Abstract
Purpose of Review
A significant proportion of patients evaluated for chest pain have ischemia with non-obstructive coronary artery disease (INOCA). Studies have shown INOCA is associated with increased risk of major adverse cardiac events and significant burden on the health care system.
Recent Findings
While there is scarce scientific evidence on management of INOCA, the CorMicA trial showed that stratified medical therapy based on the type of INOCA improved patients’ symptoms and quality of life. There are multiple ongoing trials, including Women’s IschemiA Trial to Reduce Events in Non-ObstRuctIve CORonary Artery Disease (WARRIOR trial), assessing the benefit of intensive medical therapy versus usual care for this increasingly recognized clinical entity.
Summary
In this review, we discuss the definition of INOCA, epidemiology and risk factors, pathophysiology, and management as well as the current knowledge gaps and ongoing clinical trials in this arena.
Keywords: Ischemia with non-obstructive coronary arteries, Ischemia, Angina, Microvascular dysfunction, Vasospastic angina
Introduction
Coronary artery disease (CAD) remains the leading cause of mortality and morbidity in both men and women in the USA and worldwide [1]. Classically, CAD has been linked with obstructive atherosclerotic plaques resulting in flow-limiting stenotic lesions in one or more epicardial coronary arteries [1, 2]. Recently, there has been growing interest in the entity of non-obstructive CAD, also known as “open artery ischemia,” in which a patient presents with symptoms and/or signs of myocardial ischemia but the epicardial coronary artery shows < 50% diameter stenosis [2, 3]. These patients might have subtle chronic presentation with chronic stable angina, or non-specific symptoms with objective evidence of myocardial ischemia. These patients may be classified under the definition of “ischemia with non-obstructive coronary arteries (INOCA).” This syndrome is often a direct result of demand–supply mismatch leading to inadequate myocardial perfusion secondary to limitations of the microvasculature [2, 3]. Although previously viewed as “benign,” there is accumulating evidence indicating that INOCA is associated with poor quality of life, significant burden on the health care system, and major adverse cardiac events (MACE), including acute coronary syndrome, heart failure hospitalization, stroke, and repeat cardiovascular procedures [2–4]. In this review, we discuss the definition of INOCA, epidemiology, risk factors, and management as well as knowledge gaps and ongoing clinical trials.
Definition of INOCA
The Cardiovascular Disease in Women Committee of the American College of Cardiology, in conjunction with interested parties (from the National Heart, Lung, and Blood Institute, American Heart Association, and European Society of Cardiology), convened a working group to develop a consensus on the syndrome of myocardial ischemia with no obstructive coronary arteries (INOCA) [4]. In that scientific statement, INOCA was defined as follows: (1) stable chronic (several weeks or longer) symptoms suggesting ischemic heart disease such as chest discomfort with both classic (angina pectoris) and non-classical features in terms of location, quality, and inciting factors; (2) objective evidence for myocardial ischemia from the electrocardiography (ECG) or cardiac imaging (echocardiography, nuclear imaging, magnetic resonance imaging, or spectroscopy) at rest or during stress (exercise, mental, or pharmacological); and (3) absence of flow-limiting obstruction by coronary angiography (invasive or computed tomographic angiography) as defined by any epicardial coronary artery diameter reduction ≥ 50% or fractional flow reserve ≤ 0.8 [4].
Similarly, INOCA was defined by a consensus statement from the European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation, which was also endorsed by the Coronary Vasomotor Disorders International Study (COVADIS) group, as a demand–supply mismatch of coronary artery blood flow leading to transient or recurrent cardiac chest pain related to myocardial ischemia [5•]. The mismatch between blood supply and myocardial oxygen demand may be caused by coronary microvascular dysfunction (CMD) and/or epicardial coronary artery spasm, typically in the setting of non-obstructive coronary atherosclerosis. The working group provided diagnostic criteria for microvascular angina to include the all the following: (1) symptoms of myocardial ischemia, (2) absence of obstructive CAD (< 50% diameter reduction or FFR > 0.80), (3) objective evidence of myocardial ischemia whether on electrocardiography or stress testing, and (4) evidence of impaired coronary microvascular function [5•] (Table 1).
Table 1.
