Abstract
This study evaluated the feasibility of remotely delivered yoga for improving four physical activity-related skills: motor skills, strength, balance, and flexibility in adolescents with autism spectrum disorder (ASD). Nineteen of 20 participants enrolled (age 13.2 ± 2.2 years; 60% male) completed the 12-week intervention and attended 83% of the scheduled yoga sessions. Overall, physical activity-related skills improved pre to post intervention (Φ = 0.90, p = 0.005, 95% CI 0.72–1.0). Specifically, significant increases in leg strength (12.5%, p = 0.039), flexibility (40.3%, p = 0.008), and dynamic balance on the right (11.1%, p = 0.001) and left legs (8.1%, p = 0.003) were observed across 12 weeks. These results demonstrate the feasibility and potential effectiveness of yoga to improve physical activity-related skills in adolescents with ASD.
Keywords: Autism, Adolescents, Yoga, Physical activity, Feasibility
Adolescents with autism spectrum disorder (ASD) engage in less physical activity (PA) and are at an increased risk of obesity and weight-related comorbidities compared to their typically developing peers (Must et al., 2014). Studies suggest that participation in moderate-to-vigorous physical activity (MVPA) enhances health; decreases body mass index (BMI); and improves social functioning, locomotor skills, muscular strength, and endurance (Healy et al., 2018; Pitetti et al., 2007; Sorensen & Zarrett, 2014). Additionally, between 60 and 85% of adolescents with ASD have motor impairments which are characterized by a notable loss of motor function and may include deviations from the norm in static and dynamic balance, motor planning and coordination, and fine motor problems in precision and integration (e.g., poor hand dexterity) (Bhat, 2020; Dewey et al., 2007; Manjiviona & Prior, 1995). The motor impairment can become a motor deficit if the problem is untreated or does not resolve on its own (Bhat et al., 2022).
Improving gross motor function at an early age can have a positive effect on MVPA in boys and girls (Logan et al., 2015). Studies in typically developing children found that both motor (e.g., running speed, balance) and object control (e.g., catching and throwing a ball) proficiency (Barnett et al., 2009; Wrotniak et al., 2006) were positively associated with MVPA. However, the association between MVPA and motor function is underexplored in adolescents with intellectual and developmental disabilities. A recent non-powered pilot trial demonstrated that improved locomotor skills in response to a 10-week, 1-h/week community-based PA intervention focused on gross motor function were significantly (p = 0.04) associated with increases in MVPA in 24 children with intellectual disabilities age 4–13 years (Ketcheson et al., 2021).
Diminished physical strength, hypotonia, impaired balance and coordination, and poor motor skill development associated with ASD may discourage adolescents with ASD from participating in regular PA (Serdarevic et al., 2017). Additionally, physical limitations, exacerbated by the behavioral and social issues common with ASD, create complex and multifactorial barriers that can negatively affect participation in regular PA (Must et al., 2015). These may include child-level (e.g., behavior problems, low PA self-efficacy), family-level (e.g., time constraints, lacking transportation or social support), and community-level (e.g., no access to facilities and programs) barriers. Interventions designed to improve motor skills, strength, and balance that also address these challenges may increase the likelihood of participation in PA and reduce the risk for comorbidities associated with low PA (Stanish et al., 2016).
Technology, including computers and tablets, has been used to teach academic subjects and improve social and life skills in individuals with ASD across the age spectrum (Ayres & Cihak, 2010; Kagohara et al., 2013; Ramdoss et al., 2012). Specifically, synchronous (i.e., real-time) video delivery has been successful in teaching social, communication, and daily living skills (Qi et al., 2018). Video delivery may also address social and emotional barriers to PA as well as a lack of transportation or access to exercise facilities or PA programs. It could also offer adolescents with ASD an opportunity to learn and imitate the PA-related behaviors or tasks presented better than conventional in-person PA programs delivered in environments that may be associated with sensory, emotional, or social overstimulation. Additionally, video delivery in a group format provides an opportunity for interaction and social support from other participants and the instructor (Must et al., 2015). Our investigative team has successfully delivered a PA intervention using a group remote video approach (Zoom™ on an iPad®) designed to increase daily steps and improve PA self-efficacy and enjoyment in adolescents with ASD and intellectual disabilities (Ptomey et al., 2017a), which suggests the potential for using group video for delivery of yoga to adolescents with ASD in this trial.
Yoga has several empirically-established benefits including increased flexibility, balance, coordination, and muscular strength—all necessary physical components associated with participation in sports and daily physical activity (Ross & Thomas, 2010). Yoga may also positively influence certain behavioral outcomes such as abhorrent/off-task behaviors, imitation, social skills, and speech and language skills (Radhakrishna, 2010). We are unaware of previous research which has evaluated the impact of yoga on any of these parameters in adolescents with ASD. However, evidence from a limited number of interventions (8–12 weeks) in samples which have included both children and adolescents with ASD (age range 5–13 years) delivered one-on-one (Kaur & Bhat, 2019) or in a group format to children attending a specific school for children with ASD (Shanker & Pradhan, 2022) suggests that participation in yoga has a positive impact on gross motor performance. Based on these previous results, we conducted a 12-week pilot trial to specifically evaluate the feasibility and effectiveness of a remotely delivered yoga intervention designed to impact physical factors that may be related to participation in MVPA in adolescents with ASD including motor skills, strength, balance, and flexibility.
Methods
Overview
This 12-week pilot study in 20 adolescents with ASD was conducted in the Kansas City Metropolitan Area. This study was approved by the Institutional Review Board at The University of Kansas Medical Center. Parent or legal guardian consent and adolescent assent were obtained prior to data collection.
Participants
Inclusion/Exclusion Criteria
Inclusion: Physician confirmed diagnosis of ASD, physician consent to participate in the intervention, age 11–17 years, living at home with a parent or guardian, access to wireless internet in the home, and currently participating in < 90 min/week of structured PA. Exclusion: Currently pregnant or planning to become pregnant, planning to move from the area during the 12-week intervention period, or not interested or unable to participate in yoga.
