild anemia were also at a higher risk of major complications (aIRR, 1.77; 95% CI, 1.22–2.59) and cardiovascular events (aIRR, 1.92; 95% CI, 1.26–2.96), but this was not statistically significant for infection, pneumonia, and in-hospital death after multivariate adjustment (Table 4).
Table 4.
Severity of Anemia on the Risk of Postoperative Complications in Hip Fracture Patients
| Non-anemia (N=1580) | Mild anemiaa (N=1737) | Moderate-to-severe anemiab (N=223) | Pc | |
|---|---|---|---|---|
| Primary outcome | ||||
| Major complicationsd | ||||
| Events | 94 | 252 | 72 | - |
| Risk/1000 persons (95% CI) | 59.5 (48.9–72.3) | 145.1 (129.3–162.4) | 322.9 (265.0–386.8) | - |
| Crude IRR | Reference | 2.44 (1.77–3.37) | 5.43 (3.21–9.48) | P1<0.01, P2<0.01 |
| Adjusted IRR* | Reference | 1.77 (1.22–2.59) | 2.97 (1.65–5.38) | P1<0.01, P2<0.01 |
| Secondary outcomes | ||||
| Cardiovascular eventse | ||||
| Events | 50 | 139 | 27 | - |
| Risk/1000 persons (95% CI) | 31.6 (24.0–41.4) | 80.0 (68.1–93.7) | 121.1 (84.6–170.5) | - |
| Crude IRR | Reference | 2.53 (1.76–3.67) | 3.83 (2.12–6.88) | P1<0.01, P2<0.01 |
| Adjusted IRR* | Reference | 1.92 (1.26–2.96) | 2.49 (1.27–4.78) | P1<0.01, P2<0.01 |
| Infectionf | ||||
| Events | 29 | 69 | 25 | - |
| Risk/1000 persons (95% CI) | 18.4 (12.8–26.3) | 39.7 (31.5–49.9) | 112.1 (77.1–160.2) | - |
| Crude IRR | Reference | 2.16 (1.39–3.46) | 6.11 (3.32–11.21) | P1<0.01, P2<0.01 |
| Adjusted IRR* | Reference | 1.58 (0.95–2.71) | 2.69 (1.27–5.64) | P1=0.09, P2<0.01 |
| Pneumonia | ||||
| Number of patients | 21 | 53 | 19 | - |
| Risk/1000 persons (95% CI) | 13.3 (8.7–20.2) | 30.5 (23.4–39.7) | 85.2 (55.2–129.2) | - |
| Crude OR | Reference | 2.34 (1.42–3.97) | 6.91 (3.63–13.10) | P1<0.01, P2<0.01 |
| Adjusted OR* | Reference | 1.76 (0.97–3.33) | 3.59 (1.51–8.46) | P1=0.07, P2<0.01 |
| Death | ||||
| Number of patients | 5 | 14 | 8 | - |
| Risk/1000 persons (95% CI) | 3.2 (1.4–7.4) | 8.1 (4.8–13.5) | 35.9 (18.3–69.2) | - |
| Crude OR | Reference | 2.56 (0.98–7.94) | 11.72 (3.88–39.09) | P1=0.07, P2<0.01 |
| Adjusted OR* | Reference | 2.55 (0.91–9.76) | 10.53 (2.12–55.18) | P1=0.13, P2<0.01 |
aMild anemia, Hb 90–130 g/L in men and 90–120 g/L in women. bModerate-to-severe anemia, Hb < 90 g/L both in men and women. cP1 refers to the p value for mild anemia compared with non-anemia, and P2 refers to the p value for moderate-to-severe anemia compared with non-anemia. dMajor complications include pneumonia, respiratory failure, gastrointestinal bleeding, urinary tract infection, incision infection, deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, stroke, and death. eCardiovascular events include deep venous thrombosis, pulmonary embolism, angina pectoris, myocardial infarction, arrhythmia, heart failure, and stroke. fInfection include postoperative pneumonia, urinary tract infection, and incision infection. *We adjusted all baseline variables except aCCI in Table 1 using a negative binomial or logistic regression.
