Abstract
Summary
Upper extremity (UE) fractures are prevalent age-related fractures, and stair-associated falls are a common mechanism for these injuries. Our study has identified an increasing incidence of stair-related UE fractures and associated hospitalization rates among the older United States population between 2012–2021. Targeted prevention efforts should be implemented by health systems.
Introduction
To analyze United States (US) emergency department trends in upper extremity stair-related fractures among older adults and investigate risk factors associated with hospitalization.
Methods
We queried the National Electronic Injury Surveillance System (NEISS) for all stair-related fracture injuries between 2012 and 2021 among adults 65 years or older. The US Census Bureau International Database (IDB) was analyzed to calculate incidence rates. Descriptive analysis, linear regression analysis, and multivariate regression analysis were used to interpret the collected data.
Results
Our analysis estimated 251,041 (95% CI: 211,678–290,404) upper extremity stair-related fractures among older adults occurred between 2012 and 2021. The primary anatomical locations were the humeral shaft (27%), wrist (26%), and proximal humerus (18%). We found a 56% increase in injuries (R2 = 0.77, p < 0.001), 7% increase in incidence per 100,000 persons (R2 = 0.42, p < 0.05), and an 38% increase in hospitalization rate (R2 = 0.61, p < 0.01) during the 10-year study period. Women sustained the majority of fractures (76%) and most injuries occurred in homes (89%). Advanced age (p < 0.0001), males (p < 0.0001), proximal humerus fractures (p < 0.0001), humeral shaft fractures (p < 0.0001), and elbow fractures (p < 0.0001) were associated with increased odds of hospitalization after injury.
Conclusion
Stair-related UE fracture injuries, incidence, and hospitalization rates among older adults are increasing significantly, particularly among older females. Improving bone health, optimizing functional muscle mass, and “fall-proofing” homes of older age groups may help mitigate the rising incidence of these injuries.
Keywords: Upper extremity, Fragility fracture, Older age, Stair, Epidemiology
Introduction
Falls among patients 65 years and older are associated with a marked increase in hospitalization, morbidity, mortality, and healthcare costs [1, 2]. Nearly one-third of adults among this age group experience a fall at least once per year, and half of these adults will experience a second fall [3]. This patient population is especially prone to fragility fractures – fractures that result from mechanical forces that would not ordinarily cause fractures. Each year, fragility fractures occur in the older United States (US) population at a higher rate than heart attacks, breast cancer, and strokes combined [4]. Upper extremity (UE) fractures are among the most prevalent age-related fractures, and stair-associated falls are a common mechanism [5, 6]. UE fractures, particularly among older adults, can lead to decreased quality of life, impairment in activities of daily living, and an increased risk of future falls and fractures [7].
As the US older adult population continues to grow, age-related fractures are likely to increase, mainly due to increased fall risk and decreased bone density in older age groups. While there is significant literature regarding the epidemiology and disease burden of hip and vertebral fractures in the United States, few studies explore trends in upper extremity trauma, and few examine injury characteristics and epidemiology of UE fractures in stair falls. The lack of literature in this area makes it challenging to develop and implement evidence-based prevention and management strategies for UE injuries [8–11].
Our study aimed to quantify US emergency department (ED) trends in UE stair-related fractures among older adults (≥ 65 years of age) between 2012 and 2021 and to understand key risk factors associated with these traumatic injuries and associated hospitalization. Additionally, we compared injury trends to older adult population trends between 2012 and 2021 to identify trends in the incidence of UE stair-related fractures in older age groups. We hypothesized that the total cases and incidence of UE stair-related fractures among older adults have been increasing over time, given the increased age of the United States population.
Methods
Study design
We queried the National Electronic Injury Surveillance System (NEISS) of the United States Consumer Product Safety Commission (CPSC) for all stair-related fracture injuries between 2012 and 2021 among patients 65 years or older. The NEISS database provides a nationally representative sample of US hospital emergency departments. The sample includes 100 hospital EDs nationwide stratified by hospital size and geographic location. Stratification of the sample by total ED visits allows for weighted sampling so that national estimates with sampling errors can be derived for documented injuries [12]. We also assessed population changes within our age cohort during the study period using the US Census Bureau International Database (IDB).
