Abstract
Stress in the context of the COVID-19 pandemic may have a significant impact on health, including sleep health. Older adults may be particularly vulnerable. This study examined associations between perceived stress and sleep health, mental health, physical health, and overall perceived health outcomes among older adults. We also examined whether specific coping strategies moderate these associations. Older adults (n = 115; Mage = 68.62) reported perceived stress, coping strategies, global sleep quality, depressive symptoms, and perceived mental, physical, and overall health before and during the COVID-19 pandemic. Stress-health relationships were modelled with hierarchical linear regression. Higher perceived stress was associated with greater depressive symptoms and poorer mental health concurrently and longitudinally. Coping strategies moderated the association of perceived stress with physical health and overall perceived health. For example, higher perceived stress was associated with poorer overall perceived health among those with lower problem-focussed coping, but not among those with higher problem-focussed coping. Older adults may benefit from prevention and intervention strategies targeting stress management. Furthermore, identifying people with low problem-focussed coping might be a useful strategy to prevent worsening health in future public health crises.
Keywords: coping strategies, COVID-19 pandemic, older adults, perceived stress, sleep health
1 |. INTRODUCTION
The coronavirus (SARS-CoV-2) pandemic of 2019 (COVID-19) has caused an unprecedented public health crisis in the United States and around the world (Dong et al., 2020). Although the COVID-19 pandemic has taken a significant toll on almost all populations (Estes & Thompson, 2020), its impact may vary based on age. Approximately 80% of COVID-19 pandemic-related deaths reported in the United States were among adults aged 65 and older, as of December 2020 (Centers for Disease Control and Prevention, 2020). Therefore, older adults have been considered, as a group, at high risk in the face of the COVID-19 pandemic (De Pue et al., 2021). In addition to the direct impact of COVID-19 on morbidity and mortality, older adults have been challenged by severe disruptions in their daily routines and fear of illness and death (Hwang et al., 2020; Pearman et al., 2020). Furthermore, older adults have been challenged by loneliness and isolation due to the lack of physical and social contact with other family members and friends (Chin & Cohen, 2020; Chin et al., 2018; Luanaigh & Lawlor, 2008; Ong et al., 2016). Such disturbances may negatively impact health and wellbeing among this vulnerable population.
Numerous studies have examined the effects of COVID-19 on health issues such as sleep, mental, and physical health (e.g., Fuller & Huseth-Zosel, 2021; Grossman et al., 2021; Shrira et al., 2020; Whitehead & Torossian, 2021). The COVID-19 pandemic affected sleep patterns positively for some individuals, but negatively for others. For example, Gao and Scullin (2020) examined sleep patterns among adults aged 22–75 by collecting cross-sectional, retrospective, and longitudinal data (February 2020 before quarantine phase vs. March 2020 during quarantine phase). They found that some individuals experienced unchanged or improved sleep, but others experienced an increase in sleep problems during the quarantine phase compared to before the quarantine phase of the COVID-19 pandemic (Gao & Scullin, 2020). These individual differences in why some people had improved and others worsened sleep during the pandemic can be explained by levels of perceived stress or stress vulnerability, shift work, presence of COVID-19 symptoms, adverse life impact, and caregiving status (Gao & Scullin., 2020). Furthermore, Rezaei and Grandner (2021) examined sleep patterns across all adult populations who used a Fitbit and found that individuals tended to sleep longer, later (i.e., sleep phase shifted later), and with more regular bedtimes (due to decreased weekday-weekend differences) during the COVID-19 pandemic compared to before. However, these findings are limited by the use of historical data that included different individuals, rather than examining within-persons differences (i.e., longitudinal analysis). More directly relevant to the current study, De Pue et al. (2021) found that sleep quality in adults 65 years of age and older decreased during the pandemic compared to before the pandemic. However, this study was cross-sectional in design, relying on participants to recollect their pre-pandemic sleep, and was also based on a single sleep quality item.
In addition to sleep health, the COVID-19 pandemic also affected mental and physical health issues of individuals. The disruptions to daily routines, fear of illness, death, and isolation, limited access to healthcare, and social and economic hardships may lead to mental health issues, such as anxiety and depression, as well as physical health issues. For example, Bailey et al. (2021) found that older adults, while cocooning in a cohort of community-dwelling people aged ≥70 years, reported their mental and physical health declined, and that 70% of participants exercised less frequently or not at all. However, this study is limited to a single administration to examine the decline in health, rather than utilizing a longitudinal analysis.
Overall, most previous studies were limited to cross-sectional or retrospective data. In order to fully understand the impact of the COVID-19 pandemic on health outcomes of older adults, it is important to capture changes of health in older adults at the individual level from the pre COVID-19 period to the current pandemic period utilizing a longitudinal design. The present study examined concurrent and longitudinal associations between perceived stress, coping strategies, and health outcomes of older adults in the context of the COVID-19 pandemic.
This study, in particular, is guided by the transactional theory of stress and coping (Folkman, 1997, 2008; Lazarus & Folkman, 1984), which posits that stress is a product of a transaction (interaction) that occurs between a person and his or her complex environment. In other words, when demands (pressure) outweigh the resources of the individual (i.e., the individuals’ ability to cope with stress), the situation is regarded as a threat. Stressors may affect health and wellbeing through cognitive appraisals and coping. First, individuals engage in two appraisal processes. The ‘primary appraisal’ involves determining whether a stressor is threatening, harmful, or challenging. The perception of a threat triggers a ‘secondary appraisal’ to assess the controllability of the stress and the coping efficacy. Then, individuals engage in coping strategies. Coping refers to ‘cognitive and behavioural efforts to master, reduce, or tolerate the internal and/or external demands that are created by the stressful transaction’ (Folkman, 1984, p. 843). All in all, the stressor in our study is the COVID-19 pandemic, stress appraisals in our study are the perceived stress in the context of the COVID-19 pandemic, and coping in our study represents COVID-19 pandemic related coping strategies.
Heightened stress in the context of the COVID-19 pandemic in older adults can impact various dimensions of health such as sleep health (Grossman et al., 2021), mental health (Shrira et al., 2020), physical health (Moro & Paoli, 2020), and overall perceived health across the pre-COVID-19 to the pandemic period. Stress, in particular, chronic stress, negatively impacts mental and physical health outcomes of older adults (Cohen et al., 2007; Robinson-Whelen et al., 2000). However, less is known about older adults’ perceived stress in relation to health outcomes. Individuals perceive specific stressors differently based on inner or external resources they have. Furthermore, subjective measures of stress are often more informative than objective measures of stress in predicting health and well-being (e.g., Solomon et al., 1987). Thus, the current study focussed on perceived stress and its implications for health outcomes concurrently and longitudinally. Furthermore, because sleep problems, mental health issues, and physical health issues tend to co-occur (Stone & Xiao, 2018), this study examined multiple categories of health outcomes including sleep health, mental health, physical health, and overall perceived health to allow for a more complete understanding of the role of perceived stress on health outcomes of older adults in the context of COVID-19.
Coping occurs in response to perceived stress, and specific coping strategies can moderate the relationship between perceives stress and health outcomes (Cohen & Wills, 1985; Schnell & Krampe, 2020). People typically use a mixture of several coping strategies, which may vary for each individual depending on the specific stressor (Carver et al., 1989; DeLongis & Holtzman, 2005). Coping strategies can serve as a moderator when the relationships between stress and health outcomes are dependent on the degree to which individuals habitually use certain coping strategies (e.g., individuals who use more problem-focussed coping vs. individuals who use less problem-focussed coping) (e.g., Frese, 1986). Furthermore, the stress-buffering hypothesis posits that the perceived availability of social support can buffer the impact of perceived stress on outcomes of interest, including health outcomes (Cohen & Wills, 1985; Schnell & Krampe, 2020). In this study, we focussed on the moderating role of coping strategies as well as the buffering effects of social support between perceived stress and health outcomes. A few other studies also examined the moderating role of coping strategies in the context of the COVID-19 pandemic (e.g., Lorenzo et al., 2021; Saalwirth & Leipold, 2021). For example, a study based on adults aged 18–73 in Germany found that the most used coping strategies among participants during the beginning of the COVID-10 pandemic were meaning-and problem-focussed (Saalwirth & Leipold, 2021). Furthermore, coping moderated the relationships between worry and health outcomes; they found that problem-focussed coping enhanced positive affect and meaning-focussed coping was protective of negative affect (Saalwirth & Leipold, 2021). However, we have relatively little information regarding what coping strategies older adults frequently use in the context of the COVID-19 pandemic, and how these coping strategies moderate the impact of perceived stress on health outcomes.