Abbreviations: IRR, incidence rate ratio; OR, odds ratio; CI, confidence interval.
Subgroup Analysis
Subgroup analyses of the primary endpoint (major complications) revealed consistent results among patients aged 65 years or older, women, with femoral neck fracture or intertrochanteric fracture, or aCCI ≥ 3, with an aIRR of 1.82 (95% CI, 1.23–2.70), 1.89 (95% CI, 1.20–3.01), 1.68 (95% CI, 1.03–2.76), 2.16 (95% CI, 1.18–4.15), and 1.78 (95% CI, 1.21–2.62), respectively. The risk of major complications in anemic patients was also higher in man than in non-anemic patients, although this association did not reach statistical significance after multivariable adjustment (Table 5).
Table 5.
Subgroup Analysis of Primary Outcome in hip Fracture Patients
| Non-Anemia (N=1580) | Anemia (N=1960)a | P | |
|---|---|---|---|
| Age ≥ 65 | |||
| Events | 84 | 310 | - |
| Number of patients | 1029 | 1700 | - |
| Risk/1000 persons (95% CI) | 81.6 (66.4–99.9) | 182.4 (164.8–201.5) | - |
| Crude IRR | Reference | 2.23 (1.60–3.13) | <0.01 |
| Adjusted IRR* | Reference | 1.82 (1.23–2.70) | <0.01 |
| Age < 65 | |||
| Events | 10 | 14 | - |
| Number of patients | 551 | 260 | - |
| Risk/1000 persons (95% CI) | 18.1 (9.9–33.0) | 53.8 (32.3–88.3) | - |
| Crude IRR | Reference | 2.97 (1.01–9.11) | 0.05 |
| Adjusted IRR* | Reference | NA | - |
| Women | |||
| Events | 69 | 202 | - |
| Number of patients | 988 | 1272 | - |
| Risk/1000 persons (95% CI) | 69.8 (55.5–87.4) | 158.8 (139.7–179.9) | - |
| Crude IRR | Reference | 2.27 (1.55–3.35) | <0.01 |
| Adjusted IRR* | Reference | 1.89 (1.20–3.01) | <0.01 |
| Men | |||
| Events | 25 | 122 | - |
| Number of patients | 592 | 688 | - |
| Risk/1000 persons (95% CI) | 42.2 (28.7–61.6) | 177.3 (150.6–207.6) | - |
| Crude IRR | Reference | 4.20 (2.44–7.41) | <0.01 |
| Adjusted IRR* | Reference | 1.91 (0.98–3.79) | 0.05 |
| Femoral neck fracture | |||
| Events | 73 | 142 | - |
| Number of patients | 1140 | 827 | - |
| Risk/1000 persons (95% CI) | 64.0 (51.2–79.7) | 171.7 (147.5–198.9) | - |
| Crude IRR | Reference | 2.68 (1.74–4.16) | <0.01 |
| Adjusted IRR* | Reference | 1.68 (1.03–2.76) | 0.03 |
| Intertrochanteric fracture | |||
| Events | 21 | 182 | - |
| Number of patients | 440 | 1133 | - |
| Risk/1000 persons (95% CI) | 47.7 (31.4–71.8) | 160.6 (140.4–183.1) | - |
| Crude IRR | Reference | 3.37 (1.98–5.92) | <0.01 |
| Adjusted IRR* | Reference | 2.16 (1.18–4.15) | 0.01 |
| aCCI < 3 | |||
| Events | 8 | 10 | - |
| Number of patients | 555 | 234 | - |
| Risk/1000 persons (95% CI) | 14.4 (7.3–28.2) | 42.7 (23.4–76.8) | - |
| Crude IRR | Reference | 2.96 (0.87–10.74) | 0.09 |
| Adjusted IRR* | Reference | NA | - |
| aCCI ≥ 3 | |||
| Events | 86 | 314 | - |
| Number of patients | 1025 | 1726 | - |
| Risk/1000 persons (95% CI) | 83.9 (68.4–102.5) | 181.9 (164.4–200.8) | - |
| Crude IRR | Reference | 2.17 (1.56–3.03) | <0.01 |
| Adjusted IRR* | Reference | 1.78 (1.21–2.62) | <0.01 |
aWe defined anemia as hemoglobin (Hb) < 130 g/L in men and < 120 g/L in women. *We adjusted all baseline variables except aCCI in Table 1 using the negative binomial regression model. NA indicates that adjusted IRR cannot be calculated due to the small number of events.