Summary of criteria for diagnosis of INOCA
| Criteria | Description |
|---|---|
|
1) Symptoms of myocardial ischemia |
Whether it is angina or non-classical symptoms, usually chronic symptoms for several weeks or longer |
|
2) Absence of obstructive CAD |
< 50% diameter reduction or fractional flow reserve > 0.80 |
|
3) Objective evidence of myocardial ischemia |
Whether on electrocardiography or cardiac imaging, including echocardiography, nuclear imaging, magnetic resonance imaging, or spectroscopy |
|
4) Evidence of impaired coronary microvascular function |
Coronary flow reserve measured invasively or non-invasively, intra-vascular resistance and acetylcholine response measured invasively |
Although the INOCA definition is generally reserved for patients who have documented objective ischemia, it is important to note that we do not have adequate testing to assure the absence of myocardial ischemia among patients with coronary microvascular dysfunction [2, 3]. At the present time, cardiac positron emission tomography and magnetic resonance perfusion imaging modalities appear to be the best options, but they are limited by their spatial resolution. Recent angiographic techniques with computational fluid dynamic evaluation to assess absolute coronary flow and coronary microvascular resistance using data from routine invasive coronary angiography may be more accurate; however, the clinical benefit of these techniques needs to be evaluated in future studies [6].
Epidemiology and Risk Factors
INOCA is relatively common among patients presenting with ischemic chest pain [2–4]. Approximately 3 to 4 million women and men with signs/symptoms suggestive of myocardial ischemia have non-obstructive CAD in the USA [4]. In an analysis from the National Cardiovascular Data Registry Cath-PCI Registry of 661,063 patients without history of CAD undergoing elective coronary angiography, the majority (58.4%) had evidence of non-obstructive CAD [7]. Studies have shown that approximately 60% of women and 30% of men who present with angina have non-obstructive lesions [8, 9]. Studies have also shown that INOCA patients tend to be younger, are likely women, and have non-classical presentation and low risk non-invasive test findings [7–9]. Furthermore, INOCA patients usually have lower prevalence of the traditional cardiovascular risk factors such as diabetes mellitus compared with patients with obstructive CAD [2, 3]. However, it is important to note that the presence of comorbidities, such as diabetes mellitus and hypertension, has long been linked with CMD which is associated with some of the detrimental effects observed in both structural and functional CMD [2, 3].
Pathophysiology
The underlying mechanisms involved in the pathophysiology for INOCA are multifactorial [10–12]. However, CMD remains a central component in the pathophysiology of INOCA. CMD may be broadly classified into 2 endotypes: structural CMD and functional CMD [10]. Structural CMD is characterized by reduced microvascular conductance and impaired oxygen delivering capacity to the myocardium. The decreased microvascular conductance is a result of inward remodeling of small-sized coronary arterioles, while the impaired oxygen delivering capacity to the myocardium is a product of myocardial capillary rarefaction or low coronary microvascular density [10]. Both inward remodeling of small-sized coronary arterioles and myocardial capillary rarefaction are commonly seen in structural CMD. Microvascular spasm is an example of structural CMD, in which dysfunctional vessels appear to be hypersensitive to acetylcholine and other vasoconstrictors. As with epicardial coronary spasm, microvascular spasm occurs more frequently among women [2, 10, 13]. The co-existence of epicardial spasm makes assessment of the microcirculation challenging [2, 3].
By contrast, functional CMD represents an impaired flow-mediated/endothelium-dependent vasodilation of the microvasculature [10]. Functional CMD is characterized by an elevated resting flow that is related to enhanced nitric oxide synthase activity in response to increased myocardial oxygen demands; thus, a portion of the flow reserve is exhausted, resulting in the demand–supply mismatch [10]. Similarly, coronary arterioles’ insensitivity to vasodilatory stimuli and hypersensitivity to vasoconstrictive stimuli amplify; thus, diffuse stenoses in the microvasculature can result in ischemia.
Vasospastic angina is the clinical manifestation of myocardial ischemia caused by dynamic epicardial coronary obstruction due to a vasomotor disorder. Epicardial vessel spasm typically occurs when a hyper-reactive epicardial coronary vessel segment undergoes near-maximal contraction after exposure to vasoconstrictor stimuli, such as smoking, cold temperature, drugs, elevation in blood pressure, emotional stress, or hyperventilation. Concomitant vasospastic angina and CMD is associated with a worse prognosis versus either condition alone [13].