While other studies have mainly focused on one aspect of health outcomes in relation to COVID-19 pandemic, the present study undertook intensive examination of perceived stress, coping strategies, and multiple categories of health outcomes including sleep health, mental health, physical health, and overall perceived health of older adults. We examined concurrent and longitudinal associations between perceived stress and sleep health, mental health, physical health outcomes among older adults (Aim 1). We expected that higher perceived stress would be associated with poorer concurrent sleep health, physical health, mental health, and outcomes. We also expected that sleep health, mental health, physical health, and status would longitudinally decline from the pre COVID-19 period to the pandemic period, and that such changes would be related to changes in perceived stress. We also examined the moderating roles of coping strategies in these concurrent and longitudinal associations (Aim 2). Even though stress, coping, and health among older adults in various contexts have been extensively examined (Moos et al., 2006), coping strategies among older adults during the COVID-19 pandemic are relatively understudied. Therefore, we aimed to identify the coping strategies among older adults frequently used during the COVID-19 pandemic first and did not specifically hypothesize whether coping strategies would buffer or exacerbate relationships between perceived stress and health outcomes. Thus, we consider these analyses exploratory.
2 |. METHOD
2.1 |. Participants and procedures
The current study was an ancillary study to a previously conducted study, which aimed to understand the sleep and health effects associated with working at night. Participants were recruited from a study investigating the long-term effects of shift work on the health of retired adults. All study procedures were approved by the university’s institutional review board. Participants provided written informed consent. Participants were recruited using flyers, television advertisements, and a university research participant registry. Participants were eligible if they were 60 years of age or older, either a former night shift worker or a former day worker, had not worked in a full-time position in the last 12 months, and were currently working a maximum of <10 h/week at part-time work. Individuals were not eligible if they used tobacco products, or had serious or unstable medical problems. Furthermore, individuals were not eligible if they reported regular use of medications (defined as three or more times a week) that affect sleep and/or the production of melatonin (only for the parent study, not for the stress and COVID-19 pandemic ancillary study). Eligible participants (N = 154) provided written informed consent, were enrolled and completed study measures. Data collection for the parent study took place between 2015 and 2019 (time 1; T1). The present study primarily uses measures from the survey portion of the study. At T1, the survey items were completed in person using an online survey.
Between May and July 2020 (time 2; T2) after the onset of the COVID-pandemic, participants were re-contacted via telephone to participate in follow-up data collection to evaluate the impact of COVID-19. At T2 the survey items were completed over the phone.
Of the 154 participants approached, 23 were unable to be contacted and 16 declined to participate, resulting in 115 participants who completed both timepoints. Participants completed the same questionnaires, including perceived stress, coping strategies, and health outcomes at T1 and T2. At T2, participants were instructed to answer the survey questions regarding perceived stress, coping strategies, and health outcomes in relation to how they were dealing with the COVID-19 pandemic. The actual questions themselves were not modified, but the instructions prefacing some questionnaires were modified. Education and shift work history were the only group differences between individuals who completed both T1 and T2 and those who did not participate in the follow up study. Individuals who completed both T1 (M = 16.11, SD = 2.07) and T2 (M = 14.97, SD = 2.13) had more years of education than those who did not complete the follow-up study (t(151) = 2.95, p = 0.004). The percentage of shift workers (41%) was lower among those who completed both T1 and T2 compared to those who did not participate in the follow-up study (64%) (X2(1, 154) = 5.32, p = 0.012). Participants were compensated for completing the study at each time point.
2.2 |. Measures
2.2.1 |. Perceived stress
Participants completed the 4-item version of the Perceived Stress Scale (PSS-4; Cohen et al., 1983; Cohen & Williamson, 1988). Items were rated from 0 (never) to 4 (very often). Two positively stated items (items 2 & 3) were reverse-coded, and scores were summed across all scale items. Higher values represent higher perceived stress. Internal consistency for the PSS in the current study was α = 0.71 at T1 and α = 0.69 at T2.
2.2.2 |. Coping strategies
Participants completed a 28-item version of the COPE inventory (Brief COPE) evaluating individuals’ strategies to cope with stress and problems at both timepoints (Carver, 1997). The Brief COPE consists of 14 subscales with two items each: Acceptance, active coping, positive reframing, planning, use of instrumental support, use of emotional support, behavioural disengagement, self-distraction, self-blame, humour, denial, turning to religion, venting, and substance use. Each item was rated from 1 (not at all) to 4 (a lot). Higher scores represent more frequent use of a particular coping strategy. Internal consistency of the scales computed based on the principal component analysis is reported in Table 1.
TABLE 1.
Descriptive statistics for key variables measuring stress, coping strategies, and health over time (n = 115)
| Time 1 |
Time 2 |
||||
|---|---|---|---|---|---|
| Constructs | Measures | M (SD) | M (SD) | Differences in repeated measures | Cohen’s d |
| Stress | Perceived stress | 2.45 (2.27) | 2.67 (2.52) | t(111) = 0.88, p = 0.38 | 0.08 |
| Coping strategies | Problem-focussed coping | 1.68 (0.90) | 1.65 (0.84) | t(113) = −0.41, p = 0.68 | 0.04 |
| Meaning-focussed coping | 1.35 (0.82) | 1.39 (0.84) | t(113) = 0.57, p = 0.57 | 0.05 | |
| Social support | 1.18 (0.81) | 1.41 (0.85) | t(111) = 2.57, p = 0.01 | 0.24 | |
| Acceptance | 2.22 (0.87) | 2.72 (0.48) | t(113) = 5.37, p < 0.001 | 0.50 | |
| Sleep | Global sleep quality score | 5.06 (3.11) | 5.51 (3.23) | t(110) = 1.55, p = 0.12 | 0.15 |
| Mental health | Depressive symptoms | 4.26 (4.71) | 5.07 (5.07) | t(112) = 1.86, p = 0.07 | 0.17 |
| Global mental health | 54.68 (6.06) | 53.66 (6.55) | t(112) = −1.58, p = 0.12 | 0.15 | |
| Physical health | Global physical health | 53.13 (6.70) | 51.48 (8.21) | t(112) = −2.57, p = 0.011 | 0.24 |
| Overall perceived health | Perceived general health | 1.88 (0.73) | 1.99 (0.76) | t(112) = 2.03, p = 0.045 | 0.19 |
2.2.3 |. Sleep
Sleep health was evaluated at T1 and T2 using the Pittsburgh Sleep Quality Index (PSQI), which consists of 18 self-rated questions (Buysse et al., 1989). The PSQI consists of seven components (with subscales ranged 0–3), each reflecting an important aspect of sleep: subjective sleep quality, sleep onset latency, sleep duration, sleep efficiency, presence of sleep disturbances, use of medication, and presence of daytime disturbances, indicating daytime alertness. The sum of these seven component scores yields one global score, with scores ranging from 0 to 21; higher scores reflect poorer sleep quality. Internal consistency for the PSQI in the current study was α = 0.73 at T1 and α = 0.61 at T2. Previous studies have found that the use of medication among older adults was weakly associated with the total score (e.g., Cole et al., 2006; Spira et al., 2012). Therefore, we also examined internal consistency for the PSQI without the medication component, which was α = 0.74 and α = 0.70 at T1 and T2, respectively.
2.2.4 |. Mental health
Two measures were used to index mental health at T1 and T2 including the Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977) and the mental health component of the RAND-12 Health Status Inventory (RAND-12). The CES-D is a 20-item self-report measure of symptoms of depression over the past week. Items were rated on a 0 (rarely or none of the time) to 3 (most or all of the time) scale. Four positively stated items (items 4, 8, 12, 16) were reverse-coded. Scores range from 0 to 60, with higher scores representing greater depressive symptoms. Cronbach’s alpha for the current study was 0.80 at T1 and 0.80 at T2 for all items.
