Pre-frailty is a condition that precedes frailty; in 2001, Linda Fried and colleagues defined pre-frailty as the presence of 1 or 2 out of the 5 Fried criteria [1]. Hence, pre-frail older adults represent an intermediate category between normal and frail older adults. Comorbidities are known to play a pivotal role in frailty, in addition to contributing to increasing healthcare costs [2-4]. Hypertension is one of the most common conditions in pre-frailty, and its role in the onset of frailty remains debated [5-7]. Similarly, admission and stress hyperglycemia are prevailing risk factors of adverse outcomes, with or without diabetes [8, 9]. Nevertheless, to the best of our knowledge, the impact of hyperglycemia in the pre-frailty to frailty transition has never been investigated hitherto.
Thus, we designed a study to evaluate pre-frail hypertensive older adults comparing hyperglycemic to normoglycemic patients, at baseline and at six-month follow-up. We recruited consecutive pre-frail older patients with hypertension who presented from March 2021 to December 2021 at ASL (local health unit of the Italian Ministry of Health) Avellino, Italy. All of them fulfilled the following inclusion criteria: age >65 years; previous diagnosis of hypertension with no evidence of secondary causes; a frailty status; Montreal Cognitive Assessment (MoCA) score <26. Hyperglycemia was defined by values >140 mg/dL as we previously described [9]. An informed consent was signed by each patient (or legal representative). Research was performed according to the 1975 Declaration of Helsinki and its later amendments. The Institutional Review Board of Campania Nord approved the protocol.
Global cognitive function was assessed using the MoCA test; this cognitive test covers many cognitive skills, and scores range from 0 to 30, with cognitive impairment defined by values <26. A physical frailty assessment was performed according to the Fried Criteria [1], at baseline and at six-month follow-up. A diagnosis of pre-frailty status was performed with at least one or two points out of the following five: low physical activity level, weight loss, exhaustion, weakness, slowness [1].
Data are presented as mean±SD or numbers and percentages, as appropriate. Based on our preliminary findings, we calculated the number of patients required for the study to reject the null hypothesis 95% of the time with a two-tailed type I error at the 0.05 level of significance; the sample size was calculated via G*POWER software, yielding a minimum size of 201 patients. We compared hyperglycemic and normoglycemic group. To adjust for potential confounding factors, we also performed a multivariable regression analysis. All calculations were computed using the SPSS 26 software.
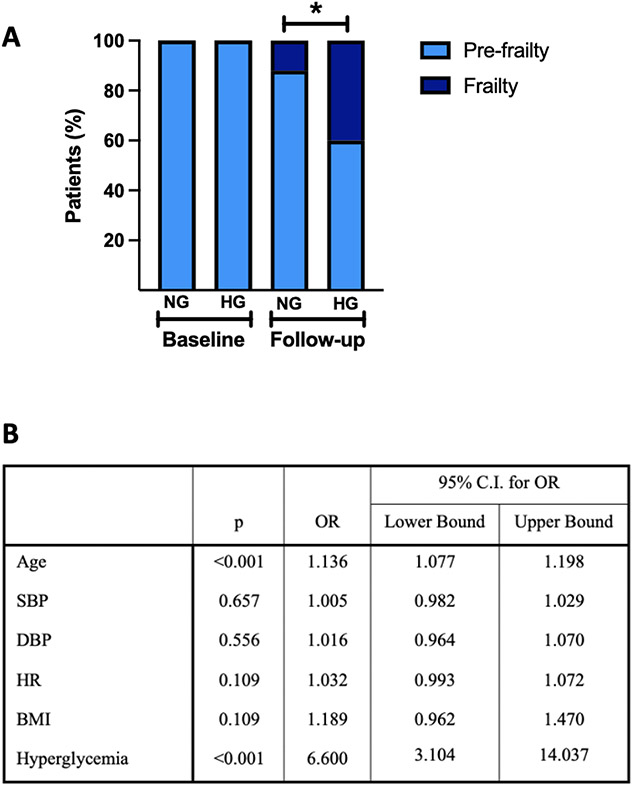
231 pre-frail older adults were enrolled and divided in two populations according to their baseline blood glucose values: normoglycemic and hyperglycemic; no significant differences were noted between these populations apart from blood glucose levels. At six-month followup, we observed that many hyperglycemic patients developed frailty whereas only few normoglycemic patients had frailty (40.2% vs. 12.1%; p<0.001) (Fig. 1A). These results were confirmed by a multivariate regression analysis, using frailty at follow-up as dependent variable (Fig. 1B).
