Abstract
Objective
This study examined the similarities in metabolic and physiological demands of a fire ground test (FGT) and a live fire training evolution.
Methods
Twenty-seven firefighters completed either a FGT (n = 13) or a live fire training evolution (n = 14). Salivary samples were collected pre, immediately post, and 30-minutes post FGT and live fire training evolution, and analyzed for cortisol, uric acid, and interleukin-1β (IL-1β). Heart rate (HR) was measured pre- and post-task.
Results
Both tasks resulted in significant elevations in cortisol, IL-1β, and HR.
Conclusions
Both the FGT and live fire training evolution appear to result in similar metabolic and physiological demands. Further work may expand upon the additional elements (i.e., added heat) of the live fire training evolution. Fire departments may consider incorporating a variety of high intensity training to prepare personnel for these occupational demands.
Keywords: Cytokines, stress, cortisol, interleukins, cardiovascular disease, fire community
INTRODUCTION
Firefighting can be physically arduous, and exposure to various occupational-specific stressors exacerbates the risk of heart disease mortality (15). In fact, firefighters engaged in active fire suppression are at 10- to 100-times higher risk of heart disease mortality compared to those responding to non-emergency calls (15). Compared to the general population, firefighters experience cardiac events at higher rates (6, 7, 16), and cardiovascular disease (CVD) is documented as the leading cause of premature mortality (~45% and 30% on-duty deaths and overall deaths, respectively) (3, 28). Additional factors such as disturbed sleep patterns, poor dietary habits (e.g., excessive consumption of processed foods, hypercaloric diets, alcohol consumption, excessive caffeine use, lack of dietary fiber), and exposure to products of incomplete combustion and heat can impair occupational performance and further contribute to risk of CVD (8, 33). While CVD is multifactorial, firefighters are exposed to a variety of stressors contributing to cardiovascular strain, inflammation, and oxidative stress, which can lead to the development and progression of CVD (12).
Fire ground performance training and testing are important ways to career firefighter performance, while the candidate physical ability test is typically used during the recruitment process. Occupational-specific evolutions are practiced via simulated activities, such as a live-fire training evolution and/or a fire ground test (FGT), which have been shown to result in acute elevated markers of inflammation and physiological stress (11, 24, 25, 39, 40, 42). Participation in fire-suppressive activities is known to elevate concentrations of interluekin-6 (IL-6) and tumor necrosis factor-α when heat exposure is present (31, 40, 42). Additionally, biomarkers such as cortisol, α-amylase, and interleukin1-β have been shown to be elevated following a live-fire training evolution search and rescue task (39). Heat exposure is a key contributor to the inflammation, physiological stress, and oxidative stress observed during fire suppression activities (40, 41), and places additional strain on the cardiovascular system (5, 14). In fact, the combination of extreme physical exertion and heat exposure during fire suppression activities leads to impaired vascular function, increased thrombus formation, and promotes myocardial ischemia and injury among firefighters (14). Additionally, during active fire suppression, firefighters are dressed in personal protective equipment (PPE) including turnout gear (bunker pants, coat, boots, and hood) and a self-contained breathing apparatus (SCBA). While this gear is intended to protect the firefighter from the dangerous environments encountered, there is a physiological cost as the gear can add an additional ~20–30 kg that can further exacerbate the physiological demands of firefighting (4, 18, 20–22, 32). For training purposes, many fire departments may lack the equipment needed to execute either a FGT or live-fire training evolution. Typically, only one or the other may be regularly performed with respect to individual departments due to equipment or facility limitations.
The various occupational tasks required of structural firefighters may include carrying heavy equipment, advancing dry and charged hose lines, performing forcible entry, carrying or dragging victims (~90 kg), and search and rescue when conducting fire suppression tasks (1). In order to practice such occupational tasks without added heat exposure, a FGT can be administered. The FGT requires firefighters to complete a battery of occupational evolution tasks (i.e., ladder carry, roof ventilation, charged hose drag, search and rescue) as quickly as possible. Although the FGT is predominantly a physical stressor, these simulated assessments activate the hypothalamic pituitary adrenal and sympathoadrenal axes, resulting in elevations in markers of oxidative stress and inflammation (25). In addition, these types of occupational evolutions and tasks may be utilized to determine a candidate’s ‘readiness’ to become a firefighter (10) and may offer additional methods of occupational training to improve the physiological stress response and performance outcomes of fire suppression activities. While the FGT cannot replace live-fire training evolution, it seems plausible that FGT may offer a training method in which firefighters are exposed to similar stressful conditions without the increased risk of heat exposure.
