Abstract
Objectives
The on-scene time of Emergency Medical Services (EMS), including time for hospital selection, is critical for people in an emergency. However, the outbreak of the novel coronavirus disease 2019 (COVID-19) led to longer delays in providing immediate care for individuals with non-COVID-19-related emergencies, such as epileptic seizures. This study aimed to examine factors associated with on-scene time delays for people with epilepsy (PWE) with seizures needing immediate amelioration.
Materials & Methods
We conducted a population-based retrospective cohort study for PWE transported by EMS between 2016 and 2021. We used data from the Hiroshima City Fire Service Bureau database, divided into three study periods: “Pre period”, the period before the COVID pandemic (2016–2019); “Early period”, the early period of the COVID pandemic (2020); and “Middle period”, the middle period of the COVID pandemic (2021). We performed linear regression modeling to identify factors associated with changes in EMS on-scene time for PWE during each period. In addition, we estimated the rate of total EMS call volume required to maintain the same on-scene time for PWE transported by EMS during the pandemic expansion.
Results
Among 2,205 PWE transported by EMS, significant differences in mean age and prevalence of impaired consciousness were found between pandemic periods. Total EMS call volume per month for all causes during the same month <5,000 (−0.55 min, 95% confidence interval [CI] −1.02 – −0.08, p = 0.022) and transport during the Early period (−1.88 min, 95%CI −2.75 – −1.00, p < 0.001) decreased on-scene time, whereas transport during the Middle period (1.58 min, 95%CI 0.70 – 2.46, p < 0.001) increased on-scene time for PWE transported by EMS. The rate of total EMS call volume was estimated as 0.81 (95%CI −0.04 – 1.07) during the expansion phase of the pandemic to maintain the same degree of on-scene time for PWE transported by EMS before the pandemic.
Conclusions
On-scene time delays on PWE in critical care settings were observed during the Middle period. When the pandemic expanded, the EMS system required resource allocation to maintain EMS for time-sensitive illnesses such as epileptic seizures. Timely system changes are critical to meet dramatic social changes.
Keywords: People with epilepsy, Emergency medical service, On-scene time delay, Resource allocation, Total call volume, Non-COVID-19 critical disease
1. Introduction
Emergency medical services (EMS) facilitate the categorization of hospital resources to identify hospitals capable of handling emergency patients and enable EMS personnel to rapidly transport patients to appropriate medical facilities [1]. In EMS systems, the on-scene time, including the time required for on-site treatment and the time for selection of a hospital, is critical in life-threatening situations. A delay in definitive treatment can lead to unfavorable outcomes [2], [3], [4], [5], [6]. Epileptic seizures resulting in status epilepticus is an emergency disease in which “time is brain”. The prognosis for status epilepticus deteriorates with increasing seizure duration [7]. Thus, extended on-scene time can result in a poorer prognosis for people with epilepsy (PWE).
The novel coronavirus disease 2019 (COVID-19) has had a tremendous impact on medical care worldwide [8]. In the EMS setting, various impacts became visible following the outbreak of COVID-19, including a surge in the number of EMS calls, delays in EMS response times, and declines in non-COVID-19 emergency cases [9], [10]. In addition, people who required immediate care for non-COVID-19 causes faced longer delays during the pandemic, which could have critical implications for neurological prognosis [11], [12]. People with epilepsy are sensitive to dramatic changes in social situations and seizure exacerbation has been reported in 17.5% of PWE during the pandemic [13], [14]. However, whether these PWE were transported promptly or experienced delays during the pandemic are uncertain, highlighting the need to examine emergency responses for PWE using EMS.
The factors contributing to on-scene time delays in EMS during unusual circumstances, including pandemics, are numerous and encompass a lack of human and material resources [15]. Identifying the factors associated with on-scene time delays in EMS during a pandemic could shed light on the limitations of the medical care system for PWE during future unusual circumstances. We, therefore, hypothesized that on-scene time delays in the treatment of PWE would be visible in EMS settings during the pandemic. In addition, such situations may be associated with demand–supply gaps in EMS, as the volume of EMS calls exceeded the availability of local medical resources, regardless of the number of PWE in emergency conditions. To this end, we conducted a longitudinal population-based study to identify factors associated with on-scene time delays in the treatment of PWE in emergencies and to evaluate the demand–supply gap in EMS.
2. Materials & methods
2.1. Study design
We conducted this population-based retrospective cohort study for PWE transported by the Hiroshima City Fire Service Bureau EMS between 1st January 2016 and 31st December 2021. Data were retrieved from the Hiroshima City Fire Service Bureau database, including patient characteristics and EMS time records. To evaluate the impacts of demographic and social factors, we used local and national government official reports and EMS provider reports. This study was approved by the Hiroshima University Hospital Ethics Committee (approval no. E-2566).