Heightened inflammation noted by elevation of pro-inflammatory markers, including C-reactive protein, IL-6, IL-1, etc., is associated with reduced coronary flow reserve and CMD [14, 15]. Chronic inflammation, as evidenced by elevated high-sensitivity C-reactive protein, is associated with adverse effects of structural and functional CMD and exacerbates the severity of angina, potentially explaining the higher prevalence of INOCA and CMD in women [14, 15]. Furthermore, autonomic nervous system activation, whether cardiac or central, is associated with intensification of the detrimental effects of functional CMD by impairing modulation between vasodilatory and vasoconstrictive stimuli [2, 3]
Diagnosis of INOCA
INOCA remains potentially underdiagnosed and thus undertreated. The diagnosis of INOCA is key to provide optimal care for these patients (Fig. 1). Briefly, these patients usually present with symptoms and/or signs of myocardial ischemia, alongside objective evidence of ischemia, whether on electrocardiogram or one of the various cardiac imaging modalities (echocardiography, nuclear imaging, magnetic resonance imaging, or spectroscopy), and absence of obstructive coronary arteries on an invasive coronary angiogram or computed tomography (stenosis of < 50%, FFR > 0.8) [1–4]. Further invasive diagnostic testing might be needed, including coronary artery functional testing (e.g., invasive coronary flow reserve, intravascular resistance, and acetylcholine response) to confirm the type of INOCA [2–4, 5•].
Fig. 1.
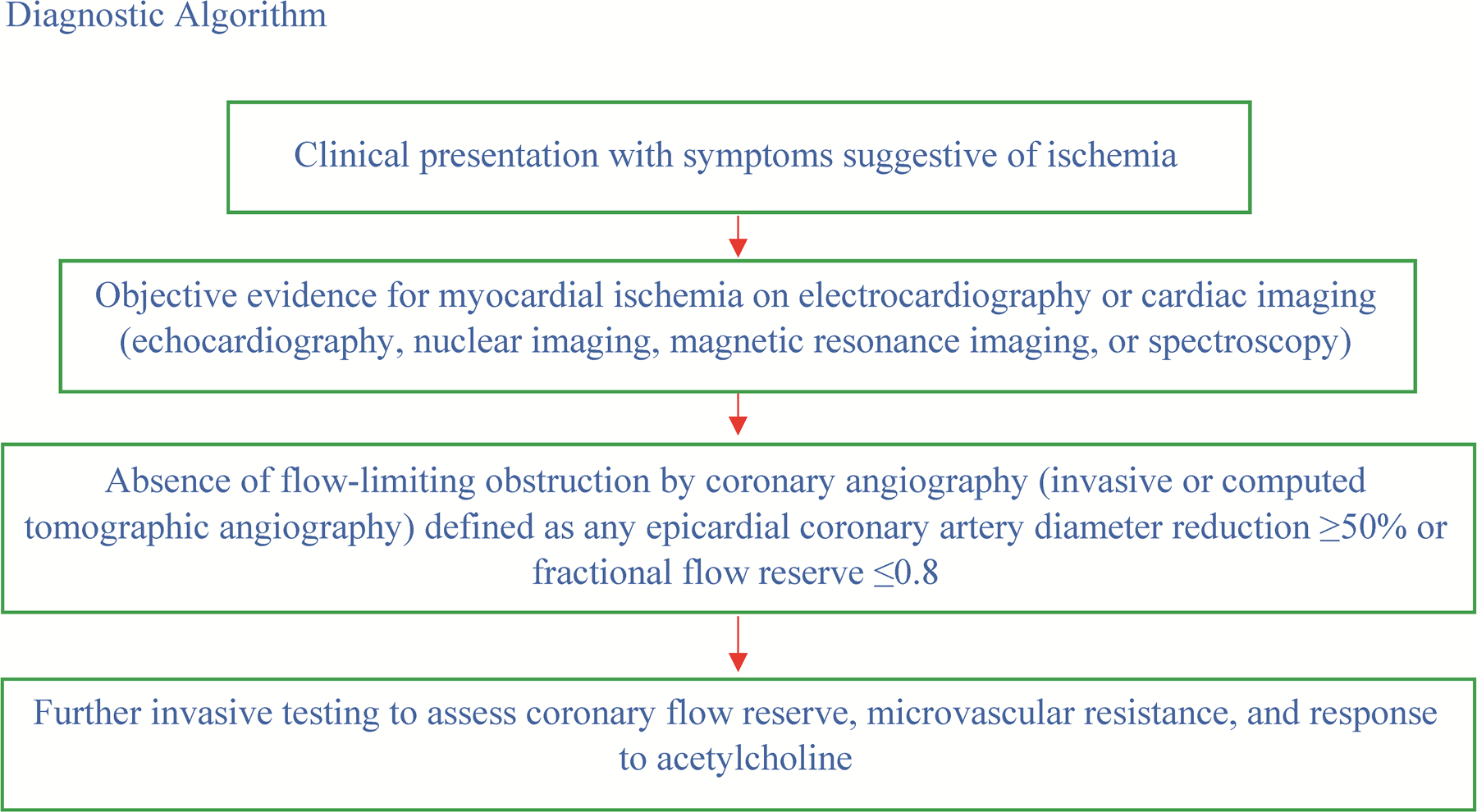
Diagnostic algorithm for patients with INOCA
Management of INOCA
It is important to emphasize that management of INOCA should be patient-centered based on the subtype and comorbidities, with a multidisciplinary care approach focusing on lifestyle modification and aggressive risk factor control, including blood pressure, glycemic and lipid management, along with smoking cessation and exercise/activity promotion [5•] (Fig. 2). Treatment of underlying comorbidities and avoiding known triggering factors are also key [5•].