Given the elevated risk of premature mortality due to cardiac events on-duty when engaged in fire suppression tasks, implementing FGT training may offer a safer training method that may be utilized more frequently to practice occupational specific evolutions without the added heat exposure. However, it is not clear if a FGT mimics the demands faced during a live-fire training evolution. Therefore, the purpose of this study was to examine the metabolic and physiological responses between a FGT and a live-fire training evolution among professional firefighters.
METHODS
Participants
A secondary analysis from previous studies was performed on baseline (25) and control data (39) to compare the metabolic and physiological responses to the either a FGT (n = 13) or a live-fire training evolution (n = 14) in which twenty-seven apparently healthy professional, male firefighters from two fire departments (Lakeway, TX and Starkville, MS, respectively) were examined. Briefly, the FGT consisted of nine firefighter-specific tasks that were completed as quickly as possible, which mimicked tasks, movements, and physical demands a firefighter may experience when responding to calls requiring fire suppression activities. The live-fire training evolution consisted of searching for three victims (i.e., 90–100-kg dummies) inside a burning building (255°C) while also attempting to extinguish the controlled burn. It should be noted this live-fire training evolution was part of a routine training that primarily focused on the search and rescue task, and did not include other evolution tasks, such as forcible entry and ventilation. Salivary samples were collected pre, immediately post, and 30-minutes post each task and analyzed for markers of stress, oxidative stress, and inflammation (cortisol, uric acid, interleukin-1β [IL-1β], respectively) to examine the physiological and metabolic demands of the FGT and live-fire conditions. Additionally, heart rate (HR) and SCBA air depletion (PSI) were measured immediately post each task to examine the physiological demands of each the FGT and live-fire conditions. Prior to data collection, participants completed a general health history questionnaire, a physical activity readiness questionnaire, and a medical history questionnaire to assess inclusion and exclusion criteria. Upon enrollment into the study, participants were asked to provide verbal and written informed consent and were brief on all study procedures and assessment protocols. Demographic data for both the FGT and live-fire training evolution group can be viewed in Table 1. This study was carried out in full accordance with the declaration of Helsinki as well as the ethical standards of the International Journal of Exercise Science (26). All experimental produces subsequently described were approved by the Institutional Review Board of Texas State University (IRB#: 6401) as well as the University of North Alabama (IRB#: 064).
Table 1.
Demographic Data (mean ± SD)
| FGT (n = 13) | Live-fire training evolution (n = 14) | |
|---|---|---|
| Age | 36.5 ± 6.9 | 30.0 ± 7.0 |
| Fire Years | 12.3 ± 7.8 | 5.8 ± 3.2 |
| Height (cm) | 178.9 ± 5.9 | 179.7 ± 7.3 |
| Body Mass (kg) | 89.5 ± 12.5 | 92.2 ± 18.9 |
| %Body Fat | 20.1 ± 6.5 | 24.1 ± 8.0 |
Values represent mean ± standard deviation.
Protocol
Each testing session occurred outdoors at the participant’s local fire department training facilities (Lakeway, TX and Starkville, MS). Participants reported to these facilities between 0700 and 0900 and all testing was completed by 1200 following an overnight fast (at least 8 hours). Participants from the Lakeway, TX group were asked to arrive fasted, if possible, but were not required. Before each visit, participants eliminated alcohol consumption for 48 hours, refrained from strenuous exercise not related to their occupation for 24 hours and abstained from caffeine consumption for 24 hours. Participants were fitted with a HR monitor (Team Polar, Polar Electro Inc., Lake Success, NY) and required to dress in full gear (i.e., full turn-out gear and SCBA). Air tanks were filled to 4500-pounds per square inch (PSI) and assessed pre- and post-FGT and the live-fire training evolution from both the cylinder and console gauges. Time-to-complete the assigned duties was recorded. Safety officers were present during all firefighter performance assessment trials. Environmental data for the FGT group can be viewed in Table 2. Note, there are not environmental data reported for the live-fire training evolution group due to the task be conducting in a controlled live-burn setting.
Table 2.
FGT Environmental Conditions
| Temperature (°C) | Humidity (%) | Barometer (in Hg) |
|---|---|---|
| 28.2 ± 3.2 | 64.1 ± 14.7 | 30.0 ± 0.0 |
Values represent mean ± standard deviation.