ED visits for stair-related fractures in older adults were identified using NEISS injury mechanism code (1842: Stairs Or Steps), diagnosis codes (57: Fracture), body part codes (30: Shoulder, 32: Elbow, 33: Lower Arm, 34: Wrist, 80: Upper Arm, 82: Hand, 92: Finger), and age (≥ 65). The included upper extremity fracture injuries were the primary injury sustained by each patient as reported in the NEISS database. Patient demographics that were collected included patient age, sex, and year of admission. Data regarding the injury that was collected included anatomic injury location, diagnosis, location of incident, and disposition. The location of incident was classified into one of three categories: home, public area, or other. "Home” included houses, private areas surrounding houses, apartments, and condominiums [12]. “Public areas” included public infrastructure, such as stores, office buildings, and residential treatment facilities (assisted living, nursing home, and extended care). “Other” was defined as an injury incident at a school, recreational area, or street.
Statistical analysis
National estimates with 95% confidence intervals were calculated by summing up sample weights and using sampling error coefficients provided by the CPSC [12]. Injury characteristics were analyzed using descriptive statistics. Linear regression analysis was performed to identify trends in upper extremity fracture, incidence per 100,000 persons, and hospitalization rates by year of injury. A multivariate regression analysis was performed to identify odds for hospitalization after upper extremity fracture injuries based on the patient age, sex, and location of injury. All statistical analyses were performed using STATA Version 17 software (StataCorp, College Station, TX, USA). Statistical significance was set at p < 0.05.
Results
Analysis of the NEISS database resulted in an estimate of 2,515,245 (95% CI: 2,125,841–2,904,648) stair-related injuries in individuals aged 65 and older between 2012 to 2021. The most common location of injuries were of the head (27%), lower extremity (24%), and upper extremity (19%). The most common diagnoses of injuries were fractures (34%), contusions or abrasions (18%), and visceral injuries (16%). The most common fracture location was the upper extremity with a national estimate of 251,041 patients (95%CI: 211,678–290,404) affected between 2012 to 2021. The majority of the fractures were identified in women (76%). Among patients with UE fractures where the physical location of the injury incident was recorded, 89% occurred at home. Demographics of the older adult population sustaining stair-related upper extremity fractures are summarized in Table 1.