Fig. 2.
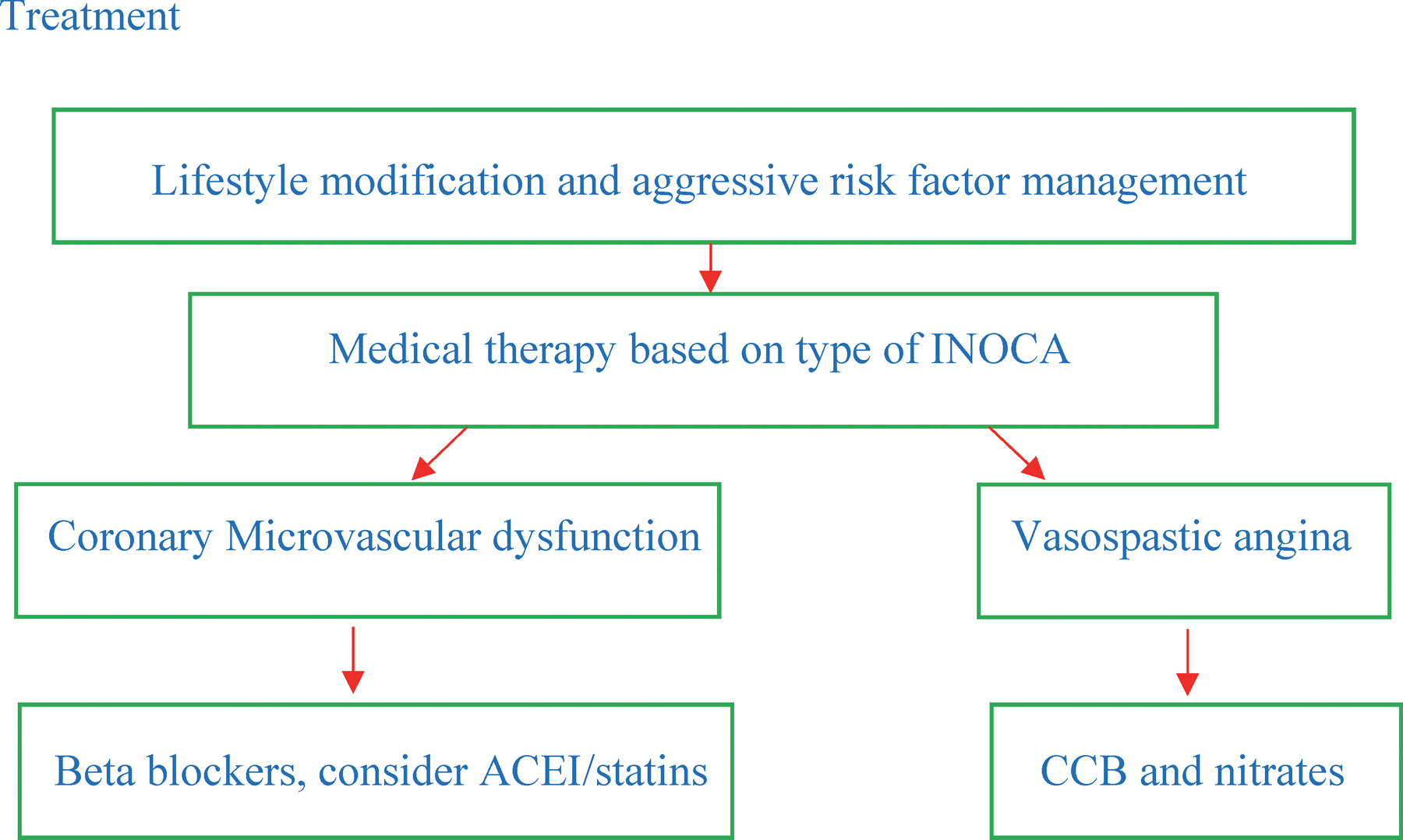
Summary of the treatment for INOCA. Abbreviations: INOCA, ischemia with non-obstructive coronary arteries; ACEI, angiotensin converting enzyme inhibitor; CCB, calcium channel blocker
Studies have suggested that certain medications maybe associated with benefit in this heterogenous group of patients. Numerous medications have been studied, including conventional cardiac medications (e.g., nitrates, beta-blockers, angiotensin converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs), and ranolazine, among others) as well as non-conventional treatment (for example, hormonal replacement therapy, exercise, tricyclic anti-depressants, and spinal cord stimulation, among other modalities) [16–19]. Beta-blockers, ACEIs, and statins have shown some promise in CMD [1–3, 16–24]. However, most data on both conventional and non-conventional therapies are driven from observational studies [2–4, 5•, 16–22]. One of the few randomized trials in this field is CorMicA, which included patients with symptoms of myocardial ischemia undergoing invasive coronary angiography [20]. Among the 151 patients with non-obstructive CAD, stratified medical therapy based on the type of CMD led to improvement in symptoms and outcomes [20]. Using this strategy, physicians were more likely to prescribe anti-anginal medications in the intervention group. Similarly, these patients were more likely to receive calcium channel blockers at 6 months. The CorMicA trial results, although of small sample size, showed that stratified therapy based on the type of microvascular dysfunction led to improvement in angina and quality of life. Patients with coronary vasospasm showed benefit from vasodilator therapy with calcium channel blockers and/or nitrate therapy, while patients with microvascular angina experienced improvement in symptoms with beta-blockers and consideration of ACEI (or equivalent)/statin therapy [20].
The ACEI therapy has been shown beneficial in CMD by either directly affecting coronary vascular function through modulation of the renin–angiotensin–aldosterone pathway, which also may provide improved blood pressure control. ACEIs have been associated with improved coronary flow reserve and coronary flow measurements by increasing endothelial nitric oxide bioavailability [17, 21]. The benefit of statins not only comes from its cholesterol-lowering effect, but also from its anti-inflammatory properties resulting in reduction of oxidative stress [21, 22]. Statins reduce plaque lipid-rich core, macrophage, and foam cell formation, decrease platelet reactivity, and promote fibrous cap thickening, leading to reduction in downstream microembolization and thrombotic events [21].