The FGT consisted of a battery of nine occupational-specific tasks that mimic commonly required tasks used with responding to a fire call. The nine specific tasks were previously described in a published study (25) and completed in the following order: (1), dry hose deployment (61 m), (2) charged hose deployment (23 m), (3) low-room search (24 m), (4) roof walk (12 m), (5) forcible entry task, (6) ladder carry (76 m), (7) stair climb and 12-meter hose hoist, (8) ceiling breach, and (9) victim removal (10 m). Participants were instructed to dress in full gear, which included turn-out gear and SCBA (~20 kg). Additionally, participants were “on air” and had air tanks filled to 4500 (PSI) prior to the start of the FGT from the cylinder and console gauges. Participants were asked to complete the battery of tasks as quickly as possible while avoiding running to mitigate the aerial phase (i.e., body lifted off the ground in order to extend stride length) for standardization. Prior to the experimental trial, one familiarization trial was completed by all participants. A H10 HR monitor (Polar Electro Inc., Bethpage, NY) was fitted across the chest to monitor HR responses and the following timepoints were used for statistical analysis: (1) pre-FGT and (2) immediately post-FGT.
The specific protocol for the live-fire training evolution can been found in a previously published study (39). Firefighters were split into teams of two and were briefed on the evolution (i.e., number of victims to rescue). The three “victims” were 90 to 100 kg dummies placed randomly throughout the building. The participants were required to maneuver through obstacles in order to locate and remove the victims as quickly as possible while maintaining situational awareness and safety. The live burn was controlled and maintained via a pair of gas tanks. The burn house temperature was recorded via an MSA Integrated Thermal Imaging Camera (G1, Cranberry Township, PA), which was collected by the fire training chief. Burn house temperature was recorded as 600 ± 34 °C and 255 ± 21 °C for the ceiling and floor, respectively. The teams worked to suppress the fire and safely rescue the victims from the building. The participants were not allowed to communicate the evolution with other teams that had yet to complete the evolution.
A passive drool saliva collection technique (Salimetrics, PA) was used to collect saliva samples. The participants were instructed to perform a mouth rinse with water 10-minutes prior to the saliva sample collection. It should be noted the mouth rinse was performed for the pre and +30 saliva collections only. During the collection, the participants were instructed to tilt their head forward and allow for the saliva to collect into a polypropylene vial until approximately ~500 μL were collected. Saliva samples were collected for both conditions at the following timepoints: PRE, immediately POST, and +30-POST-task. The saliva samples were transferred immediately onto dry ice and subsequently stored at −80°C for later analysis.
Thawed saliva samples were centrifuged at 4°C for 15-minutes at 1,500 rpm. Samples were then analyzed in duplicate for concentrations of cortisol, uric acid, IL-1β using commercially available kits (Salimetrics, PA). Absorbance was determined via a BioTek plate reader (Winooski, VT). The intra- and inter-assay coefficients of variation (CV) were < 10% for all assays.
Statistical Analysis
Statistical procedures were conducted with SPSS (version 26; IBM, Chicago, IL). All data are presented as the mean ± SD. The α level was set at p ≤ 0.05. Data were checked for normality and homogeneity. A 2 × 3 (condition [FGT vs. live-fire training evolution] × time [PRE, POST, +30-POST]) two-way mixed model repeated measures analysis of variance (RMANOVA) was used to analyze salivary concentrations of cortisol, uric acid, IL-1β. In terms of HR, a 2 × 2 (condition [FGT vs. live-fire training evolution] × time [PRE and POST]) two-way ANOVA was used. If significant main effects or interaction effects were observed, post hoc testing was performed with Bonferroni’s correction, with multiplicity-adjusted p values applied to compare the dependent variables at their respective time points. Air utilization was calculated (PSI pre-task – PSI post-task) from both the air cylinder gauge and the console gauge located on the shoulder strap. In terms of air utilization (in units of PSI depletion), an independent t test was performed to compare calculated depletion values between conditions. Effect sizes were calculated and reported as partial eta-squared where significance occurred (ηp2: < 0.01 = small effect; 0.09 – 0.25 = moderate effect; 0.25 = large effect).