Abbreviations: CI, confidence interval; aCCI, age-adjusted Charlson comorbidity index; IRR, incidence rate ratio; NA, not applicable.
Sensitivity Analysis
To provide a more conservative estimate, we performed a sensitivity analysis using logistic regression, which yielded results consistent with the primary analysis for major complications, with an aOR of 1.76 (95% CI, 1.22–2.57) (Table 3).
Discussion
Main Findings
In this study, we found that preoperative anemia is prevalent among hip fracture patients and is associated with poor physical conditions and unfavorable in-hospital outcomes. Even mild preoperative anemia is associated with a higher risk of major postoperative complications in patients undergoing hip fracture surgery. These findings would provide evidence for surgeons to better identify and manage high-risk patients in clinical practice.
Comparison with Other Studies
Previous studies have consistently reported a high prevalence of anemia on admission among hip fracture patients, ranging from 12.3% to 45.6%.5,9,19 In our study, we defined preoperative anemia as the last Hb measurement level before the operation less than 130 g/L for men and less than 120 g/L for women according to a previous study. We found that 55.4% of hip fracture patients had preoperative anemia, which is a larger proportion than previous studies. Considering the possibility of continuous blood loss at the fracture site, the last Hb level before surgery may be a more accurate indicator of the patient’s preoperative anemia status than the Hb level on admission.
Anemic patients with hip fracture tend to be frail, malnourished, and have underlying chronic comorbidities. Anemic patients in our study were older at baseline, had a lower BMI, a higher proportion of pneumonia, chronic obstructive pulmonary disease, hypertension, type 2 diabetes, coronary heart disease, arrhythmia, chronic kidney disease, and stroke, as well as a higher proportion of multiple comorbidities (aCCI ≥ 3). Previous study found that anemia is a well-recognized indicator of malnutrition, and it may lead to adverse outcomes in patients with femoral neck fractures.20 Anemia has also been shown to be a strong prognostic factor, reflecting the underlying comorbidity burden of hip fracture patients.8 Furthermore, anemia may either reflect the severity of a chronic disease or be the result of acute blood loss from injury and may be associated with poor outcomes.
Previous research has demonstrated that preoperative anemia is associated with postoperative complications in surgical patients. A large retrospective study of 10,758 orthopedic patients found that preoperative anemia was associated with 30-day morbidity (OR, 1.53; 95% CI, 1.23–1.90), and this association was observed in both mild anemia (OR, 1.53; 95% CI, 1.23–1.91) and moderate-to-severe anemia (OR, 1.52; 95% CI, 1.00–2.31).15 Given that hip fracture patients tend to be more frail and had a higher risk of complications than those receiving general orthopedic surgery, it is important to determine the impact of preoperative anemia on this patient population. In this study, we found that preoperative anemia was associated with major complications, with an aIRR of 1.87 (95% CI, 1.30–2.72). This association was consistent in both mild anemia (aIRR, 1.77; 95% CI, 1.22–2.59) and moderate-to-severe anemia (aIRR, 2.97; 95% CI, 1.65–5.38) patients. These findings imply that even mild preoperative anemia can be an indicator of high risk for major postoperative complications in hip fracture patients.
