Abstract
Thoracoscopic segmentectomy might be an alternative to lobectomy for small size lung cancer. Precise identification of the pulmonary intersegmental plane was needed for an optimal segmentectomy. Recently, (1) the ultra‐high‐definition 4K systems had claimed to overcome the lack of depth perception by secondary visual cues; (2) the no‐waiting procedure was induced as an alternative and optimized method for identifying the plane. It was unclear whether combined ultra‐high‐definition 4K endovision systems with “no‐waiting” technique in thoracoscopic segmentectomy could achieve an excellent result. A 68‐year‐old female patient was admitted into our hospital for occasional pulmonary nodule during her routine physical examination. The nodule is located between S8 and S9 segment, and was suspected to be an early‐stage lung cancer. She underwent a thoracoscopic S89 complex segmentectomy using ultra‐high‐definition 4K endovision systems and “no‐waiting” surgical technique. The intersegmental plane was clearly detected and easily treated by the endoscopic linear cutting staplers. The patient recovered well and was discharged without complications. Combining ultra‐high‐definition 4K endovision systems with “no‐waiting” technique seems to be an optimal thoracoscopic segmentectomy approach for the management of lung cancers.
Keywords: “no‐waiting” technique, 4K endovision systems, case report, pulmonary nodules, segmentectomy
In segmentectomy, the conventional method is to deal with the pulmonary artery, bronchus and pulmonary vein, then determine the intersegmental plane using “inflation–deinflation” method, and cut the plane finally. This “inflation–deinflation” method usually takes 15 minutes, or even longer. The “no waiting” method optimizes the flow of the above steps. After the pulmonary artery was processed, the intersegmental plane procedure was directly executed. During the time of the collapse of lung tissue, the bronchus and pulmonary vein were processed successively. Finally, the intersegmental plane was cut. In this process, we can save a lot of operation time. A high‐resolution 4K thoracoscope is more useful for this technique.

INTRODUCTION
There has been a noted increase in the number of small lung nodules and non‐solid lung cancers being identified because of the advances in computed tomography (CT) technology over the last decade. The National Comprehensive Cancer Network guidelines recommend that segmentectomy can be an alternative to lobectomy in terms of intent to cure early‐stage non–small cell lung cancer (NSCLC). 1 , 2
Precise identification of the pulmonary intersegmental plane is needed for optimal segmentectomy. Several techniques have been proposed for the identification and treatment of the intersegmental planes. 3 , 4 , 5 Recently, the no‐waiting procedure, as described by Wang et al., 6 was an alternative and optimized method for identifying the plane of the lung segment.
The ultra‐high‐definition 4K systems (4K systems), which has four times the pixels and double the resolution (3840 × 2160 pixels) of standard two‐dimensional high‐definition systems, claimed to overcome the lack of depth perception by secondary visual cues. 7 , 8 This has been shown in an experimental study to be comparable to three‐dimensional (3D) systems. 9 The 4K systems were applied in several surgeries, including proctectomy, 10 gastrectomy, 11 and cholecystectomy. 12 It was thought that the 4K systems might help in dealing with the intersegmental plane. However, there is still no literature about the 4K systems in segmentectomy.
This is the first study that reports a complex anterior–lateral basal (S8‐9) segmentectomy that combined the ultra–high‐definition 4K endovision systems with “no‐waiting” technique, which might be an optimal thoracoscopic segmentectomy approach.
CASE PRESENTATIONS
Patient information
A 68‐year‐old female patient was admitted into our hospital for her occasional pulmonary nodule during routine physical examination. The nodule was located between S8 and S9 segments and was suspected to be early‐stage lung cancer (Figure 1(a)). It was revealed that her cardiopulmonary function was too poor to undergo a lobectomy after carefully analysis of her medical records. It was suggested she receive a complex compromised segmentectomy that was an S8–S9 segmentectomy.
FIGURE 1.