RESULTS
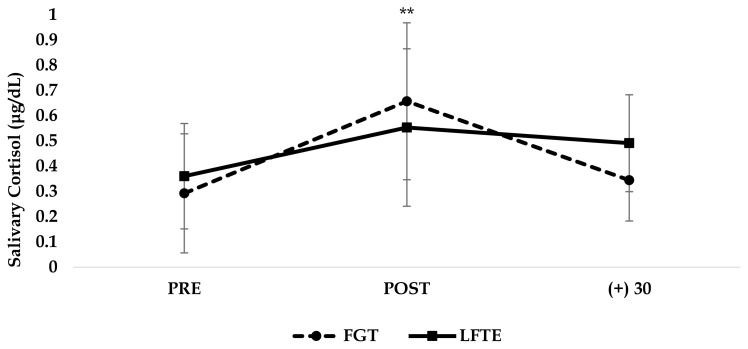
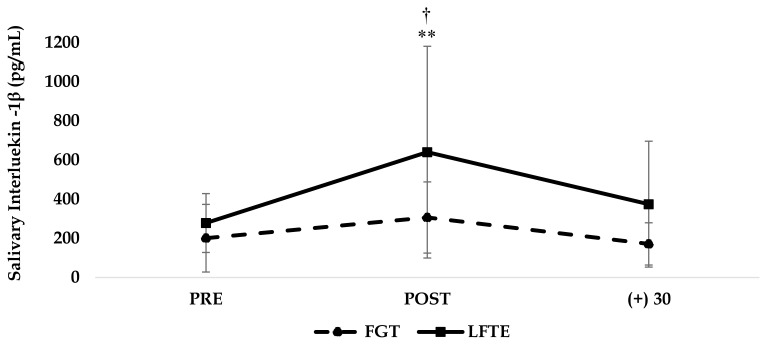
Regarding salivary cortisol concentrations, there were no significant interactions or main effects for condition (both p > 0.05); however, a significant time effect was found (F = 7.68, p = 0.001, ηp2 = 0.19). Cortisol concentrations were significantly higher among both conditions immediately POST compared to PRE (p < 0.001). Data for salivary cortisol can be found in Figure 1. Regarding uric acid concentrations, no significant interactions, main effects, or time effects were found (all p > 0.05). Data for salivary cortisol and uric acid can be found in Table 3. With respect to IL-1β, no significant condition × time interaction was found (p > 0.05); however, a significant time effect (F = 3.94, p = 0.02, ηp2 = 0.11) and a significant main effect for condition (F = 8.03, p < 0.01, ηp2 = 0.11) were found such that both groups experienced a significant increase in IL-1β immediately POST and the live-fire training evolution group overall demonstrated higher IL-1β concentrations. Data for salivary IL-1β can be found in Figure 2.
Figure 1.
Values represent mean ± standard deviation. FGT = Fire grounds test; LFTE = Live-fire training evolution.
**Denotes significantly higher salivary cortisol concentration (p ≤ 0.01) immediately-post task compared to baseline.
Table 3.
Heart Rate & PSI
| FGT (n = 13) | Live-fire training evolution (n = 14) | |
|---|---|---|
| Pre-Task HR (bpm) | 89 ± 12 | 82 ± 13 |
| Post-Task HR (bpm) | 178 ± 4* | 178 ± 19* |
| Cylinder Gauge Difference (PSI) | 2,346.2 ± 275.7 | 3,335.7 ± 486.8** |
| Console Gauge Difference (PSI) | 2,176.9 ± 404.5 | 3,382.5 ± 588.1** |
Values represent mean ± standard deviation. FGT = fire grounds test; HR = heart rate; PSI = pounds per square inch.
Denotes significantly higher (p ≤ 0.01) heart rate values compared to baseline.
Denotes significantly lower PSI depletion (p ≤ 0.01) for both the cylinder and console gauge between tasks.
Figure 2.
Values represent mean ± standard deviation. FGT = Fire grounds test; LFTE = Live-fire training evolution.
**Denotes significantly higher IL-1β concentration (p ≤ 0.01) immediately-post task compared to baseline. †Denotes overall higher IL-1β concentration for the live-fire training evolution group.
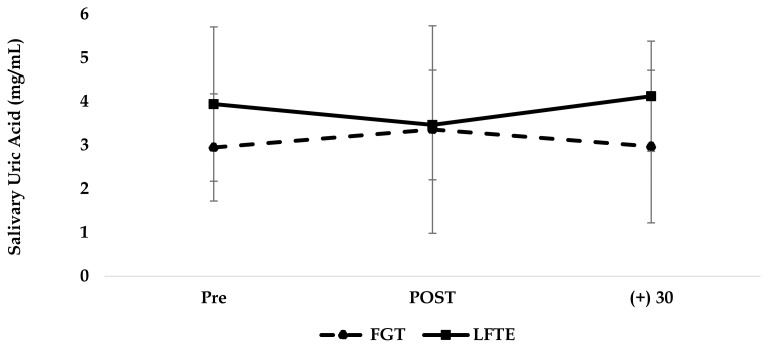
Figure 3.
Values represent mean ± standard deviation. FGT = Fire grounds test; LFTE = Live-fire training evolution.