More recently, the IMPROvE-CED phase 1/2 trial showed proof of concept using intra-coronary autologous CD34 + cell therapy for CMD [23, 25]. The study included 20 patients; 75% were women. There was a significant improvement in angina scores and coronary blood flow at 6 months compared with a standard of care group who received maximally tolerated medical therapy alone [23, 25].
These findings led to the Women’s IschemiA Trial to Reduce Events in Non-ObstRuctIve CORonary Artery Disease (WARRIOR trial, NCT03417388). This is a multicenter, prospective, randomized, open, blinded outcomes evaluation (PROBE design) pragmatic trial investigating the efficacy of an intensive medical treatment (IMT) strategy versus usual care (UC) for prevention of cardiovascular disease (MACE) events (primary outcome) in 4,422 women with symptoms and/or signs of IHD without obstructive CAD (e.g., INOCA). Additionally, quality of life and treatment satisfaction (SAQ) will also be evaluated among several secondary outcomes [24, 26•]. To further understand the biology of statin, RAS blocker, and aspirin effects used in the IMT strategy, 900 women are co-enrolled in an embedded mechanistic substudy that will determine effects of potent statins and ACEIs or ARBs on non-calcified plaque volume and high-risk plaque morphology using coronary computed tomographic angiography, as well as on blood biomarkers of vascular inflammation and immune activation.
The Precision Medicine With Zibotentan in Microvascular Angina (PRIZE) (NCT04097314) is a trial assessing benefit of zibotentan, an oral endothelin A receptor antagonist, in patients with microvascular dysfunction [27]. The hypothesis behind the use of this medication in INOCA is that the minor G allele of the non-coding single nucleotide polymorphism enhances expression of the endothelin-1 gene in human vascular cells, increasing circulating concentrations of endothelin, and the prevalence of this allele is higher in patients with ischemic heart disease [27]. The primary outcome of the PRIZE trial is to assess the treadmill exercise duration [27].