Table 1.
Characteristics of Stair-Related Upper Extremity Fracture Injuries Among Older Adults ≥ 65 Years Old Presenting to Emergency Departments, 2012–2021
| Characteristics | Number of Actual Cases | Weighted National Estimate | % of Weighted Cases | 95% CI |
|---|---|---|---|---|
| Total Injuries | 5,633 | 251,041 | 100.0% | 211,678 – 290,404 |
| Age, yrs | ||||
| 65–74 | 2,678 | 117,774 | 46.9% | 99,307 – 136,241 |
| 75–84 | 2,004 | 90,805 | 36.2% | 74,787 – 106,823 |
| 85–94 | 885 | 39,838 | 15.9% | 31,429 – 48,427 |
| ≥ 95 | 66 | 2,623 | 1.0% | 1,492 – 3,754 |
| Sex | ||||
| Male | 1,348 | 58,717 | 23.4% | 48,359 – 69,075 |
| Female | 4,285 | 192,324 | 76.6% | 162,168 – 222,480 |
| Anatomic Location | ||||
| Proximal humerus | 986 | 43,793 | 17.4% | 34,351 – 53,235 |
| Humeral shaft | 1,542 | 68,002 | 27.1% | 56,006 – 79,998 |
| Elbow | 383 | 16,850 | 6.7% | 12,557 – 21,143 |
| Forearm | 732 | 36,083 | 14.4% | 28,304 – 43,862 |
| Wrist | 1,489 | 63,888 | 25.4% | 52,618 – 75,158 |
| Proximal hand | 233 | 10,246 | 4.1% | 7,635 – 12,857 |
| Finger | 268 | 12,179 | 4.9% | 9,076 – 15,282 |
| Incident Location | ||||
| Home | 3,558 | 160,436 | 63.9% | 135,280 – 185,592 |
| Public Area | 448 | 19,569 | 7.8% | 14,583 – 24,555 |
| Other | 1,627 | 71,035 | 28.3% | 58,504 – 83,566 |
| Disposition | ||||
| Hospitalized | 1,416 | 58,401 | 23.3% | 48,099 – 68,703 |
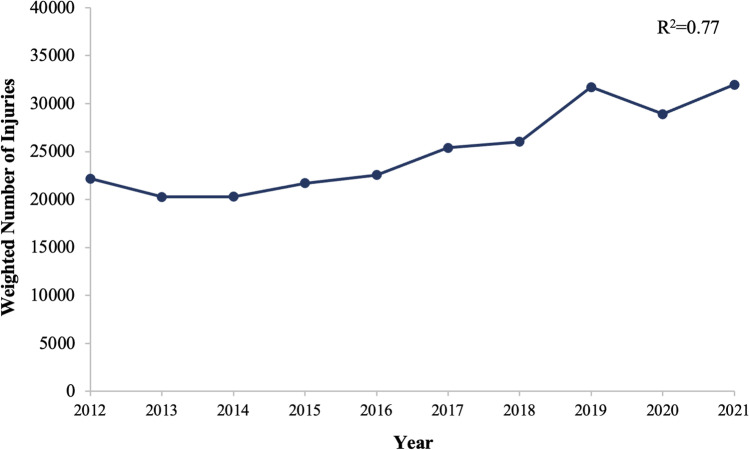
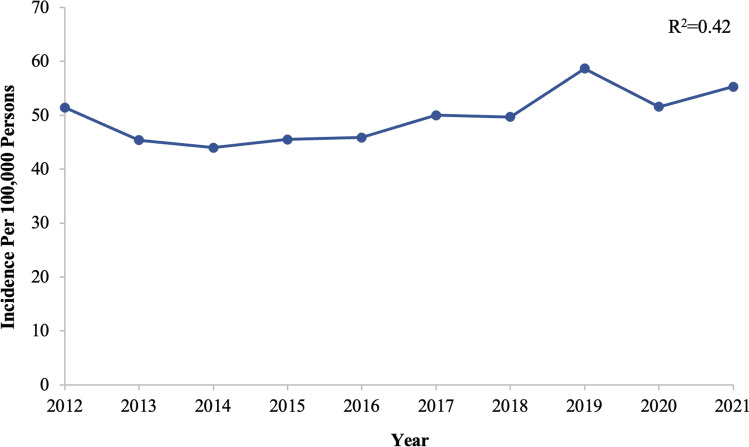
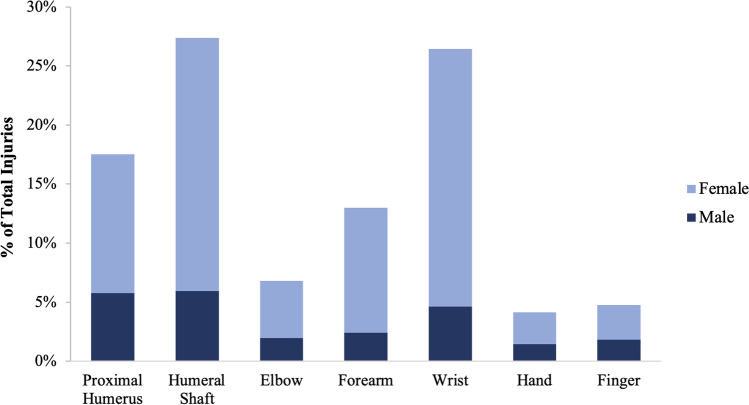
We found a significant increase in the number of reported stair-related upper extremity fractures in older adults (R2 = 0.77, p < 0.001), with an overall 56% increase in UE fractures between 2012 and 2021 (Fig. 1). Using the national estimates of UE stair-related fractures in older adults and the population data from the US Census Bureau IDB, the incidence of these injuries per 100,000 persons aged 65 years and older was also found to significantly increase by 7% in our study period (R2 = 0.42, p < 0.05) (Table 2, Fig. 2). Fractures of the humeral shaft accounted for the majority of UE fractures (27%), followed by the wrist (26%), proximal humerus (18%), forearm (13%), elbow (7%), finger (5%), and hand (4%) (Fig. 3).
