Abstract
Objectives:
To assess training needs for providers who care for adolescent and young adult (AYA) lesbian, gay, bisexual, transgender/queer questioning (LGBTQ) cancer patients, we conducted a mixed-method survey. During their cancer care experience, AYA cancer patients experience physical, psychosocial, and reproductive health challenges. In addition to these challenges, AYA LGBTQ individuals are a diverse and medically underserved population who experience unique challenges and disparities in medical care.
Methods:
Health care providers (n = 351) who participated in our reproductive health in cancer training program completed a survey with 28 quantitative items and 4 open-ended items assessing knowledge, confidence discussing reproductive health, and confidence in knowledge specific to reproductive needs and general health needs among AYA LGBTQ patients.
Results:
Confidence discussing and confidence in knowledge of reproductive and general health needs are lower regarding transgender and nonbinary patients. Nearly half of providers (45%) demonstrated low knowledge, while 38% and 17% demonstrated moderate and high knowledge, respectively. Open comments indicated providers desired more training around the needs of Trans and nonbinary patients, and creating welcoming environments.
Conclusions:
The majority of our participants demonstrate low or moderate knowledge regarding factors that can influence AYA LGBTQ patient care, suggesting that this is a key area for improvement. Furthermore, improving provider knowledge may subsequently improve confidence in general and reproductive needs of LGBTQ patients, resulting in improved patient-centered care. Improving provider knowledge and confidence may then ultimately help reduce disparities in cancer care among this patient population.
Keywords: LGBTQ, LGBT, fertility, contraception, sexual health, cancer, allied health professionals
Introduction
Reproductive health is a chief concern of adolescents and young adults (AYA) with cancer, whose needs often extend beyond infertility and fertility preservation to include sexual health with components such as romantic partnering, friendships, body image, sexuality, sexual identity and orientation, contraception, and psychosexual adjustment.1–6 Coupled with the distinct needs of AYAs with cancer are those needs of lesbian, gay, bisexual, transgender/queer questioning (LGBTQ) AYA patients with cancer. LGBTQ people are a diverse and medically underserved population who experience substantial disparities across the cancer continuum, from prevention to survivorship.7 The number of people who identify as LGBTQ are growing, as are the number of cancer diagnoses in the United States.8,9 Based on conservative LGBTQ population estimates, there may be over 1 million LGBTQ cancer survivors living in the United States.10
Little is known about whether the reproductive health needs of LGBTQ AYA with cancer substantially differ from cisgender/heterosexual AYA. However, growing evidence suggests LGBTQ AYA would benefit from safe and welcoming spaces to disclose their sexual orientation and gender identity (SOGI) information and have their needs addressed in ways that are relevant and responsive.11–14 In addition, multiple recent studies suggest the majority of clinicians and allied health professionals (AHPs) do not receive training on the care of LGBTQ AYA with cancer and are often uncertain about how to ask SOGI intake questions, why they should be asked, and/or what to do with this information if it is received.15
There are limited data on the experiences of LGBTQ AYA with cancer accessing reproductive health care and fertility referrals.16,17 The disparity in access to adequate reproductive health care, often due to the faulty assumption that this population is uninterested or ineligible, affects LGBTQ patients with cancer and the entire LGBTQ patient population.18–20
Clinicians can play a vital role in providing reproductive health services to LGBTQ AYA people with cancer. When social workers, psychologists, physician assistants, and nurse practitioners, also defined as AHPs, were surveyed on their knowledge and attitudes on providing care to LGBTQ people with cancer, the results showed high levels of comfort in providing medical care, but low knowledge regarding specific psychosocial needs of LGBTQ cancer patients.21
Both oncologists and AHPs surveyed desired additional education on the needs of LGBTQ patients with cancer. Educating Nurses about Reproductive Issues in Cancer Healthcare (ENRICH) and Enriching Communication Skills for Health Professionals in Oncofertility (ECHO) engage AHPs in training opportunities to learn about the reproductive and fertility needs of AYA cancer patients,22 but does not contain specific information on the needs of LGBTQ AYA. We conducted a mixed-method survey of former ENRICH/ECHO trainees to assess their experiences and reservations providing care to LGBTQ AYAs and their educational needs to provide reproductive health care to LGBTQ AYAs diagnosed with cancer.
Methods
A multi-method survey with 28 quantitative items and 4 open-ended items was sent electronically by Qualtrics to 686 past ENRICH & ECHO participants who completed the training between 2010 and 2019. After the completion of the survey, data were downloaded from Qualtrics. This project underwent institutional review board review and was deemed exempt by the University of South Florida's institutional review board.
The survey remained open from May to June 2020; 351 participants completed the survey (51% response rate). Survey items were based on a validated survey developed for oncology physicians.15,23 Broadly, clinician knowledge, clinician confidence discussing reproductive health with AYA patients, and confidence in understanding of reproductive health needs and general health needs were assessed. Knowledge items were assessed using a true/false response format and examples included the following: “heterosexual/straight women have more risk factors for breast cancer than lesbian women,” and “LGBTQ AYA patients avoid accessing health care due to difficulty communicating with providers.”
