Abstract
Aim
To explore the perspectives, experience, and concerns of patients with irritable bowel syndrome (IBS) in China.
Methods
We used data mining to investigate posts shared in Baidu Tieba concerned with IBS; we collected the data through the crawler code, and mined the cleaned data’s themes based on Latent Dirichlet allocation (LDA) and the Grounded theory.
Results
We found 5746 network posts related to IBS. LDA analysis generated 20 topics, and grounded theory analysis established eight topics. Combining the two methods, we finally arranged the topics according to five concepts: difficulty in obtaining disease information; serious psychosocial problems; dissatisfied with the treatment; lack of social support; and low quality of life.
Conclusion
Social media research improved patient-centric understanding of patients’ experiences and perceptions. Our study may facilitate doctor-patient communication and assist in the formulation of medical policies.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11136-023-03417-x.
Keywords: Irritable bowel syndrome, Latent Dirichlet allocation, Grounded theory, Social media
Introduction
Irritable bowel syndrome (IBS) is a prevalent functional gastrointestinal disorder characterized by chronic abdominal pain and altered bowel habits [1].The prevalence of IBS within the community is between 10 and 25% [2–4]. Meta-analysis shows global IBS prevalence at 11.2% [5]. The prevalence of IBS among Asian communities appears to be on the rise, especially in China [6]. Our previous survey of medical and engineering students in Zhejiang Province, China founded that among 1870 participants, based on Rome III criteria, 129 were diagnosed as having IBS—an overall incidence of 6.90% [7].
The pathophysiology of IBS is incompletely understood [8]. Its diagnosis is based on symptoms. Therefore, despite the high prevalence, there is a lack of established therapeutic options. IBS has a substantial impact on people's health and well-being; hence it has with considerable socioeconomic consequences [9]. A study conducted in the US showed that IBS affects 10–15% of adults in that country, and is associated with significant impairment in health-related quality of life (HRQoL) [10]. Another survey, from Singapore, indicated that IBS sufferers were significantly affected in mobility, anxiety and depression, usual activity and pain [11]. There was a significant correlation between symptom intensity of IBS and deterioration of quality life (emotional health, mental health, energy, physical function, physical role, social role) [12, 13]. Society and culture may influence the expression and interpretation of IBS [14, 15]. A study on cross-cultural differences concerning IBS compared patients’ intestinal symptom scale scores in eight countries, and the results showed significant differences in scores among countries, with Chinese patients ranking first and second in diarrhea and pain scores, respectively [16]. Recently, a team at Rome Foundation proposed that future studies of IBS should focus on regional and cross-cultural differences that are more likely to shed light on pathophysiology [17, 18]. It is particularly important to pay attention to patients with IBS according to different cultural backgrounds because it may reveal heterogeneity among nations concerning IBS research and management.
Chinese culture is strongly influenced by Confucianism and shows intrinsic sociocultural values which differ greatly from Western cultures. Previous studies from the perspective of patients with IBS, highlighted participants’ frustration [19], social isolation [9], and dissatisfaction with medical care [20]. A survey in the US indicated that 68% of IBS patients would tell their partners about their condition, and 56% would tell other family members [9]. Another American survey found that IBS patients used more than 218 different medical methods to reduce symptoms, including prescription drugs, over-the-counter drugs, herbal medicine and diet therapy, but many were still dissatisfied with the treatments [20]. Besides, patients often have insufficient knowledge of IBS, thinking for example, that IBS may cause cancer [21]. Additionally, several studies have found that patients and doctors are often inconsistent in their understanding of etiology and judgments of severity, treatment and efficacy [20–22]. However, similar studies from China are lacking. Thus, there is a growing need to understand the experience of IBS patients in Chinese culture and their perspectives on factors contributing to the condition’s severity.
Patients have gradually come to rely on the internet. An increasing number of patients, search online for relevant information before seeing a doctor, or they obtain medical services through the internet [23]. A study in the US found that 59% of users search for health information on the internet [24]. Social media play an especially important role for many people, including adolescents [25], pregnant women [26], and college students [27]. This is especially true since the onset of COVID-19 pandemic [28]. Social media allows researchers to better understand patients, especially among China’s 800 million internet users. For this study, we collected IBS-related posts from Chinese social media and explored patients’ experiences, perceptions, needs, and difficulties to patients to provide a panoramic view, based on the perspective of social media, of their feelings concerning IBS.
Materials and methods
Study design
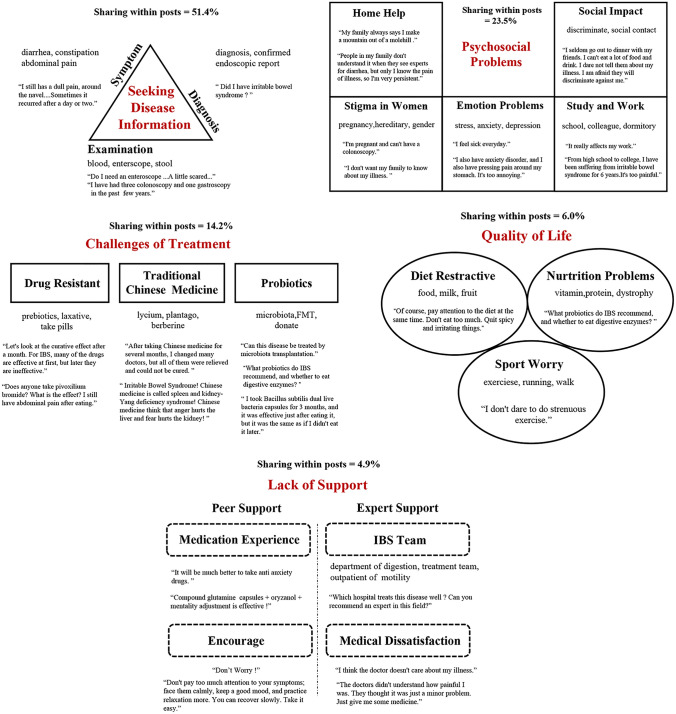
Baidu Tieba (https://tieba.baidu.com) is the largest Chinese online community; like Reddit, it consists of a variety of subcommunities addressing topics and gathers massive user groups with different interests. IBS-Bar is a sub-bar of Baidu Tieba and forms a community for IBS patients to communicate and discuss. As of May 20, 2022, the IBS-Bar had more than 10,000 followers and more than 150,000 posts and replies. The massive amount of user data generated in this open community is of great significance for analyzing IBS patients’ experiences and perceptions. In this study, we mined posts from across the IBS-Bar’s history (12 years). After data cleaning, latent Dirichlet allocation (LDA) topic modeling and grounded theory were used to explore the themes and understand the experiences and perceptions of IBS patients based on the perspective of social media. The workflow is presented in Fig. 1.
Fig. 1.