Fig. 1.
Weighted National Estimates of Stair-Related Upper Extremity Fractures in Older Adults of the United States from 2012–2021
Table 2.
Incidence of Stair-Related Upper Extremity Fractures in Older Adults from 2012–2021
| Year | Estimated Injuries | Age ≥ 65 Population | Incidence per 100,000 |
|---|---|---|---|
| 2012 | 22,191 | 43,130,363 | 51.45 |
| 2013 | 20,260 | 44,629,455 | 45.40 |
| 2014 | 20,297 | 46,157,016 | 43.97 |
| 2015 | 21,701 | 47,650,770 | 45.54 |
| 2016 | 22,564 | 49,202,071 | 45.86 |
| 2017 | 25,391 | 50,753,404 | 50.03 |
| 2018 | 26,018 | 52,369,339 | 49.68 |
| 2019 | 31,725 | 54,058,263 | 58.69 |
| 2020 | 28,908 | 56,051,566 | 51.57 |
| 2021 | 31,985 | 57,842,422 | 55.30 |
Fig. 2.
Incidence Per 100,000 Persons of Stair-Related Upper Extremity Fractures in Older Adults of the United States from 2012–2021
Fig. 3.
Distribution of Stair-Related Upper Extremity Fractures in Older Adults from 2012–2021 by Fracture Type
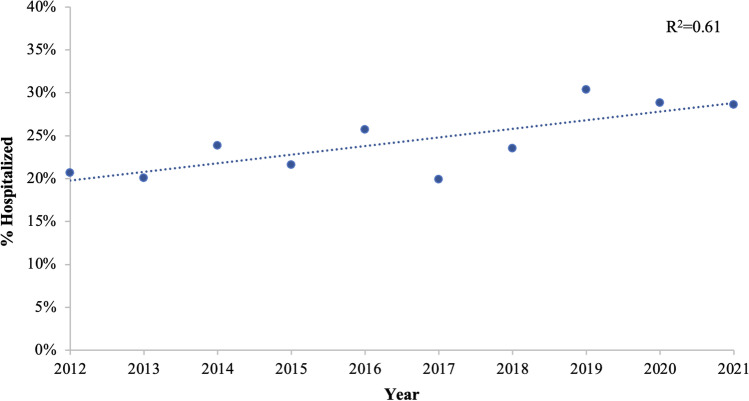
We found a significant increase (38%) in the hospitalization rate (R2 = 0.61, p < 0.01) between 2012 and 2021 (Fig. 4). Multivariable analysis was used to identify variables associated with increased odds for hospitalization from stair-related UE fracture injuries among older adults (Table 3). Males had increased odds of being hospitalized from stair-related UE fractures (OR: 1.36) compared to females. Older age was also associated with increased odds of hospitalization after injury (p < 0.0001). Fractures at specific locations of the upper extremity were associated with increased odds of hospitalization. In comparison to individuals with forearm fractures, individuals with proximal humerus (OR: 1.74), humeral shaft (OR: 1.59), and elbow (OR: 1.67) fractures had increased odds of hospitalization, while individuals with hand (OR: 0.51) and finger (OR: 0.33) fractures had decreased odds of hospitalization.
Fig. 4.
Hospitalization Rate from Stair-Related Upper Extremity Fractures in Older Adults by Year
Table 3.
