Abstract
Purpose
Based on the interpersonal theory of depression and resilience framework theory, this study tested the association between interpersonal sensitivity and depression in college students in the context of the COVID-19 pandemic. Additionally, the mediating role of resilience and the moderating role of the COVID-19 lockdown were investigated.
Methods
A total of 5193 South Chinese college students (M=19.27, SD = 1.18) were included in the study. According to which campus they were living on, the subjects were categorized as members of a lockdown group or a nonlockdown group. They completed the interpersonal sensitivity subscales of the Symptom Checklist 90 (SCL-90), Beck Depression Inventory (BDI), and Connor-Davidson Resilience Scale (CD-RISC). SPSS 26.0 statistical software was used to analyse the descriptive statistics, reliability, and correlation. Specifically, a moderated mediation model was analysed by multivariate logistic regression.
Results
Interpersonal sensitivity was significantly associated with depression (r = 0.517, p < 0.01), which was mediated by resilience (β = 0.12, 95% CI = [0.10, 0.13]). Lockdown status was shown to have a moderating effect on the relationship between resilience and depression (β = 0.03, t = 2.71, p < 0.01).
Conclusion
The high levels of interpersonal sensitivity displayed by South Chinese college students caused low resilience and then facilitated depression. The COVID-19 lockdown strengthened the effect of low resilience on depression. Lower resilience was more strongly associated with higher depression for students under lockdown conditions compared to students who were not in lockdown.
Keywords: interpersonal sensitivity, depression, resilience, lockdown, COVID-19
Introduction
To protect citizens during the COVID-19 pandemic, many local governments announced specific orders, such as self-isolation, quarantine for 14 days, stay-at-home orders, and lockdown.1 In some areas where the epidemic was severe or countries with strict policies, entertainment venues and even schools went into lockdown for an extended period. These situations greatly affected the mental and physical disorders of people of different age groups. Previous studies reported upwards trends during COVID-19 in children’s anxiety regarding physical injuries and being separated from parents,2 young female adults’ depression and headache symptoms,3 and elderly adults’ cognitive and psychological health deficiencies.4 Among these, the worsening of depression in young people has attracted our attention. A survey conducted before the COVID-19 pandemic showed that less than 16.2% of university students reported experiencing depressive symptoms.5 Surprisingly, research studying college students’ prevalence of depression in the context of the COVID-19 pandemic reported that the detection rate of depression increased to 48.14% in the US6 and 22% in China,7 with 37% being the worldwide average.8
Depression and Interpersonal Sensitivity
Depression is a severe mood disorder that causes a person to be irritable, in a state of constant sadness, and lack interest in anything.9 Depression gained increasing attention from mental health and social care professionals and researchers during the COVID-19 pandemic period.10 A cross-sectional study that surveyed respondents in five countries during the COVID-19 pandemic indicated that the prevalence of depression was higher than that of other negative mental symptoms, such as anxiety and stress.11 Santomauro et al noted that the human epidemic infection rate of COVID-19 was significantly correlated with the prevalence of major depressive disorder.12 A longitudinal study conducted among undergraduate students showed that students experienced worse levels of depressive symptoms during the COVID-19 pandemic compared to the situation before the pandemic.13 Therefore, a focus on young people’s depressive statuses during COVID-19 is essential.
Interpersonal sensitivity is an essential factor that attracts great attention when studying individual depression. It represents the ability and extent to which people are overly sensitive and respond to individual behaviours and feelings, social interactions, and the surrounding environment.14–16 The essence of interpersonal sensitivity is the level to which people care intemperately about their interpersonal relationships and fear being rejected or criticized by others so that those with high interpersonal sensitivity have greater chances of suffering from deficient social interactions and interpersonal stress.17,18 During COVID-19, many social events outside the campus were cancelled, and people were asked to engage in social distancing. Accordingly, people’s levels of interpersonal stress increased.19
Empirical and theoretical studies have provided reliable evidence supporting the direct connection between interpersonal sensitivity and depression. From the practical side, various studies have found that high interpersonal sensitivity is positively related to individual depression.18,20 From the theoretical perspective, according to the interpersonal theory of depression, different deficient interpersonal characteristics, such as interpersonal rejection sensitivity, strengthen individual depression vulnerability.21 Considering that the pandemic influenced both aspects related to people’s interpersonal sensitivity and mental health, we aim to verify the link between interpersonal sensitivity and depression again in the context of the COVID-19 pandemic. We propose that interpersonal sensitivity is positively associated with depression and significantly predicts depression in the context of the COVID-19 pandemic.
Mediating Role of Resilience
Resilience is defined as the ability to withstand stress, bounce back, maintain a stable balance in a situation, and actively adapt to the challenges of a living environment disrupted by adversity.22,23 Referring to a large number of viewpoints on resilience, resilience can be understood through the following three aspects: traits, processes, and outcomes. From the perspective of traits, resilience is a relatively stable ability to quickly and easily recover from adversity.24 From the processing perspective, resilience is viewed as a “dynamic process” in which individuals use their resources to resist and thus maintain the ability to adapt and recover easily.25 In terms of results, resilience is also viewed as the strength to achieve functional recovery, positive behavioural outcomes, and even positive socioeconomic changes in the face of a health crisis.26
Resilience may be an explanatory mechanism through which interpersonal sensitivity affects individual depression. From our conceptual knowledge, resilience is a unique positive psychological resource and quality.27 Researchers have suggested that the internal resources that young individuals possess contribute to lowering their levels of interpersonal sensitivity and alleviating their symptoms of depression.18 Some empirical evidence directly indicates the mediating role of resilience in the relationship among various negative factors, such as fear of COVID-19, envy, bullying experiences, and depression.28–30 Resilience framework theory suggests that low psychological resilience interacting with environmental factors might influence an individual’s adaptation ability and possibly induce depression.31,32 Overall, based on the existing hypothesis of interpersonal sensitivity affecting depression, we propose that resilience partly mediates the influence of interpersonal sensitivity on depression.