Flow chart of the study
Our study team was made up of clinicians and nursing staffs. Three members (SS, JC, and LC) had received qualitative analysis training, and two members (HL and YJ) had experience in data mining; BL was a clinical expert concerning IBS. Trustworthiness of the data was established through triangulation and peer checking. Research triangulation was used to verify the accuracy of the coding process. In peer checking, two gastroenterologists assessed and confirmed the congruence between the raw data and the generated code and categories. The Standards for Reporting Qualitative Research (SRQR) [29] has been followed, and the checklist was completed (see Supplemental File 1: SRQR checklist).
Data collection and cleaning
All user posts (including comments and replies to posts) were written in Chinese and published online between December 6, 2009, and May 20, 2022.
By using the ‘request’ and ‘selenium’ packages and fast web crawling based on Python, we extracted the required data from web pages. A total of 26,419 records were collected. Subsequently, each post, with corresponding comments and replies, was combined into a single document for further analysis.
To assure the quality of the data, we removed blank lines, duplicate text, special symbols, numbers, and letters from the text, further eliminating texts with string lengths of less than 10, and retaining only Chinese strings. Additionally, we manually reviewed all posts and excluded advertised posts and posts unrelated to IBS. Finally, a total of 5746 posts were used for further analysis.
LDA topic model
According to Blei et al. [30], LDA is a probability-based topic model algorithm. It assumes that documents are generated based on a certain number of topics and that a given number of topics can be extracted from a corpus containing a certain number of documents [31]. In this study, we used 5746 posts as documents for further analysis. Each post was treated as a document.
In this study, a useful Python kit call ‘Jieba’ was first adopted to segment the Chinese sentences into separate terms. The second step was the deletion of stop words whose meanings could not be recognized from the word segmentation. Finally, we combined synonyms and phrases. Coherence scores were taken into consideration to determine the number of topics. Topic coherence is the most effective method of measuring the quality of topics; higher scores represent the most appropriate number of model topics [32]. After the optimal number of topics was determined, an LDA model was implemented using Gensim [33], a package that includes LDA. According to Gensim, “alpha” and “eta” are hyperparameters that affect sparsity of the topics and both defaults to 1.0/num_topics prior. Another Python package, ‘pyLDAvis’, was adopted to visualize the topic extraction results.
Finally, we went through representative clusters of terms and examined the most representative posts to define the topics.
Grounded theory
Once the posts were identified, we randomly selected 200 posts and used the grounded theory methods for analysis, as described by Charmaz [34]. This number was chosen based on the work experience of Gonzalez et al. [24], to achieve thematic saturation, meaning the point at which themes begin to be repeated.
Grounded theory is an iterative, hypothesis-generating approach that emphasizes the generalization or emergence of information from data to establish a theory or model [35, 36].Content analysis of data involved three stages: open coding, creating categories, and abstracting [37]. In the first stage, two investigators individually coded line-by-line to identify prominent issues and concepts. Then, we reviewed the codes and incorporated them into coding categories, which are groups of similar concepts and themes. Lastly, abstraction of sub-categories and generic categories was conducted in discussion among all authors, resulting in main categories that provided an overall description of patients’ perspectives. Data analysis was completed using NVivo12 Plus software [38].
Mixed methods
The analysis of big data text based on grounded theory and LDA topic modeling has been recognized by many researchers [39–41], and the consistency of its results has also been verified. LDA helped us to synthesize a large amount of data, while grounded theory enabled us to verify identified themes and to more closely analyze the data. In this study, two researchers trained in qualitative techniques conducted analyses, comparing, contrasting, and combining topics from LDA, with themes from grounded theory to confirm similarities and differences. The final results were confirmed by the team’s IBS clinical experts.
Ethics
All datasets were taken from Baidu Tieba, a publicly available website. Ethical approval was not required for the secondary analysis of publicly available data.
Results
LDA topic model analysis
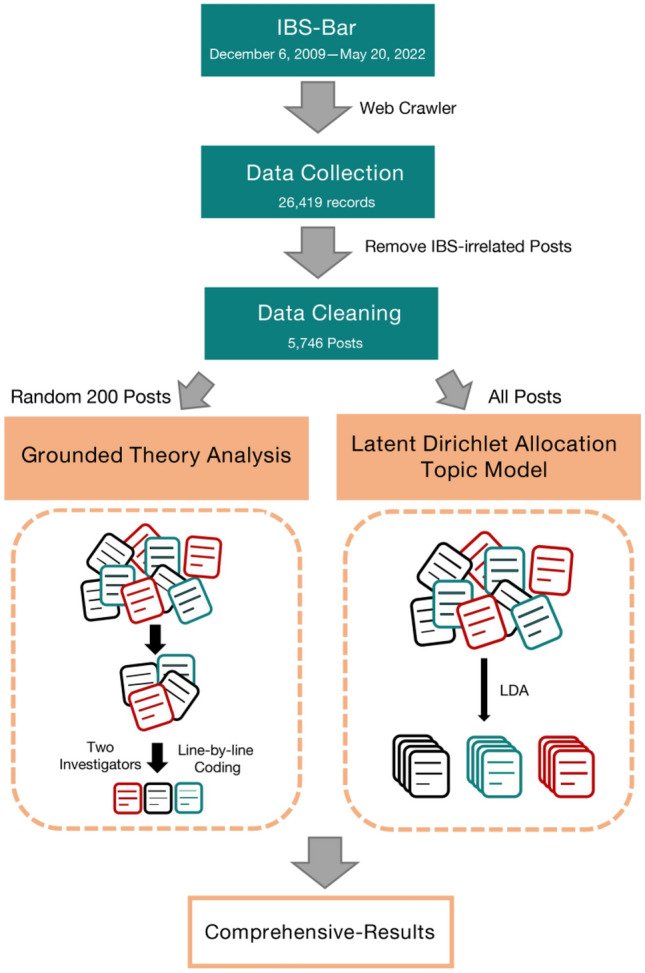
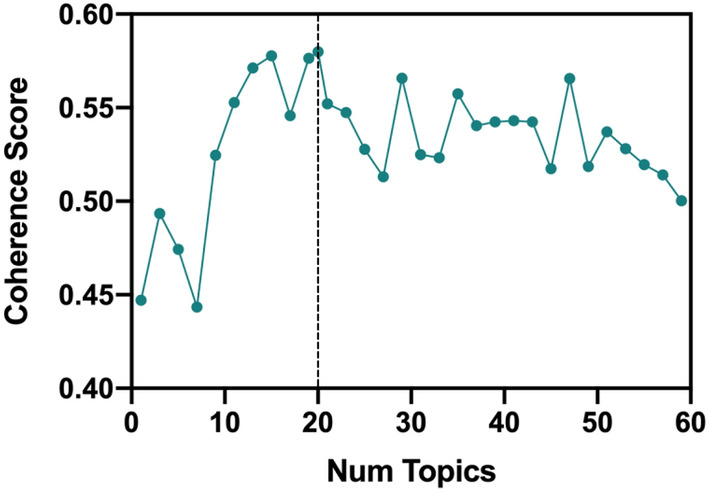
We studied 5746 high-quality posts from Chinese social media that focused on IBS. Due to the restrictions concerning user privacy and internet information protection policies, there was no demographic information related to the data. Building on previous research that found 10–30 topics [42–44], but also considering smaller and larger topic numbers, consistency scores were calculated from 1 to 60 topics to obtain the optimal number of topics (Fig. 2). While K = 16, 17, and 19 also show high scores for coherence, we tend to choose a larger K value in order to ensure the breadth and depth of posts. This was confirmed after comprehensive consideration and thus a total of 20 topics were identified (Fig. 3). More details and reasons for model selection can be founded in Supplementary file 2.