Table 1 contains a full description of knowledge items and the associated correct answer. Clinicians were asked to rate their level of confidence in discussing reproductive health with LGBTQ AYAs, their confidence in reproductive health needs, and confidence in general health needs for each LGBTQ group: gay or bisexual, bisexual or queer, and transgender or nonbinary. All confidence questions were rated on a 5-point Likert scale (strongly disagree to strongly agree). We report here on the quantitative and qualitative results.
Table 1.
Items Assessing Clinician Knowledge
| Knowledge items (true/false) | Correct answer |
|---|---|
| LGBTQ AYA patients avoid accessing health care due to difficulty communicating with providers | True |
| HPV-associated cervical dysplasia is only found in people with a history of penis in vagina intercourse | False |
| Heterosexual/straight women have more risk factors for breast cancer than lesbian women | False |
| Regularly screening gay and bisexual men for anal cancer through anal pap testing can increase life expectancy | True |
| LGBTQ individuals tend to have a higher prevalence of smoking compared to non-LGBTQ individuals | True |
| Gay male individuals tend to engage in more sun-seeking behaviors (i.e., tanning) compared to straight men | True |
| LGBTQ individuals tend to have a higher prevalence of smoking compared to non-LGBTQ individuals | True |
AYA, adolescent and young adult; HPV, Human Papillomavirus.
Quantitative analysis
Descriptive statistics were used to summarize clinician demographic and practice characteristics, knowledge items, and confidence items. Knowledge items were scored as correct/incorrect. Clinicians who answered 6–7 items correct were placed into the high knowledge group, those with 4–5 items correct were placed in the moderate knowledge group, and those with 0–3 items correct were placed in the low knowledge group. Chi square tests examined differences in confidence discussing reproductive health and confidence in knowledge of reproductive health needs and health needs by knowledge group. Within the confidence in knowledge of health need/reproductive health need items, responses of strongly disagree/disagree and strongly agree/agree options were collapsed to create one “disagree” variable and one “agree” variable. Monte Carlo simulations were conducted to examine differences by clinician type in confidence in knowledge of health needs/reproductive health needs and confidence discussing reproductive health with AYA patients.
Qualitative analysis
Of those who completed the survey, 290 included a written response to at least one of the four open-ended items and were included in the qualitative analyses reported herein. Responses were analyzed using inductive content analysis and the constant comparison method and guided by COREQ quality standards for qualitative research.24,25 Open coding was applied to inductively identify themes within each question. Themes were considered if they represented a meaningful pattern in the data. Using an Excel file created from all responses, and divided by the question to which it pertained, two coders (A.S. and G.Q.) reviewed all responses and generated a list of potential codes, noting the strength of pattern in data (e.g., the majority, a few). Each code was refined through comparison and discussion, and re-organized into key themes and subthemes until consensus was reached.
Consistent with the iterative nature of qualitative inquiry, the analytic phases were repeated until all coding discrepancies were resolved and no novel codes emerged (i.e., saturation). Inter-rater reliability was calculated among the two coders by creating a numbered list of all comments for each question and identifying the number of times each coder had labeled/rated the comment as belonging with one of the finalized codes. The level of agreement between the two coders was 0.90 (kappa coefficient). Results were organized by key themes and exemplar quotes are used to further describe each theme. Open comments were anonymous; therefore, demographics of those who provided comments are not available.
Quantitative results
Participants
Respondents were primarily White (n = 250, 80%) and averaged 41 years old, and the majority identified as cisgender female (n = 283, 87%). Respondent professions were primarily Registered Nurses (n = 109, 37%) or licensed clinical social workers (n = 47, 16%). Table 2 provides a full description of the sample and their practice characteristics.
Table 2.