Recruitment Strategy
Participants were recruited via social media, contact with local community programs/agencies serving adolescents with ASD, an autism clinic at a nearby children’s hospital, and a registry of participants from our previous studies in individuals with intellectual and developmental disabilities who expressed interest in being contacted regarding participation in future trials (Donnelly et al., 2016; Ptomey et al., 2019, 2021). Participants were recruited in 3 cohorts: October 2020 (n = 9), March 2021 (n = 5), and April 2021 (n = 6).
Yoga Intervention
Delivery
The yoga intervention was delivered to groups of adolescents with ASD (4–6 per group) in their home remotely using Zoom™ video conferencing software (Zoom™ Inc., San Jose, CA) on an iPad® (Apple iPad® 7th Generation 10.2) provided by the study. Adolescents participated in the study at home with a parent or guardian present during Zoom™ classes. Thirty-minute yoga sessions were delivered 3 times per week across the 12-week intervention and were scheduled, generally in the late afternoon or early evening, based on the collective availability of the participants and instructor. Participants received a Zoom™ call from the instructor 5 min before the start of class, but were also provided the meeting number on the iPad and by email in case they missed the call.
Equipment
In addition to the iPad® provided for the study, participants received yoga mats, blocks, and straps to use during the yoga sessions. Participants were asked to return the iPad® but were allowed to keep the yoga mats, blocks, and straps as an incentive and to encourage participants to continue practicing yoga after study completion.
Content
All Ashtanga Vinyasa yoga classes were led by the same Registered Yoga Teacher (RYT-200) who completed 200 h of training through a school registered with the Yoga Alliance. In addition to the RYT-200 training, the yoga instructor also had five years of experience teaching yoga and delivering exercise interventions to special populations. Ashtanga Vinyasa yoga focuses on smoothly transitioning through a series of poses and pairing breathing techniques with specific sequences. Sessions began with basic poses (e.g., mountain pose progressing into tree pose) and progressed to intermediate (e.g., Warrior I and Warrior II poses) and advanced poses (e.g., Reverse Warrior and Warrior III) across the intervention. Classes became increasingly more challenging as weeks progressed; however, participants were frequently able to practice both basic and intermediate poses. To make the program accessible for participants lacking adequate strength, balance, flexibility, or proprioception to complete the intermediate or advanced poses, the yoga teacher modified the poses or encouraged the use of yoga blocks to extend the arms or support the back, head, or hips during a pose. All yoga sessions were recorded with the videos placed on Dropbox™. Participants were encouraged to view the Dropbox™ recordings of missed real-time sessions and to use the recordings to review and practice poses on their own.
Outcomes
Overview
Participants reported to our exercise laboratory for a 60-min testing appointment at baseline and within 7 days after completing the 12-week intervention. Outcomes included anthropometrics, motor skills, strength, balance, and flexibility. Participants received $25 each ($50 total) for the completion of the baseline and 12-week outcome assessments.
Feasibility
Feasibility was assessed using weekly attendance expressed as the mean percentage of the three sessions that an adolescent was present averaged over the 12-week intervention. Being present was defined as attending and completing the entire 30-min yoga session. The intervention was considered feasible if the adolescents attended ≥ 75% of the remotely delivered yoga sessions. The percentage of participants viewing the Dropbox™ videos and the average number of weekly views was also considered and reported as an indicator of feasibility.
Anthropometrics (Height, Weight, and Waist Circumference)
Standing height was measured to the nearest centimeter using a portable stadiometer (Model #IP0955, Invicta Plastics Limited, Leicester, UK). Weight was assessed to the nearest 0.1 kg using a calibrated scale (Model #PS660, Belfour, Saukville, WI). BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). BMI percentile (BMI %ile) was calculated using the Centers for Disease Control and Prevention’s BMI Percentile Data Files with LMS Values (Growth Charts—Percentile Data Files with LMS Values, 2019). The LMS parameters are the power in the Box-Cox transformation (L), median (M), and generalized coefficient of variation (S). Waist circumference was measured in centimeters at the narrowest part of the torso above the umbilicus and below the xiphoid process (Lohman et al., 1988).
Motor Skills
Motor skills were evaluated using the motor quotient from the Test of Gross Motor Development—Second Edition (TGM-2). This assessment measures gross motor development across locomotor (i.e., run, gallop, hop, leap, horizontal jump, and slide) and object control skills (i.e., striking a stationary ball, stationary dribble, catch, kick, overhead throw, and underhand roll). Composite locomotor standard and sex-specific object control standard scores were used to calculate the motor quotient (Ulrich, 2000).
Muscular Strength
Lower body (leg press) strength was determined using a standard 5-repetition maximum protocol (Reynolds et al., 2006) on a Cybex plate-loaded leg press machine (Life Fitness, Franklin Park, IL). Grip strength of the dominant and non-dominant hands was measured in triplicate using a Jamar Plus Electronic hand dynamometer (Patterson Medical, Warrenville, IL) with the average of the 3 measures used in the analysis.
Static Balance
Static balance was measured using the Stork Balance Test (SBT) (Johnson & Nelson, 1979). Participants, without shoes and with their eyes open, were asked to lift one leg to their medial proximal tibia while elevating the heel of their standing foot. The test was terminated if participants were unable to maintain this pose without losing their balance, held onto any structure for assistance in maintaining their balance, or dropped their standing heel to the floor. The length of time in seconds for the best of three trials for each leg was recorded and used in the analysis.
Dynamic Balance
Dynamic balance and proprioception were measured using the Star Excursion Balance Test (SEBT). Four strips of masking tape were placed 45 degrees apart on the floor to form an 8-pointed star. Participants, without shoes, were asked to stand on one foot in the center of the star and reach their other foot in eight different directions (i.e., anterior, anteromedial, anterolateral, lateral, medial, posterior, posteromedial, and posterolateral) without losing their balance or using the reaching foot to support their body weight. Participants had a single practice trial before completing 3 trials per leg. Participants who were unable to maintain balance on their stance foot or moved their stance foot from the center of the star were asked to repeat the trial. Final standardized scores were calculated by adjusting the average distance reached from the center of the star (cm) across all 8 orientations over the 3 trials by the leg length for the side being measured and expressing the score as a percentage of each leg length (Plisky et al., 2009; Powden et al., 2019). Leg length (cm) was measured from the anterior superior iliac spine to the medial malleolus as described by Plisky et al. (2009).