No significant condition × time interaction or main effect were noted for HR (p > 0.05). However, there was a significant time effect (F = 631.873, p < 0.001, ηp2 = 0.927). Post hoc analysis found HR was significantly elevated for both conditions immediately POST (p < 0.001, FGT = 178 ± 4, live-fire training evolution = 177 ± 19). Regarding air depletion, there were significant differences in air utilization noted for the live-fire training evolution group compared to the FGT group when PSI was measured from the cylinder gauge (p < 0.001) as well as from the console gauge (p < 0.001). Air PSI depletion measured on the cylinder gauge was ~52% and ~74% for the FGT and live-fire training evolution groups, respectively. Air PSI depletion measured on the console gauge was ~48% and ~75% for the FGT and live-fire training evolution groups, respectively. Data for HR and air utilization can be found in Table 3.
DISCUSSION
The aim of the present study was to examine the metabolic and physiological responses between a FGT and a live-fire training evolution among professional firefighters. Both FGT and live-fire training evolution resulted in significant elevations in IL-1β, cortisol, and HR that were not different between the conditions. These findings suggest the FGT, and live-fire training evolution tasks may result in similar pro-inflammatory and metabolic demands.
Both conditions resulted in significant increases in salivary cortisol concentrations, as well as HR immediately POST compared to the PRE. Salivary cortisol is commonly measured as an indicator of acute and chronic stress responses (9, 27) and several studies have assessed salivary cortisol following firefighter specific tasks, such as the FGT or fire suppression (25, 27, 42, 43). Exposure to these stressors activate the hypothalamic-pituitary-adrenal axis and subsequently cause the release of cortisol (35). Cortisol then confers an anti-inflammatory effect by providing feedback to suppress the release of pro-inflammatory cytokines (29, 37). However, under severe or chronic stressful conditions (e.g., fire suppressive conditions), prolonged activation of the hypothalamic-pituitary-adrenal axis results in excessive cortisol release (2, 30). Routine exposure to occupational stressors can chronically activate the hypothalamic-pituitary-adrenal axis and result in elevations in chronic elevations of low-grade inflammation that facilitates CVD (12). Additionally, this low-grade inflammation is further exacerbated with minimal time between frequent and repeated response calls. In terms of HR, the FGT and live-fire training evolution conditions yielded HR values of ~97% and 94% HRmax. Past work has shown structural firefighting routinely results in HRmax values between 84% to 100% (17, 34). It is plausible that both FGT and live-fire training evolution tasks both mimic the high metabolic demands of firefighting and departments can benefit from routinely practicing these types of scenarios, or at least introduce physical training methods to prepare the operator for high intensity on-duty demands of the occupation. It should also be noted that the air tanks contained 4500 PSI of air prior to each task. These tanks are designed to provide air for up to 45 minutes; however, they were largely depleted (> 50%) in only ~10-minutes following completion of these tasks, which underscores the metabolic demand of firefighting.
Firefighting is known to result in elevations in inflammatory markers, such as interleukin – 6, C-reactive protein, and IL-1β (25, 40, 42, 43). Recent reviews have highlighted IL-1β as a potential target for treatment of atherosclerosis given the role in which this specific cytokine plays in acute and chronic inflammation, as well as in all stages of atherosclerosis (19, 23). It is well established that cytokines, such as IL-1β, demonstrate pro-inflammatory activity, which may be induced via acute exercise and exposure to stressful conditions. While acute exposure to these pro-inflammatory cytokines may provide a favorable effect, chronic exposure to inflammation plays a critical role in the development and progression of CVD (19, 36, 38). Although previous work may suggest added environmental heat results in a greater pro-inflammatory response (12, 13), our present study noted similar significantly elevated pro-inflammatory responses to both conditions. Interestingly, the IL-1β concentrations were approximately 2× greater immediately POST-live-fire training evolution task compared to the immediately POST-FGT IL-1β concentrations (~150% that of the FGT). However, this main effect for the condition is likely attributed to already elevated IL-1β concentration noted at baseline, which remained consistent throughout (PRE and POST live-fire training evolution). While it seems plausible that the mental challenge of having to search for a victim, in addition to the added heat exposure, could result in greater metabolic demands and stress responses, the present study suggests that the FGT and live-fire training evolution resulted in similar demands. However, larger scale studies are needed to further confirm or challenge these findings. This is an important finding for fire departments utilizing FGT-like assessments for candidacy, as those tasks appear to match metabolic demand and stress noted from live-fire training evolution.