The RAND-12 was used to create a composite measure of mental health (mental health component summary; MCS) including indices of vitality, social functioning, emotional roles, and mental health). Scoring of each item and scale is based on a single-parameter Rasch model, based on item response theory. The MCS is standardized to produce means of 50 with standard deviations of 10 in the US population, with higher scores indicating better mental health (Ware et al., 1996).
2.2.5 |. Physical health
The RAND-12 physical health component summary (PCS) included indices of physical functioning, physical roles, bodily pain, and physical health with higher scores indicating better physical health. Similar to the MCS, the PCS was normed to the US population with a mean and standard deviation of 50 and 10, respectively (Ware et al., 1996). In addition, the RAND-12 general health item, ‘In general, would you say your health is?’ measured on a scale of excellent (1) to poor (5) was used as a measure of overall perceived health (Ware et al., 1996). Use of this single item to measure overall perceived health is supported by a large body of literature, demonstrating relevant associations with other objective health outcomes, including mortality (Fechner-Bates et al., 1994; Miilunpalo et al., 1997; Wuorela et al., 2020).
2.2.6 |. Covariates
Sociodemographic covariates, age, gender, shift work history (former shift workers vs. former day workers), and the number of days between time 1 and time 2 were selected. Subjective social status has been found to be related to health outcomes and risk factors for disease, above and beyond objective measures of social status. Therefore, subjective social status was included as a covariate as well (Euteneuer, 2014).
2.3 |. Statistical analysis
2.3.1 |. Preliminary analyses
The Brief-COPE is a theoretically driven measure and is not designed to obtain an overall score. Therefore, we conducted principal components analysis (PCA) on the Brief COPE to identify factors within our older retired sample. We conducted PCA with oblimin rotation in the largest available sample of n = 154 participants at T1 to examine the factor structure of the Brief COPE in this sample of retired older adults. We used an oblimin rotation to allow factors to be correlated. We used 1) eigenvalues greater than 1 and 2) cumulative variance explained (with a target of >70%) to decide how many factors to retain. Next, descriptive analysis was performed to identify coping strategies used by older adults in the context of the COVID-19 pandemic. Finally, descriptive analyses were conducted and paired sample t-tests used to identify means of continuous variables differed between T1 and T2.
2.3.2 |. Study aim analyses
We used hierarchical linear regression to address study aims. For Aim 1, hierarchical linear regression analyses examined concurrent associations between perceived stress at T2 and health outcomes at T2 while controlling for covariates. Hierarchical regression analyses examined longitudinal associations between change in perceived stress from T1 to T2 and change of health outcomes from T1 to T2, while controlling for covariates. For Aim 2, hierarchical linear regression analyses examined whether specific coping strategies moderate associations between perceived stress and health outcomes. Predictor variables included perceived stress, individual coping strategies, and interaction effects between perceived stress and the coping strategy, while controlling for covariates (concurrent analyses). Predictor variables included change in perceived stress, coping strategies at T2, and interaction effects between change in perceived stress and each coping strategy while controlling for covariates for the longitudinal analyses. In order to examine significant interactions, we decomposed data one standard deviation above, below the mean and mean, and tested simple slopes. SPSS version 27 (IBM, 2020) was used for all analyses. Missing data in the survey averaged ∼1% (range from 0% to 3%). As missing data were minimal, we did not estimate missing data. We used pairwise deletion (available-case analysis) to handle missing data. We chose an alpha <0.05 as a threshold for statistical significance, which is appropriate for discovery-based secondary analyses. However, the large number of separate models used for questions 1 and 2 raises the risk of Type 1 error. Therefore, we also report Bonferroni-adjusted α values (p ≤ 0.001), accounting for 50 total analyses (10 for question 1 and 40 for question 2). We report actual estimated p-values for all analyses, allowing the reader to consider both unadjusted and more conservative adjusted values for interpretation.
3 |. RESULTS
3.1 |. Preliminary analyses
PCA of the Brief COPE followed by oblimin rotation revealed nine factors with eigenvalues greater than 1.0, which together accounted for 71% of the variance. Table 1 displays factors loadings of the Brief-COPE items and Cronbach’s alpha for the items included in each of nine factors across the total sample. Factor 1 includes two active coping items and two planning items. Factor 2 includes two alcohol/drug use items. Factor 3 includes two humour items. Factor 4 includes two religions and two positive reinterpretation and growth items. Factor 5 includes two denial items. Factor 6 includes two seeking of emotional support and two using instrumental support items. Factor 7 includes two self-blame and two venting of emotions items. Factor 8 includes two acceptance items. Finally, factor 9 includes two behavioural disengagement and two mental disengagement items. We conducted descriptive statistics of each of the nine factors to identify frequently used coping strategies (see the Table S1). In the current study, we focussed on the four coping strategies participants most frequently used during the COVID-19 pandemic: factors 1, 4, 6, and 8. Based on content, factor 1 was labelled problem-focussed coping, factor 4 was labelled meaning-focussed coping, factor 6 was labelled social support, and factor 8 was labelled acceptance.
Our analytic sample consisted of 115 older adults (58.3% women), ranging in age from 60 to 86 with a mean of 68.62 years old (SD = 5.41). The sample was largely white (88.7%) and non-Hispanic (99.1%). Descriptive statistics among key study variables are presented in Table 1. There were no differences in global sleep quality scores, mental health, or overall perceived health across study timepoints. However, participants reported poorer physical health during the COVID-19 pandemic than before. Pearson product-moment correlation coefficients were computed to assess the relationship between covariates and dependent variables (Table S2). We found that retired shift workers (compared to retired day workers) were likely to experience poorer sleep quality (r = 0.19, n = 111, p = 0.046). However, shift work history was not associated with other health outcomes. Table 2 presents cross-sectional and longitudinal associations of perceived stress during the pandemic with indices of sleep health, mental health, physical health. Only the final steps of the model after adjusting for covariates are presented. The level of stress experienced during the COVID-19 pandemic was cross-sectionally associated with poorer sleep measured continuously (i.e., higher total PSQI score). In contrast, change in perceived stress from T1 to T2 was not associated with change in sleep from T1 to T2. In cross-sectional analyses, the level of stress experienced during the COVID-19 pandemic was associated with greater depressive symptoms and lower levels of mental health as measured by the MCS. Moreover, increased perceived stress from T1 to T2 was associated with increased depressive symptoms and decreased global mental health scores from T1 to T2. Perceived stress during the pandemic was not associated with physical health, whether assessed concurrently or longitudinally.
TABLE 2.
Relationships between perceived stress and sleep health, mental health, physical health, and overall perceived health
| Concurrent associations between perceived stress and health outcomes |
Longitudinal associations between change of perceived stress and health outcomes |
||||||
|---|---|---|---|---|---|---|---|
| b (SE) | P * | R2/partial correlation | b (SE) | P * | R2/partial correlation | ||
| PSQI total score | 0.30 (0.11) | 2.62 | 0.26/0.25 | Change of PSQI total score | 0.14 (0.11) | 1.29 | 0.11/0.13 |
| CESD total score | 0.97 (0.17) | <0.001 | 0.35/0.50 | Change of CESD total score | 0.97 (0.14) | <0.001 | 0.34/0.51 |
| Global mental health (MCS) | −0.97 (0.23) | <0.001 | 0.24/−0.38 | Change of global mental health (MCS) | −1.10 (0.23) | <0.001 | 0.19/−0.43 |
| Global physical health (PCS) | −0.35 (0.29) | 0.24 | 0.19/−0.12 | Change of global physical health (PCS) | 0.17 (0.24) | 0.48 | 0.09/0.07 |
| Overall perceived health | 0.02 (0.03) | 0.45 | 0.30/0.07 | Change of overall perceived health | 0.01 (0.02) | 0.03 | 0.10/0.03 |
Note: Table represents the final step of the model. Table reports unstandardized coefficients (b) with standard errors (SE) in parentheses, and R Squared and partial semi correlation. Each block of estimates represents separate models for each outcome. All models control for covariates.
p is the p-value estimated for each model. Given the number of models estimated, the Bonferroni-adjusted p-value (0.001) is recommended to evaluate statistical significance.