Flexibility
Flexibility of the hamstrings and lumbar musculature was assessed using the Sit and Reach Test (Wells & Dillon, 1952). A standard cloth measuring tape was secured to the floor. Participants sat with their legs outstretched on either side of the tape with their feet (in dorsiflexion) at the 38.1 cm mark and were asked to reach as far forward as possible and maintain the stretched position for a minimum of two seconds. The position of the fingertip along the tape, best of three trials, was recorded and used in the analysis. Positive and negative scores indicated that participants were able to reach past or not reach past their feet, respectively.
Physical Activity and Sedentary Time
Physical activity and sedentary time were evaluated using the ActiGraph wGT3X-BT tri-axial accelerometer (ActiGraph LLC, Pensacola, FL). Participants were provided with the accelerometer at their testing appointments and asked to wear the accelerometer on a belt over the anterior axillary line of their non-dominant hip for 7 consecutive days. Instruction on correct positioning and orientation of the accelerometer and a pre-stamped addressed envelope to return the accelerometer to the investigators were provided to participants during their testing visits. Data were collected at 60 Hz and vertical axis activity counts were aggregated over 60-s epochs. Wear time was determined using the Choi algorithm (Choi et al., 2011) and a minimum wear time of four 8-h days, including a Friday or a weekend day, was required for inclusion in the analysis. Daily minutes of sedentary (≤ 1.5 metabolic equivalents; METs), light (1.6 to < 4 METs), and MVPA (≥ 4 METs) were estimated using the Freedson age-specific ActiGraph cut-points (Freedson et al., 1998, 2005). We also assessed the percentage of participants who achieved the recommended 60 min of MVPA each day (Piercy et al., 2018).
Statistical Analysis
We used mean ± standard deviation or frequency (percentage) to report sample characteristics and changes in motor skills, strength, balance, and flexibility from baseline to 12 weeks. Wilcoxon rank sum or Fisher’s exact tests were used to evaluate baseline sex differences in demographics (i.e., age, race/ethnicity, parent-reported PA), anthropometrics (i.e., height, weight, BMI, BMI %ile, and waist circumference), and accelerometer measured PA. We analyzed the primary outcomes (i.e., changes in motor skills, strength, balance, and flexibility across 12 weeks) using the prediction test (Montgomery & Mahnken, 2020), which is a recently developed global hypothesis test designed to aid in decision making regarding the efficacy of early-stage interventions (e.g., pilot trials). This test relies on a priori predictions regarding the expected direction of the pre-post change in each outcome of interest assuming that the intervention is effective to estimate Φ, a measure of how well the predictions match the actual results ranging from 0 (no predictions were correct) to 1 (all predictions were correct). For this trial, we predicted pre-to-post intervention improvement in each of our primary outcomes. The null hypothesis (Φ = 0.50) is that the investigators are no better at predicting the direction of change than chance alone. Rejection of the null hypothesis indicates that the observed results are more consistent with the hypothesized effects than would be expected if the intervention was ineffective. Advantages of the prediction test over comparable approaches (e.g., O’Brien’s OLS test, Hotelling’s T2 test, or the Bonferroni adjustment) to address multiplicity include the ability to account for missing data and combine information across endpoints while adjusting for correlations between endpoints, greater power with an increasing number of endpoints within a fixed sample size, and the ability to incorporate one-sided hypotheses that are not in a uniform direction into a single global test.
We also conducted post-hoc analyses using a Wilcoxon signed rank test to assess pre-post intervention changes in all outcomes. Spearman correlations were used to evaluate the association between each outcome and MVPA before the 12-week yoga intervention as well as the association between the change in outcomes and change in MVPA across 12 weeks. All analyses were completed using R version 4.1.2 (R Core Team, 2021).
Results
Twenty participants (age: 13.2 ± 2.2 years; 60% male; 85% non-Hispanic white) enrolled and 19 participants (95%) completed the 12-week intervention. There were no significant differences between males and females in any of the baseline characteristics (Table 1). Participants attended 83 ± 26% (range 58–100%) of the 3 weekly sessions with similar attendance for females (84 ± 26%) and males (82 ± 26%). Twelve participants attended > 80% of the scheduled sessions. Six participants (30%) viewed the Dropbox™ videos 34 times across the 12-week yoga intervention (2.4 ± 1.1 views/week).
Table 1.