Clinician and Practice Characteristics (n = 351)
| M (SD) | Range | |
|---|---|---|
| Clinician age | 41 (9.6) | 20–66 |
| Year of graduation from professional school | 2006 (9.5) | 1976–2020 |
| Clinician gender | n (%) | |
| Nonbinary | 7 (2.1) | |
| Cisgender female | 283 (86.8) | |
| Cisgender male | 12 (3.7) | |
| Transgender female | 1 (0.3) | |
| Transgender male | 0 | |
| Other | 7 (2.1) | |
| Prefer not to answer | 16 (4.9) | |
| Race/ethnicity | ||
| American Indian or Alaska Native | 1 (0.3) | |
| Asian | 21 (6.8) | |
| Black or African American | 11 (3.5) | |
| Hispanic, Latino, or Spanish | 22 (7.1) | |
| Middle Eastern or North African | 0 | |
| Native Hawaiian or other Pacific Islander | 1 (0.3) | |
| White | 250 (80.4) | |
| Other/not sure | 2 (0.6) | |
| Prefer not to answer | 3 (1.0) | |
| Sexual orientation | ||
| Bisexual | 15 (4.7) | |
| Gay | 1 (0.3) | |
| Heterosexual/straight | 285 (89.3) | |
| Lesbian | 5 (1.4) | |
| Queer | 2 (0.6) | |
| Not sure/questioning | 1 (0.3) | |
| Other | 1 (0.3) | |
| Prefer not to answer | 9 (2.8) | |
| Licensure | ||
| Advanced Practice Registered Nurse | 26 (8.8) | |
| Licensed Clinical Social Worker | 47 (16.0) | |
| Master of Social Work | 11 (3.7) | |
| Nurse Practitioner | 32 (10.9) | |
| PhD | 32 (10.9) | |
| PSYD | 12 (4.1) | |
| Registered Nurse | 109 (37.1) | |
| Other | 23 (7.8) | |
| Prefer not to answer | 2 (0.7) | |
| No. of patients seen per week | ||
| 0–25 | 179 (55.4) | |
| 26–50 | 98 (30.3) | |
| 51–75 | 27 (8.4) | |
| 76–100 | 8 (2.5) | |
| >100 | 6 (1.9) | |
| Do not know or prefer not to answer | 5 (1.5) | |
| Approximate percentage of patients in the last year who have identified themselves at LGBTQ | ||
| None | 12 (3.7) | |
| 1%–5% | 159 (48.9) | |
| 6%–10% | 79 (24.3) | |
| 11%–15% | 23 (7.1) | |
| 16%–20% | 17 (5.2) | |
| >20% | 3 (0.9) | |
| Do not know/prefer not to answer | 32 (9.8) | |
LGBTQ, lesbian, gay, bisexual, transgender/queer questioning.
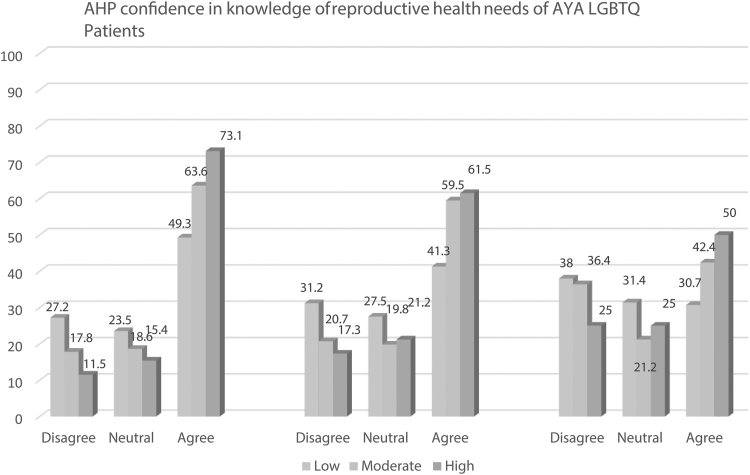
Respondents reported their confidence discussing reproductive health with each LGBTQ AYA patient group. The majority agreed (72.9%) they were confident discussing reproductive health topics with AYA patients who identify as lesbian or gay, agreed (68.2%) to being confident discussing with patients identifying as bisexual or queer, and were slightly less likely to agree (54.7%) they are confident discussing with those identifying as nonbinary or transgender. In terms of confidence in reproductive health needs, the majority agreed (58%) to being confident in their knowledge of reproductive health needs of patients identifying as lesbian or gay and agreed (51.1%) to confidence in knowledge of reproductive health needs of those identifying as bisexual or queer, yet were less likely to agree (38.7%) regarding those identifying as transgender or nonbinary.
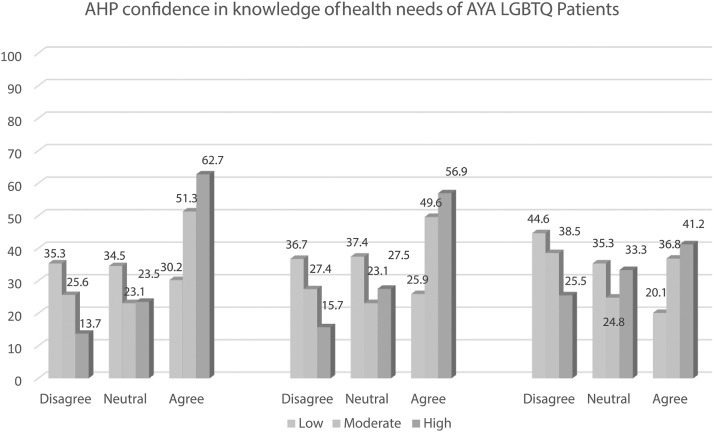
AHP confidence in knowledge of overall health needs of each AYA-LGBTQ group was generally lower across each group and particularly low regarding transgender or nonbinary patients, with only 43.3% agreeing to being confident in their knowledge of health needs of patients who identify as lesbian or gay, 39.7% agreeing regarding confidence in knowledge of health needs of those who identify as bisexual or queer, and 29.8% agreeing regarding those who identify as transgender or nonbinary.