Coping strategies moderated associations between perceived stress during the pandemic and both concurrent (Table 3) and longitudinal (Table 4) measures of health. Presented data are covariate-adjusted. Some coping strategies did moderate associations between perceived stress and both indices of physical health concurrently. However, coping strategies did not moderate any of the associations between perceived stress and indices of sleep health or mental health concurrently or longitudinally.
TABLE 3.
Moderating roles of coping strategies on the associations between perceived stress and sleep, mental health, physical health, and overall perceived health concurrently
| Problem-focussed coping |
Meaning-focussed coping |
Social support |
Acceptance |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | P * | R2/Partial correlation | b (SE) | p * | R2/partial correlation | b (SE) | p * | R2/partial correlation | b (SE) | p* | R2/partial correlation | |
| PSQI total score | ||||||||||||
| Perceived stress | 0.33 (0.15) | 0.03 | - | 0.34 (0.12) | 0.004 | - | 0.33 (0.13) | 0.01 | - | 0.29 (0.13) | 0.03 | - |
| Coping | 0.07 (0.36) | 0.85 | - | −0.31 (0.35) | 0.39 | - | −0.32 (0.35) | 0.36 | - | −0.35 (0.68) | 0.61 | - |
| Interaction | −0.08 (0.15) | 0.61 | 0.266/0.11 | −0.25 (0.16) | 0.13 | 0.28/−0.10 | −0.03 (0.11) | 0.77 | 0.27/0.07 | 0.04 (0.16) | 0.79 | 0.27/−0.12 |
| CESD total score | ||||||||||||
| Perceived stress | 0.85 (0.22) | <0.001 | - | 1.04 (0.17) | <0.001 | - | 0.93 (0.19) | <0.001 | - | 0.83 (0.19) | <0.001 | - |
| Coping | 0.43 (0.52) | 0.41 | - | −0.83 (0.51) | 0.11 | - | 0.06 (0.49) | 0.91 | - | −0.81 (0.98) | 0.41 | - |
| Interaction | 0.14 (0.21) | 0.52 | 0.35/0.33 | −0.27 (0.24) | 0.26 | 0.37/0.002 | 0.03 (0.17) | 0.86 | 0.34/0.21 | −0.20 (0.23) | 0.39 | 0.36/−0.34 |
| Global mental health (MCS) | ||||||||||||
| Perceived stress | −1.02 (0.30) | 0.001 | - | −1.08 (0.23) | <0.001 | - | −0.95 (0.24) | <0.001 | - | −1.02 (0.27) | <0.001 | - |
| Coping | −0.01 (0.72) | 0.99 | - | 1.62 (0.79) | 0.02 | - | −0.31 (0.64) | 0.62 | - | 1.72 (1.37) | 0.21 | - |
| Interaction | 0.09 (0.30) | 0.77 | 0.25/−0.20 | 0.23 (0.33) | 0.49 | 0.28/−0.03 | 0.16 (0.21) | 0.45 | 0.26 (−0.09) | −0.36 (0.33) | 0.28 | 0.26 (0.13) |
| Global physical health (PCS) | ||||||||||||
| Perceived stress | −0.67 (0.37) | 0.08 | - | −0.36 (0.30) | 0.25 | - | −0.51 (0.31) | 0.10 | - | −0.78 (0.33) | 0.02 | - |
| Coping | 1.88 (0.90) | 0.04 | - | 0.63 (0.91) | 0.49 | - | 1.23 (0.83) | 0.14 | - | −0.70 (1.70) | 0.68 | - |
| Interaction | 0.27 (0.37) | 0.46 | 0.23/−0.03 | −0.23 (0.43) | 0.59 | 0.20/−0.08 | 0.30 (0.28) | 0.29 | 0.23/0.05 | −0.89 (0.40) | 0.03 | 0.24/−0.16 |
| Overall perceived health | ||||||||||||
| Perceived stress | 0.08 (0.03) | 0.01 | - | 0.03 (0.03) | 0.35 | - | 0.04 (0.03) | 0.12 | - | 0.05 (0.03) | 0.09 | - |
| Coping | −0.28 (0.07) | <0.001 | - | −0.15 (0.08) | 0.06 | - | −0.12 (0.07) | 0.09 | - | 0.17 (0.15) | 0.25 | - |
| Interaction | −0.07 (0.03) | 0.03 | 0.40/−0.09 | 0.03 (0.04) | 0.47 | 0.33/0.11 | −0.04 (0.02) | 0.09 | 0.37/−0.13 | 0.05 (0.04) | 0.19 | 0.33/0.13 |
Note: Table represents the final step of the model. Table reports unstandardized coefficients (b) with standard errors (SE) in parentheses. Each block of estimates represents separate models for each outcome. All models control for covariates.
p is the p-value estimated for each model. Given the number of models estimated, the Bonferroni-adjusted p-value (0.001) is recommended to evaluate statistical significance.
TABLE 4.
Moderating roles of coping strategies on the associations between change of perceived stress and change of sleep, mental health, physical health, and overall perceived health longitudinally
| Problem-focussed coping |
Meaning-focussed coping |
Social support |
Acceptance |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | p * | R2/partial correlation | b (SE) | p * | R2/partial correlation | b (SE) | p * | R2/partial correlation | b (SE) | p* | R2/partial correlation | |
| PSQI total score | ||||||||||||
| Perceived stress | 0.16 (0.11) | 0.16 | - | 0.14 (0.11) | 0.19 | - | 0.17 (0.11) | 0.13 | - | 0.13 (0.12) | 0.28 | - |
| Coping | −0.25 (0.37) | 0.51 | - | −0.35 (0.36) | 0.34 | - | −0.49 (0.36) | 0.18 | - | −0.52 (0.72) | 0.47 | - |
| Interaction | −0.03 (0.12) | 0.84 | 0.12/−0.02 | −0.22 (0.14) | 0.13 | 0.14/−0.16 | −0.02 (0.12) | 0.90 | 0.12/−0.02 | 0.03 (0.15) | 0.83 | 0.12/−0.05 |
| CESD total score | ||||||||||||
| Perceived stress | 0.94 (0.15) | <0.001 | - | 1.01 (0.14) | <0.001 | - | 0.93 (0.15) | <0.001 | - | 0.90 (0.15) | <0.001 | - |
| Coping | 0.37 (0.48) | 0.45 | - | −0.66 (0.47) | 0.17 | - | 0.40 (0.47) | 0.39 | - | 0.11 (0.93) | 0.90 | - |
| Interaction | −0.002 (0.15) | 0.99 | 0.34/0.01 | −0.07 (0.18) | 0.71 | 0.35/−0.08 | −0.08 (0.15) | 0.60 | 0.34/−0.07 | −0.29 (0.19) | 0.14 | 0.35 (−0.30) |
| Global mental health (MCS) | ||||||||||||
| Perceived stress | −1.09 (0.24) | <0.001 | - | −1.14 (0.23) | <0.001 | - | −1.09 (0.23) | <0.001 | - | −1.07 (0.24) | <0.001 | - |
| Coping | −0.12 (0.77) | 0.88 | - | 1.16 (0.75) | 0.13 | - | −0.84 (0.70) | 0.23 | - | −0.20 (1.52) | 0.90 | - |
| Interaction | 0.05 (0.25) | 0.85 | 0.20/0.01 | 0.45 (0.29) | 0.13 | 0.23/0.18 | 0.16 (0.23) | 0.50 | 0.26/0.08 | 0.16 (0.32) | 0.62 | 0.20/0.17 |
| Global physical health (PCS) | ||||||||||||
| Perceived stress | 0.04 (0.24) | 0.86 | - | 0.10 (0.24) | 0.69 | - | 0.10 (0.25) | 0.70 | - | 0.11 (0.25) | 0.68 | - |
| Coping | 1.67 (0.78) | 0.03 | - | 1.13 (0.79) | 0.16 | - | 0.95 (0.77) | 0.22 | - | 0.32 (1.56) | 0.84 | - |
| Interaction | −0.07 (0.25) | 0.79 | 0.13/−0.01 | −0.03 (0.31) | 0.93 | 0.11/−0.01 | −0.02 (0.26) | 0.95 | 0.11 (−0.01) | −0.29 (0.32) | 0.38 | 0.10/−0.11 |
| Overall perceived health | ||||||||||||
| Perceived stress | 0.02 (0.02) | 0.31 | - | 0.01 (0.02) | 0.47 | - | 0.02 (0.02) | 0.41 | - | −0.0001 (0.02) | 1.00 | - |
| Coping | −0.18 (0.06) | 0.004 | - | −0.14 (0.06) | 0.03 | - | −0.14 (0.06) | 0.03 | - | −0.13 (0.13) | 0.30 | - |
| Interaction | −0.01 (0.02) | 0.62 | 0.17/−0.06 | −0.004 (0.03) | 0.87 | 0.14/−0.02 | −0.02 (0.02) | 0.34 | 0.15/−0.10 | −0.001 (0.03) | 0.97 | 0.11/−0.07 |
Note: Table represents the final step of the model. Table reports unstandardized coefficients (b) with standard errors (SE) in parentheses. Each block of estimates represents separate models for each outcome. All models control for covariates.