Preoperative anemic patients are also more vulnerable to cardiovascular events in surgical patients. A previous study found that preoperative anemia is significantly associated with 30-day cardiac complications (aOR, 1.45; 95% CI, 1.29–1.65) and venous thromboembolism (aOR, 1.33; 95% CI, 1.22–1.46) in non-cardiac surgery.15 Nevertheless, few study examined this association in hip fracture patients. A recent meta-analysis found that low level of Hb was a risk factor for deep vein thrombosis (aOR, 0.32; 95% CI, 0.21–0.43) in hip fracture patients.21 A previous study of 283 hip fracture patients found anemia was a risk factor for postoperative heart failure (OR, 3.09; 95% CI, 1.29–5.91) in elderly patients with hip fracture.22 In our study, we observed preoperative anemia was associated with postoperative cardiovascular events (aIRR, 2.49; 95% CI, 1.27–4.78) in hip fracture patients.
In addition, preoperative anemic patients are also more susceptible to postoperative infections, such as pneumonia, urinary tract infection, and incision infection. A previous meta-analysis found that preoperative anemia was associated with a higher incidence of infection in cardiac surgery (OR, 2.65; 95% CI, 1.98–3.55).6 Similarly, preoperative anemia was also found to be associated with increased postoperative urinary tract infection (OR, 1.44; 95% CI, 1.25–1.66) and incision infection (OR, 1.36; 95% CI, 1.17–1.58) in patients undergoing total hip arthroplasty surgery.23,24 However, few studies have examined this association in hip fracture populations. A previous study of 395 hip fracture patients did not demonstrate a significant increase in the risk of specific postoperative infections in patients with anemia, likely due to insufficient statistical power.9 Here, we found preoperative anemia was associated with postoperative infection (aIRR, 1.68; 95% CI, 1.01–2.86) and pneumonia (aOR, 1.91; 95% CI, 1.06–3.57) in hip fracture patients.
Preoperative anemia is also strongly associated with in-hospital mortality. Previous studies have consistently reported an increased risk of in-hospital mortality in hip fracture patients, with risk ratios ranging from 1.64 to 2.90.4,6 In this study, we found that anemic patients had a higher risk of in-hospital mortality compared to non-anemic patients, with an aOR of 3.17 (95% CI, 1.06–11.89). These findings underscore the importance of identifying and managing preoperative anemia in hip fracture patients.
Potential Mechanism
Several potential mechanisms may explain the negative impact of preoperative anemia on poor postoperative outcomes. First, preoperative anemia can limit oxygen delivery to end organs and tissues, thereby lowering ischemia tolerance during hemorrhage.25 Low hemoglobin concentrations can also cause hypoxia in cells, leading to disturbances in intracellular homeostasis, decreased adenosine triphosphate concentrations, and ultimately cellular death.26 The increased susceptibility to infection due to anemia may be related to the suppression of immune system function caused by inadequate blood and oxygen supply.27 Another possible explanation may be that anemic patients are generally more vulnerable, malnourished, and have more chronic comorbidities as we found in the present study. These factors may contribute to the higher risk of poor outcomes in this patient population. However, it remains unclear whether preoperative anemia is merely a marker of a patient’s physical condition or whether it directly mediates poorer outcomes in hip fracture surgery.
Clinical Implication
These findings of our study have important implications for surgical decision-making and preoperative planning in these high-risk patients. Given the high prevalence of preoperative anemia and its associated complications, we recommend early detection of anemia and a thorough evaluation of its underlying cause, followed by appropriate treatments to minimize the risk of postoperative complications, and improve overall outcomes.