AHPs were placed into one of three categories based on their correct responses to the seven knowledge items. The majority of AHPs answered 0–3 items correctly and fell into the low knowledge group (45%), 38.2% answered 4–5 items correctly and fell into the moderate knowledge group, and 16.8% answered 6–7 items correctly and fell into the high knowledge group.
Confidence in knowledge of health needs and reproductive/sexual health needs by level of AHP knowledge
AHPs in the high knowledge group reported feeling confident in their knowledge of health needs of all AYA-LGBTQs: gay or lesbian [χ2(4, n = 307) = 21.56, p < 0.001]; bisexual or queer [χ2(4, n = 307) = 23.55, p < 0.001], and transgender or nonbinary [χ2(4, n = 307) = 14.23, p < 0.01] (Fig. 1). Similarly, those in the high knowledge group demonstrated significantly greater confidence in knowledge of reproductive health needs of patients identifying as gay or lesbian [χ2(4, n = 307) = 11.15, p < 0.05] and patients identifying as bisexual or queer [χ2(4, n = 307) = 11.18, p < 0.05] (Fig. 2). No significant difference was observed in confidence in knowledge of reproductive health needs of patients identifying as transgender or nonbinary and in confidence discussing reproductive health with all AYA-LGBTQs by clinician level of knowledge.
FIG. 1.
AHP confidence in knowledge of health needs among AYA-LGBTQ patients by level of AHP knowledge (n = 351). AHP, Allied Health Professionals; AYA, adolescent and young adult; LGBTQ, lesbian, gay, bisexual, transgender/queer questioning.
FIG. 2.
AHP confidence in knowledge of reproductive health needs among AYA-LGBTQ patients by level of AHP knowledge (n = 351).
Differences in knowledge and confidence by AHP specialty
No significant difference was observed by AHP type in confidence discussing reproductive health with AYA patients and confidence in knowledge of health needs, and reproductive health needs.
Qualitative results
Respondents were asked to “describe any personal experiences treating LGBTQ AYA patients with cancer or survivors that you consider important.” A minority said they had no experience with this population. From those who did report experiences, the majority focused on issues related to their own lack of experience and a desire for more training. There were four major trends among the experiences reported:
Identity disclosure: who knows, who does not know, and who should know
Respondents noted the challenges of maintaining confidentiality when the patient had disclosed their SOGI to the provider, but the patients' parents were unaware or disapproved of their child's choice.
I did take care of a transgender patient ….and I remember there being a lot of discussion within the medical team about pronouns, making sure we call (the patient) the preferred name, and being careful about what conversations were had in front of the parent who disapproved of child's choice.
Teenage transgender (patient) who was ‘out’ with peers and at school opted to identify as sex assigned at birth during cancer treatment to simplify things for parents. I wonder about prevalence of this?
I ….have had several patients ‘come out’ ….during treatment. For one patient, I was only the 3rd person he had told. I worked with him on talking with his parents.
Participants also reported concerns about navigating situations in which they knew the SOGI of patients, but others on the care team did not.
I have encountered many LGBTQ patients/survivors who are not ‘out’ with their care team…. This leads to decreased support (not inviting partners to come to visits, or the partner being presumed to be a sister/brother/friend, or potential risk behaviors not being addressed, or assumed risk behaviors being lectured on, or reproductive options not being correctly addressed with resources).
I was working with a patient who disclosed sexual orientation to me, but was not out with other providers. It was difficult for me to know how to convey important information to … med onc team that was related to orientation (e.g., had just lost partner), but not disclose sexual orientation which patient considered private information.
Fertility: who is interested?
About half of respondents commented specifically on issues related to fertility among LGBTQ AYA patients with cancer. These comments tended to focus on clinicians' assumptions that LGBTQ AYA were less interested in fertility preservation and misperceptions among LGBTQ AYA about their family-building options
I believe that a lot of healthcare professionals do not address fertility issues with LGBTQ patients and survivors assuming that they do not want children.
In informing my practice of LGBTQ AYA patients with cancer, I have learned a lot from an older gay man about family planning needs and how culture can influence family planning. In essence, he chose to give up on a family because adoption was not possible as it was more important for him to choose authenticity, even though this is a regret in his life. I am reminded of my privilege as a heterosexual cisgender woman, something I have taken for granted throughout my life.
I had a male, gay patient who originally declined sperm banking. His stated reason was ‘I'm gay.’ We discussed that many gay men have chosen to have biological or adopted children. After discussing use of stored sperm, he decided to proceed with sperm banking.