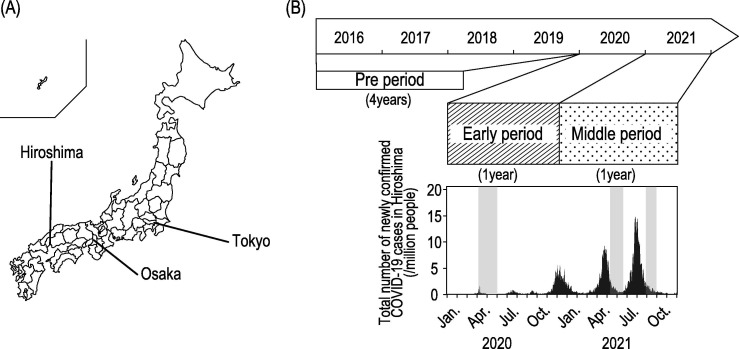
2.2. Geography and the medical care system in Hiroshima City
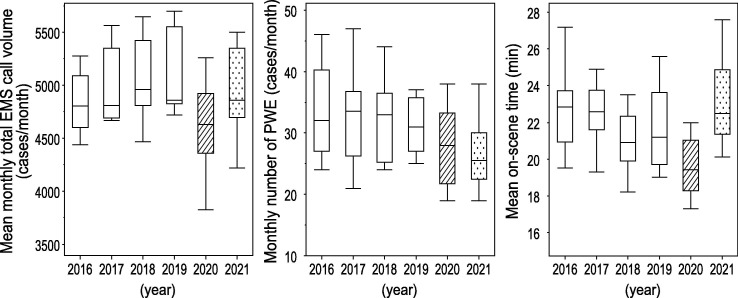
Hiroshima city is an ordinance-designated city in western Japan, with an urban and suburban area of 906.69 km2 and a population of approximately 1.19 million (Fig. 1 A) [16]. Trends in newly confirmed patients with COVID-19 per million people in this area are summarized in Fig. 1B [17], [18]. The EMS system in Japan is designed uniformly nationwide and operated throughout the country by local fire departments [1], [19]. In Hiroshima City, EMS is through the Hiroshima City Fire Service Bureau, which responds to emergency requests via a universal emergency call number. The total EMS call volume for all causes before the pandemic in this area was about 55,000–60,000 per year and 4,500–5,500 per month [20]. Monthly total EMS call volume trends with all causes in this area are summarized in Fig. 2 [20]. Emergency medical services for PWE in Hiroshima City has been provided by some emergency and critical care medical centers cooperating with the Epilepsy Center in Hiroshima University Hospital, the largest epilepsy center in Hiroshima prefecture, accredited by the Japanese Epilepsy Society.
Fig. 1.
Geography and newly confirmed COVID-19 cases in Hiroshima, (A) Geography of Hiroshima. (B) The three observational periods and total number of newly confirmed COVID-19 cases per million people in Hiroshima. Striped meshing area indicated a 1-year phase early in the COVID pandemic as “Early period”. Dot meshing area indicated a 1-year phase middle in the COVID pandemic as “Middle period”. Half-tone dot meshing areas indicate periods under a declaration of a state of emergency.
Fig. 2.
Annual summary of emergency medical services in this study, Annual trends in mean monthly total emergency medical services (EMS) call volume for all causes in this area, mean monthly number of patients with epilepsy (PWE) transported by EMS, and mean on-scene time for PWE transported by EMS are summarized. Striped meshing area indicated “Early period”. Dot meshing area indicated “Middle period”. EMS, emergency medical services; PWE, patients with epilepsy.
2.3. Data sources
Emergency medical services system records are collected using standardized data collection forms and include patient characteristics, time of day, and time course of transport [19]. Emergency room doctors at the receiving hospital clinically determine diagnoses for the illness. These data are completed by EMS personnel and then transferred to the information center at the local fire department [19]. In the present study, we used data for all emergency patients with epileptic seizures who required EMS in 2016–2021 obtained from the Hiroshima City Fire Service Bureau after the removal of all personal identifiers.