There are some limitations within the present study that should be addressed. First, this study compared responses to separate firefighting tasks/conditions between participants. Further research should assess the responses for the same subject completing both conditions in a randomized order. Although the present study was unable to compare responses for the same participants for both conditions, these finding provide preliminary insight to the potential similarities in terms of the physiological and stress responses to fire-suppressive activities. Additionally, there are a variety of occupational stressors that may influences the physiological stress and inflammatory responses measured, which are difficult to account for and control when studying this occupation. However, it would be important to note any response calls experiences within an acute window prior to the testing sessions as these responses can impact the markers measured. Second, time was not equated per the two conditions (FGT = 8.05 minutes, live-fire training evolution = 10.60 minutes). However, it should also be noted that that the live-fire training evolution is inherently not a time-trial assessment and time is generally recognized as an outcome variable for this specific assessment. It was not possible under these conditions to equate time and total work with these tasks. Further research may explore comparisons of the FGT and live-fire training evolution tasks with time equated. Lastly, the collection window per the salivary markers is relatively short in duration, and further research should expand beyond the 30-minutes post-task collection window to assess the stress and inflammatory response trajectory.
Firefighting is an extremely physiologically and psychological demanding occupation, and the numerous stressors (i.e., environmental toxins, smoke exposure, added heat, and extreme physical exertion) further exacerbate the stress and inflammatory response to occupation-specific tasks. Repeated and chronic exposure to such conditions results in elevations in inflammatory, oxidative stress, and physiological stress biomarkers that contribute to the increased risk of cardiovascular disease. The present findings highlight the intense metabolic and physiological stress demands of various occupation-specific tasks, and it appears that the FGT and live-fire training evolution tasks can result in similar metabolic stress and pro-inflammatory responses. Additional research involving larger scale, crossover design studies are needed to explore if elements such as added heat and mental challenges of the live-fire training evolution can result in greater inflammatory responses and physiological demand compared to the FGT as well as if the FGT may be an ideal frequent training method used to practice fire-suppressive activities when equipment and access to live-burn conditions are limited. While both tasks are important in preparing firefighters for the extreme conditions faced on-duty, fire departments may want to consider introducing a wider variety of high intensity training methods to prepare their personnel to handle these demands.
ACKNOWLEDGEMENTS
The authors would like to thank the members of the local Lake Travis, Texas and the Starkville, Mississippi Fire Departments for their involvement in the study.
REFERENCES
- 1.Abel MG, Palmer TG, Trubee N. Exercise program design for structural firefighters. Strength & Conditioning Journal. 2015;37(4):8–19. [Google Scholar]
- 2.Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proceedings of the National Academy of Sciences. 2012;109(16):5995–5999. doi: 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dobson M, Choi B, Schnall PL, Wigger E, Garcia-Rivas J, Israel L, Baker DB. Exploring occupational and health behavioral causes of firefighter obesity: a qualitative study. American Journal of Industrial Medicine. 2013;56(7):776–790. doi: 10.1002/ajim.22151. [DOI] [PubMed] [Google Scholar]
- 4.Eves ND, Jones RL, Petersen SR. The influence of the self-contained breathing apparatus (SCBA) on ventilatory function and maximal exercise. Can J Appl Physiol. 2005;30(5):507–519. doi: 10.1139/h05-137. [DOI] [PubMed] [Google Scholar]
- 5.Fahs CA, Yan H, Ranadive S, Rossow LM, Agiovlasitis S, Echols G, Smith D, Horn GP, Rowland T, Lane A. Acute effects of firefighting on arterial stiffness and blood flow. Vascular medicine. 2011;16(2):113–118. doi: 10.1177/1358863X11404940. [DOI] [PubMed] [Google Scholar]
- 6.Fahy RF. US firefighter fatalities due to sudden cardiac death, 1995 –2004. National Fire Protection Association Quincy; MA: 2005. [PubMed] [Google Scholar]
- 7.Fahy RF, Petrillo JT, Molis JL. Firefighter fatalities in the US-2019. National fire protection association; 2020. pp. 1–26. [PubMed] [Google Scholar]