Fig. 2.
Coherence scores for different numbers of topics
Fig. 3.
Intertopic distance map
Table 1 shows the representative term cluster with each term’s prevalence and assigned topic. The most common topic of the posts focused on discussions surrounding diagnosis and symptoms (mean share within posts = 24.2%), followed by topics on examination (13.7%) and diagnosis (13.5%). Discussions on mechanisms were also found as a separate but rather low-prevalence topic (1.7%). We also found one topic on emotional problems, the fourth most prevalent in the corpus (12.2%). Another two topics featured expressions of concern about drugs (10.1%) and complaints about life (10%). Four low-prevalence topics paid attention to medication experience (3.7%), alert symptoms (2.5%), Traditional Chinese medicine (TCM) (2.8%), and probiotics (1.3%). The remaining topics with low prevalence were distributed in peer support (0.8%), diet (0.8%), sport (0.6%), women (0.5%), nutrition (0.3%), social impact (0.4%), expert support (0.4%), study and work (0.4%), and nutrition (0.3%).
Table 1.
Representative term cluster with prevalence and assigned topic
| Representative term cluster | Prevalence (%) | Topic |
|---|---|---|
| IBS, diarrhea, abdominal pain, symptoms, weight, constipation, chronic, toilet, tingling, prickling, halitosis, alternate, navel | 24.2 | Symptoms |
| Examination, enteroscope, stool, small bowel, blood routine, calprotectin, ulcer, uric acid, gastroscope, empyema, gastrointestinal tract | 13.7 | Examination |
| Diagnosis, confirmed, endoscopic report, criteria | 13.5 | Diagnosis |
| Spirit, mood, nervous, stress, anxiety, psychological, pain, depression, tired, discouraged, fear, adversity, shame, burden | 12.2 | Emotional problems |
| Take pills, cure, solve, loperamide, lansoprazole, laxative, sleeping pill, ineffective, resistant, gradually, wrong, invalid, futile | 10.1 | Drug resistant |
| Life quality, sleep, morning, catch cold, night, after meal, air-conditioning, attention, restricted diet, hobby, entertainment | 10 | Individuals’ lives |
| Experience, medicine, effective, side effect, course, curative effect, useless, valid, standard, health products, Flupentixol and Melitracen Tablets, prebiotics, | 3.7 | Medication experience |
| Traditional Chinese Medicine, chines herbology, Recuperate, Lycium barbarum L, citri reticulatae pericarpium, dried ginger, Chinese jujube, plantago, saponism, ginger | 2.8 | Traditional Chinese medicine |
| Recrudescence, polyp, tumor, bleed, occult blood, organic, functional, angiography, positive signs, bacteria, colitis, allergy, hemorrhoids | 2.5 | Alarming symptoms |
| Inhibitory effect, Mechanism, Mast cell, inflammation, release, immune system, visceral sensitivity, sensitive, | 1.7 | Mechanism |
| Fecal Microbiota Transplantation, indication, effect, fecal bank, eradicate, donate, clinical experiment | 1.3 | Probiotics |
| Fellow sufferer, advice, give up, backer, share, method, healthy, communicate, Wechat group, hope, post | 0.8 | Peer support |
| Diet, fruit, milk, yoghurt, egg, flour, dinner, drink, tea with milk, bland diet, breakfast, lunch, vegetables, seafood | 0.8 | Diet |
| Sport, sweat, running, basketball, aerobic exercise, swimming, fitness, heart, walk, bike | 0.6 | Sport |
| Pregnancy, human milk, lactation, women, hereditary, menstruation, family, child, mother, sexual intercourse, gender | 0.5 | Women |
| Social contact, humble abode, inferiority, trouble, estranged, discrimination, stigma, friend, awkward | 0.4 | Social impact |
| Expert, doctor, hospital, Beijing, Shanghai, outpatient service, Peking Union Medical College, consult, hospitalization, recommend, third-class hospitals, popularization of science | 0.4 | Expert Support |
| Work, study, friend, go to school, work, colleague, occupation, dormitory, ridicule, community, night shift, stay up to late | 0.4 | Study and Work |
| Nutrition, dystrophy, weight, wasting, hunger, appetite, vitamin, protein, smoke, alcohol | 0.3 | Nutrition |
| Culture, season, reimbursement, country, resistance, progress | 0.2 | Others |
Grounded theory
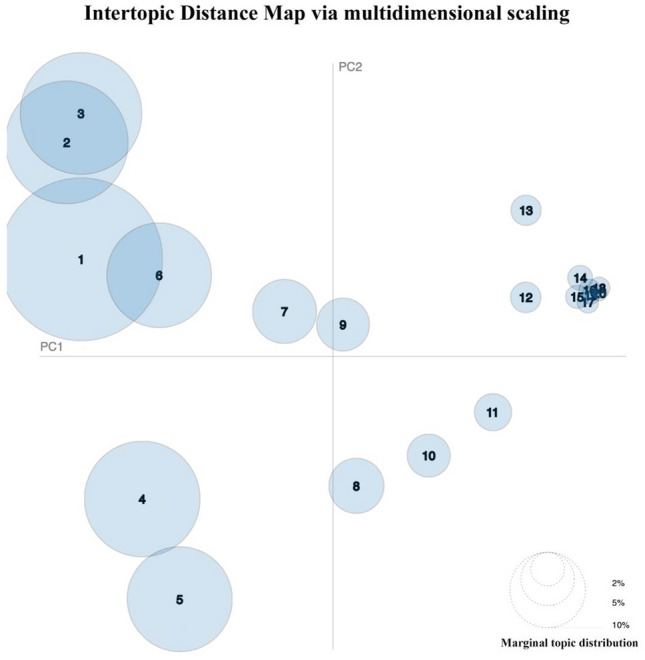
During data analysis using grounded theory, we identified eight preliminary themes related to IBS patients’ experiences and perception (Fig. 4): (i) Seeking disease information, (ii) Drug resistant/ drug ineffective, (iii) Lack of Home help, (iv) Avoiding social events, (v) Stigma in Women with IBS, (vi) Traditional Chinese Medicine, (vii) Seeking professional IBS hospitals/doctors, and (viii) Desire to improve quality of life.