Multivariate Analysis of Odds for Hospitalization from Stair-Related Upper Extremity Fractures in Older Adults
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Age | |||
| 65–74 | Referent | Referent | |
| 75–84 | 1.38 | 1.20–1.58 | < 0.0001 |
| 85–94 | 2.07 | 1.75–2.45 | < 0.0001 |
| ≥ 95 | 3.13 | 1.90–5.18 | < 0.0001 |
| Sex | |||
| Female | Referent | Referent | |
| Male | 1.36 | 1.18–1.56 | < 0.0001 |
| Fracture | |||
| Forearm | Referent | Referent | |
| Proximal humerus | 1.74 | 1.39–2.19 | < 0.0001 |
| Humeral shaft | 1.59 | 1.29–1.96 | < 0.0001 |
| Elbow | 1.67 | 1.26–2.22 | < 0.0001 |
| Wrist | 0.91 | 0.73–1.14 | 0.427 |
| Hand | 0.51 | 0.34–0.79 | 0.002 |
| Finger | 0.33 | 0.21–0.52 | < 0.0001 |
Discussion
In our study, we sought to determine the incidence and characteristic trends of upper extremity stair-related fractures in the older adult United States population. We found that the upper extremity is the most common fracture site in stair-related injuries and our analysis estimated that there were 251,041 stair-related UE fractures among older adults in the United States between 2012 and 2021. These findings emphasize the importance of developing and implementing effective strategies for the prevention of upper extremity fractures in older adults.
As hypothesized, stair-related UE fracture cases and incidence in older adults are increasing at a significant rate, as we found an overall 56% increase in cases and a 7% increase in incidence per 100,000 persons between 2012 and 2021. Moreover, the associated severity of injury requiring hospitalization is also increasing, with a 38% increase in hospitalization rate over our study period. This increase in the incidence and severity of UE fracture injuries is consistent with existing literature pertaining to the overall incidence of both fragility fractures and stair-related injuries in the United States and other developed countries over the past several decades [5, 9, 13, 14]. A 2018 study by Blazewick et al. found that stair-related injuries across all age categories increased by 24% in the US from 1996 to 2012 [15]. Among these injuries, the stair-related injury rate was highest in adults over the age of 60 years. The cost burden of these fragility fractures highlights the need for improved interventions and clinical care. The overall annual cost of osteoporosis-related fractures in US older adult populations is projected to be $21 billion in 2025, a 48% increase from 2005 [13]. Most research on fragility fractures has focused on hip and vertebral fractures, likely due to the higher relative cost and disability burden of these fractures. However, the significant rise in UE fractures among older adults poses a high cost and disability burden that must be mitigated.
There are multiple possible explanations for the increased incidence and hospitalization rates of stair-related UE fractures among older adults. For the older adult population, bone fragility and the likelihood of falling are the two major risk factors predisposing them to stair-related UE fractures [9]. Many reports indicate that frailty, which is generally described as “a clinical state of increased vulnerability after a stressor event,” has been steadily increasing within the older adult US population, thereby increasing fragility fracture risk [16]. This increase in frailty is due in part to the increasing median age of those in the older adult population (65 + age category) [17]. Osteoporosis, a contributor to frailty and a major risk factor for fragility fractures, has also been on the rise among older adults [9, 18, 19]. While an increase in severity of fracture may explain the increased rates of hospitalization from UE fractures, changing trends in operative management of these injuries may also be a contributing factor. Significant increases have been observed in operative fixation of distal upper extremity fractures over the past several decades [20]. For distal radius fractures, open surgical treatment has been associated with lower complication rates and greater function in comparison to nonoperative treatment modalities [21]. However, closed fixation of stable fractures among older adults remains the consensus for the majority of upper extremity fracture management, including distal upper extremity fractures.
We found proximal upper extremity fractures, particularly those of the proximal humerus, humeral shaft, and elbow, to be at increased odds for hospitalization compared to forearm fractures. Distal upper extremity fractures of the hand and finger were less likely to require hospitalization. The increase in hospitalization associated with proximal upper extremity fractures is likely due to the higher energy needed to create these fractures, therefore, it may also be a marker for concomitant injuries, such as rib fractures. Additionally, hospitalization may be needed after proximal upper extremity fractures to perform acute medical and surgical interventions rather than conservative management. Nonoperative treatment is the preferred treatment modality for moderately displaced humeral fractures and stable radius fractures [21, 22]. However, operative treatment is a beneficial option for the management of more complex humeral fractures, as Sabharwal et al. found that patients treated operatively for these fractures have a higher quality of life [23]. Similarly, Mackenney et al. reported malunion rates up to 50% among older adult patients treated nonoperatively for unstable distal radius fractures [24]. Hospitalization is generally required for more complex fractures and may indicate an increasing trend in the severity of UE fractures among older adults.