Baseline characteristics by sex for adolescents with autism spectrum disorder participating in a yoga intervention
| Overall samplea (n = 20) | By sex | ||
|---|---|---|---|
| Malea (n = 12) | Femalea (n = 8) | ||
| Age (years) | 13.2 ± 2.2 | 13.3 ± 2.4 | 13.0 ± 1.9 |
| Non-Hispanic White | 17 (85%) | 10 (83%) | 7 (88%) |
| Parent report | |||
| PA ≥ 60 min (days/week) | 1.3 ± 1.7 | 1.1 ± 1.5 | 1.6 ± 1.9 |
| TV ≥ 2 h/day | 9 (45%) | 5 (42%) | 4 (50%) |
| Video games ≥ 2 h/day | 14 (70%) | 9 (75%) | 5 (62%) |
| PE class (days/week) | 1.7 ± 1.9 | 1.2 ± 1.4 | 2.5 ± 2.2 |
| Play on a sports team | 5 (25%) | 2 (17%) | 3 (38%) |
| Anthropometrics | |||
| Weight (kg) | 57.9 ± 15.7 | 62.6 ± 17.2 | 50.9 ± 10.2 |
| Height (cm) | 156.3 ± 9.7 | 157.5 ± 10.1 | 154.6 ± 9.4 |
| BMI (kg/m2) | 23.6 ± 5.8 | 25.1 ± 6.1 | 21.5 ± 4.8 |
| BMI percentile | 69.7 ± 31.9 | 75.4 ± 28.8 | 61.3 ± 36.3 |
| Waist (cm) | 76.8 ± 13.5 | 81.0 ± 13.9 | 70.5 ± 10.5 |
| Physical activityb | |||
| Sedentary time (min/day) | 506.7 ± 84.6 | 515.0 ± 69.6 | 491.4 ± 113.1 |
| Light activity (min/day) | 240.4 ± 78.2 | 234.1 ± 77.3 | 251.8 ± 85.9 |
| MVPA (min/day) | 18.6 ± 14.9 | 15.0 ± 12.3 | 25.2 ± 18.0 |
PE Physical Education
Mean ± Standard Deviation or n (%); No statistical differences between males and females (all p > 0.1) using Wilcoxon Rank Sum or Fisher’s exact test
Sample size is 17 for physical activity after exclusion of invalid wear time; MVPA (Moderate to Vigorous Physical Activity)
Results for change in motor skills, strength, flexibility, and balance across the 12-week intervention are presented in Table 2 and Fig. 1. The pre-post intervention changes in 9 of 11 outcomes assessing motor skill, strength, flexibility, and balance were in the predicted direction. Results from the prediction test supported our primary hypothesis that the 12-week yoga intervention would improve physical function outcomes (n = 19; p = 0.005, Φ = 0.90, 95% CI 0.72–1.0). Post hoc analyses indicated significant increases in leg strength (12.5%, p = 0.039), flexibility (40.3%, p = 0.008), and dynamic balance on the right (11.1%, p = 0.001) and left legs (8.1%, p = 0.003) across the 12-week intervention. The changes in all other variables assessed were not statistically significant.
Table 2.
Changes in motor skills, strength, flexibility, and balance for adolescents with autism spectrum disorder participating in the yoga intervention
| Baseline N = 20a | 12-weeks N = 19a | Difference (% Change) | p-value* | |
|---|---|---|---|---|
| Motor skillsb | ||||
| Locomotor standard score | 9.0 ± 3.4 | 9.7 ± 3.7 | 0.7 (7.8%) | 0.138 |
| Object control standard score | 7.5 ± 3.7 | 7.8 ± 4.2 | 0.3 (4.0%) | 0.249 |
| Motor quotient | 89.5 ± 19.6 | 92.4 ± 21.3 | 2.9 (3.2%) | 0.153 |
| Strengthb | ||||
| Leg press 5 RM | 64.9 ± 21.0 | 73.0 ± 14.3 | 8.1 (12.5%) | 0.039 |
| Dominant grip strength | 21.2 ± 6.6 | 21.8 ± 6.8 | 0.6 (2.8%) | 0.284 |
| Non-dominant grip strength | 20.2 ± 6.9 | 20.8 ± 7.0 | 0.6 (3.0%) | 0.245 |
| Flexibilityb | ||||
| Sit & reach | − 6.7 ± 10.9 | − 4.0 ± 11.5 | 2.7 (40.3%) | 0.008 |
| Balanceb | ||||
| Right SBT | 4.3 ± 4.0 | 4.3 ± 3.1 | 0.0 (0.0%) | 0.517 |
| Left SBT | 3.6 ± 3.2 | 3.5 ± 2.4 | − 0.1 (− 2.8%) | 0.483 |
| Right SEBT | 77.6 ± 15.9 | 86.2 ± 14.7 | 8.6 (11.1%) | 0.001 |
| Left SEBT | 77.5 ± 15.2 | 83.8 ± 15.5 | 6.4 (8.1%) | 0.003 |
Unadjusted one-sided Wilcoxon signed rank (alternative hypothesis of greater values after yoga)
Mean ± Standard Deviation
Motor skill assessment outcomes are unitless; Lower and upper body strength measured in kilograms; Sit & Reach test for flexibility measured in centimeters; SBT measured in seconds; SEBT standardized as a percentage of leg length
Fig. 1.
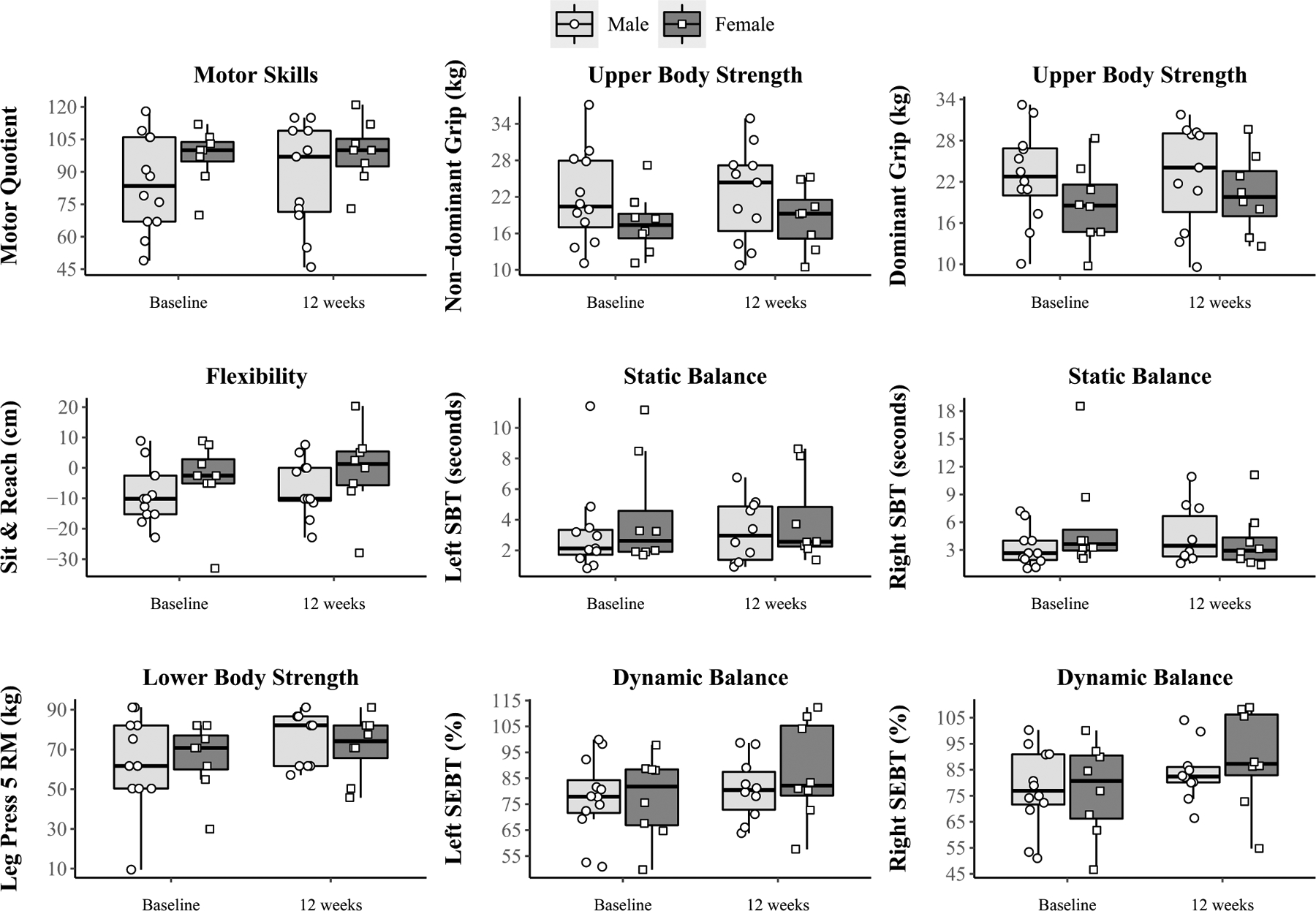
Physical skills related to physical activity stratified by sex at baseline and 12 weeks in adolescents with autism spectrum disorder participating in a yoga intervention. SBT Stork Balance Test, SEBT Start Excursion Balance Test