Fig. 4.
Themes identified using mixed methods
Most of the topics encoded using grounded theory had been established in LDA topic modeling. However, grounded theory allowed us to be more explicit about patient attitudes, concerns, and perspectives. Besides, an additional important topic was found in our coding analysis: stigma in women with IBS. (e.g., “I don't want my family to know about my illness. I feel a little embarrassed”).
Table 2 showed the process from codes to categorization using grounded theory. Coding tree presented complete main, generic, and sub-categories derived through the inductive content analysis process (Supplementary Fig. 1).
Table 2.
Examples of coding processes using grounded theory
| Meaningful unit | Code | Sub-category | Generic category | Main category |
|---|---|---|---|---|
| ‘I still has a dull pain, around the navel…Sometimes it recurred after a day or two.’ | Abdominal pain | Symptom of IBS | Asking about the symptoms and diagnosis | (i) Seeking disease information |
| ‘I need to flush into the toilet every morning, and repeat it many times.’ | Diarrhea | |||
| ‘I have done many enteroscopy examination because of abdominal pain.’ | Enteroscopy | Diagnosis of IBS | ||
| ‘I went to the hospital for abdominal pain and performed an abdominal CT scan.’ | Abdominal CT | |||
| ‘My family never thought it was a problem.’ | Overlook of family | Family ignored needs | Attitude of families | (v) Lack of home help |
| ‘My parents think this is common gastrointestinal symptoms.’ |
Results of mixed methods
Themes were generated using LDA and compared to the themes identified in the grounded theory analysis. We identified five themes with several subthemes, all of which are summarized in Fig. 4.
The most common theme (mean share within posts = 51.4%) were focused on seeking disease information, followed by psychosocial problems (23.5%), such as difficulties in studying and working, lack of support at home, impaired social relations, and emotional problems. Besides, some populations, such as women, were particularly worried about pregnancy, genetics, and other issues. Treatment-related challenges were another serious problems (14.2%). Chinese IBS patients were disappointed with drug resistance but had high hopes for TCM and microbiota treatment. The remaining two low-prevalence themes focused on quality of life (6%) and lack of support (4.9%).
Discussion
A patient's perception of disease and medical treatment is at the core of medical practice [45]. Patients' emotions and life challenges are often more important than the physical discomfort caused by the IBS [19].There has been increased scientific attention to understand the nature of medical disorders from the patient’s perspectives. Patients with IBS often experience symptoms for many years, with an average duration of 10 years or more [46]. There has been an underestimation of the impact of IBS on an individual's functioning and quality of life (QoL) [47]. When IBS patients show up at outpatient clinics, physicians intuitively assess symptoms’ severity to plan diagnostic evaluation and treatment recommendations [48], however, evidence suggests that physician-determined prevalence of moderate and severe IBS has been underestimated [49, 50]. Thus, severity of IBS must be based on the patient’s experience. Currently, little is known concerning how to define or understand, from the patient’s perspective, factors contributing to severity. Our research summarized posts on IBS-Bar over 12 years, and we conducted a comprehensive analysis in order to fully understand the patients’ perspective, experience, and concerns.
Patients always seek information related to a specific illnesses or disease [51]. In our study, seeking disease information is a major concern, when it comes to IBS. IBS, as one kind of functional bowel disorder, contains four subtypes [52]. In our study, the two main symptoms that troubled patients were abdominal pain and diarrhea. The results were consistent with previous studies. These people posting these descriptions wanted to know if they could be diagnosed with IBS. A survey of 29 international experts showed that 53% believed bloating was the most important feature of IBS patients; abdominal pain was agreed by only 25% of the experts [53]. The Rome IV diagnostic criteria only lists abdominal pain as the main symptom of IBS [54], but Chinese experts believe that both abdominal distension and abdominal discomfort should be included in the definition of IBS [55]. It is therefore more likely that a problem of overdiagnosis leads to unnecessary, repeated medical treatment and psychological effects. Besides, we found some posters thought they had IBS, although they hadn’t been to the hospital for a diagnosis. Worldwide, 30–70% of patients with IBS visit a doctors, with an overall visit rate of 40% [56]; however, the rate is only 22% in China [57]. Thus, China’s IBS patients may tend to self-diagnose rather than seek medical diagnoses. This could possibly introduce treatment error because self-medication is strongly related to self-diagnosis [58].
In our study, psychosocial problems marked the second-largest group of themes mentioned by Chinese patients with IBS. In a US population-based survey, IBS led to a mean of 0.8 missed days and 4.9 days’ disrupted productivity per month [59]. Another American study showed that in addition to significantly interfering with normal work, IBS caused people to miss out on leisure and on social interaction [19]. In addition, some posters felt that family members did not fully understand their distress. This indicates that Chinese patients with IBS cannot get good help at home. This finding differs from previous studies [9]. We speculate that it may be related to cultural background, because Chinese families may lack suitable atmosphere for direct emotional expression [60]. Various kinds of help or assistance from family, friends, and others were described as social support. In our study, emotional problems were another major category of problems patients had with self-expression. Some individuals reported distress, anxious and depression, even thoughts about death. According to evidence, disordered gut-brain interaction is one of the causes of IBS [61]. Depression, anxiety, and somatoform disorders are the most common psychiatric diagnoses in IBS [62]. Several previous studies from China have shown that patients with IBS are associated with psychosomatic abnormalities, and neuromodulators can improve gastrointestinal symptom [63, 64]. It is worth noting that some groups, such as women tended to experience greater with IBS. Some female patients often expressed a sense of stigma in their posts. It made them feel embarrassed to tell anyone about their symptoms, even their husbands or family members. A study by Toner et al. found that bowel functioning becomes a source of shame and embarrassment for more women compared to man [65]. In a sex-related study of IBS, Björkman and colleagues concluded that women and men experience IBS differently because of their different roles in society [66]. Besides, some women, especially pregnant if they are pregnant, worry that IBS may be passed on to their children. Some pregnant women do not dare to take any medicine for fear of affecting their children.
Treatment of IBS remains a challenge [67]. Many patients approve drugs’ efficacy on their initial use, but after an initial period, drugs lose their effects. This leads patients to switch medicines repeatedly and keep seeking other treatments. A survey in the United States found that patients with IBS were treated using 281 different medical methods; less than a third of the patients were satisfied with the effects, and two fifths expressed very dissatisfaction [20]. Frequent changes of doctors and discontinuations of treatment are also quite common for patients with IBS [68]. Current therapies based on adjusting the gut microbiome mainly include probiotics and fecal transplantation. Our study shows that Chinese patients with IBS have high hopes for both. Recent studies suggest a role for such alterations in gut microbiota [69, 70]. Multiple meta-analyses have provided evidence for the beneficial effects of probiotics in IBS treatment, including mitigation of abdominal pain, bloating, and overall symptom scores [71]. However, not all probiotics exhibit beneficial effects, and it is not clear which probiotics are the most beneficial. Similarly, a study of Fecal Microbiota Transplantation (FMT) in patients with moderate-to-severe IBS-D or IBS M showed that 3 months after transplantation, IBS symptoms were significantly improved in the FMT group compared with the placebo group. The remission rate was significantly higher in the FMT group than in the placebo group (65% vs. 43%) [72]. Since then, numerous other studies have been carried out, but in a recent meta-analysis, it was shown that FMT did not significantly alleviate patients’ clinical symptoms of IBS, and the results were highly heterogeneous [73]. While probiotics and FMT treatment are still in the early stages of research, their specific efficacy is still being repeatedly verified.