Our results indicate that females sustain the vast majority (76%) of stair-related UE fractures. This, too, is consistent with countless fracture-related studies, which indicate a higher fracture incidence for females [4, 5, 7, 10]. It is well-established that women, particularly post-menopausal women, are more susceptible to frailty and osteoporosis [25]. However, we observed that males experiencing stair-related UE fractures were 1.36 times more likely to be hospitalized. It is worth noting that despite having a lower fracture incidence, men tend to have higher mortality associated with fragility fractures [26]. It is, therefore, possible that men sustain more severe stair-related injuries which then warrants hospitalization.
It is also worth noting that 89% of stair-related UE fractures occurred at home in our study. This is consistent with existing literature indicating that most falls among older adults and most fragility fractures occur at home [3]. The majority of stair-related injuries across all age groups also occur at home, according to Blazewick et al., who postulated that women are more likely to sustain stair-related injuries because they statistically spend more time at home [15]. Additionally, as more people stayed in their homes during the COVID-19 pandemic, this may contribute to the rising incidence of UE stair-related fractures seen near the end of the study period. This finding regarding the primary incident location of UE stair-related fractures has important implications for fall-prevention strategies, as one-half of US households contain stairs [27].
The NEISS database is a very useful tool for identifying injuries that present to US emergency departments. As is the case with all database studies, our analysis has many limitations. The NEISS database does not account for injuries addressed outside of EDs, such as in urgent care or outpatient clinics, leading to potential underestimates of UE fracture incidence. The database relies on estimates for incidence rates, thus reducing accuracy. The data may also be impacted by incorrect or incomplete documentation by ED personnel. Additionally, the results may be confounded by associated concomitant injuries that are not recorded in the database. Lastly, it is assumed that most fractures in this study are fragility fractures based on the sample age and stair-related mechanism of injury, however, the database does not categorize fragility and non-fragility fractures separately. Despite these limitations, the NEISS database has significant external validity, and this study contributes key findings to a scarce body of literature on upper extremity fractures among older adults.
As the majority of upper-extremity fractures are caused by falls, fall prevention strategies are a critical next step [28]. A large body of literature already exists regarding fall and fracture prevention for older adults [29]. These measures range from behavioral changes and promotion of better bone health to improved lighting and alterations to the home environment. This study indicates the need for enhanced prevention efforts related to stair design and construction. The biomechanics of falling varies significantly between fracture types [28]. According to Ensrud et al., patients with hip fractures are more likely to report falling sideways, while patients with UE fractures more often report falling backward or forward (and using their arms to break the fall) [9]. People tend to not fall sideways on stairs as the typical movement pattern required is forwards with side walls or railings preventing sideways falls. Evidence-based strategies to improve stair safety include installing handrails that allow the hand to grip all the way around the railing, maintaining uniform stair pattern and geometry, increasing the length of the horizontal surfaces between stair ledges, improving the lighting around stairs, and removing stairway clutter [15]. In addition, policymakers should consider revising home and building codes to maximize compliance with stair-safety recommendations.
Healthcare providers should also direct increased attention toward maintaining optimal functional muscle mass, bone health, balance, and senses among older adult patients. By the age of 40–50 years, notable loss of muscle mass and strength begins to take place, which becomes more significant as one ages. Individuals of older age are at increased likelihood of sustaining subsequent fragility fractures after their first fracture. Resistance exercise training at high intensity has been shown to improve muscle mass and reverse frailty [30]. Diagnosing decreased bone strength and recommending nutritional support or, if needed, pharmacologic agents to prevent further bone loss among those with osteoporosis is also indicated for fragility fracture prevention. Patients older than 60 years are at increased likelihood of sustaining subsequent fragility fractures after their first fracture, making prevention of any initial fracture of the utmost importance [31]. While UE fractures may not appear to have as significant consequences as hip or vertebral fractures, such fractures may be a harbinger of bone weakness and underlying balance, mobility, and gait impairments that should not be overlooked in the clinical setting [7]. Furthermore, older adults may present with a fear of falling after sustaining a fracture that may hinder their daily life. Edwards et al. reported that clinically important functional decline following wrist fractures is similar in magnitude to that associated with diabetes, stroke, and arthritis [32]. Older adults with upper extremity fractures should receive an evaluation for fall risk and treatment for decreased strength, gait impairment, and the fear of falling as needed to prevent subsequent falls and functional decline.