The Moderating Role of Lockdown
Lockdown refers to a policy or an order put forwards by the local governments to block the use of a place in response to an urgent and serious situation, such as shutting down a school, an entertainment venue, or an amusement park.33 As COVID-19 spread worldwide, many cities and countries hit by the epidemic implemented lockdown measures, completely banning entry and exit from areas to strengthen control of the epidemic. For the group of Chinese college students we target in the current study, the most common COVID-19 epidemic experience involved the students being locked on campus by the universities to ensure that they were isolated from the pandemic risk that may exist in the outside world. They were usually forbidden to leave the campus, and all learning, living, and entertainment were restricted to areas on campus. Thus, we will use the term “lockdown” throughout the article to represent the situation that they experienced.
As an external factor that occurred during the COVID-19 pandemic, lockdowns may have influenced people’s inner experiences differently.34 Researchers have suggested that the basic function of interpersonal sensitivity is related to experiencing and interacting with the circumstances.16 This implies that lockdowns may have influenced interpersonal sensitivity. In addition, resilience framework theory highlights the interacting effects of the external environment and how resilience could affect people’s adaptive ability,31 which reveals the corresponding moderating role of environmental changes on resilience affecting individuals’ adaptive outcomes. Moreover, a number of studies conducted during the COVID-19 period reported that people who were in lockdown exhibited more negative mental symptoms, such as depressed mood, insomnia, anxiety, and depression.35,36 In summary, we hypothesize that the COVID-19 lockdown may have a moderating effect on the path of interpersonal sensitivity-resilience, the path of resilience-depression, and even the path of interpersonal sensitivity-depression.
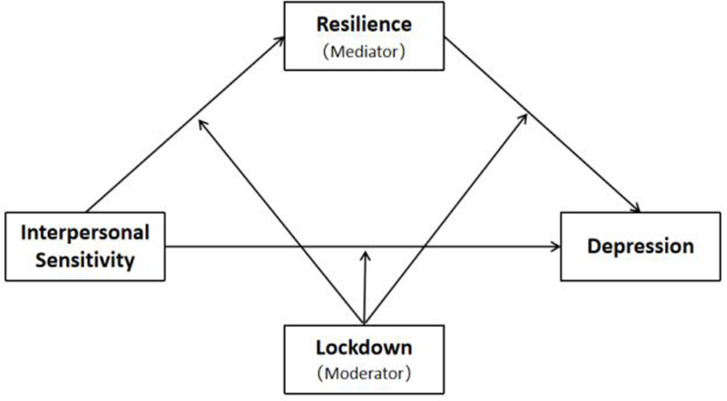
People in different countries, or even in different regions of the same country, might have experienced different lockdown policies. Some have been through prolonged lockdown periods, while others have not. It is worth exploring whether the external factor of experiencing a lockdown will generate different impacts on people’s internal states, such as depressive status and resilience. In addition, interpersonal sensitivity is believed to be a risk factor for depression, but no studies have verified this association during the COVID-19 pandemic. Additionally, the mechanisms concerning the relationship between interpersonal sensitivity and depression remain elusive and need to be explored further. To address these research gaps, the present study aimed to test the relationship between interpersonal sensitivity and depression in the specific context of the COVID-19 pandemic. Based on the interpersonal theory of depression and resilience framework theory, the mediating and moderating mechanisms of the relationship were examined from the perspective of the internal factor (resilience) and the external factor (lockdown) among Chinese college students. The conceptual framework of the current study is shown in Figure 1. We aim to test the following hypotheses:
Hypothesis 1: Interpersonal sensitivity is positively associated with depression and significantly predicts depression in the context of the COVID-19 pandemic.
Hypothesis 2: Resilience partly mediates the influence of interpersonal sensitivity on depression.
Hypothesis 3: The COVID-19 lockdown has had a moderating effect on the relationships between interpersonal sensitivity and resilience, resilience and depression, and interpersonal sensitivity and depression.
Figure 1.
The conceptual model of the study.
Materials and Methods
Participants and Procedures
We implemented the research in November 2020, when the first batch of college students commenced their studies at the university after the outbreak of the COVID-19 pandemic around the world. Convenience sampling was adopted in this study. We invited all first-year students at Guangxi International Business Vocational College, South China, to participate in the study. The homogeneity of the subjects was well controlled. The current study was also part of this university’s freshmen mental health screening survey. This screening survey was similar to a course for first-year college students and aimed at screening out students with serious mental illnesses so that the university could provide specific interventions for them. Students were informed about the purpose of the survey, in accordance with the Declaration of Helsinki. In the case that a serious mental illness was detected, well-trained psychology teachers intervened to provide the appropriate help. The screening survey was approved by the university’s administration and supported by the educational department of China.
We shared online links and QR codes with representatives of all the academic departments of the university. Then, they organized all the class instructors to arrange for students to fill in the questionnaires by directly using their smartphones’ instant message feature to click the online links or scan the QR codes. Every first-year student was successfully informed of the survey and invited to participate. The class instructors told the students about the test’s aim, voluntary nature, and confidentiality. If they agrees to participate, they were informed that they should complete the questionnaires within a specific time slot (within 2–3 days). Finally, 5326 college students completed the questionnaires.