(The medical record) …cited sexual orientation as reason patient did not want to do fertility preservation—Seemingly did not plan to naturally have children before cancer diagnosis
A few comments were specific to participants' experiences engaging in fertility discussions with transgender AYAs with cancer. Providers wondered how to tailor conversations about fertility to simultaneously acknowledge patients' gender identity and discuss options based on gametes available. Participants also described instances in which transgender people were not offered preservation.
I was asked to do a fertility consult for a newly diagnosed young adult patient. The patient's name in the chart was masculine, and gender was male, but the name the medical team told me was more feminine and not their given name. They then told me that she was transgender. Had I not gone in knowing that she was biologically a male, and addressed fertility preservation for a male, it would have made her even more distrustful than she already was, and really compromised trust.
Patient was offended when I explained sperm banking…. Patient said they didn't associate sperm with their body, although they were assigned male at birth.
I specifically have had [transgender] patients/survivors who were not offered fertility preservation, contraception…and end of life discussions due to and/or appropriate for their ….status.
Reservations treating the LGBTQ AYA population
Respondents were asked if they had any reservation treating the LGBTQ AYA population. All said they had no moral or value-based reservations, but the majority noted feeling they lacked knowledge and wanted more education.
I need to know more about increased health risks to this population, as well as differences in attitudes about sexuality/fertility/reproductive and sexual health.
The needs for education focused on gender-affirming hormones or puberty blockers and their impact on cancer and fertility.
Would love to know more about fertility preservation and puberty blockers and/or HRT care for trans patients undergoing cancer treatment.
I feel like my knowledge gap is in hormone replacement, contraception and other related concerns with transgender care.
About half of the respondents focused on lack of comfort with using correct pronouns for transgender and nonbinary patients.
I do worry that I may make not use the correct pronouns every time. It is important to me to treat the LGBTQ AYA patient with respect.
This same group also had concerns that their lack of knowledge may offend or upset a patient.
I worry I won't say the right things. I feel as though I need further education to make them feel completely comfortable and at ease having our clinic provide them care. This is so important!
LGBTQ-friendly environments
Several respondents noted a lack of supportive environment based on inadequate intake forms for collecting SOGI data or living in a geographic area that was “conservative.”
No reservations personally, though I would prefer that my institute have more accepting and open practices that may help the LGBTQ AYA population feel more comfortable (e.g., including gender identity/pronouns on intake forms).
I live in a more conservative state, and the ignorance and bias is an issue where we have even had staff refused to care for them, refused to acknowledge their preferred names or pronouns, etc. It's unfortunate….
Respondents were asked what suggestions they had for improving the sexual and reproductive health, and cancer care of the LGBTQ AYA population. All respondents said more education and training. Specific content of training was related to fertility care and sexual health, taking a sexual history and creating welcoming environments.
I think there is a lot to be learned about the LGBTQ population and how it relates to reproductive health, fertility, and cancer treatment, as well as more generally in the context of health-care.
….actual training and chances to practice interactions of using gender neutral pronouns; asking about sexual practices of the person in front of you (i.e., not all people who report being lesbian have had no sex with a man, consensual or otherwise) and not presuming you know what people are doing or at risk for…
Creating welcoming environment explicitly (normalizing of asking…. pronouns, having literature on LGBTQ health issues in the clinic) would be helpful in building trust between patients and health care providers.
Have LGBTQ specific written materials on sexual health…. And fertility and family building.
Discussion
Survey respondents believed all patients deserve affirming care and they would like more education and guidance to provide welcoming environments, reproductive health, and cancer care to their LGBTQ AYA patients. These training needs were clear in explicit statements by respondents and may be noted by the language used in responses such as outdated words, wording that infers blame or sexual orientation as choice, and other phrases that illustrate lack of knowledge of inclusive and affirming care. A desire for LGBTQ education has been seen in other contexts such as general cancer care,15 nursing education,26 dentistry,27 and resident training programs.28
The majority of our survey participants also demonstrated low (45%) or moderate (38.2%) knowledge on various items related to risk factors, screening, health behaviors, and access to care among AYA LGBTQ cancer patients. This also illustrates the need and benefit for training targeted toward providers who treat LGBTQ AYA patients. There is limited research on the effectiveness of training programs focused on LGBTQ cancer care and even less so among AYAs. Existing research has demonstrated increases in knowledge among providers and increased awareness of strategies to implement in clinical practice when treating LGBTQ AYAs.29
The need to use affirming language, but the inability to document or identify name and pronouns was cited as a barrier to care; respondents noted that electronic medical record documentation standards were challenging to capture a patient's correct pronoun and name, especially for nonbinary and transgender patients. This issue represents a challenge across hospital systems that have not yet adopted agile Electronic Medical Record systems to document sex assigned at birth, organ inventories, and gender identity. Lapinski et al. recommends utilizing organ inventories as a routine part of assessments to better provide affirming care.5
Other issues identified from respondents focused on confidentiality, especially when working with multidisciplinary teams where only one member was aware of a patient's sexual orientation or gender identity. More problematic was when a parent was unaware, as this creates conflict between protecting the patient's privacy and using affirming language or properly addressing supportive care persons and caregivers. Ancker et al. examined how right to privacy and confidentiality would impact the clinician/patient relationships, identifying teens and young adults would not share information with their medical team if a parent had access to their medical record.30
Our quantitative results demonstrate that provider level of knowledge and provider confidence in knowledge appear to be related, such that those who demonstrated high knowledge also reported higher confidence in knowledge of health needs and reproductive health needs of AYA patients who identify as gay or lesbian and bisexual or queer. While providers in our study demonstrated high confidence in reproductive health needs and in discussing reproductive health with each AYA LGBTQ patient group (gay or lesbian; bisexual or queer; transgender or nonbinary), providers were less confident in overall health needs across each group. In addition, provider confidence consistently appeared lower regarding care in every category of transgender or nonbinary AYAs.