Eighty-five (n = 17) and 58% (n = 11) percent of participants provided valid accelerometer data at baseline and 12 weeks, respectively. Fifty percent (n = 10) of participants provided valid accelerometer data at both baseline and 12 weeks. Sedentary time was essentially unchanged from baseline (507 ± 85 min/day) to 12-weeks (500 ± 112 min/day) while light PA decreased from 240 ± 78 min/day to 226 ± 88 min/day and MVPA decreased from 19 ± 15 min/day to 7 ± 7 min/day pre-to-post intervention. No participants met the recommended level of MVPA (60 min/day) at either baseline or 12 weeks. We found positive correlations between baseline locomotor motor skills and MVPA (n = 17, rho: 0.62, p = 0.01). We did not calculate correlations between the change in physical factors and change in MVPA that were planned as data for both physical factors and MVPA at both baseline and 12 weeks were available for < 50% of our sample.
Discussion
Our study demonstrated that a group-based yoga intervention delivered by video was both feasible and potentially effective in improving motor skills, strength, balance, and flexibility in adolescents with ASD.
Feasibility
Ninety-five percent of participants completed the 12-week trial and attended 83% of the scheduled yoga sessions which exceeded the 75% attendance rate we established to demonstrate the feasibility of the remotely delivered yoga intervention. Our observed attendance rate (83%) was ~ 12% higher than an 8-week, 4 session per week yoga intervention in 24 children with ASD age 5–13 years (Kaur & Bhat, 2019) and ~ 6% higher than in previous trials by our research team which used group-based video to remotely deliver PA interventions to adolescents with intellectual and developmental disabilities (Ptomey et al., 2017a). Although our mean attendance rate was high, there was considerable inter-individual variability with attendance ranging from 58 to 100%. Anecdotal evidence suggests that the variation in attendance in this trial may have been at least partially due to the fact that 25% of participants engaged in extracurricular activities which often conflicted with attendance at yoga sessions scheduled after school in the late afternoon or early evening.
Effectiveness
Results from the prediction test supported our primary hypothesis that the 12-week yoga intervention would improve physical function outcomes. Additionally, we observed significant increases in leg strength, flexibility, and dynamic balance across the 12-week intervention. However, no significant improvement in motor quotient, grip strength, or static balance were observed.
We are unaware of previous research which has evaluated the impact of a remotely delivered yoga intervention on physical function parameters in adolescents with ASD. However, evidence from a limited number of yoga interventions, predominantly delivered within school settings, that have included both children and adolescents with ASD and in typically developing children are in general agreement with the results from the current trial. For example, Kaur and Bhat (2019) reported increased motor performance assessed by the Bruininks-Oseretsky Test of Motor Proficiency—2nd edition (BOT-2) in children (n = 11, age 5–13 years) who completed an 8-week yoga intervention (4 sessions/week, 45 min/session) but not in 12 children assigned to a control group who participated in sedentary activities such as reading, arts and crafts, etc. Shanker and Pradhan (2022) also reported improved performance on the BOT-2 in children attending 4 special schools for children with ASD who were randomized to a group-based yoga intervention (n = 23) or a non-intervention control (n = 20). Together, the results of the available trials suggest that the impact of yoga on physical function parameters in children with ASD may be similar to those observed from short-term trials (6–16 weeks) in children with ASD (n < 20, age 6–10 years) using other intervention strategies targeting increased physical activity (Healy et al., 2018) and fundamental motor skills (Healy et al., 2021). Interventions beginning at an early age in children with ASD remain needed since children with ASD perform similar to typically developing children who are half their chronological age when matched on movement skill (Staples & Reid, 2010).