Measures
Interpersonal Sensitivity
Interpersonal sensitivity was measured by a subscale of the Symptom Checklist 90 (SCL-90).37 The SCL-90, which has been found to have high reliability and validity, has been widely used in the testing of mental symptoms, such as anxiety, hostility, obsessive-compulsive, depression, and interpersonal sensitivity, in individuals. The interpersonal sensitivity subscale includes 9 items that are rated on a five-point scale (1 = no; 5 = severe). The Cronbach’s alpha of the subscale in this study is 0.84, which indicates a high reliability of this scale.
Depression
Depression was assessed by the popular Beck Depression Inventory (BDI), which was developed by the American psychologist Beck.38 The scale consists of 21 items that represent various symptoms of and attitude types related to depression, such as the sense of failure, lack of satisfaction, sleep disturbance, and fatigue. Each item consists of 4 options, and the options are ordered by symptom severity. That is, participants are asked to choose one of these descriptions, and their answers are recorded on a 4-point scale, where a larger number indicates more severe depression in the participant. The Cronbach’s alpha of BDI tested here is 0.86, indicating high reliability.
Resilience
Connor and Davidson developed the Connor-Davidson Resilience Scale (CD-RISC) to test the level of resilience displayed by individuals.39 The scale was revised by Yu and Zhang in Chinese and verified to have high reliability and validity.40 We used the Chinese CD-RISC in this study. It contains 25 items. Participants were asked to rate their agreement with these statements on a five-point scale (0=never; 4=all the time). The Cronbach’s alpha of the CD-RISC in this study is 0.94, which indicates a very high reliability of this scale.
Lockdown
“Lockdown or not” in this study was measured not by a scale but by the campus zone in which participants lived. The participating university in this study consists of two campuses: one in City N and the other in City F. Students are admitted to either campus according to their majors. The distance between the two cities is only 143.1 kilometres, but implemented different COVID-19 epidemic prevention policies due to political, geographical, and other reasons. Participants began their studies on these two campuses in September 2020 and participated in the current research in November 2020. During these two months, the university issued a strict lockdown order to the students attending campus F beginning at the time that the students reached the campus due to the serious epidemic situation in City F. According to this order, students were not allowed to leave campus without special reasons and multiple levels of approval, so students were isolated from the outside campus environment. Based on the definition of lockdown,33 we defined the case of students living in such an isolated situation for 2 months as experiencing a lockdown in this study. Conversely, this order did not apply to campus N, so students attending this campus could enter or leave the campus freely. They were free to interact with the environment outside the campus during these 2 months. Thus, we termed this situation on the campus N nonlockdown.
Data Analysis
The data of 5326 participants were computed and imported into IBM SPSS version 26. First, we removed those participants whose data in those three measurements went beyond the mean±3SD to ensure data authenticity and reliability.41 Second, Harman’s single-factor approach was used to test common method deviation in this study.42 Third, we conducted Pearson correlations to examine the relationships among lockdown, interpersonal sensitivity, resilience, and depression. Fourth, we used Hayes’ PROCESS macro (Model 4, Model 59, Model 14) to examine the proposed moderated mediation model.43 Finally, we conducted a simple slope analysis to clarify how the lockdown situation influenced the link between resilience and depression and adopted a simple effect test to conduct an additional analysis of how the interaction between resilience and lockdown influenced students’ depression.
Results
Control and Verification of Common Method Variance
We used Harman’s single-factor approach to test common method deviation in the current study. The results suggested that there were eight factors with eigenvalues greater than one. The mutation rate interpretation of the first factor was 24.12%, which is less than 40%. Therefore, we claim that the study does not have common method variance.
Descriptive Statistics
Regarding the data collected from the 5326 participants, we calculated and removed those participants whose data in those three measurements went beyond mean±3SD. Finally, we excluded 82 participants with extreme values on the interpersonal sensitivity test, 11 participants with extreme values on the resilience test, and 40 participants with extreme values on the depression test. As a result, 5193 participants (63% females, 37% males; age mean = 19.27, age SD = 1.18) were included in this study’s following analysis.
The relationships among lockdown, interpersonal sensitivity, resilience, and depression were tested using Pearson correlations. The means, standard deviations (SDs), and the correlation matrix for all the variables are shown in Table 1. We found that lockdown, interpersonal sensitivity, resilience, and depression were significantly related to each other (p < 0.01). Specifically, the significant-positive association between interpersonal sensitivity and depression supported Hypothesis 1.
Table 1.
Descriptive Statistics and Associations Among the Variables (N=5139)
| Variables | M | SD | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1 | Gender | — | — | ||||
| 2 | Age | 19.27 | 1.18 | ||||
| 3 | Lockdown | 1.59 | 0.49 | 1 | |||
| 4 | Interpersonal sensitivity | 15.15 | 4.87 | 0.068** | 1 | ||
| 5 | Resilience | 55.49 | 17.65 | 0.01 | −0.349** | 1 | |
| 6 | Depression | 8.00 | 7.59 | −0.018 | 0.517** | −0.366** | 1 |
Note: **p < 0.01.
Testing for Mediating Effects
We use Hayes’ PROCESS macro (Model 4) to test the mediating effect of resilience on the relationship between interpersonal sensitivity and depression.43 We chose 5000 bootstrap samples and 95% confidence intervals. As expected, interpersonal sensitivity could directly predict depression (β = 0.69, t = 35.99, p < 0.001, CI = [0.66, 0.73]), which verified Hypothesis 1 again. In addition, interpersonal sensitivity negatively predicted resilience (β = −1.27, t = −26.84, p < 0.001, CI = [−1.36, −1.17]), and resilience also showed a significant negative predictive effect on depression (β = −0.09, t = −17.07, p < 0.001, CI = [−0.10, −0.08]). In summary, resilience played a partial mediating role in the association between interpersonal sensitivity and depression. The mediated predicting effect (β = 0.12) and direct predicting effect (β = 0.69) accounted for 14.9% and 85.1%, respectively, of the overall effect (shown in Table 2). Thus, the results supported Hypothesis 2.