While several studies on fragility fractures have focused on hip and vertebral fractures, the rapidly rising prevalence of UE fractures renders the need for future prospective studies investigating epidemiological trends in UE fractures among older adults. Particular attention should be placed on investigating additional demographics, injury characteristics, risk factors, and efficacy of preventative measures.
Data Availability
The data that supports the findings of this study are publicly available from the United States Consumer Product Safety Commission through the National Electronic Injury Surveillance System database.
Declarations
Ethical approval
For this type of study formal consent is not required.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tinetti ME, Baker DI, King M, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359:252–261. doi: 10.1056/NEJMoa0801748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89:324–332. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blake AJ, Morgan K, Bendall MJ, et al. Falls by elderly people at home: prevalence and associated factors. Age Ageing. 1988;17:365–372. doi: 10.1093/ageing/17.6.365. [DOI] [PubMed] [Google Scholar]
- 4.Sabesan VJ, Valikodath T, Childs A, Sharma VK. Economic and social impact of upper extremity fragility fractures in elderly patients. Aging Clin Exp Res. 2015;27:539–546. doi: 10.1007/s40520-014-0295-y. [DOI] [PubMed] [Google Scholar]
- 5.Kang S-W, Shin WC, Moon NH, Suh KT. Concomitant hip and upper extremity fracture in elderly patients: Prevalence and clinical implications. Injury. 2019;50:2045–2048. doi: 10.1016/j.injury.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 6.Startzell JK, Owens DA, Mulfinger LM, Cavanagh PR. Stair negotiation in older people: a review. J Am Geriatr Soc. 2000;48:567–580. doi: 10.1111/j.1532-5415.2000.tb05006.x. [DOI] [PubMed] [Google Scholar]
- 7.McDonough CM, Colla CH, Carmichael D, et al. Falling down on the job: evaluation and treatment of fall risk among older adults with upper extremity fragility fractures. Phys Ther. 2017;97:280–289. doi: 10.1093/ptj/pzx009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wenzinger E, Rivera-Barrios A, Gonzalez G, Herrera F. Trends in upper extremity injuries presenting to US emergency departments. Hand N Y N. 2019;14:408–412. doi: 10.1177/1558944717735943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ensrud KE. Epidemiology of fracture risk with advancing age. J Gerontol A Biol Sci Med Sci. 2013;68:1236–1242. doi: 10.1093/gerona/glt092. [DOI] [PubMed] [Google Scholar]
- 10.Hemmann P, Ziegler P, Konrads C, et al. Trends in fracture development of the upper extremity in Germany-a population-based description of the past 15 years. J Orthop Surg. 2020;15:65. doi: 10.1186/s13018-020-1580-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boele van Hensbroek P, Mulder S, Luitse JSK, van Ooijen MR, Goslings JC. Staircase falls: high-risk groups and injury characteristics in 464 patients. Injury. 2009;40:884–889. doi: 10.1016/j.injury.2009.01.105. [DOI] [PubMed] [Google Scholar]
- 12.CPSC. National Electronic Injury Surveillance System. US Consum Prod Saf Comm n.d. https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data/Neiss-Frequently-Asked-Questions (Accessed 12 Nov 2022).
- 13.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res Off J Am Soc Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 14.Borgström F, Karlsson L, Ortsäter G, et al. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos. 2020;15:59. doi: 10.1007/s11657-020-0706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blazewick DH, Chounthirath T, Hodges NL, Collins CL, Smith GA. Stair-related injuries treated in United States emergency departments. Am J Emerg Med. 2018;36:608–614. doi: 10.1016/j.ajem.2017.09.034. [DOI] [PubMed] [Google Scholar]
- 16.Buckinx F, Rolland Y, Reginster J-Y, Ricour C, Petermans J, Bruyère O. Burden of frailty in the elderly population: perspectives for a public health challenge. Arch Public Health. 2015;73:19. doi: 10.1186/s13690-015-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bureau UC. The U.S. Joins Other Countries With Large Aging Populations. CensusGov n.d. https://www.census.gov/library/stories/2018/03/graying-america.html (accessed November 11, 2022).