2.4. Inclusion and exclusion criteria
We included patients ≥16 years of age who experienced an epileptic seizure and were transported by the Hiroshima City Fire Service Bureau EMS between 1st January 2016 and 31st December 2021. This study focused on patients who experienced chronically recurrent seizures, particularly those who were expected to require emergency transport services repetitively. Thus, PWE were eligible for inclusion. In contrast, patients with acute symptomatic seizures (seizures occur in close temporal relationship with an acute CNS insult, which may be metabolic, toxic, structural, infectious, or due to inflammation) and psychiatric causes were excluded [21].
2.5. Observational periods
This study period was divided into three observational periods based on temporal spikes in infections during the COVID-19 pandemic in Japan: a 4-year period before the COVID pandemic (“Pre period”, January 2016–December 2019, representing baseline data); a 1-year period early in the COVID pandemic (“Early period”, January–December 2020, a year after the World Health Organization Country Office in China was informed of cases of pneumonia of unknown etiology); and a 1-year period in the middle of the COVID pandemic (“Middle period”, January–December 2021, a year after the COVID-19 vaccine started in Japan) (Fig. 1B) [18], [22].
2.6. Demographic and clinical parameters for EMS response
We evaluated patient-associated factors including age, sex, and initial field vital signs (level of consciousness and body temperature). We classified patients with body temperature ≥37.5 °C as having fever and patients in states other than fully awake and oriented as having impaired consciousness. We also evaluated clock-associated factors as the date and time of day, divided into daytime (08:00–19:59) and nighttime (20:00–07:59).
2.7. EMS response time
EMS response time was defined as the elapsed time from initiation of an EMS call to arrival at a hospital and was further divided into three categories: response time; on-scene time; and transport time [15], [23]. On-scene time was defined as the time from arrival at the scene to departure from the scene [15], [23].
2.8. Confounding factors for EMS response
Operations of the EMS were influenced by several social-related factors, particularly during the pandemic [9]. We thus also examined socio-medical conditions concurrent with the transportation of PWE by EMS, including total EMS call volume per month for all causes (such as trauma, internal medical causes, and psychiatric causes) during the same month, the total number of newly confirmed COVID-19 cases per week per million people on the same day, occupation rate of hospital beds on the same day, and declaration of a state of emergency. Total EMS call volume per month was typically around 4,500–5,500 and was categorized as decreasing for values ≤5,000 and increasing for values >5,000. In addition, we determined the expansion of the pandemic using indicators determined by the government office, i.e., the total number of newly confirmed patients with COVID-19 per week per million people >25 and occupation of total hospital beds >50% [24].
2.9. Data analyses
To identify factors associated with a change in emergency transporting time for PWE during the COVID-19 pandemic, we performed a three-step analysis. First, we analyzed the demographic characteristics, clinical characteristics, EMS on-scene time, and socio-medical situations of each patient in the study period. We performed an analysis of variance (ANOVA) followed by Tukey’s posthoc test for categorical variables, and the chi-square test adding to residual analysis for continuous variables to identify features of each phase in the pandemic period.
Second, we performed linear regression modeling to identify factors associated with changes in EMS on-scene time for patients with seizures during each period: the whole period, 2016–2021 (Model 1); the pre-pandemic period, 2016–2019 (Model 2); and the pandemic period, 2020–2021 (Model 3). Parameters for each model were: Model 1, age per 1-year increase, impaired consciousness, transport during the daytime, total EMS call volume per month for all causes during the same month ≤5,000, and transport during the Pre, Early, or Middle period of the pandemic. Model 2: age per 1-year increase, impaired consciousness, transport during the daytime, and total EMS call volume per month for all causes during the same month ≤5,000. Model 3: age per 1-year increase, impaired consciousness, transport during the daytime, total EMS call volume per month for all causes during the same month ≤5,000, the total number of newly confirmed COVID-19 cases per week per million people during the same day ≤25, occupancy of total hospital beds during the same day ≤50%, and being under a declaration of a state of emergency [19], [25]. We conducted pairwise deletion for this analysis.
Third, the rate of total EMS call volume per month for all causes was reverse-estimated to maintain the same degree of on-scene time for PWE transported by EMS during the non-expansion phase of the pandemic (total number of newly confirmed COVID-19 cases per week per million people ≤25, and hospital bed occupancy ≤50%) or expansion phase of the pandemic (total number of new confirmed COVID-19 cases per week per million >25, and hospital bed occupancy >50%). In all analyses, values of p < 0.05 were considered significant. All statistical analyses were conducted using JMP Pro software (version 16; SAS Institute, Cary, NC, USA).