Table 2.
Mediating Analysis of the Relationship Between Interpersonal Sensitivity and Depression (N=5139)
| Effect | se | Proportion | LLCI | ULCI | |
|---|---|---|---|---|---|
| Direct | 0.69*** | 0.02 | 85.1% | 0.66 | 0.73 |
| Indirect | 0.12*** | 0.01 | 14.9% | 0.10 | 0.13 |
| Total | 0.81*** | 0.02 | 0.77 | 0.84 |
Note: ***p < 0.001.
Testing for Moderated Mediation
Then, consistent with our hypothetical model, we employed the PROCESS macro (Model 59) to examine the moderated mediation. A total of 5000 bootstrap samples and 95% confidence intervals were used in the data analysis. The results varied from those hypothesized. The interaction between interpersonal sensitivity and lockdown could not significantly predict resilience (Interpersonal sensitivity × Lockdown: β = 0.15, t = 1.52, p > 0.05) and was not a significant predictor of depression (Interpersonal sensitivity × Lockdown: β = −0.01, t = −0.22, p > 0.05). However, the interaction between resilience and lockdown significantly predicted depression (Resilience × Lockdown: β = 0.03, t = 2.46, p < 0.05). The results indicated that lockdown only moderated the mediating path of resilience affecting depression.
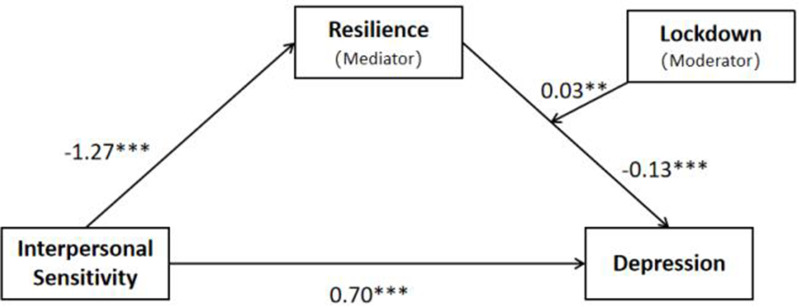
To test the moderated mediation effect more precisely, we used Model 14 (Model 14 only moderates the second stage of the mediation model, which is consistent with our preliminary analysis results) in the SPSS extension macro to analyse the data again. The final results are listed in Table 3. In Model 1, we treated resilience as the criterion in the regression analysis and verified again that interpersonal sensitivity was a significant predictor of resilience (β= −1.27, t = −26.84, p < 0.001, CI = [−1.36, −1.17]). After adding lockdown into the model (Model 2), we found a significant effect of resilience on depression (β = −0.13, t = −7.98, p < 0.001, CI = [−0.17, −0.10]), which was moderated by lockdown (β = 0.03, t = 2.71, p < 0.01, CI = [0.01, 0.05]). The final model proved by the current study is depicted in Figure 2.
Table 3.
Testing the Moderated Mediation Effect of Interpersonal Sensitivity on Depression (N=5139)
| Predictors | Model 1 (Resilience) | Model 2 (Depression) | ||||
|---|---|---|---|---|---|---|
| β | t | 95% CI | β | t | 95% CI | |
| Interpersonal sensitivity | −1.27 | −26.84*** | [−1.36, −1.17] | 0.70 | 36.28*** | [0.66, 0.74] |
| Lockdown | −2.22 | −3.80*** | [−3.36, −1.08] | |||
| Resilience | −0.13 | −7.98*** | [−0.17, −0.10] | |||
| Resilience×Lockdown | 0.03 | 2.71** | [0.01, 0.05] | |||
| R² | 0.12 | 0.31 | ||||
| F | 720.35*** | 581.94*** | ||||
Notes: **p < 0.01; ***p < 0.001.
Figure 2.
The final model of the association between interpersonal sensitivity and depression: the mediating role of resilience and the moderating role of lockdown. (N=5139; **p < 0.01; ***p < 0.001.).
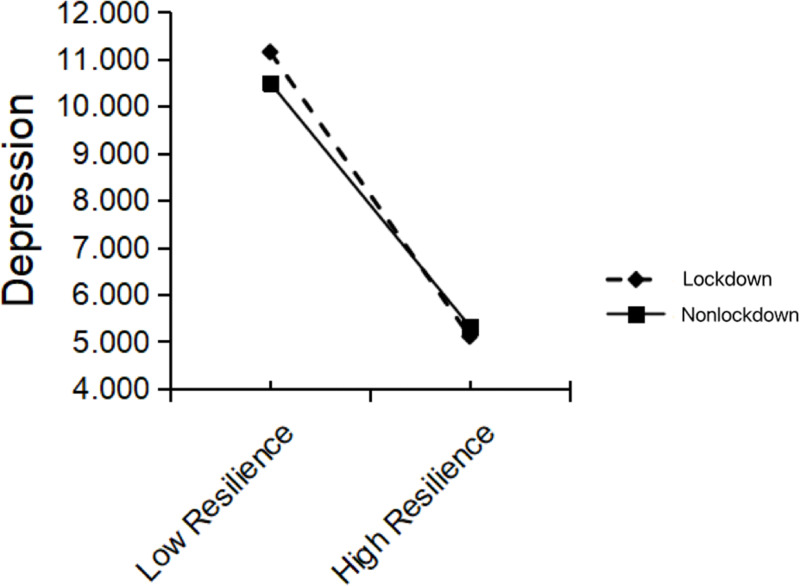
To clarify how lockdown influenced the link between resilience and depression, we conducted a simple slope analysis and visualized the results in Figure 3. The simple slope test results indicated that higher resilience was more strongly associated with lower depression for the students who were in lockdown during COVID-19 compared to those who were not in lockdown during COVID-19 (in lockdown: βsimple = −0.17, p < 0.001; not in lockdown: βsimple = −0.15, p < 0.001). Namely, compared to students who were not in lockdown, the effect of resilience on depression was more substantial among those who were experiencing lockdown. Hence, the data indicated that lockdown could strengthen the link between low resilience and depression.