p is the p-value estimated for each model. Given the number of models estimated, the Bonferroni-adjusted p-value (.001) is recommended to evaluate statistical significance.
Acceptance as a coping strategy moderated the cross-sectional relationship between perceived stress during the pandemic and PCS-assessed physical health: higher levels of perceived stress were associated with poorer physical health among those who used acceptance coping an average amount (t = −2.34, p = 0.02) or a greater-than-average amount (1 standard deviation above the mean) (t = −2.69, p = 0.01). However, perceived stress was not associated with physical health among those who less frequently engaged in acceptance coping (1 standard deviation below) (t = −1.14, p = 0.26; see Figure 1a). We further used the Johnson–Neyman technique to probe the interaction and to identify ranges of values of the moderator (acceptance) for which the interaction effect is significant. Figure 2 is the J–N plot of the simple slope of perceived stress on physical health when perceived stress is held at its mean and acceptance is allowed to vary (Figure 1b). The simple slope of perceived stress differed significantly outside the range of −6.17 to −0.18 for acceptance.
FIGURE 1.
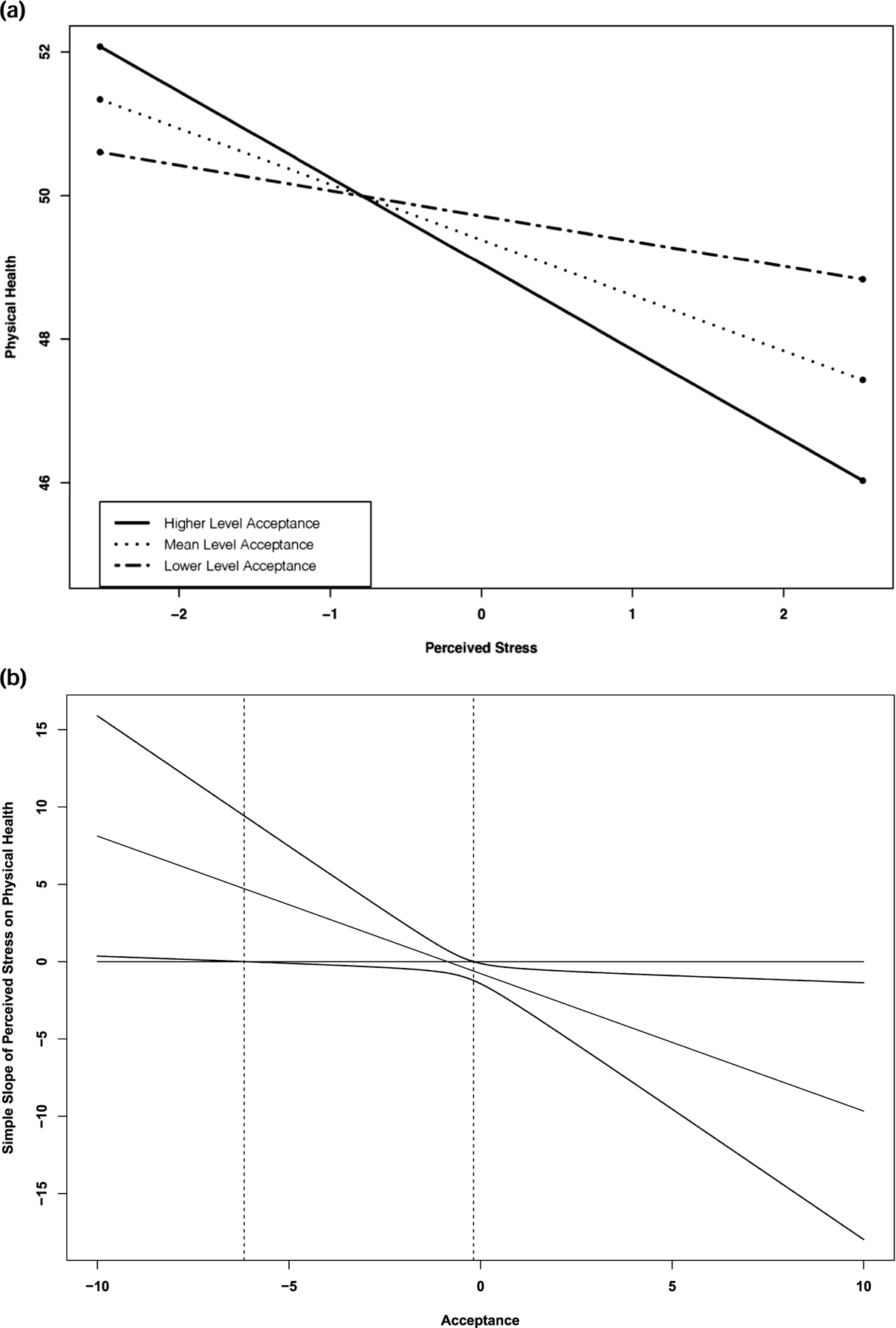
(a) Concurrent relationship between perceived stress and global physical health (PCS) during the pandemic was moderated by acceptance coping. Higher values on the y-axis indicate better physical health. We decomposed data one standard deviation above, below the mean and mean, and tested simple slopes. (b) Johnson–Neyman plot of the simple slope of perceived stress on physical health at the average value (0) of perceived stress across the range of acceptance. Dotted lines represent the 95% of confidence interval
FIGURE 2.