Anemia in hip fracture patients can have multiple underlying causes. Acute blood loss from fracture and soft tissue injury, as well as chronic blood loss from gastrointestinal bleeding and tumor-associated anemia, are among the main causes. Additionally, previous research has shown that about 1/3 of elderly patients with anemia are associated with malnutrition, followed by deficiencies in iron, folate, and vitamin B12 deficiencies, renal insufficiency, anemia of chronic inflammation, and other conditions.28
Timely diagnosis and treatment of the underlying cause of anemia in hip fracture patients is crucial for perioperative risk stratification and modification. Various treatments are available for anemia in hip fracture patients, including reducing bleeding, stimulating hematopoiesis, and blood transfusion, although high quality evidence for improved clinical outcomes with these treatments is limited.25 Recent randomized controlled trials have shown that oral or intravenous iron therapy has only modest benefit for erythropoiesis in anemic patients with hip fracture and does not significantly reduce postoperative complications and improve clinical outcomes.29–31 Blood transfusion, which is another common treatment choice, may theoretically improve the prognosis of hip fracture patients by correcting anemia.32 However, studies have shown that transfusion did not reverse the harms of perioperative anemia in elderly hip fracture patients, and it is associated with poor outcomes such as subsequent infection, fluid overload, prolonged hospital stays, and increased mortality.33–35 Given the shortage of blood supply, restrictive transfusion (70–90 g/L) may be a viable alternative that can reduce transfusion rates by 39–43% compared to unrestricted transfusion (90–110 g/L) and does not increase risk of complications such as myocardial infarction or mortality.35,36 Therefore, the American Academy of Orthopaedic Surgeons (AAOS) clinical practice guidelines recommend a transfusion threshold of no higher than 80 g/L in patients with hip fractures.37 Understanding the trade-offs of blood transfusion in terms of improved clinical outcomes versus increased risk of complications would help determine the optimal blood transfusion threshold and inform clinical decision-making.
Although current therapeutic measures may not significantly improve the poor outcomes associated with anemia, it is essential to make a timely diagnosis of preoperative anemia to effectively stratify high-risk patient populations. Identifying these patients as high-risk can guide perioperative management, including early minimally invasive surgery, controlled intraoperative hypotension, the use of tranexamic acid to reduce bleeding and other means of patient blood management, or additional monitoring to detect insufficient oxygen delivery to sensitive organs, prevention of surgical site infection through a combination of effective interventions (such as optimization of patient risk factors prior to surgery, administering appropriate antimicrobial prophylaxis, skin disinfection, preoperative showering, appropriate hair removal, maintenance of normothermia, wound irrigation, antimicrobial suture wound closure, and post-operative wound care).38,39 Ultimately, such strategies might help improve patient outcomes.
Further Research
To confirm the association and establish causality between anemia and postoperative complications, a larger sample size and longer follow-up study are required. In addition, the heterogeneity between different causes of preoperative anemia, which should be investigated in future studies. Further research is also needed to examine the potential mechanisms by which low preoperative Hb concentrations increase the risk of postoperative complications, determine the optimal perioperative Hb goal for anemic patients that might vary depending on sex and age, and evaluate the effectiveness of treatment strategies and their impact on clinical outcomes, including postoperative complications. These studies will contribute to the development of more robust perioperative management strategies for hip fracture patients with anemia.
Strengthens and Limitations
We conducted a systematic examination of the association between preoperative anemia and major complications in an 18-year longitudinal cohort of 3540 hip fracture patients and provided population-specific estimates. Our study also included stratified analyses of important patient characteristics and found that preoperative anemia significantly increased postoperative complications in patients aged 65 years or older, women, those with femoral neck or intertrochanteric fracture, or aCCI ≥ 3. These findings have practical implications for surgeons in identifying high-risk patients in clinical practice.
This study has limitations. First, this is a single-center observational study; thus, the results might not be generalizable to the broader hip fracture populations or other types of surgeries or patient populations. The study design does not establish causality between anemia and postoperative complications. Second, the study only examined thirteen major postoperative complications, clearly not exhaustive. Other important complications, such as delirium and acute kidney injury were not examined. Third, although the sample size is relatively large, the high number of variables and outcomes analyzed may increase the risk of type I error. Therefore, we advise against over-interpretation of the results of secondary outcomes. Finally, as an observational study, there may be unmeasured confounders, such as intra-operative blood loss and the use of perioperative blood transfusions. To assess the potential impact of such confounding, we calculated E-values, which suggest that substantial unmeasured confounders would be needed to explain away the observed association between preoperative anemia and major postoperative complications.40
Conclusions
Our study confirms that even mild preoperative anemia is significantly associated with major postoperative complications among hip fracture patients. These findings hold important implications for orthopedic surgeons, who can utilize this information to facilitate informed discussion with their patients regarding surgical planning and perioperative care.