Peer support provides a unique perspective of shared experience that can instill hope and assist other patients [74, 75]. Although many posts referenced experience of treatment and encouraged others to seek treatment, many patients still hoped for more experience of medication, side effect, efficacy, and so forth. However, peer support may disseminate inaccurate information. Numerous studies have shown that peer-support providers find the transition from “patients” to “provider” challenging [76, 77], suggesting that providers of peer support may need training before they can play their new role well. The severity of IBS cannot be determined objectively because symptoms are subjective [19]; thus, expert support based on rich experience, is necessary. In our study, some individuals complained about their terrible experience during medical visits. They felt that their condition was not fully understood or taken seriously by doctors. A similar situation has appeared in other studies [78]. In addition, some posts revealed there are people who don’t think they are getting professional treatment. This indicates a need for more professional functional gastroenterologists to meet patients’ needs in China.
IBS can have a substantial effect on a person’s quality of life. Studies have shown that the patients’ quality of life is significantly lower with IBS than with organic diseases, such as diabetes and gastroesophageal reflux disease [10]. Our study found that diet, sport, and nutrition were serious concerns for patients with IBS. Some posts suggested that the doctors can't give specific dietary advice; patients can only grope and record observations by themselves. This also makes them worry about their own nutritional problems. Diet plays an important role not only in the treatment of IBS, but also as a tool that improves symptoms and quality of life [79]. Recent studies show that low-FODMAP diet alleviated bloating, flatulence, diarrhea, and global symptoms in 50%-80% of patients with IBS [80]. Some patients believe that IBS prevents them from exercising vigorously. In fact, increased physical activity improves GI symptoms in patients with IBS [81, 82] and may be used as a primary modality for treatment of IBS [83]. The evidence indicates that Chinese patients with IBS still risk making cognitive errors and need more health education.
This study combined grounded theory with LDA topic modeling, the former a qualitative approach and from interpretive social science [84] and the latter a quantitative approach from natural language processing. This allowed us to process massive quantities of data and to maintain the linguistic, contextual, and interpretive insight that can only come from human reading [39]. Compared to a solely quantitative analysis, a qualitative approach can realize deep insights from textual data. Although qualitative research requires more manpower and time, it is worthwhile because it enables us to find topics that may be ignored during the LDA analysis. In addition, we were able to compare themes derived using each method to ensure consistency in capturing the breadth and depth of online discussions.
There remain limitations concerning this study. Some of the posts included in the analysis may have been made by people with gastrointestinal symptoms, which may not be due to IBS. Data quality would be improved if the posts could be identified by a machine learning classifier. Of course, this still needs further research. Moreover, Our study ignored patients with IBS, who were not users of social media. Further, Our study focused on Chinese patients, thus lacking comparative data on patients from other cultural backgrounds. It is worth noting that all the data in this study were based on the network. Compared with traditional interview methods, it remains unknown whether the methods adopted in this article reach the required data depth. Hopefully some of our peers will do more work in this regard. In addition, member checks were not completed as part of this study. Since this is based on data from social media sources, we would not have been able to get timely feedback from participants to correct our themes.
Conclusion
Patients’ experience of IBS, and their perceptions of the condition, have important clinical and public health implications. To better understand these implications, our study turned to social media. The results shed light on the needs and difficulties of Chinese patients with IBS: difficulty in obtaining disease information; serious psychosocial problems; dissatisfaction with the treatment; lack of social support, and low quality of life. This study can help medical staff predict the thoughts and concerns that IBS patients may have during the treatment process, facilitate doctor-patient communication, and assist in the formulation of medical policies.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors of this study express their heartfelt thanks to the data provided by Baidu Tieba. This study received funding from National Science Foundation of China and Zhejiang Provincial Nature Foundation of China. The funders had no role in study design, data collection and analysis, and interpretation of the results.
Author contributions
SS, and JC wrote the main manuscript text; SS and HL analyzed the data; YL and LC prepared the figures; BL designed this study and revised the article.
Funding
This publication was funded by National Science Foundation of China (Grant no. 81970470), the Zhejiang Provincial Nature Foundation of China (Grant no. LQ21H030001) and the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (Grant no. 2021KY828).
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Competing interest
The authors declare no competing interests.
Ethical approval
All datasets were taken from Baidu Tieba, a publicly available website. Ethical approval was not required for the secondary analysis of publicly available data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shaopeng Sun and Jiajia Chen have contributed equally to this work.