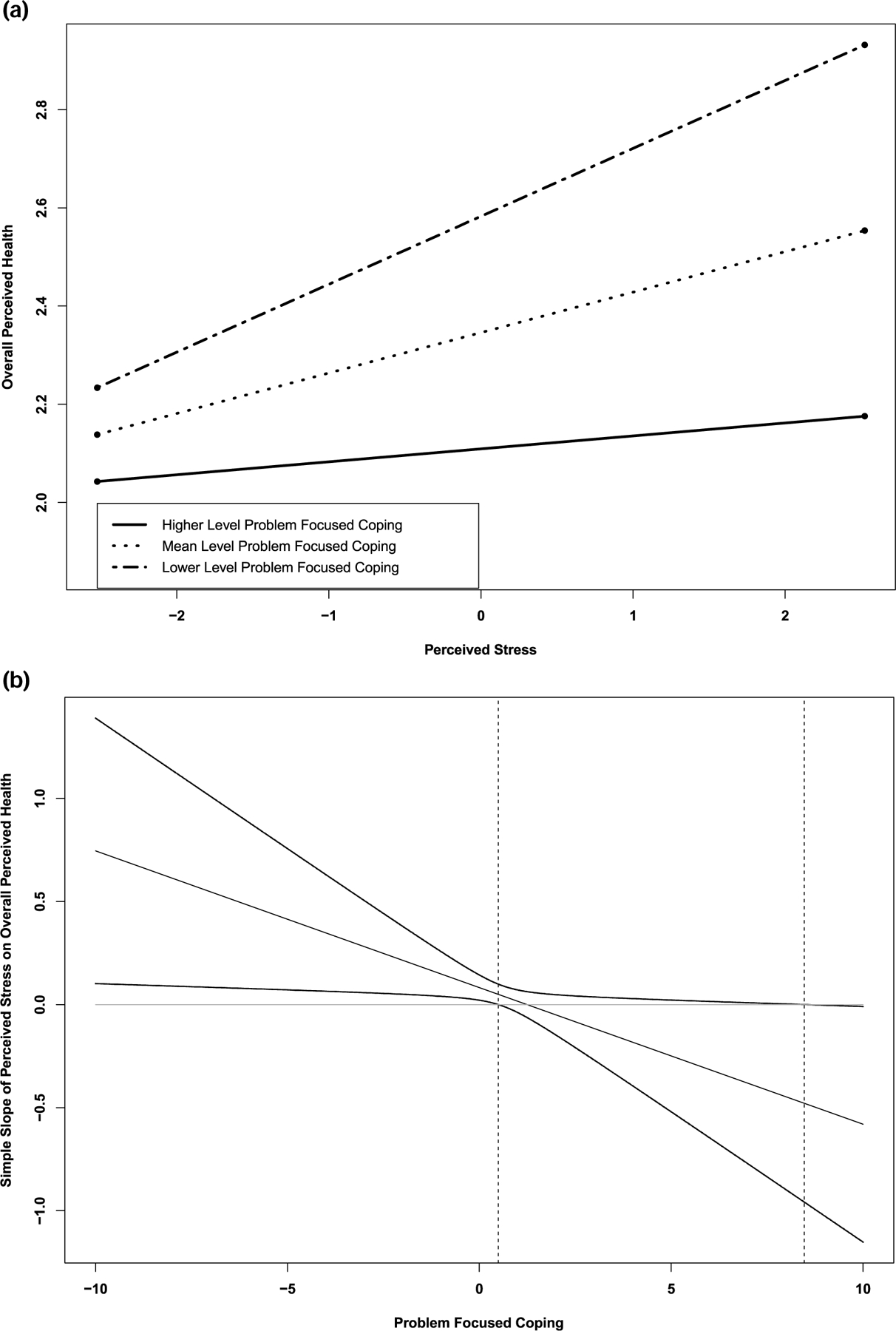
(a) Moderation of relationship between perceived stress and overall perceived health by problem-focussed coping. Higher values on the y-axis indicate poorer overall perceived health. Concurrent relationship between perceived stress and overall perceived health during the pandemic was moderated by problem-focussed coping. We decomposed data one standard deviation above, below the mean and mean, and tested simple slopes. (b) Johnson–Neyman plot of the simple slope of perceived stress on overall perceived health at the average value (0) of perceived stress across the range of problem-focussed coping. Dotted lines represent the 95% of confidence interval
Problem-focussed coping moderated the concurrent association between perceived stress during the pandemic and overall perceived health. That is, higher levels of perceived stress were associated with poorer overall perceived health among those who infrequently used problem-focussed coping infrequently (1 standard deviation below) (t = 2.73, p = 0.007) or with average frequency (t = 2.67, p = 0.009). However, perceived stress was not associated with overall perceived health among those who more frequently engaged in problem-focussed coping (1 standard deviation above) (t = 1.02, p = 0.31) (see Figure 2a). We further used the Johnson–Neyman technique to probe for interaction and to identify ranges of values of the moderator (problem-focussed coping) for which the interaction effect is significant. Figure 2b is the J–N plot of the simple slope of perceived stress on overall perceived health when perceived stress is held at its mean and problem-focussed coping is allowed to vary. The simple slope of perceived stress differs significantly outside the range of 0.50–8.47 for problem-focussed coping.
4 |. DISCUSSION
This study explored associations between perceived stress during the COVID-19 pandemic and indices of sleep, mental, and physical health before and during the pandemic in older adults. We also examined the moderating role of coping on these associations. Consistent with research on the impact of perceived stress on health (Karabulut et al., 2020; Oumohand et al., 2020), the level of stress experienced during the COVID-19 pandemic was associated with poorer sleep and mental health, including prospective decreases in mental health in the context of the pandemic. Furthermore, higher perceived stress was associated with lower mental health, longitudinally. That is, we found both concurrent and longitudinal associations for mental health, but we only found a concurrent association for sleep health. This result may imply that mental health may be more sensitive to a change in perceived stress than sleep health. We did not find any significant associations between perceived stress and global physical and general health. We also identified the four coping strategies older adults used most frequently during the COVID-19 pandemic: problem-focussed coping, meaning-focussing coping, social support, and acceptance. Although we did not find main effects between perceived stress and global physical and general health, coping strategies moderated the association of perceived stress during the pandemic with global physical and general health.
A significant contribution of the present study was to examine associations between perceived stress and sleep, mental health, and global physical and general health by utilizing both concurrent and longitudinal data. As anticipated, the level of stress experienced during the COVID-19 pandemic was associated with poorer sleep and mental health. Overall, these findings are consistent with previous literature in that even though everyone experienced a similar life stressor—the COVID-19 pandemic, in this case—some individuals perceive the stressor to a large extent are likely to experience sleep and mental health problems (Catabay et al., 2019; Eskildsen et al., 2017). Furthermore, there is a growing number of studies to examine health outcomes in the context of the COVID-19 pandemic. For example, consistent with our findings, a study found that higher pandemic-related stress was associated with poorer sleep health such as increased nightly awakenings and increased nightmares (Pesonen et al., 2020). All in all, these results imply that perceived stress has differential impacts on health outcomes, and mental health outcomes are sensitive to both concurrent perceived stress and an increase in perceived stress.
Although we did not find main effects between perceived stress and global physical and general health, moderation findings indicate that coping strategies may affect these relationships.
We found that problem-focussed coping in the context of the COVID-19 pandemic buffered the adverse association between perceived stress and overall perceived general health, consistent with previous studies that have suggested the adaptive nature of problem-focussing coping (e.g., Alok et al., 2014; Stoneman & Gavidia-Payne, 2006). Specifically, this study found that problem-focussed coping strategies (i.e., planning, active coping) protected older adults against the negative effect of perceived stress on general health in the context of COVID-19 pandemic. Others have proposed that older adults who frequently use problem-focussed coping strategies might have higher self-efficacy when coping with the stressful situations (Sharts-Hopco et al., 1996) and higher self-esteem (Mullis & Chapman, 2000). Thus, problem-focussed coping may buffer the effects of stress on health through generation of solutions that remove or dampen stress (Lazarus & Folkman, 1984). As a result, older adults who engage in problem-focussed coping may be less vulnerable to the impact of stress on perceived general health.
Acceptance as a coping strategy seemed to play a rather complicated role in the relationships between perceived stress during the COVID-19 pandemic and health, again consistent with previous mixed findings regarding the effect of acceptance as a coping strategy (e.g., Buckland et al., 2020; Nakamura & Orth, 2005). In some studies acceptance is adaptive because it might facilitate closure on a stressor and moving on in life, enhancing well-being. In contrast, acceptance might require acknowledging the reality of the stressor, so individuals might be preoccupied with thinking about it, which can cause negative well-being (e.g., Buckland et al., 2020; Cook & Hayes, 2010; Nakamura & Orth, 2005). In the present sample, greater use of acceptance as a coping strategy by older adults reporting high levels of perceived stress during the COVID-19 pandemic was associated with poorer global physical health while perceived stress was unrelated to global physical health in older adults who did not typically engage in acceptance coping. In addition, it is important to note that physical health was highest (i.e., good health) for those who had higher acceptance and lower perceived stress, but physical health was lowest for those who had higher acceptance and higher perceived stress. That is, lower, not higher, use of acceptance as a coping strategy during the pandemic seemed to play a protective role in the association between perceived stress and physical health among older adults in the context of the COVID-19 pandemic. Taken together, acceptance may be adaptive for those who have lower perceived stress, but can be maladaptive for those who have higher perceived stress. Future studies should examine the antecedents of acceptance as a coping strategy (e.g., types of stressors, severity of stress, personality) to better characterize the complex associations between perceived stress and health outcomes.