Acknowledgments
We thank Mr. Jianchao Liu of the PLA General Hospital for his contribution in data preparation.
Funding Statement
HL received grants support from the Excellent Young Scholars Training Program by the Chinese PLA General Hospital (2020-YQPY-001), Young Elite Scientist Sponsorship Program by Beijing Association for Science and Technology (BYESS2022021). PT received grant support from the National Natural Science Foundation of China (81972102).
Abbreviations
AAOS, American Academy of Orthopaedic Surgeons; aCCI, age adjusted Charlson Comorbidity Index; BMI, Body Mass Index; CI, Confidence Interval; Hb, Hemoglobin; IRR, Incidence Rate Ratio; OR, Odds Ratio; PLA, People’s Liberation Army; PLAGH, People’s Liberation Army General Hospital; RR, Relative Risk.
Data Sharing Statement
Due to patient privacy and Institutional Review Board requirements, the original data cannot be made publicly available. However, summary-level data can be obtained by contacting the corresponding author. Email: houchenlyu@301hospital.com.cn.
Ethics Approval and Informed Consent
This study was approved by the Institutional Review Board of the Chinese PLA General Hospital and conducted in accordance with the Declaration of Helsinki. Patient consent was waived due to the retrospective nature of the study, which involves minimal risk to the patients. Appropriate measures were taken to ensure patient confidentiality and protection of their personal information.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare no conflicts of interest that could bias this work.
References
- 1.Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–2062. doi: 10.1056/NEJMcp1611090 [DOI] [PubMed] [Google Scholar]
- 2.Pradarelli JC, Healy MA, Osborne NH, Ghaferi AA, Dimick JB, Nathan H. Variation in medicare expenditures for treating perioperative complications: the cost of rescue. JAMA Surg. 2016;151(12):e163340. doi: 10.1001/jamasurg.2016.3340 [DOI] [PubMed] [Google Scholar]
- 3.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after Hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Potter LJ, Doleman B, Moppett IK. A systematic review of pre-operative anaemia and blood transfusion in patients with fractured hips. Anaesthesia. 2015;70(4):483–500. doi: 10.1111/anae.12978 [DOI] [PubMed] [Google Scholar]
- 5.Yombi JC, Putineanu DC, Cornu O, Lavand’homme P, Cornette P, Castanares-Zapatero D. Low haemoglobin at admission is associated with mortality after Hip fractures in elderly patients. Bone Joint J. 2019;101-B(9):1122–1128. doi: 10.1302/0301-620X.101B9.BJJ-2019-0526.R1 [DOI] [PubMed] [Google Scholar]
- 6.Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102(11):1314–1324. doi: 10.1002/bjs.9861 [DOI] [PubMed] [Google Scholar]
- 7.Zhang L, Yin P, Lv H, et al. Anemia on admission is an independent predictor of long-term mortality in hip fracture population: a prospective study with 2-year follow-up. Medicine. 2016;95(5):e2469. doi: 10.1097/MD.0000000000002469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Halm EA, Wang JJ, Boockvar K, et al. The effect of perioperative anemia on clinical and functional outcomes in patients with Hip fracture. J Orthop Trauma. 2004;18(6):369–374. doi: 10.1097/00005131-200407000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ. The relationship between admission hemoglobin level and outcome after Hip fracture. J Orthop Trauma. 2002;16(1):39–44. doi: 10.1097/00005131-200201000-00009 [DOI] [PubMed] [Google Scholar]
- 10.Clemmesen CG, Palm H, Foss NB. Delay in detection and treatment of perioperative anemia in Hip fracture surgery and its impact on postoperative outcomes. Injury. 2019;50(11):2034–2039. doi: 10.1016/j.injury.2019.09.001 [DOI] [PubMed] [Google Scholar]