3. Results
Among 12,320 cases with any seizures transported by EMS, 10,115 cases with <16 years of age, acute symptomatic seizures, or psychiatric causes were excluded. Thus, we reviewed the cases of 2,205 PWE transported by EMS (Table 1 ). Significant differences in mean age and prevalence of impaired consciousness were seen between periods of the pandemic. During the Early period, the mean on-scene time for EMS was 19.6 ± 8.2 min, and the mean total EMS call volume per month for all causes was 4,665.6 ± 411.0, both of which were lower than those observed during the other periods of the pandemic (p < 0.001) (Table 1). Trends in mean on-scene time, number of PWE, and mean total EMS call volume per month for all causes during each year and each period are summarized in Fig. 2.
Table 1.
Characteristics of patients with epilepsy transported by emergency medical services per period of the COVID-19 pandemic.
| Total (n = 2,205) |
Pre period (n = 1,546) |
Early period (n = 335) |
Middle period (n = 324) |
p | |
|---|---|---|---|---|---|
| Age, years, mean (SD) | 48.2 ± 23.4 | 47.1 ± 23.2 | 50.0 ± 23.5 | 51.6 ± 23.5** | 0.002 |
| Female, n (%) | 883 (40.0) | 618 (40.0) | 132 (39.4) | 133 (41.1) | 0.906 |
| Fever (>37.5℃), n (%) | 209 (13.5) | 127 (13.9) | 38 (11.8) | 44 (14.4) | 0.569 |
| Impaired consciousness, n (%) | 1783 (80.1) | 1224 (79.3) | 281 (84.1) | 278 (85.8) | 0.007 |
| Daytime (08:00–19:59), n (%) | 1510(68.5) | 1066 (69.0) | 228 (68.1) | 216 (66.7) | 0.712 |
| On-scene time, mean (SD) | 21.8 ± 10.8 | 22.0 ± 10.7 | 19.6 ± 8.2*** | 23.2 ± 13.1 | <0.001 |
| Total EMS call volume per months for all causes during same month, mean (SD) | 4,951.9 ± 424.1 | 5,012.6 ± 414.4 | 4,665.6 ± 411.0*** | 4,957.7 ± 358.5 | <0.001 |
*p < 0.05; **p < 0.01; ***p < 0.001.
COVID-19, coronavirus disease 2019; SD, standard deviation; EMS, emergency medical services.
Second, during the whole period, in addition to the demographic and clinical characteristics, total EMS call volume per month related to all causes during the same month <5,000 (−0.55 min, 95% confidence interval [CI] −1.02 – −0.08, p = 0.022), and transport during the Early period (−1.88 min, 95%CI −2.75 – −1.00, p < 0.001) showed decreased on-scene time, but patients transported during the Middle period (1.58 min, 95%CI 0.70 – 2.46, p < 0.001) showed the increased on-scene time for PWE transported by EMS (Model 1). However, in the Pre period, the total EMS call volume per month for all causes during the same month did not affect the on-scene time for PWE transported by EMS (Model 2). During the pandemic period, in addition to demographic and clinical characteristics, total EMS call volume per month for all causes during the same month <5,000 (−1.21 min, 95%CI −2.19 – −0.23, p = 0.016) decreased on-scene time for PWE transported by EMS. However, the total number of newly confirmed COVID-19 cases, occupancy of total hospital beds, and being under a declaration of a state of emergency did not affect the on-scene time for PWE transported by EMS (Model 3) (Table 2 ).
Table 2.
Factors associated with on-scene time of patients with epilepsy transported by emergency medical services per period of COVID-19 pandemic.
| Variable | Model 1 (whole period) |
Model 2 (Pre-period) |
Model 3 (pandemic period) |
|||
|---|---|---|---|---|---|---|
| On-scene time (95%CI) | p | On-scene time (95%CI) | p | On-scene time (95%CI) | p | |
| Age (per 1-year increase) | −0.05 (−0.07 – −0.03) | <0.001 | −0.06 (−0.08 – −0.03) | <0.001 | −0.04 (−0.08 – −0.01) | 0.021 |
| Impaired consciousness | 0.93 (0.36 – 1.50) | 0.001 | 0.94 (0.28 – 1.59) | 0.005 | 0.90 (−0.26 – 2.06) | 0.127 |
| Daytime (08:00–19:59) | −1.24 (−1.72 – −0.76) | <0.001 | −0.88 (−1.45 – −031) | 0.003 | −2.02 (−2.91 – −1.13) | <0.001 |
| Total EMS call volume per month for all causes during same month (<5,000/month) | −0.55 (−1.02 – −0.08) | 0.022 | −0.40 (−0.95 – 0.14) | 0.15 | −1.21 (−2.19 – −0.23) | 0.016 |
| Period (Early period) | −1.88 (−2.75 – −1.00) | <0.001 | ||||
| Period (Middle period) | 1.58 (0.70 – 2.46) | <0.001 | ||||
| Total number of newly confirmed COVID-19 cases per week per million people during same day (<25/million people) | −1.39 (−3.15 – 0.37) | 0.121 | ||||
| Occupation of total hospital beds during same day (<50%) | −0.40 (−1.79 – 0.99) | 0.568 | ||||
| Under declaration of state of emergency | 0.07 (−1.08 – 1.21) | 0.908 | ||||
Model 1: age per 1-year increase, impaired consciousness, transported during daytime, total EMS call volume per month for all causes during same month ≤5,000, transported during Pre, Early, or Middle period.