The CorCTCA (NCT03477890) is another ongoing trial aiming to clarify the prevalence and outcomes of INOCA when coronary computed tomography angiography is used as the initial diagnostic modality [28]. The primary outcome is reclassification of the initial computed tomography’s diagnosis based on the interventional diagnostic procedure [28].
As biomarkers to detect ischemic myocardial injury continue to improve, myocardial infarction (MI) with open coronary arteries is increasingly observed and may contribute to 10–15% of the MI population. The Randomized Evaluation of Beta Blocker and ACEI/ARB Treatment in MINOCA Patients—MINOCA-BAT (NCT 03,686,696) is underway in Europe, Australia, and the USA. The primary objective of this pragmatic, randomized trial is to determine whether oral beta-blockade compared to no oral beta-blockade, and whether management with ACEI/ARB, compared with no ACEI/ARB, reduces all-cause death and readmission because of acute MI, ischemic stroke, or heart failure in patients discharged with MINOCA and with no clinical signs of heart failure and with LVEF ≥ 40%.
The few ongoing trials in this arena to address the optimal therapy in these patients with INOCA are summarized in Table 2.
Table 2.
Summary of ongoing trials in syndrome of ischemia with non-obstructive coronary arteries (INOCA)
| Trial | Objective |
|---|---|
| The WARRIOR trial (NCT03417388) [24, 26•] | Evaluate the benefit of intensive medical therapy with statin, angiotensin-converting enzyme inhibitors/angiotensin receptor blocker therapy, aspirin and lifestyle counseling and their impact on major adverse cardiac events in symptomatic women with INOCA |
| The PRIZE trial (NCT04097314) [27] | The Precision Medicine With Zibotentan in Microvascular Angina (PRIZE) trial’s goal is to assess the benefit of zibotentan, an oral endothelin A receptor antagonist, in patients with microvascular dysfunction. The primary outcome of the PRIZE trial is to assess the treadmill exercise duration using the Bruce protocol |
| The CorCTCA trial (NCT03477890) [28] | The trial’s aim is to clarify the prevalence and outcomes of INOCA when coronary computed tomography angiography is used as the initial diagnostic modality. Primary outcome is reclassification of the initial computed tomography’s diagnosis based on the interventional diagnostic procedure |
Knowledge Gaps and Ongoing Trials
There is a paucity of strong evidence evaluating the optimal therapy in patients with signs and/or symptoms of suspected ischemia and non-obstructive CAD, as our current data are mainly based on observational studies with the exception of CorMicA trial [20]. While CorMicA showed evidence supporting the benefit of an algorithmic approach to patients with suspected CMD with stratified treatment based on the specific endotype of CMD, CMD remains a heterogenous clinical condition with knowledge gaps in understanding the pathophysiology with potential disease mechanisms, interactions of different risk factors, cost-effective diagnostic testing, and optimal management options with their impact on outcomes as well as prognosis of different types of CMD. Moreover, INOCA may be associated with higher risk of developing heart failure with preserved ejection fraction, through potential mechanisms including ventricular remodeling and aortic stiffness. However, this association is not completely understood, and future studies addressing this knowledge gap are needed [29, 30].
Observational studies have shown potential benefit of ACEIs and statins, as well as beta-blockers; however, the benefit of these medications compared with no medication has not been confirmed in large randomized clinical trials [16–20]. Thus, large randomized clinical trials are needed to confirm the benefit and role of the different pharmacological and behavioral treatments.
Conclusions
INOCA is increasingly recognized as a heterogenous clinical entity, mainly affecting women. Diagnosis of INOCA is key, because recognizing which INOCA endotype the patient has guides our management, as illustrated by the CorMicA trial. There is still scarcity of evidence in the optimal therapy for these patients. However, there are current, ongoing clinical trials enrolling patients, and these trials will help us answer some of these questions in INOCA and CMD.
Funding
Dr. Pepine receives funding related to the topic from the National Institutes of Health (R01HL146158, WISE HFpEF https://clinicaltrials.gov/ct2/show/NCT02582021) and the US Department of Defense (W81XWH-17-2-0030, WARRIOR https://clinicaltrials.gov/ct2/show/NCT03417388).