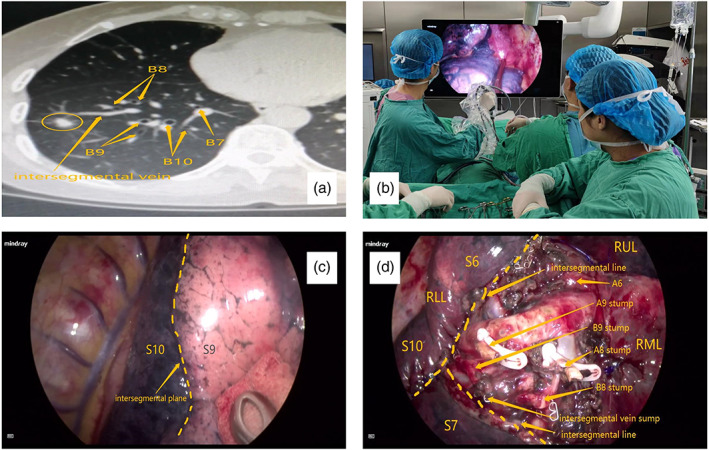
A complex anterior‐lateral basal segmentectomy. (a) The computed tomography (CT) showed a small nodule located between S8 and S9 segment, and was suspected to be an early‐stage lung cancer. (b) The ultra–high‐definition 4K systems were applied in the surgery. (c) The intersegmental plane between S9 and S10 was clearly detected in the Mindray 4K device. (d) The final surgical field after the S8–S9 pulmonary tissues were removed
Surgical methods
The patient was placed in the left lateral decubitus position with double‐lumen intubation and one‐lung ventilation. An almost 3‐cm incision was made on the fifth intercostal space in the right midaxillary line and then a protector was placed. The ultra–high‐definition 4K systems (HyPixel U1, Mindray) was applied (Figure 1(b)). After confirming the chest cavity was without tumor spread, we dissected the basal trunk of the low right lobe pulmonary artery along the oblique fissure, sparing the A7, and then dissected the A8 and ligated it. The A9–A10 trunks were exposed, and A9 was separated and ligated as well. We instructed the anesthesiologist to inflate the right lungs with pure oxygen and allow the left lungs ventilate continuously after all the lower right lobe lung tissues had expanded completely. We continued to dissect the B8 and B9 bronchi, severing them separately with the endoscopic linear cutting staplers (ENDO SRC, Reach Surgical). The bronchial stump of B8 and B9 were allowed, and the intersegmental vein V8a was explored and ligated. Finally, the intersegmental plane was clearly detected, and we used the endoscopic linear cutting staplers (ENDO SRC, Reach Surgical) to deal with this plane (Figure 1(c),(d)). The patient recovered well and was discharged.
DISCUSSION AND CONCLUSIONS
Segmentectomy can achieve an adequate surgical margin for a cT1N0M0 NSCLC located at the central area of the pulmonary segment, including ground glass nodules. Nevertheless, the major challenge is to identify targeted segmental bronchus and intersegmental veins and arteries, to guarantee an adequate anatomical resection. The ongoing prospective randomized study by the Japanese Clinical Oncology Group 1211 (JCOG1211), 13 the JCOG0802/West Japan Oncology Group 4607L, 14 and the Cancer and Leukemia Group B 140503 15 trials will provide important information about this. In the near future, anatomical resection, including segmentectomy with lymph node dissection or sampling, will become a standard treatment for patients with early‐stage NSCLC.
With the development of endosurgical equipment, the thoracoscopic segmentectomy was supposed to be a mature technique. 16 The 4K system with a large monitor (55 inches) and a remarkably high resolution (3840 × 2160 pixels) is expected to provide visual cues that can overcome the lack of binocular vision. The 4K systems were helpful in performing laparoscopic cholecystectomy, transabdominal preperitoneal herniorrhaphy, and Heller's cardiomyotomy. 12 However, no study was conducted on thoracoscopic segmentectomy.
Some authors demonstrated that 3D computed tomography bronchography and angiography (3D‐CTBA) or three‐dimensionally printed models are preoperative tools that may facilitate the planning of segmentectomy. 17 It was believed that these methods could help identify the variation of segmental structures and design the safety surgical margin. However, they were not used in all the institutions because of inadequate equipment, complex operational processes, and costly fees.
Recently, Wang et al. 6 reported the “no‐waiting” technique, which severed the target segmental pulmonary artery, inflated the lung with atmospheric air, dissected the hilum, and divided the target segmental bronchus. The entire procedures were performed at a stretch without any pause. This implied that “no waiting” technique optimized the surgical procedure and was an alternative and optimized method for identifying the intersegmental plane.
Taken together, our aim in this study was to evaluate if there were any advantages that combined the 4K systems and “no‐waiting” technique in thoracoscopic segmentectomy.
In this case, the preoperative 3D‐CTBA was not performed. We applied the 4K systems in this surgery, and the major segmental structures were distinguished easily. Moreover, the “no waiting” technique was used, that was after cutting the targeted segmental artery and inflating the right lungs. We, then, dissected the other targeted structures continuously. Because of the ultra–high‐definition 4K devices, the intersegmental plane was well discovered, which help assert whether the segmental structures, including exact dissection of the segmental bronchi and intersegmental veins.
To our knowledge, this was the first time to declare the merit of 4K systems in segmentectomy for a pulmonary nodule. In our opinion, the combined 4K systems and “no waiting” technique could: (1) shorten the waiting time of intersegmental plane detection and reduce the total operation time; (2) compensate the insufficiency of lacking preoperative 3D‐CTBA; and (3) avoid unnecessary exploration of the other pulmonary structures.