Model 2: age per 1-year increase, impaired consciousness, transported during daytime, total EMS call volume per month for all causes during same month ≤5,000.
Model 3: age per 1-year increase, impaired consciousness, transported during daytime, total EMS call volume per month for all causes during same month ≤5,000, total number of newly confirmed COVID-19 cases per week per million people during same day ≤25, occupancy of total hospital beds during same day ≤50%, under declaration of state of emergency.
COVID-19, coronavirus disease 2019; EMS, emergency medical services; CI, confidence interval.
Third, the rate of total EMS call volume per month for all causes was 1.01 (95%CI 0.95 – 1.22) in the non-expansion phase of the pandemic but was 0.81 (95%CI −0.04 – 1.07) in the expansion phase of the pandemic to maintain the same degree of on-scene time for PWE transported by EMS (21.8 min; mean on-scene time for the whole period) (Table 3 ).
Table 3.
Estimated rate of total EMS call volume per month for all causes during same month to maintain the same degree of on-scene time for PWE transported by EMS in the pandemic period.
| On-scene time (min) | Variable |
Estimated rate of total EMS call volume per month for all causes during same month (95%CI) | |
|---|---|---|---|
| Total number of newly confirmed COVID-19 cases per week per million people during same day (/ million people) | Hospital bed occupancy during same day (%) | ||
| 21.8 | ≤25 | ≤50 | 1.01 (0.95 – 1.22) |
| 21.8 | ≤25 | >50 | 0.98 (0.65 – 1.16) |
| 21.8 | >25 | ≤50 | 0.85 (0.35 – 1.05) |
| 21.8 | >25 | >50 | 0.81 (-0.04 – 1.07) |
EMS, emergency medical services; PWE, people with epilepsy; COVID-19, coronavirus disease 2019; CI, confidence interval.
4. Discussion
In the present study, on-scene time delays for PWE with seizures in emergencies were observed in the Middle period, despite the absence of any corresponding increase in the number of PWE cases transported by EMS. On-scene time for PWE was unaffected by total EMS call volume during the Pre period but was impacted by this factor during the pandemic period, despite a lack of increase in call volume. The estimated rate of total EMS call volume indicated a discrepancy between the demand and supply of critical care services in the healthcare system during the expansion phase of the pandemic in our study area. These findings collectively suggest that when total EMS call volume exceeds the availability of local medical resources, EMS on-scene time may occasionally be delayed in unusual circumstances, such as the COVID-19 pandemic, particularly during the expansion phase. Given that prolonged epileptic seizures need to be treated immediately, effecting a transformative adaptation of emergency transport systems in response to substantial alterations in social conditions is imperative.
We confirmed that on-scene time was dramatically affected during the periods of the pandemic. In the Early period, overall call volumes decreased, similar to outcomes reported in other regions [26]. In the Middle period, government offices in Japan changed the policy for COVID-19 infections based on perceived immunity in the population obtained from vaccination or natural infection [27]. The total call volume for EMS in this area recovered to the same degree as seen in the Pre period [20]. Our findings confirm that demand–supply discrepancies in the critical care system were negligible during the non-expansion phase of the pandemic, but substantial during the expansion phase. The COVID-19 pandemic necessitated the redistribution of various healthcare resources when demand exceeded supply [28]. These results imply that the on-scene time for time-sensitive illnesses, such as epileptic seizures, may be influenced by the availability of EMS resources in unusual circumstances.
Since the onset of the pandemic, despite the worldwide efforts of national and local governments to maintain the quality of healthcare services at the same level as before the pandemic, a decrease in the number of non-COVID-19 emergency cases has been documented globally [9], [27], [29], [30]. In the present study, the incidence of seizures that EMS transported declined during the pandemic. These seizures were associated with higher patient age and a higher prevalence of altered consciousness compared to the pre-pandemic period. During the pandemic period, some societies recommended reducing in-person healthcare facility visits for PWE with stable seizures, which decreased outpatient visits and admissions in epilepsy centers [31]. Our results might indicate that PWE with non-life-threatening status but a need for medication avoided calls to EMS, as in another study on stroke patients [32]. Thus, clinicians should promote intensive follow-up by telemedicine in both new and follow-up patients, especially during pandemics [30].