Footnotes
Declarations
Conflict of Interest The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Women and Ischemic Heart Disease
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2022 Update: a report from the American Heart Association. Circulation 2022;145(8):e153–e639. 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Elgendy IY, Ya’Qoub L, Chen KH, Pepine CJ. Coronary microvascular dysfunction in patients with non-obstructive coronary arteries: current gaps and future directions. Drugs 2022;82(3):241–250. 10.1007/s40265-021-01667-y. [DOI] [PubMed] [Google Scholar]
- 3.Ya’qoub L, Elgendy IY, Pepine CJ. Syndrome of nonobstructive coronary artery diseases: a comprehensive overview of open artery ischemia. Am J Med 2021;134(11):1321–9. 10.1016/j.amjmed.2021.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and No Obstructive Coronary Artery Disease (INOCA): developing evidence-based therapies and research agenda for the next decade. Circulation 2017;135:1075–92. 10.1161/CIRCULATIONAHA.116.024534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation endorsed by Coronary Vasomotor Disorders International Study Group. EuroIntervention 2021;16:1049–69. 10.4244/EIJY20M07_01. This reference represents an expert consensus document for diagnosis and current management of patients with INOCA; it is important because it provides comprehensive data regarding the diagnosis and management approaches for INOCA based on the scientific evidence at the present time.
- 6.Morris PD, Gosling R, Zwierzak I, Evans H, Aubiniere-Robb L, Czechowicz K, et al. A novel method for measuring absolute coronary blood flow and microvascular resistance in patients with ischaemic heart disease. Cardiovasc Res 2021;117:1567–77. 10.1093/cvr/cvaa220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel MR, Dai D, Hernandez AF, Douglas PS, Messenger J, Garratt KN, et al. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J 2014;167:846–52.e2. 10.1016/j.ahj.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. ; WISE Investigators. Insights from the NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study, part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol 2006;47(suppl):S21–S29. 10.1016/j.jacc.2004.12.084. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhary R, Sukhi A, Chaudhary R, Jindal M, Vyas A, Rout A, et al. Gender differences in thrombogenicity among patients with angina and non-obstructive coronary artery disease. J Thromb Thrombolysis 2019;48:373–81. 10.1007/s11239-019-01901-1. [DOI] [PubMed] [Google Scholar]
- 10.Rahman H, Demir OM, Khan F, Ryan M, Ellis H, Mills MT, et al. Physiological stratification of patients with angina due to coronary microvascular dysfunction. J Am Coll Cardiol 2020;75:2538–49. 10.1016/j.jacc.2020.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830–40. 10.1056/NEJMra061889. [DOI] [PubMed] [Google Scholar]
- 12.Mejia-Renteria H, van der Hoeven N, van de Hoef TP, Heemelaar J, Ryan N, Lerman A, et al. Targeting the dominant mechanism of coronary microvascular dysfunction with intracoronary physiology tests. Int J Cardiovasc Imaging 2017;33:1041–59. 10.1007/s10554-017-1136-9. [DOI] [PubMed] [Google Scholar]
- 13.Sato K, Kaikita K, Nakayama N, Horio E, Yoshimura H, Ono T, et al. Coronary vasomotor response to intracoronary acetylcholine injection, clinical features, and long-term prognosis in 873 consecutive patients with coronary spasm: analysis of a single-center study over 20 years. J Am Heart Assoc 2013;2: e000227. 10.1161/JAHA.113.000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakr SA, Abbas TM, Amer MZ, Dawood EM, El-Shahat N, Abdel Aal IA, Ramadan MM. Microvascular angina: the possible role of inflammation, uric acid, and endothelial dysfunction. Int Heart J 2009;50:407–19. 10.1536/ihj.50.407. [DOI] [PubMed] [Google Scholar]