- 8.Gonzalez DE, McAllister MJ, Waldman HS, Ferrando AA, Joyce J, Barringer ND, Dawes JJ, Kieffer AJ, Harvey T, Kerksick CM, Stout JR, Ziegenfuss TN, Zapp A, Tartar JL, Heileson JL, VanDusseldorp TA, Kalman DS, Campbell BI, Antonio J, Kreider RB. International society of sports nutrition position stand: tactical athlete nutrition. Journal of the International Society of Sports Nutrition. 2022;19(1):267–315. doi: 10.1080/15502783.2022.2086017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hellhammer DH, Wüst S, Kudielka BM. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology. 2009;34(2):163–171. doi: 10.1016/j.psyneuen.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 10.Hollerbach BS, Jahnke SA, Poston WSC, Harms CA, Heinrich KM. Examining a novel firefighter exercise training program on simulated fire ground test performance, cardiorespiratory endurance, and strength: a pilot investigation. Journal of Occupational Medicine and Toxicology. 2019;14(1):12. doi: 10.1186/s12995-019-0232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horn GP, Kesler RM, Motl RW, Hsiao-Wecksler ET, Klaren RE, Ensari I, Petrucci MN, Fernhall B, Rosengren KS. Physiological responses to simulated firefighter exercise protocols in varying environments. Ergonomics. 2015;58(6):1012–1021. doi: 10.1080/00140139.2014.997806. [DOI] [PubMed] [Google Scholar]
- 12.Huang C-J, Webb H, Zourdos M, Acevedo E. Cardiovascular reactivity, stress, and physical activity. Frontiers in Physiology. 2013;4(314) doi: 10.3389/fphys.2013.00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang CJ, Webb HE, Garten RS, Kamimori GH, Evans RK, Acevedo EO. Stress hormones and immunological responses to a dual challenge in professional firefighters. Int J Psychophysiol. 2010;75(3):312–318. doi: 10.1016/j.ijpsycho.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Hunter AL, Shah ASV, Langrish JP, Raftis JB, Lucking AJ, Brittan M, Venkatasubramanian S, Stables CL, Stelzle D, Marshall J, Graveling R, Flapan AD, Newby DE, Mills NL. Fire simulation and cardiovascular health in firefighters. Circulation. 2017;135(14):1284–1295. doi: 10.1161/CIRCULATIONAHA.116.025711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. N Engl J Med. 2007;356(12):1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- 16.Kales SN, Soteriades ES, Christoudias SG, Christiani DC. Firefighters and on-duty deaths from coronary heart disease: a case control study. Environmental Health. 2003;2(1):1–13. doi: 10.1186/1476-069X-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lemon P, Hermiston RT. The human energy cost of fire fighting. Journal of Occupational Medicine. 1977:558–562. [PubMed] [Google Scholar]
- 18.Lesniak AY, Bergstrom HC, Clasey JL, Stromberg AJ, Abel MG. The effect of personal protective equipment on firefighter occupational performance. J Strength Cond Res. 2020;34(8):2165–2172. doi: 10.1519/JSC.0000000000003384. [DOI] [PubMed] [Google Scholar]
- 19.Libby P. Interleukin-1 beta as a target for atherosclerosis therapy: biological basis of CANTOS and beyond. J Am Coll Cardiol. 2017;70(18):2278–2289. doi: 10.1016/j.jacc.2017.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Louhevaara V, Smolander J, Tuomi T, Korhonen O, Jaakkola J. Effects of an SCBA on breathing pattern, gas exchange, and heart rate during exercise. Journal of occupational medicine: official publication of the Industrial Medical Association. 1985;27(3):213–216. [PubMed] [Google Scholar]
- 21.Louhevaara V, Tuomi T, Korhonen O, Jaakkola J. Cardiorespiratory effects of respiratory protective devices during exercise in well-trained men. European journal of applied physiology and occupational physiology. 1984;52(3):340–345. doi: 10.1007/BF01015224. [DOI] [PubMed] [Google Scholar]
- 22.Louhevaara V, Tuomi T, Smolander J, Korhonen O, Tossavainen A, Jaakkola J. Cardiorespiratory strain in jobs that require respiratory protection. International Archives of Occupational and Environmental Health. 1985;55(3):195–206. doi: 10.1007/BF00383753. [DOI] [PubMed] [Google Scholar]
- 23.Mai W, Liao Y. Targeting IL-1β in the treatment of atherosclerosis. Front Immunol. 2020;11:589654–589654. doi: 10.3389/fimmu.2020.589654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McAllister MJ, Basham SA, Smith JW, Waldman HS, Krings BM, Mettler JA, Butawan MB, Bloomer RJ. Effects of environmental heat and antioxidant ingestion on blood markers of oxidative stress in professional firefighters performing structural fire exercises. J Occup Environ Med. 2018;60(11):e595–e601. doi: 10.1097/JOM.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 25.McAllister MJ, Gonzalez AE, Waldman HS. Time restricted feeding reduces inflammation and cortisol response to a firegrounds test in professional firefighters. J Occup Environ Med. 2021;63(5):441–447. doi: 10.1097/JOM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 26.Navalta JW, Stone WJ, Lyons S. Ethical issues relating to scientific discovery in exercise science. International journal of exercise science. 2019;12(1):1. [PMC free article] [PubMed] [Google Scholar]