These results align with qualitative results demonstrating that clinicians noted difficulty in using affirming language specifically when discussing fertility preservation and sexual health. Trans and nonbinary patients may have their own language for how they refer to their body parts and there is no “one size fits all” in terms of the “right words” to use for each patient.5,31 Thus, education should be focused on encouraging collaborative relationships between patients and providers where providers feel empowered to ask patients what they need and patients feel safe telling providers.32 This is needed for all aspects of cancer care, but even more so specific to fertility and preservation.
Language is just one element of education, as our respondents also noted gaps in clinical aspects of caring for patients receiving puberty blockers and hormone replacement therapy, pursuing fertility preservation. While all patients pursuing fertility preservation have to suspend the use of puberty blockers, those taking gender-affirming hormones can sometimes still pursue oocyte and sperm banking.33 Estrogen has been shown to potentially affect spermatogenesis and testosterone effects on ovarian function are less clear.33 Gender-affirming hormones are not a contraindication to pursuing fertility preservation.33 All cancer patients on gender-affirming hormones should be counseled on fertility preservation following ASCO guidelines.34
LGBTQ AYA patients with cancer represent a diverse population with differing interests, goals for care, perceived bias and discrimination, and experiences of bias and discrimination that can shape the care they receive. Similarly, providers vary in their level of knowledge and exposure to different communities of patients, which shape the care they provide.
Respondents noted instances of misconceptions regarding LGBTQ AYA desire for family building. Russell et al. found LGBTQ AYA cancer survivors were just as likely as heterosexual cancer survivors to report not being fully informed of cancer's potential effect on future fertility.17 Clinicians conflated sexual orientation with desire not to pursue fertility preservation. SOGI have a documented effect on desire for family building, but clinicians should follow their patient's lead and make no assumption about individual patient's family building desires.35 Furthermore, family building options such as adoption may also be fraught with perceived or actual discriminatory practices.36
A common theme that arose was the difficulty in navigating the clinical environment where care was provided. Lack of appropriate intake forms represented a structural barrier to documenting SOGI information in the clinic. Rullo et al. found that 97% of patients accepted SOGI disclosure as a routine part of clinical data collection.37 Respondents in conservative states noted that regardless of education, staff often objected to using affirming language for patients. These institutional barriers reflect issues in providing affirming care that goes beyond educating individual clinicians. Few existing interventions focus on how to change health care system operations on a macro level, and this is a limitation to clinician-focused education.38
However, educating individuals can affect change institutionally by creating champions. Menkin et al., names organizational buy-in and health system polices as essential components of high-quality inclusive LGBTQ+ care.38 Macro level education could be a tool to address systematic barriers to care. Similar to institution wide compliance or sexual harassment training, institutions should implement LGBTQ health training to address the structural issues specific to their locality. In addition, institutions could designate LGBTQ navigators similar to AYA specialists within cancer centers who provide resources to patients and training to staff.
In the interim, training on LGBTQ reproductive health must also include ways to navigate structural barriers for LGBTQ AYA patients. Providers can learn how to create additional notes on their existing intake forms to document SOGI status and tactics to encourage resistant staff to use affirming language. Respondents reported feeling “stuck” in their encounters where they were unable to provide affirming care at the fault of their own lack of education or barriers beyond their control. Education can begin by providing knowledge to clinicians to apply affirming language in their patient encounters and expand to empowering clinicians to become leaders creating welcoming environments within their clinics.
Finally, clinicians should consider that LGBTQ AYA patients with cancer may be as equally interested or disinterested as cisgender/heterosexual patients in their desire for future children. In addition, LGBTQ is not a monolith, and each subgroup may have unique cancer and family building considerations. Having open discussions about fertility preservation options and future family building techniques may seem foreign to LGBTQ patients who may be unaware of the variety of options that exist. Improved patient counsel can be facilitated by increasing clinician training in the approach to the discussion and the use of patient educational materials that are not heteronormative.