Figure 3.
The moderating effect of lockdown. Low-level resilience and high-level resilience refer to 1 SD below and above the mean, respectively. The continuous data of resilience were mean-centered first before the analysis.
To further understand how the interaction of resilience and lockdown influenced students’ depression, we adopted a simple effect test to perform additional analysis. The simple effect test results showed that compared to college students with high-level resilience, college students with low-level resilience exhibited more depression during the lockdown than they did when not under lockdown (F(1, 3490)=5.72, p < 0.05). However, for the students who had high-level resilience, depression did not change significantly when under lockdown (F(1, 3490)=1.22, p > 0.05). Therefore, the results showed that low-level resilience could also strengthen the relationship between the COVID-19 lockdown and depression.
Discussion
The Positive Association Between Interpersonal Sensitivity and Depression
As expected, college students with higher levels of interpersonal sensitivity might be more likely to suffer from depression. The significant relationship found here was consistent with previous research findings that interpersonal sensitivity acts as an essential risk factor for depressive symptoms.44–47 Additionally, depressed individuals expressed higher interpersonal sensitivity levels than those without depressive symptoms.14 For young people, the university period is a vital transition from adolescence to adulthood. Individuals at this stage are highly sensitive to interpersonal relationships because they need rich interpersonal interactions, such as peer communication, to strengthen their sense of identity.48 Coyne indicated that people with high interpersonal sensitivity levels tend to engage in interpersonal avoidance and experience deficits in social interactions.21 These adverse interpersonal experiences may cause them to have more negative beliefs about themselves, which may accordingly strengthen their depressive symptoms.47
In this COVID-19 pandemic setting, college students’ learning mode has changed from face-to-face to online courses. Most social activities have been banned, and interpersonal relationships have become more alienated. Students may even be confined to campus due to lockdown orders, so they have limited interpersonal contact. These impaired interpersonal relations may induce depression in individuals.49 In addition, the interpersonal theory of depression indicates the following four specific aspects that facilitate depression in an individual: loss of significant others, life changes, interpersonal conflicts, and deficits.50 Therefore, during the COVID-19 pandemic, students with high levels of interpersonal sensitivity may experience more severe interpersonal stress because of life changes and feel deeper depression. Our results empirically validate this theory and show that it is equally applicable to explain the relationship between interpersonal sensitivity and depression during COVID-19.
The Mediating Role of Resilience and the Moderating Role of the COVID-19 Lockdown
Our finding from the mediating model supported the hypothesis that resilience negatively mediated the relationship between interpersonal sensitivity and depression, consistent with previous studies.28–30 People with high interpersonal sensitivity levels are cautious and show low self-esteem in interpersonal relationships.37 They may encounter more difficulties in interpersonal communication and underperform in handling dilemmas. The lack of the ability to solve difficulties smoothly and recover from them quickly is a typical symptom of poor resilience.51 College students usually attempt to build solid interpersonal resources through social interactions and finally strengthen their resilience.18,52 However, if a person fails to increase his interpersonal resources and instead shows difficulties in social interactions, the individual may have poor psychological resilience.
The conservation of resources theory (COR) highlights that scarce personal resources might lead to negative consequences for individuals, such as depression.53 Low resilience is a severe risk factor for depression because individuals with low resilience have difficulty recovering from poor behavioural outcomes and feelings of sadness.54 Similarly, researchers have proposed that high resilience acts as a protective factor for depression and a positive factor that reduces the likelihood of adverse mental health outcomes.55 Moreover, resilience framework theory also supports the mediating effect of resilience by introducing a close causal relationship between resilience and depression influenced by the COVID-19 pandemic.31,32 In other words, during the COVID-19 pandemic period, college students with high interpersonal sensitivity levels might experience worse depressive symptoms due to their poor resilience.
Our results also found that the COVID-19 lockdown moderated the effect of resilience on depression. Specifically, compared to those who were not experiencing lockdown, lower levels of resilience were more closely associated with higher levels of depression for college students who were in lockdown. According to resilience framework theory, the interacting effects of resilience and environmental contexts may work together to affect people’s ability to adapt.31 In the frustrating epidemic context, students who have lower levels of resilience will have more difficulty dealing with the unexpected and annoying issues caused by lockdown, such as academic stress simultaneously instituted due to changes in studying styles,56 and feelings of loneliness caused by the cessation of social activities.57 All of the adverse behavioural outcomes and negative emotional states contribute to a high likelihood of increasing an individual’s vulnerability toward depression.58 However, those with higher levels of resilience might exhibit better problem-solving skills to deal with the difficulties caused by the lockdown and recover from depressive emotions sooner. This would explain why the current results show that students with high resilience might not exhibit worse depression due to lockdown. According to these results, attention should be given to low-resilience students experiencing lockdown or quarantine. Potential measures and help to prevent depression are needed for this group.