- 27.Perroni F, Tessitore A, Cibelli G, Lupo C, D'Artibale E, Cortis C, Cignitti L, De Rosas M, Capranica L. Effects of simulated firefighting on the responses of salivary cortisol, alpha-amylase and psychological variables. Ergonomics. 2009;52(4):484–491. doi: 10.1080/00140130802707873. [DOI] [PubMed] [Google Scholar]
- 28.Poston WS, Haddock CK, Jahnke SA, Jitnarin N, Tuley BC, Kales SN. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. Journal of occupational and environmental medicine. 2011;53(3):266. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reichlin S. Neuroendocrine-immune interactions. New England Journal of Medicine. 1993;329(17):1246–1253. doi: 10.1056/NEJM199310213291708. [DOI] [PubMed] [Google Scholar]
- 30.Silverman MN, Sternberg EM. Glucocorticoid regulation of inflammation and its functional correlates: from HPA axis to glucocorticoid receptor dysfunction. Annals of the New York Academy of Sciences. 2012;1261(1):55–63. doi: 10.1111/j.1749-6632.2012.06633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith DL, Friedman NMG, Bloom SI, Armero WL, Pence BD, Cook MD, Fernhall B, Horn GP, Woods J. Firefighting induces acute inflammatory responses that are not relieved by aspirin in older firefighters. J Occup Environ Med. 2019;61(7):617–622. doi: 10.1097/JOM.0000000000001626. [DOI] [PubMed] [Google Scholar]
- 32.Smolander J, Louhevaara V, Tuomi T, Korhonen O, Jaakkola J. Cardiorespiratory and thermal effects of wearing gas protective clothing. Int Arch Occup Environ Health. 1984;54(3):261–270. doi: 10.1007/BF00379055. [DOI] [PubMed] [Google Scholar]
- 33.Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters: a systematic review. Cardiol Rev. 2011;19(4):202–215. doi: 10.1097/CRD.0b013e318215c105. [DOI] [PubMed] [Google Scholar]
- 34.Sothmann MS, Saupe K, Jasenof D, Blaney J. Heart rate response of firefighters to actual emergencies: Implications for cardiorespiratory fitness. Journal of Occupational Medicine. 1992:797–800. doi: 10.1097/00043764-199208000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Steensberg A, Fischer CP, Keller C, Møller K, Pedersen BK. Il-6 enhances plasma IL-1ra, IL-10, and cortisol in humans. American Journal of Physiology-Endocrinology And Metabolism. 2003;285(2):e433–E437. doi: 10.1152/ajpendo.00074.2003. [DOI] [PubMed] [Google Scholar]
- 36.Szekely Y, Arbel Y. A review of interleukin-1 in heart disease: where do we stand today? Cardiol Ther. 2018;7(1):25–44. doi: 10.1007/s40119-018-0104-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turnbull AV, Rivier CL. Regulation of the hypothalamic-pituitary-adrenal axis by cytokines: actions and mechanisms of action. Physiological reviews. 1999 doi: 10.1152/physrev.1999.79.1.1. [DOI] [PubMed] [Google Scholar]
- 38.Van Tassell BW, Raleigh JMV, Abbate A. Targeting interleukin-1 in heart failure and inflammatory heart disease. Current heart failure reports. 2015;12(1):33–41. doi: 10.1007/s11897-014-0231-7. [DOI] [PubMed] [Google Scholar]
- 39.Waldman HS, Bryant AR, Shepherd BD, Egan B, McAllister MJ. No effect of a ketone monoester on markers of stress and performance in a live-burn search and rescue in firefighters. J Strength Cond Res. 2022;36(3):763–771. doi: 10.1519/JSC.0000000000004194. [DOI] [PubMed] [Google Scholar]
- 40.Walker A, Keene T, Argus C, Driller M, Guy JH, Rattray B. Immune and inflammatory responses of Australian firefighters after repeated exposures to the heat. Ergonomics. 2015;58(12):2032–2039. doi: 10.1080/00140139.2015.1051596. [DOI] [PubMed] [Google Scholar]
- 41.Walker BR. Glucocorticoids and cardiovascular disease. Eur J Endocrinol. 2007;157(5):545–559. doi: 10.1530/EJE-07-0455. [DOI] [PubMed] [Google Scholar]
- 42.Wolkow A, Aisbett B, Jefferies S, Main LC. Effect of heat exposure and simulated physical firefighting work on acute inflammatory and cortisol responses. Ann Work Expo Health. 2017;61(5):600–603. doi: 10.1093/annweh/wxx029. [DOI] [PubMed] [Google Scholar]
- 43.Wolkow A, Aisbett B, Reynolds J, Ferguson SA, Main LC. The impact of sleep restriction while performing simulated physical firefighting work on cortisol and heart rate responses. International archives of occupational and environmental health. 2016;89(3):461–475. doi: 10.1007/s00420-015-1085-3. [DOI] [PubMed] [Google Scholar]