Limitations
This study has several limitations. First, the sample had already participated in a general training on the reproductive health needs of AYA cancer patients; therefore, their knowledge and confidence may be higher than the general population of AHPs. Second, not all respondents answered every item or provided a response to the open-ended questions. Finally, due to the anonymous nature of the survey, we were unable to link demographic information to the open-ended comments.
Conclusions
Clinicians who provide care for AYA patients with cancer must recognize that some of these patients identify as LGBTQ. By creating welcoming environments where patients feel safe answering questions, clinicians can effect change in their institutions. The majority of prior ENRICH/ECHO learners wanted additional training in approach to reproductive health care for LGBTQ AYA with cancer. Providers' level of knowledge and confidence in LGBTQ AYA needs demonstrated in our study illustrate this need for training as well.
Macro and micro interventions have a role in improving care for LGBTQ AYA cancer patients, recognizing that institutional changes as well as clinician education play a role in delivery of care. More research is needed on the family building desires and experiences of LGBTQ AYA patients with cancer and how the oncology community can best provide affirming information in a welcoming environment. This research will inform changes in care at both the individual and the institutional level as more clinicians learn and see the evidence, more clinicians can become advocates for affirming care, and more LGBTQ patients feel safe to disclose their identities and share their experiences.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This project was funded by a supplement from the National Institutes of Health/National Cancer Institute: 3R25CA142519-09S1 LOvE (LGBT Oncofertility Education) ECHO Administrative Supplement to R25: Enriching Communication Skills for Health Professionals in Oncofertility (ECHO).
References
- 1. Bleyer A, Barr R, Hayes-Lattin B, et al. . The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8(4):288–98. [DOI] [PubMed] [Google Scholar]
- 2. Carter J, Penson R, Barakat R, Wenzel L. Contemporary quality of life issues affecting gynecologic cancer survivors. Hematol Oncol Clin North Am. 2012;26(1):169–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(5):386–405. [DOI] [PubMed] [Google Scholar]
- 4. Partridge AH, Gelber S, Peppercorn J, et al. . Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22(20):4174–83. [DOI] [PubMed] [Google Scholar]
- 5. Lapinski J, Covas T, Perkins JM, et al. . Best practices in transgender health: a clinician's guide. Prim Care. 2018;45(4):687–703. [DOI] [PubMed] [Google Scholar]
- 6. Reinman L, Coons HL, Sopfe J, Casey RJC. Psychosexual care of adolescent and young adult (AYA) cancer survivors. Children (Basel). 2021;8(11):1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Griggs J, Maingi S, Blinder V, et al. . American Society of Clinical Oncology Position Statement: strategies for reducing cancer health disparities among sexual and gender minority populations. J Clin Oncol. 2017;35(19):2203–08. [DOI] [PubMed] [Google Scholar]
- 8. Morales C. More Adult Americans Are Identifying as L.G.B.T., Gallup Poll Finds. 2021. Accessed April 2, 2022 from: https://www.nytimes.com/2021/02/24/us/lgbt-identification-usa.html?register=email&auth=register-email.
- 9. Scott AR, Stoltzfus KC, Tchelebi LT, et al. . Trends in cancer incidence in US adolescents and young adults, 1973–2015. JAMA Network Open. 2020;3(12):e2027738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kamen C. Lesbian, gay, bisexual, and transgender (LGBT) survivorship. Semin Oncol Nurs. 2018;34:52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clarke M, Lewin J, Lazarakis S, Thompson K. Overlooked minorities: The intersection of cancer in lesbian, gay, bisexual, transgender, and/or intersex adolescents and young adults. J Adolesc Young Adult Oncol. 2019;8(5):525–8. [DOI] [PubMed] [Google Scholar]
- 12. Webster R, Drury-Smith HJR. How can we meet the support needs of LGBT cancer patients in oncology? A systematic review. Radiography (Lond). 2021;27(2):633–44. [DOI] [PubMed] [Google Scholar]
- 13. Rhoten B, Burkhalter JE, Joo R, et al. . Impact of an LGBTQ cultural competence training program for providers on knowledge, attitudes, self-efficacy and intensions. J Homosex. 2022;69:1030–41. [DOI] [PubMed] [Google Scholar]
- 14. Haviland K, Burrows Walters C, Newman SJH. Barriers to palliative care in sexual and gender minority patients with cancer: a scoping review of the literature. Health Soc Care Community. 2021;29(2):305–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schabath MB, Blackburn CA, Sutter ME, et al. . National survey of oncologists at National Cancer Institute–designated comprehensive cancer centers: attitudes, knowledge, and practice behaviors about LGBTQ patients with cancer. J Clin Oncol. 2019;37(7):547–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kirubarajan A, Patel P, Leung S, et al. . Sterility. Cultural competence in fertility care for lesbian, gay, bisexual, transgender, and queer people: a systematic review of patient and provider perspectives. Fertil Steril. 2021;115:1294–301. [DOI] [PubMed] [Google Scholar]