- 11.Jiang Y, Luo Y, Li J, et al. Chronic kidney disease and risk of postoperative cardiovascular events in elderly patients receiving Hip fracture surgery. Injury. 2022;53(2):596–602. doi: 10.1016/j.injury.2021.12.032 [DOI] [PubMed] [Google Scholar]
- 12.Adesina SA, Eyasan SU, Amole IO, et al. Closed reduction and locked intramedullary nailing of diaphyseal long bone fractures without intra-operative imaging and fracture table. Int Orthop. 2022;46(1):51–59. doi: 10.1007/s00264-021-05091-5 [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Carrozzino D, Guidi J, Patierno C. Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom. 2022;91(1):8–35. doi: 10.1159/000521288 [DOI] [PubMed] [Google Scholar]
- 14.Richards T, Baikady RR, Clevenger B, et al. Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. Lancet. 2020;396(10259):1353–1361. doi: 10.1016/S0140-6736(20)31539-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Musallam KM, Tamim HM, Richards T, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378(9800):1396–1407. doi: 10.1016/S0140-6736(11)61381-0 [DOI] [PubMed] [Google Scholar]
- 16.Everett BM, MacFadyen JG, Thuren T, Libby P, Glynn RJ, Ridker PM. Inhibition of interleukin-1b and reduction in atherothrombotic cardiovascular events in the CANTOS trial. J Am Coll Cardiol. 2020;76(14):1660–1670. doi: 10.1016/j.jacc.2020.08.011 [DOI] [PubMed] [Google Scholar]
- 17.Krishna CVM, Rao GA, Anuradha S. Analysing the impact of contextual segments on the overall rating in multi-criteria recommender systems. J Big Data. 2023;10(1):16. doi: 10.1186/s40537-023-00690-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.VanderWeele TJ, Ding P. Sensitivity Analysis in observational research: introducing the E-Value. Ann Intern Med. 2017;167(4):268–274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 19.Spahn DR. Anemia and patient blood management in hip and knee surgery. Anesthesiology. 2010;113(2):482–495. doi: 10.1097/ALN.0b013e3181e08e97 [DOI] [PubMed] [Google Scholar]
- 20.O’Leary L, Jayatilaka L, Leader R, Fountain J. Poor nutritional status correlates with mortality and worse postoperative outcomes in patients with femoral neck fractures: an observational study in a large UK teaching hospital. Bone Joint J. 2021;103-B(1):164–169. doi: 10.1302/0301-620X.103B1.BJJ-2020-0991.R1 [DOI] [PubMed] [Google Scholar]
- 21.Wang T, Guo J, Long Y, Yin Y, Hou Z. Risk factors for preoperative deep venous thrombosis in Hip fracture patients: a meta-analysis. J Orthop Traumatol. 2022;23(1):19. doi: 10.1186/s10195-022-00639-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.You F, Ma C, Sun F, Liu L, Zhong X. The risk factors of heart failure in elderly patients with Hip fracture: what should we care. BMC Musculoskelet Disord. 2021;22(1):1–7. doi: 10.1186/s12891-021-04686-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grosso MJ, Boddapati V, Cooper HJ, Geller JA, Shah RP, Neuwirth AL. The effect of preoperative anemia on complications after total hip arthroplasty. J Arthroplasty. 2020;35(6):S214–S218. doi: 10.1016/j.arth.2020.01.012 [DOI] [PubMed] [Google Scholar]
- 24.Myers E, Grady PO, Dolan AM. The influence of preclinical anaemia on outcome following total hip replacement. Arch Orthop Trauma Surg. 2004;124(10):699–701. doi: 10.1007/s00402-004-0754-6 [DOI] [PubMed] [Google Scholar]
- 25.Bolliger D, Mauermann E, Buser A. Preoperative anaemia in cardiac surgery: preoperative assessment, treatment and outcome. Br J Anaesth. 2022;128(4):599–602. doi: 10.1016/j.bja.2021.12.049 [DOI] [PubMed] [Google Scholar]