The present study also found an unexpected result that lockdown did not show moderating effects on the paths of interpersonal sensitivity affecting resilience and depression. This phenomenon could be explained by the stable trait of interpersonal sensitivity.24 As researchers proposed, interpersonal sensitivity was a depression-prone personality trait,59 and depressed individuals were associated with a particular characteristic of being interpersonally sensitive to life stressors.45 This evidence indicated that depression and interpersonal sensitivity might share some common underlying traits. In addition, Boyce et al suggested that the association between interpersonal sensitivity and depression was partly due to genetics. Thus, the relationship was firm and not easily influenced by external factors, including the early parental environment.60 Interpersonal relationships are so crucial for college students that a deficiency in interpersonal competence will greatly hurt young people’s feelings and make it difficult for them to solve the problems they are facing,61 finally causing low psychological resilience.52 Although external environmental factors can influence individual inner factors, our findings showed that the external factor of the COVID-19 lockdown was not strong enough to generate effects on the relationship between interpersonal sensitivity and resilience or the relationship between interpersonal sensitivity and depression.
Implications
The present research yielded interesting results, making a meaningful contribution to the literature and public policy recommendations. First, the significant association between interpersonal sensitivity and depression verified the interpersonal theory of depression through empirical data and tested its validation in the special context of the COVID-19 pandemic. Interpersonal therapy has been widely practised to reduce depression,62 and this study accordingly proved it to be theoretically valuable and essential. The resilience framework theory was also demonstrated by the interaction between resilience and lockdown. Second, the moderating effect of lockdown on the path of resilience affecting depression can provide guidance for social policies. To reduce mental illness during a pandemic, especially depressive symptoms, government authorities can conduct various activities to improve their resilience, such as online resilience intervention programs.63 At the same time, leaders of schools or organizations should pay attention to groups with low resilience and help them if the cities or regions they live in are implementing lockdown orders. This will contribute to preventing depression among individuals during the COVID-19 pandemic period.
Limitations and Future Directions
It is essential to clarify some limitations of this study. First, there is a lack of a precise operational definition of a lockdown. According to the actual situation that the participants experienced, this study categorized the experience of school lockdown for two months in City F as a “lockdown” and defined the experience of free access to campus in City N as “nonlockdown”. However, this definition is not strictly academic and lacks standards. Second, lockdown is a type of policy that the government or executive branch implements. Several subsequent factors behind the lockdown may account for the connection between interpersonal sensitivity, resilience, and depression, for instance, trust in government, social distancing, loneliness, and anxiety. Future studies related to exploring these personal factors will help us learn further about the influence of COVID-19 on our behavioural consequences and mental symptoms. Third, the subjects in the current study were mainly first-year students concentrated in one university. Future work needs to be verified in diverse populations to ensure the generalization of the findings.
Conclusion
The current study is among the first to test the association among interpersonal sensitivity, resilience, and depression in the context of the COVID-19 pandemic among college students in South China. The moderating effect of lockdown in the research model has also been tested. The results suggested that South Chinese college students’ resilience mediated the relationship between interpersonal sensitivity and depression. Lockdown was a significant moderator facilitating the effects of low resilience on depression. The study contributes to extending the theoretical literature, such as the interpersonal theory of depression and resilience framework theory, with empirical evidence and provides academic support for alleviating depressive symptoms through interpersonal therapies. Additionally, the findings highlight the importance of cultivating people’s resilience to keep them safe from depression, especially for those who experience a lockdown.
Funding Statement
This research was supported by the 2020 Guangxi Basic Research Ability Improvement Project for Young and Middle-aged Teachers at University (Project Number: 2020KY38011).
Ethics Approval
The study was part of the freshmen mental health screening survey, which was approved by the Student Affairs Office of Guangxi International Business Vocational College (Student Affairs Office [2020] No. 61). Consent was obtained by participants prior to study commencement.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Emodi-Perlman A, Eli I, Uziel N, et al. Public concerns during the COVID-19 lockdown: a multicultural cross-sectional study among internet survey respondents in three countries. J Clin Med. 2021;10(8):1577. doi: 10.3390/jcm10081577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kevser K, Yucel G. Anxiety and harmful oral habits in preschool children during the 2020 first-wave COVID-19 lockdown in Turkey. Dent Med Probl. 2021;58(4):433–439. doi: 10.17219/dmp/142284 [DOI] [PubMed] [Google Scholar]