Results from interventions evaluating the impact of yoga on physical function parameters in typically developing are in general agreement with those reported in children with ASD. For example, school-based yoga interventions (8–12 weeks) in typically developing healthy pre-school (Aleksić Veljković et al., 2021) and elementary school children (Donahoe-Fillmore & Grant, 2019; Folleto et al., 2016) have reported improved coordination (Aleksić Veljković et al., 2021), balance (Aleksić Veljković et al., 2021; Donahoe-Fillmore & Grant, 2019), and strength (Folleto et al., 2016). School-based yoga interventions (12–16 weeks) have also shown improved flexibility and strength in 9–16 year old (n = 83) children with visual impairments (Mohanty et al., 2019) and improved static balance, eye hand coordination, agility, and reaction time in 10–15 year old children (n = 70) with mild-to-moderate intellectual disabilities (Pise et al., 2018). Wurz et al. (2014) also observed improved functional mobility and hamstring flexibility in 8 pediatric cancer patients (age 12 years) who completed a 12-week community-based yoga intervention.
In agreement with the literature (Healy et al., 2019; Liang et al., 2020), baseline MVPA in our sample of adolescents with ASD was extremely low (19 min/day) with no participants achieving the 60 min/day of MVPA recommended to achieve health benefits (Piercy et al., 2018). The observation of low baseline MVPA suggests the importance of the development and evaluation of intervention strategies to improve the level of MVPA in adolescents with ASD. We observed an ~ 63% reduction in daily MVPA from baseline to 12 weeks. This finding, which is contrary to our expectations, should be cautiously interpreted as only 11 of the 19 participants (58%) completed the accelerometer protocol at 12 weeks. Poor compliance with waist worn accelerometer protocols in individuals with ASD and other intellectual disabilities has been previously reported by our research group (Ptomey et al., 2017b, 2021) and others (Melville et al., 2011; Spanos et al., 2016). This suggests that additional strategies to improve compliance with widely used waist worn accelerometer protocols or the development of protocols and PA intensity cut-points for wrist worn accelerometers which may improve compliance (Fairclough et al., 2016) are worthy of consideration.
Strengths of our study include the use of video conferencing and a trained and experienced instructor to deliver the yoga intervention to groups of adolescents in their homes and the assessment of a variety of physical outcomes with the potential to be positively impacted by participation in yoga including motor skills, flexibility, strength, and static and dynamic balance. Limitations include the use of a single arm design, relatively small sample size (n = 20), short intervention duration (12 weeks), lack of assessment of ASD severity, and as mentioned previously, poor compliance with our accelerometer protocol for the assessment of MVPA.
Conclusion
The results of our pilot trial suggest the feasibility and potential effectiveness of remotely delivered group-based yoga for improving physical factors that may be related to participation in MVPA in adolescents with ASD including motor skills, strength, balance, and flexibility. Our results also suggest that longer duration (e.g., ≥ 6 months), adequately powered randomized trials to examine the impact of remotely delivered group-based yoga interventions on physical factors and the potential association of improvements in these physical outcomes with increased participation in MVPA for adolescents with ASD are warranted. If ultimately shown to be effective in improving physical factors and MVPA, group-based remotely delivered yoga interventions have tremendous potential for widespread implementation, dissemination, and reach with the potential to have a positive impact on the health and quality of life for adolescents with ASD.
Funding
This project was funded by the Health Resources & Services Administration (HRSA) throughthe Healthy Weight Research Network (HWRN; UA3MC25735). The first author of thismanuscript was also supported by a Clinical and Translational Science Award (CTSA) fromNational Center for Advancing Translational Sciences (NCATS) awarded to the University ofKansas for Frontiers: University of Kansas Clinical and Translational Science Institute(Grant No. TL1TR002368). The contents are solely the responsibility of the authors and do not necessarilyrepresent the official views of the HWRN, HRSA, NCATS, or the National Institutes of Health.
Footnotes
Conflict of interest The authors have no conflicts.
References
- Aleksić Veljković A, Katanić B, & Masanovic B (2021). Effects of a 12-weeks yoga intervention on motor and cognitive abilities of preschool children. Frontiers in Pediatrics, 9, 799226. 10.3389/fped.2021.799226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres K, & Cihak D (2010). Computer- and video-based instruction of food-preparation skills: Acquisition, generalization, and maintenance. Intellectual and Developmental Disabilities, 48(3), 195–208. 10.1352/1944-7558-48.3.195 [DOI] [PubMed] [Google Scholar]
- Barnett LM, van Beurden E, Morgan PJ, Brooks LO, & Beard JR (2009). Childhood motor skill proficiency as a predictor of adolescent physical activity. Journal of Adolescent Health, 44(3), 252–259. 10.1016/j.jadohealth.2008.07.004 [DOI] [PubMed] [Google Scholar]
- Bhat AN (2020). Is motor impairment in autism spectrum disorder distinct from developmental coordination disorder? A report from the SPARK Study. Physical Therapy, 100(4), 633–644. 10.1093/ptj/pzz190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat AN, Boulton AJ, & Tulsky DS (2022). A further study of relations between motor impairment and social communication, cognitive, language, functional impairments, and repetitive behavior severity in children with ASD using the SPARK study dataset. Autism Research. 10.1002/aur.2711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi L, Liu Z, Matthews CE, & Buchowski MS (2011). Validation of accelerometer wear and nonwear time classification algorithm. Medicine and Science in Sports and Exercise, 43(2), 357–364. 10.1249/MSS.0b013e3181ed61a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey D, Cantell M, & Crawford SG (2007). Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. Journal of the International Neuropsychological Society, 13(2), 246–256. 10.1017/s1355617707070270 [DOI] [PubMed] [Google Scholar]