- 26.Hazen YJJM, Noordzij PG, Gerritse BM, et al. Preoperative anaemia and outcome after elective cardiac surgery: a Dutch national registry analysis. Br J Anaesth. 2022;128(4):636–643. doi: 10.1016/j.bja.2021.12.016 [DOI] [PubMed] [Google Scholar]
- 27.Jonker FAM, Boele van Hensbroek M. Boele van Hensbroek M. Anaemia, iron deficiency and susceptibility to infections. J Infect. 2014;69:S23–S27. doi: 10.1016/j.jinf.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 28.Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004;104(8):2263–2268. doi: 10.1182/blood-2004-05-1812 [DOI] [PubMed] [Google Scholar]
- 29.Parker MJ. Iron supplementation for anemia after hip fracture surgery: a randomized trial of 300 patients. J Bone Joint Surg. 2010;92(2):265–269. doi: 10.2106/JBJS.I.00883 [DOI] [PubMed] [Google Scholar]
- 30.Moppett IK, Rowlands M, Mannings AM, Marufu TC, Sahota O, Yeung J. The effect of intravenous iron on erythropoiesis in older people with Hip fracture. Age Ageing. 2019;48(5):751–755. doi: 10.1093/ageing/afz049 [DOI] [PubMed] [Google Scholar]
- 31.Bielza R, Llorente J, Thuissard IJ, et al. Effect of intravenous iron on functional outcomes in Hip fracture: a randomised controlled trial. Age Ageing. 2021;50(1):127–134. doi: 10.1093/ageing/afaa107 [DOI] [PubMed] [Google Scholar]
- 32.Farrow L, Brasnic L, Martin C, et al. A nationwide study of blood transfusion in Hip fracture patients: linked analysis from the Scottish hip fracture audit and the Scottish national blood transfusion service. Bone Joint J. 2022;104-B(11):1266–1272. doi: 10.1302/0301-620X.104B11.BJJ-2022-0450.R1 [DOI] [PubMed] [Google Scholar]
- 33.Cata JP, Wang H, Gottumukkala V, Reuben J, Sessler DI. Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions. Br J Anaesth. 2013;110(5):690–701. doi: 10.1093/bja/aet068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Judd L, Hof L, Beladdale L, et al. Prevalence of pre‐operative anaemia in surgical patients: a retrospective, observational, multicentre study in Germany. Anaesthesia. 2022;77(11):1209–1218. doi: 10.1111/anae.15847 [DOI] [PubMed] [Google Scholar]
- 35.Gillies MA, Ghaffar S, Moppett IK, et al. A restrictive versus liberal transfusion strategy to prevent myocardial injury in patients undergoing surgery for fractured neck of femur: a feasibility randomised trial (RESULT-NOF). Br J Anaesth. 2021;126(1):77–86. doi: 10.1016/j.bja.2020.06.048 [DOI] [PubMed] [Google Scholar]
- 36.Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Injuries Group. Cochrane Database Syst Rev. 2016;2016(10):CD002042. doi: 10.1002/14651858.CD002042.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Connor MI, Switzer JA. AAOS clinical practice guideline summary: management of hip fractures in older adults. J Am Acad Orthop Surg. 2022;30(20):e1291–e1296. doi: 10.5435/JAAOS-D-22-00125 [DOI] [PubMed] [Google Scholar]
- 38.Vicentini C, Bordino V, Cornio AR, Canta I, Marengo N, Zotti CM. Surgical site infection prevention through bundled interventions in Hip replacement surgery: a systematic review. Int J Surg. 2021;95:106149. doi: 10.1016/j.ijsu.2021.106149 [DOI] [PubMed] [Google Scholar]
- 39.Edmiston CE, Leaper DJ. Prevention of orthopedic prosthetic infections using evidence-based surgical site infection care bundles: a narrative review. Surg Infect (Larchmt). 2022;23(7):645–655. doi: 10.1089/sur.2022.146 [DOI] [PubMed] [Google Scholar]
- 40.Ioannidis JPA, Tan YJ, Blum MR. Limitations and misinterpretations of e-values for sensitivity analyses of observational studies. Ann Intern Med. 2019;170(2):108. doi: 10.7326/M18-2159 [DOI] [PubMed] [Google Scholar]