References
- 1.Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clinical Epidemiology. 2014;6:71–80. doi: 10.2147/CLEP.S40245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson S, Roberts L, Roalfe A, Bridge P, Singh S. Prevalence of irritable bowel syndrome: A community survey. British Journal of General Practice. 2004;54(504):495–502. [PMC free article] [PubMed] [Google Scholar]
- 3.Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: An international survey of 40,000 subjects. Alimentary Pharmacology & Therapeutics. 2003;17(5):643–650. doi: 10.1046/j.1365-2036.2003.01456.x. [DOI] [PubMed] [Google Scholar]
- 4.García Rodríguez LA, Ruigómez A, Wallander MA, Johansson S, Olbe L. Detection of colorectal tumor and inflammatory bowel disease during follow-up of patients with initial diagnosis of irritable bowel syndrome. Scandinavian Journal of Gastroenterology. 2000;35(3):306–311. doi: 10.1080/003655200750024191. [DOI] [PubMed] [Google Scholar]
- 5.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clinical Gastroenterology and Hepatology. 2012;10(7):712–721.e4. doi: 10.1016/j.cgh.2012.02.029. [DOI] [PubMed] [Google Scholar]
- 6.Gwee KA, Lu CL, Ghoshal UC. Epidemiology of irritable bowel syndrome in Asia: Something old, something new, something borrowed. Journal of Gastroenterology and Hepatology. 2009;24(10):1601–1607. doi: 10.1111/j.1440-1746.2009.05984.x. [DOI] [PubMed] [Google Scholar]
- 7.Chu L, Zhou H, Lü B, Li M, Chen MY. An epidemiological study of functional bowel disorders in Zhejiang college students and its relationship with psychological factors. Zhonghua Nei Ke Za Zhi. 2012;51(6):429–432. [PubMed] [Google Scholar]
- 8.Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. The Lancet. 2020;396(10263):1675–1688. doi: 10.1016/S0140-6736(20)31548-8. [DOI] [PubMed] [Google Scholar]
- 9.Hungin AP, Chang L, Locke GR, Dennis EH, Barghout V. Irritable bowel syndrome in the United States: Prevalence, symptom patterns and impact. Alimentary Pharmacology & Therapeutics. 2005;21(11):1365–1375. doi: 10.1111/j.1365-2036.2005.02463.x. [DOI] [PubMed] [Google Scholar]
- 10.Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology. 2000;119(3):654–660. doi: 10.1053/gast.2000.16484. [DOI] [PubMed] [Google Scholar]
- 11.Wang YT, Lim HY, Tai D, Krishnamoorthy TL, Tan T, Barbier S, Thumboo J. The impact of irritable bowel syndrome on health-related quality of life: A Singapore perspective. BMC Gastroenterology. 2012;12:104. doi: 10.1186/1471-230X-12-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hahn BA, Kirchdoerfer LJ, Fullerton S, Mayer E. Patient-perceived severity of irritable bowel syndrome in relation to symptoms, health resource utilization and quality of life. Alimentary Pharmacology & Therapeutics. 1997;11(3):553–559. doi: 10.1046/j.1365-2036.1997.00160.x. [DOI] [PubMed] [Google Scholar]
- 13.Cañón M, Ruiz AJ, Rondón M, Alvarado J. Prevalence of irritable bowel syndrome and health-related quality of life in adults aged 18 to 30 years in a Colombian University: An electronic survey. Annals of Gastroenterology. 2017;30(1):67–75. doi: 10.20524/aog.2016.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang L, Toner BB, Fukudo S, Guthrie E, Locke GR, Norton NJ, Sperber AD. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130(5):1435–1446. doi: 10.1053/j.gastro.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 15.Schmulson M, Corazziari E, Ghoshal UC, Myung SJ, Gerson CD, Quigley EM, Gwee KA, Sperber AD. A four-country comparison of healthcare systems, implementation of diagnostic criteria, and treatment availability for functional gastrointestinal disorders: A report of the Rome Foundation Working Team on cross-cultural, multinational research. Neurogastroenterology and Motility. 2014;26(10):1368–1385. doi: 10.1111/nmo.12402. [DOI] [PubMed] [Google Scholar]
- 16.Gerson MJ, Gerson CD, Awad RA, Dancey C, Poitras P, Porcelli P, Sperber AD. An international study of irritable bowel syndrome: Family relationships and mind-body attributions. Social Science and Medicine. 2006;62(11):2838–2847. doi: 10.1016/j.socscimed.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 17.Sperber AD, Dumitrascu D, Fukudo S, Gerson C, Ghoshal UC, Gwee KA, Hungin APS, Kang JY, Minhu C, Schmulson M, Bolotin A, Friger M, Freud T, Whitehead W. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: A Rome Foundation working team literature review. Gut. 2017;66(6):1075–1082. doi: 10.1136/gutjnl-2015-311240. [DOI] [PubMed] [Google Scholar]
- 18.Sperber AD, Gwee KA, Hungin AP, Corazziari E, Fukudo S, Gerson C, Ghoshal UC, Kang JY, Levy RL, Schmulson M, Dumitrascu D, Gerson MJ, Chen M, Myung SJ, Quigley EM, Whorwell PJ, Zarzar K, Whitehead WE. Conducting multinational, cross-cultural research in the functional gastrointestinal disorders: Issues and recommendations. A Rome Foundation working team report. Alimentary Pharmacology & Therapeutics. 2014;40(9):1094–1102. doi: 10.1111/apt.12942. [DOI] [PubMed] [Google Scholar]
- 19.Drossman DA, Chang L, Schneck S, Blackman C, Norton WF, Norton NJ. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Digestive Diseases and Sciences. 2009;54(7):1532–1541. doi: 10.1007/s10620-009-0792-6. [DOI] [PubMed] [Google Scholar]
- 20.Heitkemper M, Carter E, Ameen V, Olden K, Cheng L. Women with irritable bowel syndrome: Differences in patients' and physicians' perceptions. Gastroenterology Nursing. 2002;25(5):192–200. doi: 10.1097/00001610-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Lacy BE, Weiser K, Noddin L, Robertson DJ, Crowell MD, Parratt-Engstrom C, Grau MV. Irritable bowel syndrome: Patients' attitudes, concerns and level of knowledge. Alimentary Pharmacology & Therapeutics. 2007;25(11):1329–1341. doi: 10.1111/j.1365-2036.2007.03328.x. [DOI] [PubMed] [Google Scholar]
- 22.Halpert A, Dalton CB, Palsson O, Morris C, Hu Y, Bangdiwala S, Hankins J, Norton N, Drossman D. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National Survey on Patient Educational Needs in IBS and development and validation of the Patient Educational Needs Questionnaire (PEQ) The American Journal of Gastroenterology. 2007;102(9):1972–1982. doi: 10.1111/j.1572-0241.2007.01254.x. [DOI] [PubMed] [Google Scholar]
- 23.Jiang X, Xie H, Tang R, Du Y, Li T, Gao J, Xu X, Jiang S, Zhao T, Zhao W, Sun X, Hu G, Wu D, Xie G. Characteristics of online health care services from China's largest online medical platform: Cross-sectional survey study. Journal of Medical Internet Research. 2021;23(4):e25817. doi: 10.2196/25817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gonzalez G, Vaculik K, Khalil C, Zektser Y, Arnold CW, Almario CV, Spiegel BMR, Anger JT. Social media analytics of overactive bladder posts: What do patients know and want to know? International Urogynecology Journal. 2021;32(10):2729–2736. doi: 10.1007/s00192-021-04686-1. [DOI] [PubMed] [Google Scholar]
- 25.O'Reilly M, Dogra N, Whiteman N, Hughes J, Eruyar S, Reilly P. Is social media bad for mental health and wellbeing? Exploring the perspectives of adolescents. Clinical Child Psychology and Psychiatry. 2018;23(4):601–613. doi: 10.1177/1359104518775154. [DOI] [PubMed] [Google Scholar]
- 26.Chan KL, Chen M. Effects of social media and mobile health apps on pregnancy care: Meta-analysis. JMIR Health and Health. 2019;7(1):e11836. doi: 10.2196/11836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li M, Liu L, Yang Y, Wang Y, Yang X, Wu H. Psychological impact of health risk communication and social media on college students during the COVID-19 pandemic: Cross-sectional study. Journal of Medical Internet Research. 2020;22(11):e20656. doi: 10.2196/20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15(4):e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 30.Blei DM, Ng A, Jordan MI. Latent dirichlet allocation. The Journal of Machine Learning Research. 2003;3:993. [Google Scholar]
- 31.Xie T, Ping Q, Zhu L. Study on the topic mining and dynamic visualization in view of LDA model. Modern Applied Science. 2018;13(1):204. doi: 10.5539/mas.v13n1p204. [DOI] [Google Scholar]
- 32.Zhang Y, Jin R, Zhou ZH. Understanding bag-of-words model: A statistical framework. International Journal of Machine Learning & Cybernetics. 2010;1(1–4):43–52. doi: 10.1007/s13042-010-0001-0. [DOI] [Google Scholar]
- 33.Ehek, R., & Sojka, P. (2004). Software Framework for Topic Modelling with Large Corpora. In Proceedings of the LREC 2010 Workshop on New Challenges for NLP Frameworks.