- Donahoe-Fillmore B, & Grant E (2019). The effects of yoga practice on balance, strength, coordination and flexibility in healthy children aged 10–12 years. Journal of Bodywork and Movement Therapies, 23(4), 708–712. 10.1016/j.jbmt.2019.02.007 [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Ptomey LT, Goetz JR, Sullivan DK, Gibson CA, Greene JL, Lee RH, Mayo MS, Honas JJ, & Washburn RA (2016). Weight management for adolescents with intellectual and developmental disabilities: Rationale and design for an 18month randomized trial. Contemporary Clinical Trials, 51, 88–95. 10.1016/j.cct.2016.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairclough SJ, Noonan R, Rowlands AV, Van Hees V, Knowles Z, & Boddy LM (2016). Wear compliance and activity in children wearing wrist- and hip-mounted accelerometers. Medicine and Science in Sports and Exercise, 48(2), 245–253. 10.1249/mss.0000000000000771 [DOI] [PubMed] [Google Scholar]
- Folleto JC, Pereira KR, & Valentini NC (2016). The effects of yoga practice in school physical education on children’s motor abilities and social behavior. International Journal of Yoga, 9(2), 156–162. 10.4103/0973-6131.183717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, & Sirard J (1998). Calibration of the computer science and applications Inc. accelerometer. Medicine & Science in Sports & Exercise, 30(5), 777–781. 10.1097/00005768-199805000-00021 [DOI] [PubMed] [Google Scholar]
- Freedson P, Pober D, & Janz KF (2005). Calibration of accelerometer output for children. Medicine and Science in Sports and Exercise, 37(11 Suppl), S523–530. 10.1249/01.mss.0000185658.28284.ba [DOI] [PubMed] [Google Scholar]
- Growth Charts—Percentile Data Files with LMS Values. (2019, 2019–01-11T05:00:31Z/). https://www.cdc.gov/growthcharts/percentile_data_files.htm
- Healy S, Aigner CJ, Haegele JA, & Patterson F (2019). Meeting the 24-hr movement guidelines: An update on US youth with autism spectrum disorder from the 2016 National Survey of Children’s Health. Autism Research, 12(6), 941–951. 10.1002/aur.2095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy S, Nacario A, Braithwaite RE, & Hopper C (2018). The effect of physical activity interventions on youth with autism spectrum disorder: A meta-analysis. Autism Research, 11(6), 818–833. 10.1002/aur.1955 [DOI] [PubMed] [Google Scholar]
- Healy S, Obrusnikova I, & Getchell N (2021). Fundamental motor skill interventions in children with autism spectrum disorder: A systematic review of the literature including a methodological quality assessment. Research in Autism Spectrum Disorders, 81, 101717. 10.1016/j.rasd.2020.101717 [DOI] [Google Scholar]
- Johnson BL, & Nelson JK (1979). Practical measurements for evaluation in physical education (3rd ed.). Burgess Pub. Co. [Google Scholar]
- Kagohara DM, van der Meer L, Ramdoss S, O’Reilly MF, Lancioni GE, Davis TN, Rispoli M, Lang R, Marschik PB, Sutherland D, Green VA, & Sigafoos J (2013). Using iPods (R) and iPads (R) in teaching programs for individuals with developmental disabilities: A systematic review. Research in Developmental Disabilities, 34(1), 147–156. 10.1016/j.ridd.2012.07.027 [DOI] [PubMed] [Google Scholar]
- Kaur M, & Bhat A (2019). Creative yoga intervention improves motor and imitation skills of children with autism spectrum disorder. Physical Therapy, 99(11), 1520–1534. 10.1093/ptj/pzz115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ketcheson LR, Centeio EE, Snapp EE, McKown HB, & Martin JJ (2021). Physical activity and motor skill outcomes of a 10-week intervention for children with intellectual and developmental disabilities ages 4–13: A pilot study. Disability and Health Journal, 14(1), 100952. 10.1016/j.dhjo.2020.100952 [DOI] [PubMed] [Google Scholar]
- Liang X, Li R, Wong SHS, Sum RKW, & Sit CHP (2020). Accelerometer-measured physical activity levels in children and adolescents with autism spectrum disorder: A systematic review. Preventive Medicine Reports, 19, 101147. 10.1016/j.pmedr.2020.101147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan SW, Kipling Webster E, Getchell N, Pfeiffer KA, & Robinson LE (2015). Relationship between fundamental motor skill competence and physical activity during childhood and adolescence: A systematic review. Kinesiology Review, 4(4), 416–426. [Google Scholar]
- Lohman TG, Roche AF, & Martorell R (1988). Anthropometric standardization reference manual. Human kinetics books. [Google Scholar]
- Manjiviona J, & Prior M (1995). Comparison of Asperger syndrome and high-functioning autistic children on a test of motor impairment. Journal of Autism and Developmental Disorders, 25(1), 23–39. 10.1007/bf02178165 [DOI] [PubMed] [Google Scholar]
- Melville CA, Boyle S, Miller S, Macmillan S, Penpraze V, Pert C, Spanos D, Matthews L, Robinson N, Murray H, & Hankey CR (2011). An open study of the effectiveness of a multi-component weight-loss intervention for adults with intellectual disabilities and obesity. British Journal of Nutrition, 105(10), 1553–1562. 10.1017/s0007114510005362 [DOI] [PubMed] [Google Scholar]
- Mohanty S, Pradhan B, & Hankey A (2019). Yoga practices as an alternative training for physical fitness in children with visual impairment. Adapted Physical Activity Quarterly, 36(4), 431–446. 10.1123/apaq.2018-0167 [DOI] [PubMed] [Google Scholar]
- Montgomery RN, & Mahnken JD (2020). A prediction-based test for multiple endpoints. Statistics in Medicine, 39(28), 4267–4280. 10.1002/sim.8724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A, Phillips SM, Curtin C, Anderson SE, Maslin M, Lividini K, & Bandini LG (2014). Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism, 18(4), 376–384. 10.1177/1362361313479039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A, Phillips S, Curtin C, & Bandini LG (2015). Barriers to physical activity in children with autism spectrum disorders: relationship to physical activity and screen time. Journal of Physical Activity & Health, 12(4), 529–534. 10.1123/jpah.2013-0271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, & Olson RD (2018). The physical activity guidelines for Americans. JAMA, 320(19), 2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pise V, Pradhan B, & Gharote M (2018). Effect of yoga practices on psycho-motor abilities among intellectually disabled children. Journal of Exercise Rehabilitation, 14(4), 581–585. 10.12965/jer.1836290.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitetti KH, Rendoff AD, Grover T, & Beets MW (2007). The efficacy of a 9-month treadmill walking program on the exercise capacity and weight reduction for adolescents with severe autism. Journal of Autism and Developmental Disorders, 37(6), 997–1006. 10.1007/s10803-006-0238-3 [DOI] [PubMed] [Google Scholar]
- Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, & Elkins B (2009). The reliability of an instrumented device for measuring components of the star excursion balance test. North American Journal of Sports Physical Therapy, 4(2), 92–99. [PMC free article] [PubMed] [Google Scholar]
- Powden CJ, Dodds TK, & Gabriel EH (2019). The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: A systematic review. International Journal of Sports Physical Therapy, 14(5), 683–694. [PMC free article] [PubMed] [Google Scholar]
- Ptomey LT, Washburn RA, Goetz JR, Sullivan DK, Gibson CA, Mayo MS, Krebill R, Gorczyca AM, Montgomery RN, Honas JJ, Helsel BC, & Donnelly JE (2021). Weight loss interventions for adolescents with intellectual disabilities: An RCT. Pediatrics, 148(3), e2021050261. 10.1542/peds.2021-050261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptomey LT, Washburn RA, Lee J, Greene JL, Szabo-Reed AN, Sherman JR, Danon JC, Osborne LN, Little TD, & Donnelly JE (2019). Individual and family-based approaches to increase physical activity in adolescents with intellectual and developmental disabilities: Rationale and design for an 18 month randomized trial. Contemporary Clinical Trials, 84, 105817. 10.1016/j.cct.2019.105817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptomey LT, Willis EA, Greene JL, Danon JC, Chumley TK, Washburn RA, & Donnelly JE (2017a). The feasibility of group video conferencing for promotion of physical activity in adolescents With intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 122(6), 525–538. 10.1352/1944-7558-122.6.525 [DOI] [PubMed] [Google Scholar]
- Ptomey LT, Willis EA, Lee J, Washburn RA, Gibson CA, Honas JJ, & Donnelly JE (2017b). The feasibility of using pedometers for self-report of steps and accelerometers for measuring physical activity in adults with intellectual and developmental disabilities across an 18-month intervention. Journal of Intellectual Disability Research, 61(8), 792–801. 10.1111/jir.12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi CH, Barton EE, Collier M, & Lin Y-L (2018). A systematic review of single-case research studies on using video modeling interventions to improve social communication skills for individuals with autism spectrum disorder. Focus on Autism and Other Developmental Disabilities, 33(4), 249–257. 10.1177/1088357617741282 [DOI] [Google Scholar]
- R Core Team. (2021, 2021). R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Radhakrishna S (2010). Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. International Journal of Yoga, 3(1), 26–30. 10.4103/0973-6131.66775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramdoss S, Machalicek W, Rispoli M, Mulloy A, Lang R, & O’Reilly M (2012). Computer-based interventions to improve social and emotional skills in individuals with autism spectrum disorders: A systematic review. Developmental Neurorehabilitation, 15(2), 119–135. 10.3109/17518423.2011.651655 [DOI] [PubMed] [Google Scholar]
- Reynolds JM, Gordon TJ, & Robergs RA (2006). Prediction of one repetition maximum strength from multiple repetition maximum testing and anthropometry. Journal of Strength and Conditioning Research, 20(3), 584–592. 10.1519/r-15304.1 [DOI] [PubMed] [Google Scholar]
- Ross A, & Thomas S (2010). The health benefits of yoga and exercise: A review of comparison studies. Journal of Alternative and Complementary Medicine, 16(1), 3–12. 10.1089/acm.2009.0044 [DOI] [PubMed] [Google Scholar]
- Serdarevic F, Ghassabian A, van Batenburg-Eddes T, White T, Blanken LME, Jaddoe VWV, Verhulst FC, & Tiemeier H (2017). Infant muscle tone and childhood autistic traits: A longitudinal study in the general population. Autism Research, 10(5), 757–768. 10.1002/aur.1739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanker S, & Pradhan B (2022). Effect of yoga on the motor proficiency of children with autism spectrum disorder and the feasibility of its inclusion in special school environments. Adapted Physical Activity Quarterly. 10.1123/apaq.2021-0108 [DOI] [PubMed] [Google Scholar]
- Sorensen C, & Zarrett N (2014). Benefits of physical activity for adolescents with autism spectrum disorders: A comprehensive review. Review Journal of Autism and Developmental Disorders, 1(4), 344–353. 10.1007/s40489-014-0027-4 [DOI] [Google Scholar]
- Spanos D, Hankey CR, & Melville CA (2016). The effectiveness of a weight maintenance intervention for adults with intellectual disabilities and obesity: A single stranded study. Journal of Applied Research in Intellectual Disabilities, 29(4), 317–329. 10.1111/jar.12181 [DOI] [PubMed] [Google Scholar]
- Stanish HI, Curtin C, Must A, Phillips S, Maslin M, & Bandini LG (2016). Physical activity enjoyment, perceived barriers, and beliefs among adolescents with and without intellectual disabilities. Journal of Physical Activity & Health, 13(1), 102–110. 10.1123/jpah.2014-0548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staples KL, & Reid G (2010). Fundamental movement skills and autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(2), 209–217. 10.1007/s10803-009-0854-9 [DOI] [PubMed] [Google Scholar]
- Ulrich DA (2000). Test of gross motor development-2 (TGM-2). ProEd, Inc. [Google Scholar]
- Wells KF, & Dillon EK (1952). The sit and reach—A test of back and leg flexibility. Research Quarterly. American Association for Health, Physical Education and Recreation, 23(1), 115–118. [Google Scholar]
- Wrotniak BH, Epstein LH, Dorn JM, Jones KE, & Kondilis VA (2006). The relationship between motor proficiency and physical activity in children. Pediatrics, 118(6), e1758–1765. 10.1542/peds.2006-0742 [DOI] [PubMed] [Google Scholar]
- Wurz A, Chamorro-Vina C, Guilcher GM, Schulte F, & Culos-Reed SN (2014). The feasibility and benefits of a 12-week yoga intervention for pediatric cancer out-patients. Pediatric Blood & Cancer, 61(10), 1828–1834. 10.1002/pbc.25096 [DOI] [PubMed] [Google Scholar]