Certain facilities within stroke care units were found to exhibit no significant delay in the interval between hospital arrival and initiation/intervention [32], [33]. These observations suggested that patients in critical care settings can receive adequate treatment even during a pandemic if prompt transport to appropriate medical facilities is achieved. Patients hospitalized for seizures are often readmitted due to modifiable factors in the care process, such as seizure exacerbation or multiple medical comorbidities [34]. Mitigating readmission rates could alleviate the demand–supply discrepancy in EMS. Home-care support clinics can mitigate the likelihood of rehospitalization in critical care settings, such as in cases of heart failure [35]. These findings collectively suggest that cooperation between professionals in a multidisciplinary team providing emergency care, recovery or chronic care, and epilepsy experts may enhance seizure outcomes and overall health results for PWE.
Some limitations to the present study warrant notation. First, the present study was performed using population-based data from a single region. Thus, there are limitations in generalizing the results of this study. As the EMS system in Japan is operated by local fire departments (733 fire departments in total), regional differences in the EMS system and the distribution of medical facilities were not negligible [19], [36]. However, the EMS system in Japan is well-designed. The median time between EMS call to EMS arrival on the scene varies only by less than a minute across different regions in Japan [19]. Hence, population-based data including multiple regions are needed to confirm the significance and generalizability of the present results. Second, as we were unable to follow-up with PWE using EMS after arrival in the hospital, we could not evaluate how the pandemic affected outcomes. Last, multiple potential factors could not be added to our analysis. Total EMS call volume was influenced by health risk messaging by the media and national authorities [30]. Reducing risk factors such as road traffic accidents, falls and injuries, and air-borne infectious diseases could all affect the total call volume to EMS [30]. Our present study could not analyze these multiple potential factors.
5. Conclusions
In conclusion, on-scene time delays on PWE in critical care settings were noticed during the expansion phase of the pandemic. During the non-expansion phase of the pandemic, the impact of increasing total EMS call volume was inconsequential. However, during the pandemic expansion, the EMS system required proper resource allocation to effectively manage time-sensitive illnesses such as epileptic seizures. Thus, our study underscores the need for national and local governments to prepare and allocate resources and funding for comparable public health crises, in order to ensure sufficient availability of EMS and healthcare. Additionally, clinicians should also consider providing intensive follow-up through telemedicine to prevent occasional seizure worsening for PWE during pandemics. Timely changes in the system are essential to address significant societal shifts.
Declarations
Ethics approval and consent to participate:
This was a population-based, observational study. Our study was performed with anonymous clinical data under close supervision following approval by the Ethics Committee of the Hiroshima University Hospital (E2021-2566-01). Informed consent was obtained in the form of an opt-out on the hospital website. All procedures involving human participants were performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent for publication:
Informed consent was obtained in the form of an opt-out on the hospital website. Those who opted out were to be excluded from the analysis. In the present study, no patients opted out.
Availability of data and materials:
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval statement
This study was approved by the Ethics Committee of Hiroshima University Hospital (approval no. E2021-2566-01).
Patient consent statement
All patients provided informed consent to participate.
Funding:
None.
Authors' contributions:
• Hidetada Yamada and Shuichiro Neshige: designed and conceptualized the study; analyzed the data; and drafted the manuscript for intellectual content.
• Shiro Aoki and Yu Yamazaki: interpreted the data; and revised the manuscript for intellectual content.
• Megumi Nonaka, Yoshiko Takebayashi, Haruka Ishibashi, and Atsuko Motoda: analyzed and interpreted the data.
• Hirofumi Maruyama; revised the manuscript for intellectual content.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors would like to express their appreciation to Dr. Hirofumi Wakaki, a Professor at Hiroshima University, and Dr. Keisuke Fukui, an Associate Professor at Hiroshima University, for lending their expertise on statistical data analysis.
We are grateful to Mr. Toru Nakata and Mr. Jun Iwai from the Hiroshima City Fire Service Bureau, and Dr. Junki Ishii from the Department of Emergency and Critical Care Medicine at Hiroshima University for providing access to the EMS database, and to the multidisciplinary team members in emergency and critical care medical centers providing EMS for PWE in Hiroshima city.