- 3.Wieckiewicz M, Danel D, Pondel M, et al. Identification of risk groups for mental disorders, headache and oral behaviors in adults during the COVID-19 pandemic. Sci Rep. 2021;11(1):10964. doi: 10.1038/s41598-021-90566-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richardson SJ, Carroll CB, Close J, et al. Research with older people in a world with COVID-19: identification of current and future priorities, challenges and opportunities. Age Ageing. 2020;49(6):901–906. doi: 10.1093/ageing/afaa149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liang J, Zhang X, Wang J, et al. Mental health status of college freshmen and influencing factors. Psychology. 2020;11(05):737–747. doi: 10.4236/psych.2020.115050 [DOI] [Google Scholar]
- 6.Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. doi: 10.2196/22817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Y, Bao X, Yan J, Miao H, Guo C. Anxiety and depression in Chinese students during the COVID-19 pandemic: a meta-analysis. Front Public Health. 2021;9:697642. doi: 10.3389/fpubh.2021.697642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C, Wen W, Zhang H, et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: a systematic review and meta-analysis. J Am Coll Health. 2021:1–8. doi: 10.1080/07448481.2021.1960849 [DOI] [PubMed] [Google Scholar]
- 9.Horwitz AV, Wakefield JC. The Loss of Sadness: How Psychiatry Transformed Normal Sorrow into Depressive Disorder. Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- 10.Pollock A, Campbell P, Cheyne J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Effective Practice and Organisation of Care Group, ed. Cochrane Database Syst Rev. 2020;2020(11). doi: 10.1002/14651858.CD013779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al Omari O, Al Sabei S, Al Rawajfah O, et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an online cross-sectional multicountry study. Depress Res Treat. 2020;2020:1–9. doi: 10.1155/2020/8887727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020;15(7):e0236337. doi: 10.1371/journal.pone.0236337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boyce P, Parker G. Development of a scale to measure interpersonal sensitivity. Aust N Z J Psychiatry. 1989;23(3):341–351. [PubMed] [Google Scholar]
- 15.Davidson J, Zisook S, Giller E, Helms M. Symptoms of interpersonal sensitivity in depression. Compr Psychiatry. 1989;30(5):357–368. doi: 10.1016/0010-440X(89)90001-1 [DOI] [PubMed] [Google Scholar]
- 16.Hall JA, Bernieri FJ. Interpersonal Sensitivity: Theory and Measurement. Psychology Press; 2001. [Google Scholar]
- 17.Luo Y, Shi Z, Zhang B, Peng Y, Zhang A, Zeng Y. Interpersonal sensitivity and social avoidance and distress in female college students: mediating role of self-inconsistency and moderating role of self-consciousness. J Psychol Afr. 2021;31(3):219–225. doi: 10.1080/14330237.2021.1927342 [DOI] [Google Scholar]
- 18.Xu H, Peng L, Wang Z, Zeng P, Liu X. Interpersonal sensitivity on college freshmen’s depression: a moderated moderation model of psychological capital and family support. Front Psychiatry. 2022;13:921045. doi: 10.3389/fpsyt.2022.921045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dickey L, West M, Pegg S, Green H, Kujawa A. Neurophysiological responses to interpersonal emotional images prospectively predict the impact of COVID-19 pandemic–related stress on internalizing symptoms. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(9):887–897. doi: 10.1016/j.bpsc.2021.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCabe RE, Blankste KR, Mills JRS. Interpersonal sensitivity and social problem-solving: relations with academic and social self-esteem, depressive symptoms, and academic performance. Cogn Ther Res. 1999;23(6):587–604. [Google Scholar]
- 21.Coyne JC. Depression and the response of others. J Abnorm Psychol. 1976;85(2):186–193. doi: 10.1037/0021-843X.85.2.186 [DOI] [PubMed] [Google Scholar]
- 22.Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. Eur Psychol. 2013;18(1):12–23. doi: 10.1027/1016-9040/a000124 [DOI] [Google Scholar]
- 23.Rutter M. Resilience: some conceptual considerations. J Adolesc Health. 1993;14(8):626–631. doi: 10.1016/1054-139X(93)90196-V [DOI] [PubMed] [Google Scholar]
- 24.Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J Pers Soc Psychol. 2006;91(4):730–749. doi: 10.1037/0022-3514.91.4.730 [DOI] [PubMed] [Google Scholar]
- 25.Windle G. What is resilience? A review and concept analysis. Rev Clin Gerontol. 2011;21(2):152–169. doi: 10.1017/S0959259810000420 [DOI] [Google Scholar]
- 26.Khanlou N, Wray R, Whole Community A. Approach toward Child and Youth Resilience Promotion: a Review of Resilience Literature. Int J Ment Health Addict. 2014;12(1):64–79. doi: 10.1007/s11469-013-9470-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ding J, Jia Y, Zhao J, Yang F, Ma R, Yang X. Optimizing quality of life among Chinese physicians: the positive effects of resilience and recovery experience. Qual Life Res. 2020;29(6):1655–1663. doi: 10.1007/s11136-020-02414-8 [DOI] [PubMed] [Google Scholar]
- 28.Chen Y, Liu Y, Zhang Y, Li Z, Zhou T. The effect of fear of the COVID-19 on depression among Chinese outbound students studying online in China Amid the COVID-19 pandemic period: the role of resilience and social support. Front Psychol. 2021;12:750011. doi: 10.3389/fpsyg.2021.750011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin LY, Chien YN, Chen YH, Wu CY, Chiou HY. Bullying experiences, depression, and the moderating role of resilience among adolescents. Front Public Health. 2022;10:872100. doi: 10.3389/fpubh.2022.872100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiang Y, Dong X, Zhao J. Effects of envy on depression: the mediating roles of psychological resilience and social support. Psychiatry Investig. 2020;17(6):547–555. doi: 10.30773/pi.2019.0266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson DR, Adger WN, Brown K. Adaptation to environmental change: contributions of a resilience framework. Annu Rev Environ Resour. 2007;32(1):395–419. doi: 10.1146/annurev.energy.32.051807.090348 [DOI] [Google Scholar]
- 32.Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord. 2010;126(3):411–414. doi: 10.1016/j.jad.2010.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Armbruster S, Klotzbücher V. Lost in lockdown? COVID-19, social distancing, and mental health in Germany; 2020. Available from: https://www.econstor.eu/handle/10419/218885. Accessed October 22, 2022.