- 17. Russell AM, Galvin KM, Harper MM, Clayman ML. A comparison of heterosexual and LGBTQ cancer survivors' outlooks on relationships, family building, possible infertility, and patient-doctor fertility risk communication. J Cancer Surviv. 2016;10(5):935–42. [DOI] [PubMed] [Google Scholar]
- 18. Klein DA, Malcolm NM, Berry-Bibee EN, et al. . Quality primary care and family planning services for LGBT clients: a comprehensive review of clinical guidelines. LGBT Health. 2018;5(3):153–70. [DOI] [PubMed] [Google Scholar]
- 19. Keuroghlian AS, Ard KL, Makadon HJ. Advancing health equity for lesbian, gay, bisexual and transgender (LGBT) people through sexual health education and LGBT-affirming health care environments. Sex Health. 2017;14(1):119–22. [DOI] [PubMed] [Google Scholar]
- 20. Lunde CE, Spigel R, Gordon CM, Sieberg CB. Beyond the binary: sexual and reproductive health considerations for transgender and gender expansive adolescents. Front Reprod. 2021;3:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sutter ME, Bowman-Curci ML, Duarte Arevalo LF, et al. . A survey of oncology advanced practice providers' knowledge and attitudes towards sexual and gender minorities with cancer. J Clin Nurs. 2020;29:2953–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Quinn GP, Bowman Curci M, Reich RR, et al. . Impact of a web-based reproductive health training program: ENRICH (Educating Nurses about Reproductive Issues in Cancer Healthcare). Psychooncology. 2019;28(5):1096–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sutter ME, Simmons VN, Sutton SK, et al. . Oncologists' experiences caring for LGBTQ patients with cancer: qualitative analysis of items on a national survey. Patient Educ Couns. 2020;104:871–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 25. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. [DOI] [PubMed] [Google Scholar]
- 26. Lim FA, Brown Jr. DV, Jones H. Lesbian, gay, bisexual, and transgender health: fundamentals for nursing education. J Nurs Educ. 2013;52(4):198–203. [DOI] [PubMed] [Google Scholar]
- 27. Aguilar E, Fried J. Enhancing dental and dental hygiene student awareness of the lesbian, gay, bisexual and transgender population. J Dent Hyg. 2015;89(1):11–6. [PubMed] [Google Scholar]
- 28. Moll J, Krieger P, Moreno-Walton L, et al. . The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med. 2014;21(5):608–11. [DOI] [PubMed] [Google Scholar]
- 29. Pratt-Chapman ML, Goltz H, Latini D, et al. Affirming Care for Sexual and Gender Minority Prostate Cancer Survivors: results from an Online Training. J Cancer Educ. 2020; 10.1007/s13187-020-01930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ancker JS, Sharko M, Hong M, et al. . Should parents see their teen's medical record? Asking about the effect on adolescent–doctor communication changes attitudes. J Am Med Inform Assoc. 2018;25(12):1593–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moseson H, Lunn MR, Katz A, et al. . Development of an affirming and customizable electronic survey of sexual and reproductive health experiences for transgender and gender nonbinary people. PLoS One. 2020;15(5):e0232154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kamen CS, Alpert A, Margolies L, et al. . “Treat us with dignity”: a qualitative study of the experiences and recommendations of lesbian, gay, bisexual, transgender, and queer (LGBTQ) patients with cancer. Support Care Cancer. 2019;27(7):2525–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Quinn GP, Tishelman AC, Chen D, Nahata L. Reproductive health risks and clinician practices with gender diverse adolescents and young adults. Andrology. 2021;9(6):1689–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Oktay K, Harvey BE, Partridge AH, et al. . Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994–2001. [DOI] [PubMed] [Google Scholar]
- 35. Chen D, Matson M, Macapagal K, et al. . Attitudes toward fertility and reproductive health among transgender and gender-nonconforming adolescents. J Adolesc Health. 2018;63(1):62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Goldberg AE, Frost RL, Miranda L, et al. . LGBTQ individuals' experiences with delays and disruptions in the foster and adoption process. Child Youth Serv Rev. 2019;106:104466. [Google Scholar]
- 37. Rullo JE, Foxen JL, Griffin JM, et al. . Patient acceptance of sexual orientation and gender identity questions on intake forms in outpatient clinics: a pragmatic randomized multisite trial. Health Serv Res. 2018;53(5):3790–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Menkin D, Tice D, Flores D. Implementing inclusive strategies to deliver high-quality LGBTQ+ care in health care systems. J Nurs Manag. 2020. [Epub ahead of print]; DOI: 10.1111/jonm.13142. [DOI] [PubMed] [Google Scholar]