We also thank Dr. Megumi Toko, Dr. Hiroyuki Naito, Dr. Takamichi Sugimoto, Dr. Masahiro Nakamori, and Dr. Tomohisa Nezu for their useful contributions.
References
- 1.Tanigawa K., Tanaka K. Emergency medical service systems in Japan: past, present, and future. Resuscitation. 2006;69(3):365–370. doi: 10.1016/j.resuscitation.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 2.Coute RA, Nathanson BH, Kurz MC, McNally B, Mader TJ; CARES Surveillance Group. The association between scene time interval and neurologic outcome following adult bystander witnessed out-of-hospital cardiac arrest. Am J Emerg Med 2021;46:628–33. [DOI] [PubMed]
- 3.Shin S.D., Kitamura T., Hwang S.S., Kajino K., Song K.J., Ro Y.S., et al. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014;85(2):203–210. doi: 10.1016/j.resuscitation.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 4.Ordoobadi A.J., Peters G.A., Westfal M.L., Kelleher C.M., Chang D.C. Disparity in prehospital scene time for geriatric trauma patients. Am J Surg. 2022;223(6):1200–1205. doi: 10.1016/j.amjsurg.2021.10.031. [DOI] [PubMed] [Google Scholar]
- 5.Alarhayem A.Q., Myers J.G., Dent D., Liao L., Muir M., Mueller D., et al. Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour”. Am J Surg. 2016;212(6):1101–1105. doi: 10.1016/j.amjsurg.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 6.Gauss T., Ageron F.X., Devaud M.L., Debaty G., Travers S., Garrigue D., et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019;154(12):1117–1124. doi: 10.1001/jamasurg.2019.3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trinka E., Kälviäinen R. 25 years of advances in the definition, classification and treatment of status epilepticus. Seizure. 2017;44:65–73. doi: 10.1016/j.seizure.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Amiry A., Maguire B.J. Emergency medical services (EMS) calls during COVID-19: early lessons learned for systems planning (a narrative review) Open Access Emerg Med. 2021;13:407–414. doi: 10.2147/OAEM.S324568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jaffe E., Strugo R., Bin E., Blustein O., Rosenblat I., Alpert E.A., et al. The role of emergency medical services in containing COVID-19. Am J Emerg Med. 2020;38(7):1526–1527. doi: 10.1016/j.ajem.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim H.S., Jang T.C., Kim G.M., Lee S.H., Ko S.H., Seo Y.W. Impact of the coronavirus disease 2019 outbreak on the transportation of patients requiring emergency care. Medicine (Baltimore) 2020;99(50):e23446. doi: 10.1097/MD.0000000000023446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zachrison KS, Nielsen VM, de la Ossa NP, Madsen TE, Cash RE, Crowe RP, et al. Prehospital stroke care part 1: emergency medical services and the stroke systems of care. Stroke 2022; Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 13.Neshige S., Aoki S., Takebayashi Y., Shishido T., Yamazaki Y., Iida K., et al. A longitudinal seizure outcome following the COVID-19 pandemic in 2020 and 2021: transient exacerbation or sustainable mitigation. J Neurol Sci. 2022;434 doi: 10.1016/j.jns.2021.120100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fountain N.B., Van Ness P.C., Bennett A., Absher J., Patel A.D., Sheth K.N., et al. Quality improvement in neurology: Epilepsy Update Quality Measurement Set. Neurology. 2015;84(14):1483–1487. doi: 10.1212/WNL.0000000000001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morita T., Tsubokura M., Furutani T., Nomura S., Ochi S., Leppold C., et al. Impacts of the 2011 Fukushima nuclear accident on emergency medical service times in Soma District, Japan: a retrospective observational study. BMJ Open. 2016;6(9):e013205. doi: 10.1136/bmjopen-2016-013205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Summary of the Hiroshima City Fire Service Bureau. 2022 September 13, 2022; Available from: https://www.city.hiroshima.lg.jp/site/shobo/12062.html. [accessed 10 January 2023].
- 17.Summary of the confirmed cases for a patient with COVID-19 in Hiroshima city. 2023 January 10, 2023; Available from: https://www.city.hiroshima.lg.jp/site/shobo/12062.html. [accessed 10 January 2023].
- 18.COVID-19 TRACKER in Japan. 2022 July 15, 2022; Available from: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/ja/countries-and-territories/japan/. [accessed 10 January 2023].