- 34.Charmaz, K. (1983). The grounded theory method: An explication and interpretation.
- 35.Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Routledge; 1968. [Google Scholar]
- 36.de la Espriella R, Gómez RC. Grounded theory. Revista Colombiana de Psiquiatría (English Edition) 2020;49(2):127–133. doi: 10.1016/j.rcp.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 37.Clemmensen TH, Lauridsen HH, Andersen-Ranberg K, Kristensen HK. 'I know his needs better than my own'—Carers' support needs when caring for a person with dementia. Scandinavian Journal of Caring Sciences. 2021;35(2):586–599. doi: 10.1111/scs.12875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.International Q. (2015). Qualitative Data Analysis Software.
- 39.Baumer E, Mimno D, Guha S, Quan E, Gay GK. Comparing grounded theory and topic modeling: Extreme divergence or unlikely convergence? Journal of the Association for Information Science & Technology. 2017;68(6):1397–1410. doi: 10.1002/asi.23786. [DOI] [Google Scholar]
- 40.Gonzalez G, Vaculik K, Khalil C, Zektser Y, Arnold C, Almario CV, Spiegel BMR, Anger JT. Women's experience with stress urinary incontinence: Insights from social media analytics. Journal of Urology. 2020;203(5):962–968. doi: 10.1097/JU.0000000000000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gonzalez G, Vaculik K, Khalil C, Zektser Y, Arnold CW, Almario CV, Spiegel BMR, Anger JT. Experiences of women with interstitial cystitis/bladder pain syndrome: What can we learn from women's online discussions? Journal of Urology. 2023;209(1):208–215. doi: 10.1097/JU.0000000000002955. [DOI] [PubMed] [Google Scholar]
- 42.Dzubur E, Khalil C, Almario CV, Noah B, Minhas D, Ishimori M, Arnold C, Park Y, Kay J, Weisman MH, Spiegel BMR. Patient concerns and perceptions regarding biologic therapies in ankylosing spondylitis: insights from a large-scale survey of social media platforms. Arthritis Care Res (Hoboken) 2019;71(2):323–330. doi: 10.1002/acr.23600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kong D, Chen A, Zhang J, Xiang X, Lou WQV, Kwok T, Wu B. Public discourse and sentiment toward dementia on Chinese Social Media: Machine Learning analysis of Weibo Posts. Journal of Medical Internet Research. 2022;24(9):e39805. doi: 10.2196/39805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Feldhege J, Moessner M, Wolf M, Bauer S. Changes in language style and topics in an online eating disorder community at the beginning of the COVID-19 pandemic: Observational Study. Journal of Medical Internet Research. 2021;23(7):e28346. doi: 10.2196/28346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Helman CG. Communication in primary care: The role of patient and practitioner explanatory models. Social Science and Medicine. 1985;20(9):923–931. doi: 10.1016/0277-9536(85)90348-X. [DOI] [PubMed] [Google Scholar]
- 46.Hahn BA, Yan S, Strassels S. Impact of irritable bowel syndrome on quality of life and resource use in the United States and United Kingdom. Digestion. 1999;60(1):77–81. doi: 10.1159/000007593. [DOI] [PubMed] [Google Scholar]
- 47.Mönnikes H. Quality of life in patients with irritable bowel syndrome. Journal of Clinical Gastroenterology. 2011;45(Suppl):S98–101. doi: 10.1097/MCG.0b013e31821fbf44. [DOI] [PubMed] [Google Scholar]
- 48.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123(6):2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 49.Drossman DA, Thompson WG. The irritable bowel syndrome: Review and a graduated multicomponent treatment approach. Annals of Internal Medicine. 1992;116(12 Pt 1):1009–1016. doi: 10.7326/0003-4819-116-12-1009. [DOI] [PubMed] [Google Scholar]
- 50.Lembo A, Ameen VZ, Drossman DA. Irritable bowel syndrome: Toward an understanding of severity. Clinical Gastroenterology and Hepatology. 2005;3(8):717–725. doi: 10.1016/S1542-3565(05)00157-6. [DOI] [PubMed] [Google Scholar]
- 51.Ramsey I, Corsini N, Peters MDJ, Eckert M. A rapid review of consumer health information needs and preferences. Patient Education and Counseling. 2017;100(9):1634–1642. doi: 10.1016/j.pec.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 52.Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. The Lancet Gastroenterology and Hepatology. 2016;1(2):133–146. doi: 10.1016/S2468-1253(16)30023-1. [DOI] [PubMed] [Google Scholar]
- 53.Pimentel M, Talley NJ, Quigley EM, Hani A, Sharara A, Mahachai V. Report from the multinational irritable bowel syndrome initiative 2012. Gastroenterology. 2013;144(7):e1–5. doi: 10.1053/j.gastro.2013.04.049. [DOI] [PubMed] [Google Scholar]
- 54.Drossman DA, Hasler WL. Rome IV-functional GI disorders: Disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–1261. doi: 10.1053/j.gastro.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 55.Wu J, Lu AD, Zhang LP, Zuo YX, Jia YP. Study of clinical outcome and prognosis in pediatric core binding factor-acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2019;40(1):52–57. doi: 10.3760/cma.j.issn.0253-2727.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Choi MG, Jung HK. Health related quality of life in functional gastrointestinal disorders in Asia. Journal of Neurogastroenterology and Motility. 2011;17(3):245–251. doi: 10.5056/jnm.2011.17.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xiong LS, Chen MH, Chen HX, Xu AG, Wang WA, Hu PJ. A population-based epidemiologic study of irritable bowel syndrome in South China: Stratified randomized study by cluster sampling. Alimentary Pharmacology & Therapeutics. 2004;19(11):1217–1224. doi: 10.1111/j.1365-2036.2004.01939.x. [DOI] [PubMed] [Google Scholar]
- 58.Maita H, Kobayashi T, Osawa H, Kato H. Self-diagnosis of seasonal influenza in a rural primary care setting in Japan: A cross sectional observational study. PLoS ONE. 2018;13(5):e0197163. doi: 10.1371/journal.pone.0197163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Heidelbaugh JJ, Stelwagon M, Miller SA, Shea EP, Chey WD. The spectrum of constipation-predominant irritable bowel syndrome and chronic idiopathic constipation: US survey assessing symptoms, care seeking, and disease burden. American Journal of Gastroenterology. 2015;110(4):580–587. doi: 10.1038/ajg.2015.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shek D. Chinese adolescents' perceptions of family functioning: Personal, school-related, and family correlates. Genetic Social & General Psychology Monographs. 2002;128(4):358. [PubMed] [Google Scholar]