- 18.Sarafrazi N (2021) Osteoporosis or Low Bone Mass in Older Adults: United States, 2017–2018. National Center for Health Statistics. 10.15620/cdc:103477.
- 19.Reginster J-Y, Burlet N. Osteoporosis: a still increasing prevalence. Bone. 2006;38:S4–9. doi: 10.1016/j.bone.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 20.Patel AA, Buller LT, Fleming ME, Chen DL, Owens PW, Askari M. National trends in ambulatory surgery for upper extremity fractures: a 10-year analysis of the US National Survey of Ambulatory Surgery. Hand N Y N. 2015;10:254–259. doi: 10.1007/s11552-014-9703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mauck BM, Swigler CW. Evidence-based review of distal radius fractures. Orthop Clin North Am. 2018;49:211–222. doi: 10.1016/j.ocl.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Navarro CM, Brolund A, Ekholm C et al (2018) Treatment of humerus fractures in the elderly: A systematic review covering effectiveness, safety, economic aspects and evolution of practice. PLOS ONE 13:e0207815. 10.1371/journal.pone.0207815 [DOI] [PMC free article] [PubMed]
- 23.Sabharwal S, Patel NK, Griffiths D, Athanasiou T, Gupte CM, Reilly P. Trials based on specific fracture configuration and surgical procedures likely to be more relevant for decision making in the management of fractures of the proximal humerus: Findings of a meta-analysis. Bone Jt Res. 2016;5:470–480. doi: 10.1302/2046-3758.510.2000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]
- 25.Alswat KA (2017) Gender Disparities in Osteoporosis. J Clin Med Res 9:382–387. 10.14740/jocmr2970w [DOI] [PMC free article] [PubMed]
- 26.Migliorini F, Giorgino R, Hildebrand F, et al. Fragility fractures: risk factors and management in the elderly. Medicina (Mex) 2021;57:1119. doi: 10.3390/medicina57101119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bureau UC. American Housing Survey. CensusGov 2021. https://www.census.gov/programs-surveys/ahs/about.html (Accessed 12 Nov 2022)
- 28.Palvanen M, Kannus P, Parkkari J, et al. The injury mechanisms of osteoporotic upper extremity fractures among older adults: a controlled study of 287 consecutive patients and their 108 controls. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2000;11:822–831. doi: 10.1007/s001980070040. [DOI] [PubMed] [Google Scholar]
- 29.Santy-Tomlinson J, Speerin R, Hertz K, Tochon-Laruaz AC, van Oostwaard M (2018) Falls and Secondary Fracture Prevention. In: Hertz K, Santy-Tomlinson J, editors. Fragility Fract. Nurs. Holist. Care Manag. Orthogeriatric Patient, Springer, Cham [PubMed]
- 30.Coll PP, Phu S, Hajjar SH, Kirk B, Duque G, Taxel P. The prevention of osteoporosis and sarcopenia in older adults. J Am Geriatr Soc. 2010;69:1388–1398. doi: 10.1111/jgs.17043. [DOI] [PubMed] [Google Scholar]
- 31.Sriruanthong K, Philawuth N, Saloa S, Daraphongsataporn N, Sucharitpongpan W (2022) Risk factors of refracture after a fragility fracture in elderly. Arch Osteoporos 17:98. 10.1007/s11657-022-01143-4 [DOI] [PubMed]
- 32.Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA (2010) Functional decline after incident wrist fractures--Study of Osteoporotic Fractures: prospective cohort study. BMJ 341:c3324. 10.1136/bmj.c3324 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that supports the findings of this study are publicly available from the United States Consumer Product Safety Commission through the National Electronic Injury Surveillance System database.