- 19.Nakao S., Katayama Y., Kitamura T., Hirose T., Sado J., Ishida K., et al. Epidemiological profile of emergency medical services in Japan: a population-based descriptive study in 2016. Acute Med Surg. 2020;7(1):e485. doi: 10.1002/ams2.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Annual review Hiroshima City Fire Service Bureau. 2022 November 1, 2022; Available from: https://www.city.hiroshima.lg.jp/site/shobo/list1809-3710.html. [accessed 10 January 2023].
- 21.Beghi E., Carpio A., Forsgren L., Hesdorffer D.C., Malmgren K., Sander J.W., et al. Recommendation for a definition of acute symptomatic seizure. Epilepsia. 2010;51(4):671–675. doi: 10.1111/j.1528-1167.2009.02285.x. [DOI] [PubMed] [Google Scholar]
- 22.The 53rd meeting of Novel Coronavirus Response Headquarters. 2021; Available from: https://www.kantei.go.jp/jp/singi/novel_coronavirus/th_siryou/sidai_r030122.pdf. [accessed 10 January 2023].
- 23.Spaite D.W., Valenzuela T.D., Meislin H.W., Criss E.A., Hinsberg P. Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med. 1993;22(4):638–645. doi: 10.1016/s0196-0644(05)81840-2. [DOI] [PubMed] [Google Scholar]
- 24.The 2nd Meeting of Subcommittee on Novel Coronavirus Disease Control. 2021; Available from: https://www.cas.go.jp/jp/seisaku/ful/taisakusuisin/bunkakai/dai2/kansensaikakudaiboushi_shihyou_teigen.pdf. [accessed 10 January 2023].
- 25.The summary of the declaration of the state of emergency. 2023; Available from: https://corona.go.jp/news/news_20200421_70.html. [accessed 10 January 2023].
- 26.Jasani G., Alemayehu T., Chizmar T., Wilson L. Changes in EMS utilization in the state of Maryland during the first 6 months of the COVID-19 pandemic. Am J Disaster Med. 2022;17(1):41–48. doi: 10.5055/ajdm.2022.0418. [DOI] [PubMed] [Google Scholar]
- 27.The 103rd Meeting of the Advisory Board on Countermeasures to COVID-19 Infections. 2022; Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000121431_00395.html. [accessed 10 January 2023].
- 28.Ehmann M.R., Zink E.K., Levin A.B., Suarez J.I., Belcher H.M.E., Daugherty Biddison E.L., et al. Operational recommendations for scarce resource allocation in a public health crisis. Chest. 2021;159(3):1076–1083. doi: 10.1016/j.chest.2020.09.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tuczyńska M., Matthews-Kozanecka M., Baum E. Accessibility to non-COVID health services in the world during the COVID-19 pandemic: review. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.760795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lastrucci V., Collini F., Forni S., D'Arienzo S., Di Fabrizio V., Buscemi P., et al. The indirect impact of COVID-19 pandemic on the utilization of the emergency medical services during the first pandemic wave: a system-wide study of Tuscany region, Italy. PLoS One. 2022;17(7):e0264806. doi: 10.1371/journal.pone.0264806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuroda N., Kubota T., Horinouchi T., Ikegaya N., Kitazawa Y., Kodama S., et al. Impact of COVID-19 pandemic on epilepsy care in Japan: a national-level multicenter retrospective cohort study. Epilepsia Open. 2022;7(3):431–441. doi: 10.1002/epi4.12616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siegler J.E., Heslin M.E., Thau L., Smith A., Jovin T.G. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29(8) doi: 10.1016/j.jstrokecerebrovasdis.2020.104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mitsuhashi T, Tokugawa J, Mitsuhashi H. Long-term evaluation of the COVID-19 pandemic impact on acute stroke management: an analysis of the 21-month data from a medical facility in Tokyo. Acta Neurol Bell 2022:1–8. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 34.Blank L.J., Crispo J.A.G., Thibault D.P., Davis K.A., Litt B., Willis A.W. Readmission after seizure discharge in a nationally representative sample. Neurology. 2018;92(5):e429–e442. doi: 10.1212/WNL.0000000000006746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sun Y, Iwagami M, Komiyama J, Sugiyama T, Inokuchi R, Sakata N, et al. The effect of home care support clinics on hospital readmission in heart failure patients in Japan. J Gen Intern Med 2023; Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 36.Matsuyama T., Kitamura T., Katayama Y., Kiyohara K., Hayashida S., Kawamura T., et al. Factors associated with the difficulty in hospital acceptance among elderly emergency patients: a population-based study in Osaka City. Japan Geriatrics Gerontol Int. 2017;17(12):2441–2448. doi: 10.1111/ggi.13098. [DOI] [PubMed] [Google Scholar]