- 15.Schroder J, Mygind ND, Frestad D, Michelsen M, Suhrs HE, Bove KB, et al. Pro-inflammatory biomarkers in women with non-obstructive angina pectoris and coronary microvascular dysfunction. Int J Cardiol Heart Vasc 2019;24: 100370. 10.1016/j.ijcha.2019.100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bairey Merz CN, Handberg EM, Shufelt CL, Mehta PK, Minissian MB, Wei J, et al. A randomized, placebo-controlled trial of late Na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): impact on angina and myocardial perfusion reserve. Eur Heart J 2016;37:1504–13. 10.1093/eurheartj/ehv647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pauly DF, Johnson BD, Anderson RD, Handberg EM, Smith KM, Cooper-DeHoff RM, et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: a double-blind randomized study from the National Heart, Lung and Blood Institute Women’s Ischemia Syndrome Evaluation (WISE). Am Heart J 2011;162:678–84. 10.1016/j.ahj.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cox ID, Hann CM, Kaski JC. Low dose imipramine improves chest pain but not quality of life in patients with angina and normal coronary angiograms. Eur Heart J 1998;19:250–4. 10.1053/euhj.1997.0615. [DOI] [PubMed] [Google Scholar]
- 19.Lanza GA, Sestito A, Sandric S, Cioni B, Tamburrini G, Barollo A, et al. Spinal cord stimulation in patients with refractory anginal pain and normal coronary arteries. Ital Heart J 2001;2:25–30. [PubMed] [Google Scholar]
- 20.Ford TJ, Stanley B, Good R, Rocchiccioli P, McEntegart M, Watkins S, et al. Stratified medical therapy using invasive coronary function testing in angina: the CorMicA Trial. J Am Coll Cardiol 2018;72(23 Pt A):2841–55. 10.1016/j.jacc.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Pizzi C, Manfrini O, Fontana F, Bugiardini R. Angiotensin-converting enzyme inhibitors and 3-hydroxy-3-methylglutaryl coenzyme A reductase in cardiac Syndrome X: role of superoxide dismutase activity. Circulation 2004;109:53–8. 10.1161/01.CIR.0000100722.34034.E4. [DOI] [PubMed] [Google Scholar]
- 22.Zhang X, Li Q, Zhao J, Li X, Sun X, Yang H, et al. Effects of combination of statin and calcium channel blocker in patients with cardiac syndrome X. Coron Artery Dis 2014;25:40–4. 10.1097/MCA.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 23.Corban MT, Toya T, Albers D, Sebaali F, Lewis BR, Bois J, et al. IMPROvE-CED Trial: intracoronary autologous CD34+ cell therapy for treatment of coronary endothelial dysfunction in patients with angina and nonobstructive coronary arteries. Circ Res 2022;130:326–38. 10.1161/CIRCRESAHA.121.319644. [DOI] [PubMed] [Google Scholar]
- 24.Bairey Merz CN, Pepine CJ, Shimokawa H, Berry C. Treatment of coronary microvascular dysfunction. Cardiovasc Res 2020;116:856–70. 10.1093/cvr/cvaa006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henry TD, Bairey Merz CN, Wei J, Corban MT, Quesada O, Joung S, et al. Autologous CD34+ stem cell therapy increases coronary flow reserve and reduces angina in patients with coronary microvascular dysfunction. Circ Cardiovasc Interv 2022;15: e010802. 10.1161/CIRCINTERVENTIONS.121.010802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. • Handberg EM, Bairey Merz CN, Cooper-Dehoff RM, Wei J, Conlon M, Lo MC, et al. Rationale and design of the Women’s Ischemia Trial to Reduce Events in Nonobstructive CAD (WARRIOR) trial. Am Heart J 2021;237:90–103. 10.1016/j.ahj.2021.03.011 This reference summarizes the study design of the WARRIOR trial, a randomized clinical trial assessing the benefit of intensive medical therapy with ACEI, statin, beta blockers as well as behavioral therapy compared with standard of care. It will confirm or refute what previous observational studies have shown.
- 27.Morrow AJ, Ford TJ, Mangion K, Kotecha T, Rakhit R, Galasko G, et al. Rationale and design of the Medical Research Council’s Precision Medicine with Zibotentan in Microvascular Angina (PRIZE) trial. Am Heart J 2020;229:70–80. 10.1016/j.ahj.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sidik NP, McEntegart M, Roditi G, Ford TJ, McDermott M, Morrow A, et al. Rationale and design of the British Heart Foundation (BHF) Coronary Microvascular Function and CT Coronary Angiogram (CorCTCA) study. Am Heart J 2020;221:48–59. 10.1016/j.ahj.2019.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Samuel TJ, Wei J, Sharif B, Tamarappoo BK, Pattisapu V, Maughan J, et al. Diastolic dysfunction in women with ischemia and no obstructive coronary artery disease: mechanistic insight from magnetic resonance imaging. Int J Cardiol 2021;331:1–7. 10.1016/j.ijcard.2021.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elgendy IY, Pepine CJ. Heart failure with preserved ejection fraction: is ischemia due to coronary microvascular dysfunction a mechanistic factor? Am J Med 2019;132:692–7. 10.1016/j.amjmed.2018.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]