These findings could have useful clinical implications. First, older adults may benefit from interventions targeting stress management and reduction. For example, a study evaluated the efficacy of a resilience building workshop among disaster workers previously exposed to Hurricane Sandy. The study found significantly greater improvements in stress management and fewer incidents of mental health symptoms among individuals who were assigned to the workshop group as compared to those in a waitlist control group (Mahaffey et al., 2021). Determining reasons for perceived stress in the context of the COVID-19 pandemic, evaluating perceived stress levels, and intervening when perceived stress is high may reduce the sleep and mental health risk of older adults. The results of the current study also suggest that older adults may benefit from interventions to improve their problem-focussed coping strategies to reduce the impact of perceived stress on overall perceived general health. Furthermore, identifying people with low problem-focussed coping might be a useful strategy to prevent worsening health in future public health crises.
The results should be interpreted in the context of some limitations. First, we cannot make any causal claims, particularly for cross-sectional associations (e.g., stress with sleep). Although the stress-sleep association is likely bidirectional, chronic stress is prospectively associated with sleep disturbance in midlife women (Hall et al., 2015) and experimentally induced acute stress reduces REM counts (Germain et al., 2003), suggesting that stress can impact sleep. Alternatively, experimental sleep deprivation increases physiological indices of cardiovascular disease risk, including blood pressure, heart rate (Franzen et al., 2011), and cortisol (Minkel et al., 2014). Second, data were solely self-report. Using clinical reports and objective measures of stress, sleep, and mental and physical health may provide additional insights into how threatening and uncontrollable stressors like the COVID-19 pandemic may relate to sleep and health. Third, the sample consisted of older adults who were quite healthy compared to population-based norms (Gandek et al., 1998), and were largely non-Hispanic white, all of which limit the generalizability of our findings. Future studies should attempt to replicate these findings in broader populations because of the documented effects of age and race/ethnicity on sleep, mental, and physical health (e.g., Johnson et al., 2019; Weinstock et al., 2011). Fourth, the current study did not include measures of social isolation and types of stressors participants experience during the COVID-19 pandemic. Understanding social isolation and types of stressors may explain the relationships between perceived stress and health outcomes. Finally, the current study excludes those who engage in regular use of sleep medication at time 1. Therefore, the findings of the current study might not generalize to those who used sleep medications regularly before the COVID-19 pandemic.
In conclusion, during the COVID-19 pandemic, perceived stress in older adults was directly associated with sleep and mental health outcomes. In addition, perceived stress was associated with physical health and perceived general health depended on coping strategies. This study provides a foundation for future research that examines the potential underlying physiological, psychological, and behavioural (e.g., health behaviours, such as exercise and diet) mechanisms of differential effects of perceived stress and coping strategies on each health outcome.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank the study staff and subjects for their gracious participation. The study was not preregistered. This work was supported by NIA program project grant (R01AG047139). Other support was provided by Center for Sleep and Circadian Science and clinical and translational science institute (TR001857). Individual support was provided by T32HL082610 (HML), T32HL007560 (BC), and T32MH019986 (ELT).
Funding information
NIA, Grant/Award Numbers: R01AG047139, T32HL007560, T32HL082610, T32MH019986; Center for Sleep and Circadian Science and clinical and translational science institute, Grant/Award Number: TR001857
Footnotes
CONFLICT OF INTEREST
There is no conflict of interest.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- Alok R, Das SK, Agarwal GG, Tiwari SC, Salwahan L, & Srivastava R (2014). Problem-focused coping and self-efficacy as correlates of quality of life and severity of fibromyalgia in primary fibromyalgia patients. Journal of Clinical Rheumatology: Practical Reports on Rheumatic & Musculoskeletal Diseases, 20, 314–316. [DOI] [PubMed] [Google Scholar]
- Bailey L, Ward M, DiCosimo A, Baunta S, Cunningham C, Romero-Ortuno R, Kenny RA, Purcell R, Lannon R, McCarroll K, Nee R, Robinson D, Lavan A, & Briggs R (2021). Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM: Monthly Journal of the Association of Physicians, 114, 648–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckland NJ, Swinnerton LF, Ng K, Price M, Wilkinson LL, Myers A, & Dalton M (2020). Susceptibility to increased high energy dense sweet and savoury food intake in response to the COVID-19 lockdown: The role of craving control and acceptance coping strategies. Appetite, 158, 105017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- Carver CS (1997). You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4, 92–100. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, & Weintraub JK (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283. [DOI] [PubMed] [Google Scholar]
- Catabay CJ, Stockman JK, Campbell JC, & Tsuyuki K (2019). Perceived stress mental health: The mediating roles of social support and resilience among black women exposed to sexual violence. Journal of Affective Disorders, 259, 143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). COVID-19 death data and resources Retrieved from https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm#AgeAndSex [PubMed]
- Chin B, & Cohen S (2020). Review of the association between number of social roles and cardiovascular disease: Graded or threshold effect? Psychosomatic Medicine, 82, 471–486. [DOI] [PubMed] [Google Scholar]
- Chin B, Murphy ML, & Cohen S (2018). Age moderates the association between social integration and diurnal cortisol measures. Psychoneuroendocrinology, 90, 102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, & Miller GE (2007). Psychological stress and disease. JAMA: Journal of the American Medical Association, 298, 1685–1687. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. [PubMed] [Google Scholar]
- Cohen S, & Williamson G (1988). Perceived stress in a probability sample of the U.S. In Spacapam S & Oskamp S (Eds.), The social psychology of health: Claremont symposium on applied social psychology (pp. 31–67). Sage. [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. [PubMed] [Google Scholar]
- Cole JC, Motivala SJ, Buysse DJ, Oxman MN, Levin MJ, & Irwin MR (2006). Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep (New York, N.Y.), 29(1), 112–116. [DOI] [PubMed] [Google Scholar]
- Cook D, & Hayes SC (2010). Acceptance-based coping and the psychological adjustment of Asian and Caucasian Americans. International Journal of Behavioral Consultation and Therapy, 6, 186–197. [Google Scholar]
- De Pue S, Gillebert C, Dierckx E, Vanderhasselt M-A, De Raedt R, & Van den Bussche E (2021). The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Scientific Reports, 11, 4636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLongis A, & Holtzman S (2005). Coping in context: The role of stress, social support, and personality in coping. Journal of Personality, 73, 1633–1656. [DOI] [PubMed] [Google Scholar]
- Dong E, Du H, & Gardner L (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases, 20, 533–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eskildsen A, Fentz HN, & Andersen LP (2017). Perceived stress, disturbed sleep and cognitive impairments in patients with work-related stress complaints: A longitudinal study. Stress, 20, 371–378. [DOI] [PubMed] [Google Scholar]
- Estes KD, & Thompson RR (2020). Preparing for the aftermath of COVID-19: Shifting risk and downstream health consequences. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S31–S32. [DOI] [PubMed] [Google Scholar]
- Euteneuer F (2014). Subjective social status and health. Current Opinion in Psychiatry, 27(5), 337–343. [DOI] [PubMed] [Google Scholar]
- Fechner-Bates S, Coyne JC, & Schwenk TL (1994). The relationship of self-reported distress to depressive disorders and other psychopathology. Journal of Consulting and Clinical Psychology, 62, 550–559. [DOI] [PubMed] [Google Scholar]
- Folkman S (1984). Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology, 46(4), 839–852. 10.1037/0022-3514.46.4.839 [DOI] [PubMed] [Google Scholar]
- Folkman S (1997). Positive psychological states and coping with severe stress. Social Science & Medicine, 45, 1207–1221. [DOI] [PubMed] [Google Scholar]
- Folkman S (2008). The case for positive emotions in the stress process. Anxiety, Stress & Coping, 21, 3–14. [DOI] [PubMed] [Google Scholar]