- 34.Xi Y, Xu Y, Wang Y. Too-much-of-a-good-thing effect of external resource investment—a study on the moderating effect of psychological capital on the contribution of social support to work engagement. Int J Environ Res Public Health. 2020;17(2):437. doi: 10.3390/ijerph17020437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Panchal U, Salazar de Pablo G, Franco M, et al. The impact of COVID-19 lockdown on child and adolescent mental health: systematic review. Eur Child Adolesc Psychiatry. 2021. doi: 10.1007/s00787-021-01856-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Derogatis LR, Rickels K, Rock AF. The SCL-90 and the MMPI: a step in the validation of a New Self-Report Scale. Br J Psychiatry. 1976;128(3):280–289. doi: 10.1192/bjp.128.3.280 [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Alford BA. Depression: Causes and Treatment. University of Pennsylvania Press; 2009. [Google Scholar]
- 39.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 40.Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Personal Int J. 2007;35(1):19–30. doi: 10.2224/sbp.2007.35.1.19 [DOI] [Google Scholar]
- 41.Zhang H, Xu J. Modern Psychology and Educational Statistics. 3rd ed. Beijing Normal University Press; 2009. [Google Scholar]
- 42.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 43.Bolin JH. Hayes, Andrew F. (2013). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: the Guilford Press. J Educ Meas. 2014;51(3):335–337. doi: 10.1111/jedm.12050 [DOI] [Google Scholar]
- 44.Boyce P, Parker G, Barnett B, Cooney M, Smith F. Personality as a vulnerability factor to depression. Br J Psychiatry J Ment Sci. 1991;159:106–114. doi: 10.1192/bjp.159.1.106 [DOI] [PubMed] [Google Scholar]
- 45.Boyce P, Hickie I, Parker G, Mitchell P, Wilhelm K, Brodaty H. Specificity of interpersonal sensitivity to non-melancholic depression. J Affect Disord. 1993;27(2):101–105. doi: 10.1016/0165-0327(93)90082-U [DOI] [PubMed] [Google Scholar]
- 46.Liu RT, Kraines MA, Massing-Schaffer M, Alloy LB. Rejection sensitivity and depression: mediation by stress generation. Psychiatry Interpers Biol Process. 2014;77(1):86–97. doi: 10.1521/psyc.2014.77.1.86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luty SE, Joyce PR, Mulder RT, Sullivan F, McKenzie JM. The interpersonal sensitivity measure in depression: associations with temperament and character. J Affect Disord. 2002;70(3):307–312. doi: 10.1016/S0165-0327(01)00312-3 [DOI] [PubMed] [Google Scholar]
- 48.Davis K. Young people’s digital lives: the impact of interpersonal relationships and digital media use on adolescents’ sense of identity. Comput Hum Behav. 2013;29(6):2281–2293. doi: 10.1016/j.chb.2013.05.022 [DOI] [Google Scholar]
- 49.Dziedzic B, Sarwa P, Kobos E, et al. Loneliness and Depression among Polish High-School Students. Int J Environ Res Public Health. 2021;18(4):1706. doi: 10.3390/ijerph18041706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Klerman GL, Weissman MM. Interpersonal Psychotherapy of Depression: A Brief, Focused, Specific Strategy. Jason Aronson, Incorporated; 1994. [Google Scholar]
- 51.Dyer JG, McGuinness TM. Resilience: analysis of the concept. Arch Psychiatr Nurs. 1996;10(5):276–282. doi: 10.1016/S0883-9417(96)80036-7 [DOI] [PubMed] [Google Scholar]
- 52.Zhao Y, Zhao Y, Lee YT, Chen L. Cumulative interpersonal relationship risk and resilience models for bullying victimization and depression in adolescents. Personal Individ Differ. 2020;155:109706. doi: 10.1016/j.paid.2019.109706 [DOI] [Google Scholar]
- 53.Hobfoll SE, Halbesleben J, Neveu JP, Westman M. Conservation of resources in the organizational context: the reality of resources and their consequences. Annu Rev Organ Psychol Organ Behav. 2018;5(1):103–128. doi: 10.1146/annurev-orgpsych-032117-104640 [DOI] [Google Scholar]
- 54.Haeffel GJ, Vargas I. Resilience to depressive symptoms: the buffering effects of enhancing cognitive style and positive life events. J Behav Ther Exp Psychiatry. 2011;42(1):13–18. doi: 10.1016/j.jbtep.2010.09.003 [DOI] [PubMed] [Google Scholar]
- 55.Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health. 2008;56(4):445–453. doi: 10.3200/JACH.56.44.445-454 [DOI] [PubMed] [Google Scholar]
- 56.Kumalasari D, Akmal SZ. Less stress, more satisfied in online learning during the COVID-19 pandemic: the moderating role of academic resilience. Psychol Res Urban Soc. 2021;4(1):36. doi: 10.7454/proust.v4i1.115 [DOI] [Google Scholar]
- 57.Marchini S, Zaurino E, Bouziotis J, Brondino N, Delvenne V, Delhaye M. Study of resilience and loneliness in youth (18–25 years old) during the COVID‐19 pandemic lockdown measures. J Community Psychol. 2021;49(2):468–480. doi: 10.1002/jcop.22473 [DOI] [PubMed] [Google Scholar]
- 58.Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005 [DOI] [PubMed] [Google Scholar]
- 59.Boyce P, Mason C. An overview of depression-prone personality traits and the role of interpersonal sensitivity. Aust N Z J Psychiatry. 1996;30(1):90–103. doi: 10.3109/00048679609076076 [DOI] [PubMed] [Google Scholar]
- 60.Boyce P, Hickie I, Gordon P. Parents, partners or personality? Risk factors for post-natal depression. J Affect Disord. 1991;21(4):245–255. doi: 10.1016/0165-0327(91)90004-C [DOI] [PubMed] [Google Scholar]
- 61.Baumeister RF, Brewer LE, Tice DM, Twenge JM. Thwarting the need to belong: understanding the interpersonal and inner effects of social exclusion: belonging and rejection. Soc Personal Psychol Compass. 2007;1(1):506–520. doi: 10.1111/j.1751-9004.2007.00020.x [DOI] [Google Scholar]
- 62.Weissman MM, Markowitz JC, Klerman GL. The Guide to Interpersonal Psychotherapy: Updated and Expanded Edition. Oxford University Press; 2017. [Google Scholar]
- 63.Smith B, Shatté A, Perlman A, Siers M, Lynch WD. Improvements in resilience, stress, and somatic symptoms following online resilience training: a dose–response effect. J Occup Environ Med. 2018;60(1):1–5. doi: 10.1097/JOM.0000000000001142 [DOI] [PMC free article] [PubMed] [Google Scholar]