- 61.Ohman L, Simrén M. Pathogenesis of IBS: Role of inflammation, immunity and neuroimmune interactions. Nature Reviews. Gastroenterology & Hepatology. 2010;7(3):163–173. doi: 10.1038/nrgastro.2010.4. [DOI] [PubMed] [Google Scholar]
- 62.Surdea-Blaga T, Băban A, Dumitrascu DL. Psychosocial determinants of irritable bowel syndrome. World Journal of Gastroenterology. 2012;18(7):616–626. doi: 10.3748/wjg.v18.i7.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhu L, Huang D, Shi L, Liang L, Xu T, Chang M, Chen W, Wu D, Zhang F, Fang X. Intestinal symptoms and psychological factors jointly affect quality of life of patients with irritable bowel syndrome with diarrhea. Health and Quality of Life Outcomes. 2015;13:49. doi: 10.1186/s12955-015-0243-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu J, Shi L, Huang D, Fan W, Li X, Zhu L, Wei J, Fang X. Depression and structural factors are associated with symptoms in patients of irritable bowel syndrome with diarrhea. Journal of Neurogastroenterology and Motility. 2020;26(4):505–513. doi: 10.5056/jnm19166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Toner BB, Akman D. Gender role and irritable bowel syndrome: Literature review and hypothesis. American Journal of Gastroenterology. 2000;95(1):11–16. doi: 10.1111/j.1572-0241.2000.01698.x. [DOI] [PubMed] [Google Scholar]
- 66.Björkman I, Dellenborg L, Ringström G, Simrén M, Jakobsson UE. The gendered impact of Irritable Bowel Syndrome: A qualitative study of patients' experiences. Journal of Advanced Nursing. 2014;70(6):1334–1343. doi: 10.1111/jan.12294. [DOI] [PubMed] [Google Scholar]
- 67.Bonetto S, Fagoonee S, Battaglia E, Grassini M, Saracco GM, Pellicano R. Recent advances in the treatment of irritable bowel syndrome. Polish Archives of Internal Medicine. 2021;131(7–8):709–715. doi: 10.20452/pamw.16067. [DOI] [PubMed] [Google Scholar]
- 68.Bertram S, Kurland M, Lydick E, Locke GR, 3rd, Yawn BP. The patient's perspective of irritable bowel syndrome. Journal of Family Practice. 2001;50(6):521–525. [PubMed] [Google Scholar]
- 69.Bhattarai Y, Muniz Pedrogo DA, Kashyap PC. Irritable bowel syndrome: A gut microbiota-related disorder? American Journal of Physiology. Gastrointestinal and Liver Physiology. 2017;312(1):G52–g62. doi: 10.1152/ajpgi.00338.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xiao L, Liu Q, Luo M, Xiong L. Gut microbiota-derived metabolites in irritable bowel syndrome. Frontiers in Cellular and Infection Microbiology. 2021;11:729346. doi: 10.3389/fcimb.2021.729346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dale HF, Rasmussen SH, Asiller Ö, Lied GA. Probiotics in irritable bowel syndrome: An up-to-date systematic review. Nutrients. 2019;11(9):2048. doi: 10.3390/nu11092048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Johnsen PH, Hilpüsch F, Cavanagh JP, Leikanger IS, Kolstad C, Valle PC, Goll R. Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: A double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. The Lancet Gastroenterology & Hepatology. 2018;3(1):17–24. doi: 10.1016/S2468-1253(17)30338-2. [DOI] [PubMed] [Google Scholar]
- 73.Xu D, Chen VL, Steiner CA, Berinstein JA, Eswaran S, Waljee AK, Higgins PDR, Owyang C. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: A systematic review and meta-analysis. American Journal of Gastroenterology. 2019;114(7):1043–1050. doi: 10.14309/ajg.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Badger K, Acton A, Peterson P. Aftercare, survivorship, and peer support. Clinics in Plastic Surgery. 2017;44(4):885–891. doi: 10.1016/j.cps.2017.05.020. [DOI] [PubMed] [Google Scholar]
- 75.Shalaby RAH, Agyapong VIO. Peer support in mental health: Literature review. JMIR Mental Health. 2020;7(6):e15572. doi: 10.2196/15572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moll S, Holmes J, Geronimo J, Sherman D. Work transitions for peer support providers in traditional mental health programs: Unique challenges and opportunities. Work. 2009;33(4):449–458. doi: 10.3233/WOR-2009-0893. [DOI] [PubMed] [Google Scholar]
- 77.Gates LB, Akabas SH. Developing strategies to integrate peer providers into the staff of mental health agencies. Administration and Policy In Mental Health. 2007;34(3):293–306. doi: 10.1007/s10488-006-0109-4. [DOI] [PubMed] [Google Scholar]
- 78.Håkanson C. Everyday life, healthcare, and self-care management among people with irritable bowel syndrome: An integrative review of qualitative research. Gastroenterology Nursing. 2014;37(3):217–225. doi: 10.1097/SGA.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 79.El-Salhy M, Hatlebakk JG, Hausken T. Diet in irritable bowel syndrome (IBS): Interaction with gut microbiota and gut hormones. Nutrients. 2019;11(8):1824. doi: 10.3390/nu11081824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Staudacher HM, Whelan K. The low FODMAP diet: Recent advances in understanding its mechanisms and efficacy in IBS. Gut. 2017;66(8):1517–1527. doi: 10.1136/gutjnl-2017-313750. [DOI] [PubMed] [Google Scholar]
- 81.Guo YB, Zhuang KM, Kuang L, Zhan Q, Wang XF, Liu SD. Association between diet and lifestyle habits and irritable bowel syndrome: A case-control study. Gut Liver. 2015;9(5):649–656. doi: 10.5009/gnl13437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Omagari K, Murayama T, Tanaka Y, Yoshikawa C, Inoue S, Ichimura M, Hatanaka M, Saimei M, Muto K, Tobina T, Masaki M, Kato S. Mental, physical, dietary, and nutritional effects on irritable bowel syndrome in young Japanese women. Internal Medicine. 2013;52(12):1295–1301. doi: 10.2169/internalmedicine.52.0248. [DOI] [PubMed] [Google Scholar]
- 83.Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: A randomized controlled trial. American Journal of Gastroenterology. 2011;106(5):915–922. doi: 10.1038/ajg.2010.480. [DOI] [PubMed] [Google Scholar]
- 84.Nelson LK. Computational grounded theory: A methodological framework. Sociological Methods & Research. 2020;49(1):3–42. doi: 10.1177/0049124117729703. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.