- Franzen PL, Gianaros PJ, Marsland AL, Hall MH, Siegle GJ, Dahl RE, & Buysse DJ (2011). Cardiovascular reactivity to acute psychological stress following sleep deprivation. Psychosomatic Medicine, 73, 679–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frese M (1986). Coping as a moderator and mediator between stress at work and psychosomatic complaints. In: Appley MH, Trumbull R (Eds.), Dynamics of stress. The plenum series on stress and coping (pp. 183–206). Springer, [Google Scholar]
- Fuller HR, & Huseth-Zosel A (2021). Lessons in resilience: Initial coping among older adults during the COVID-19 pandemic. The Gerontologist. 61, 114–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, & Sullivan M (1998). Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. International Quality of Life Assessment. Journal of Clinical Epidemiology, 51(11), 1171–1178. [DOI] [PubMed] [Google Scholar]
- Gao C, & Scullin MK (2020). Sleep health early in the coronavirus disease 2019 (COVID-19) outbreak in the United States: Integrating longitudinal, cross-sectional, and retrospective recall data. Sleep Medicine, 73, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain A, Buysse DJ, Ombao H, Kupfer DJ, & Hall M (2003). Psychophysiological reactivity and coping styles influence the effects of acute stress exposure on rapid eye movement sleep. Psychosomatic Medicine, 65, 857–864. [DOI] [PubMed] [Google Scholar]
- Grossman ES, Hoffman YSG, Palgi Y, & Shrira A (2021). COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Personality and Individual Differences, 168, 110371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall MH, Casement MD, Troxel WM, Matthews KA, Bromberger JT, Kravitz HM & Buysse DJ, (2015). Chronic stress is prospectively associated with sleep in midlife women: The SWAN sleep study. Sleep, 38(10), 1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang T-J, Rabheru K, Peisah C, Reichman W, & Ikeda M (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32, 1217–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. Released (2020). IBM SPSS statistics for windows, version 27.0 IBM Corp. [Google Scholar]
- Johnson DA, Jackson CL, Williams NJ, & Alcántara C (2019). Are sleep patterns influenced by race/ethnicity - a marker of relative advantage or disadvantage? Evidence to date. Nature and Science of Sleep, 11, 79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karabulut N, Gürçayır D, Yaman Aktaş Y, Kara A, Kızıloğlu B, Arslan B, & Bölükbaş N (2020). The effect of perceived stress on anxiety and sleep quality among healthcare professionals in intensive care units during the coronavirus pandemic. Psychology Health & Medicine, 26, 119–130. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping Springer. [Google Scholar]
- Lorenzo NE, Zeytinoglu S, Morales S, Listokin J, Almas AN, Degnan KA, Henderson H, Chronis-Tuscano A, & Fox NA (2021). Transactional associations between parent and late adolescent internalizing symptoms during the COVID-19 pandemic: The moderating role of avoidant coping. Journal of Youth and Adolescence, 50, 459–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luanaigh CÓ, & Lawlor BA (2008). Loneliness and the health of older people International Journal of Geriatric Psychiatry, 23, 1213–1221. [DOI] [PubMed] [Google Scholar]
- Mahaffey BL, Mackin DM, Rosen J, Schwartz RM, Taioli E, & Gonzalez A (2021). The disaster worker resiliency training program: A randomized clinical trial. International Archives of Occupational and Environmental Health, 94(1), 9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miilunpalo S, Vuori I, Oja P, Pasanen M, & Urponen H (1997). Self-rated health status as a health measure: The predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. Journal of Clinical Epidemiology, 50, 517–528. [DOI] [PubMed] [Google Scholar]
- Minkel J, Moreta M, Muto J, Htaik O, Jones C, Basner M, & Dinges D (2014). Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychology, 33, 143. [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, & Moos BS (2006). Older adults’ coping with negative life events: Common processes of managing health, interpersonal, and financial/work stressors. International journal of aging & human development, 62, 39–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moro T, & Paoli A (2020). When COVID-19 affects muscle: Effects of quarantine in older adults. European Journal of Translational Myology, 30, 219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullis RL, & Chapman P (2000). Age, gender, and self-esteem differences in adolescent coping styles. The Journal of Social Psychology, 140, 539–541. [DOI] [PubMed] [Google Scholar]
- Nakamura YM, & Orth U (2005). Acceptance as a coping reaction: Adaptive or not? Swiss Journal of Psychology, 64, 281–292. [Google Scholar]
- Ong AD, Uchino BN, & Wethington E (2016). Loneliness and health in older adults: A mini-review and synthesis. Gerontology (Basel), 62, 443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oumohand SE, Ward DD, Boenniger MM, Merten N, Kirschbaum C, & Breteler MMB (2020). Perceived stress but not hair cortisol concentration is related to adult cognitive performance. Psychoneuroendocrinology, 121. 104810. [DOI] [PubMed] [Google Scholar]
- Pearman A, Hughes ML, Smith EL, & Neupert SD (2020). Age differences in risk and resilience factors in COVID-19-related stress. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 76, e38–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesonen A-K, Makela J-M, Halonen R, Elovainio M, Lipsanen J, Antila M, & Sandman N (2020). Pandemic dreams: Network analysis of dream content during the COVID-19 lockdown. Frontiers in Psychology, 11, 573961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Rezaei N, & Grandner MA (2021). Changes in sleep duration, timing, and variability during the COVID-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health, 7, 303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson-Whelen S, Kiecolt-Glaser JK, & Glaser R (2000). Effects of chronic stress on immune function and health in the elderly. In Manuck SB, Jennings R, Rabin BS, Baum A, (Eds.), Behavior, health, and aging (pp. 69–82). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Saalwirth C, & Leipold B (2021). Well-being and sleep in stressful times of the COVID-19 pandemic: Relations to worrying and different coping strategies. Stress and health: journal of the International Society for the Investigation of Stress, 37, 973, 985, 10.1002/smi.3057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnell T, & Krampe H (2020). Meaning in life and self-control buffer stress in times of COVID-19: Moderating and mediating effects with regard to mental distress. Frontiers in Psychiatry, 11, 582352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharts-Hopco NC, Regan-Kubinski MJ, Lincoln PS, & Heverly MA (1996). Problem-focused coping in HIV-infected mothers in relation to self-efficacy, uncertainty, social support, and psychological distress. IMAGE: Journal of Nursing Scholarship, 28, 107–111. [DOI] [PubMed] [Google Scholar]
- Shrira A, Hoffman Y, Bodner E, & Palgi Y (2020). COVID-19-Related loneliness and psychiatric symptoms among older adults: The buffering role of subjective age. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 28, 1200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon Z, Mikulincer M, & Hobfoll SE (1987). Objective versus subjective measurement of stress and social support: Combat-related reactions. Journal of Consulting and Clinical Psychology, 55(4), 577–583. [DOI] [PubMed] [Google Scholar]
- Spira AP, Beaudreau SA, Stone KL, Kezirian EJ, Lui LY, Redline S, Ancoli-Israel S, Ensrud K, Stewart A, & Osteoporotic Fractures in Men Study. (2012). Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 67(4), 433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone KL, & Xiao Q (2018). Impact of poor sleep on physical and mental health in older women. Sleep Medicine Clinics, 13, 457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoneman Z, & Gavidia-Payne S (2006). Marital adjustment in families of young children with disabilities: Associations with daily hassles and problem-focused coping. American Journal on Mental Retardation, 111, 1–14. [DOI] [PubMed] [Google Scholar]
- Ware J Jr, Kosinski M, & Keller SD (1996). A 12-item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220–233. [DOI] [PubMed] [Google Scholar]
- Weinstock RS, Teresi JA, Goland R, Izquierdo R, Palmas W, Eimicke JP, Ebner S, & Shea S (2011). Glycemic control and health disparities in older ethnically diverse underserved adults with Diabetes: Five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabetes Care, 34, 274–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead BR, & Torossian E (2021). Older adults’ experience of the COVID-19 pandemic: A mixed-methods analysis of stresses and joys. The Gerontologist, 61, 36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wuorela M, Lavonius S, Salminen M, Vahlberg T, Viitanen M, & Viikari L (2020). Self-rated health and objective health status as predictors of all-cause mortality among older people: A prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatrics, 20, 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request from the authors.