Fig. 1.
A. Percentages of patients with pre-frailty or frailty at baseline and at follow-up. B. Logistic Regression with frailty at follow-up as the dependent variable. BMI: Body mass index; DBP: diastolic blood pressure; HG: Hyperglycemia; HR: heart rate; NG: Normoglycemia; SBP: systolic blood pressure; *:p<0.001.
Taken together, our data indicate the importance of hyperglycemia in the development of frailty and suggest that glycemic control remains a fundamental goal to be achieved in hypertensive pre-frail older adults with or without diabetes. The management of pre-frailty is indeed a crucial aspect in older adults. Hence, a careful clinical evaluation and a good geriatric assessment should be considered as the preferred ways to prevent or delay the onset of frailty.
One of the common features of hypertension and hyperglycemia is endothelial dysfunction, which is known to increase the risk of oxidative stress, inflammation, and atherosclerosis [10]. In this scenario, the transition from pre-frailty to frailty triggered by hyperglycemia in hypertensive older adults could depend on the increased endothelial dysfunction. We reckon that our study is not exempt from limitations, including being conducted in a single center with a relatively short follow-up; further investigations with a longer follow-up and larger sample size are warranted to corroborate our data.
Acknowledgements
We thank Dr. Wilson and Dr. Wang for helpful discussion.
Funding
Prof. Gaetano Santulli is supported in part by the Monique Weill-Caulier and Irma T. Hirschl Trusts (to G.S.).
Footnotes
CRediT authorship contribution statement
Pasquale Mone: Formal analysis, Conceptualization, Data curation, Investigation, Writing – original draft. Stefano De Gennaro: Formal analysis, Investigation, Software, Validation, Visualization. Salvatore Frullone: Data curation, Investigation, Project administration, Resources, Visualization. Anna Marro: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization. Gaetano Santulli: Visualization, Conceptualization, Funding acquisition, Writing – review & editing.
Declaration of Competing Interest
All authors declare that they have no competing interests.
References
- [1].Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56. [DOI] [PubMed] [Google Scholar]
- [2].Massussi M, Adamo M, Rosato S, Seccareccia F, Barbanti M, Biancari F, et al. Functional and metabolic frailty predicts mortality in patients undergoing TAVI: insights from the OBSERVANT II study. Eur J Intern Med 2022;106:90–6. [DOI] [PubMed] [Google Scholar]
- [3].Vetrano DL, Foebel AD, Marengoni A, Brandi V, Collamati A, Heckman GA, et al. Chronic diseases and geriatric syndromes: the different weight of comorbidity. Eur J Intern Med 2016;27:62–7. [DOI] [PubMed] [Google Scholar]
- [4].Simpson FR, Justice JN, Pilla SJ, Kritchevsky SB, Boyko EJ, Munshi MN, et al. An examination of whether diabetes control and treatments are associated with change in frailty index across 8 years: an ancillary exploratory study from the action for health in diabetes (Look AHEAD) trial. Diabetes Care 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res 2019;124:1045–60. [DOI] [PubMed] [Google Scholar]
- [6].Mone P, Pansini A, Frullone S, de Donato A, Buonincontri V, De Blasiis P, et al. Physical decline and cognitive impairment in frail hypertensive elders during COVID-19. Eur J Intern Med 2022;99:89–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Zucchelli A, Vetrano DL, Marengoni A, Grande G, Romanelli G, Calderon-Larranaga A, et al. Frailty predicts short-term survival even in older adults without multimorbidity. Eur J Intern Med 2018;56:53–6. [DOI] [PubMed] [Google Scholar]
- [8].Russo MP, Elizondo CM, Giunta DH, Grande Ratti MF. Prevalence of hyperglycemia and incidence of stress hyperglycemia in hospitalized patients: a retrospective cohort. Eur J Intern Med 2017;43. e15–e7. [DOI] [PubMed] [Google Scholar]
- [9].Mone P, Gambardella J, Minicucci F, Lombardi A, Mauro C, Santulli G. Hyperglycemia drives stent restenosis in STEMI patients. Diabetes Care 2021;44. e192–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yoda K, Inaba M, Hamamoto K, Yoda M, Tsuda A, Mori K, et al. Association between glycemic control and morning blood pressure surge with vascular endothelial dysfunction in type 2 diabetic patients. Diabetes Care 2014;37:644–50. [DOI] [PubMed] [Google Scholar]