Therefore, combining ultra–high‐definition 4K endovision systems with “no‐waiting” technique seems to be an optimal thoracoscopic segmentectomy approach for the management of lung cancers. However, we believe this still needs a lot of further study to confirm our initial discoveries.
AUTHOR CONTRIBUTIONS
Chun Chen and Mingqiang Liang designed this study. Mingqiang Liang, Liang Wang, Yifang Wang and Bowen Wang performed the surgery, and Jinhai Xu, Zhiliang Duan, Jiabin Gao and Shixin Li analyzed and interpreted the data. Mingqiang Liang was the major contributors in writing the manuscript. All authors read and approved the final manuscript.
FUNDING INFORMATION
This work was supported by Fujian Provincial Health Technology Project (2020CXA023) and Key Laboratory of Cardio‐Thoracic Surgery (Fujian Medical University), Fujian Province University Construction (No.2019‐67).
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. Written informed consent to publish these images was obtained from study participants.
ACKNOWLEDGMENTS
We would like to thank Editage (www.editage.cn) for English language editing.
Liang M, Wang L, Gao J, Duan Z, Xu J, Wang Y, et al. An optimal thoracoscopic segmentectomy approach: Combined ultra‐high‐definition 4K endovision systems with “no‐waiting” technique in S8‐9 complex segmentectomy. Thorac Cancer. 2023;14(12):1098–1101. 10.1111/1759-7714.14833
Contributor Information
Bowen Wang, Email: wbwzh68@163.com.
Chun Chen, Email: chenchun0209@fjmu.edu.cn.
DATA AVAILABILITY STATEMENT
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
REFERENCES
- 1. Okada M, Yoshikawa K, Hatta T, Tsubota N. Is segmentectomy with lymph node assessment an alternative to lobectomy for non‐small cell lung cancer of 2 cm or smaller? Ann Thorac Surg. 2001;71(3):956–60. [DOI] [PubMed] [Google Scholar]
- 2. Schuchert MJ, Pettiford BL, Keeley S, D'Amato TA, Kilic A, Close J, et al. Anatomic segmentectomy in the treatment of stage I non‐small cell lung cancer. Ann Thorac Surg. 2007;84(3):926–33. [DOI] [PubMed] [Google Scholar]
- 3. Okada M, Mimura T, Ikegaki J, Katoh H, Itoh H, Tsubota N. A novel video‐assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg. 2007;133(3):753–8. [DOI] [PubMed] [Google Scholar]
- 4. Oh S, Suzuki K, Miyasaka Y, Matsunaga T, Tsushima Y, Takamochi K. New technique for lung segmentectomy using indocyanine green injection. Ann Thorac Surg. 2013;95(6):2188–90. [DOI] [PubMed] [Google Scholar]
- 5. Saito D, Matsumoto I, Waseda R, Tatemichi K, Tanaka Y, Yoshida S, et al. A method to identify pulmonary intersegmental planes with intravenous vitamin B2 injection. Surg Today. 2021;51(5):836–43. [DOI] [PubMed] [Google Scholar]
- 6. Wang C, Cai L, Chen Q, et al. No‐Waiting Segmentectomy: An Optimized Approach for Segmentectomy. J Thorac Dis. 2021;13(2):784–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Woo P. 4K video‐laryngoscopy and video‐Stroboscopy: preliminary findings. Ann Otol, Rhinol, Laryngol. 2016;125(1):77–81. [DOI] [PubMed] [Google Scholar]
- 8. Rigante M, Rocca GL, Lauretti L, et al. Preliminary experience with 4K ultra‐high definition endoscope: analysis of pros and cons in skull base surgery. Acta Otorhinolaryngol Ital. 2017;37(3):237–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harada H, Kanaji S, Hasegawa H, Yamamoto M, Matsuda Y, Yamashita K, et al. The effect on surgical skills of expert surgeons using 3D/HD and 2D/4K resolution monitors in laparoscopic phantom tasks. Surg Endosc. 2018;32(10):4228–34. [DOI] [PubMed] [Google Scholar]
- 10. Zhang XJ, Ma PF, Li S, Zhang JL, Zhao YZ. 4K laparoscopic total mesorectal excision for ultralow rectal cancer. Tech Coloproctol. 2021;25(1):137–8. [DOI] [PubMed] [Google Scholar]
- 11. Zhang L, Hong H, Zang L, Dong F, Lu A, Feng B, et al. Application value of 4K high‐definition system in laparoscopic gastrectomy: preliminary results and initial experience. J Laparoendosc Adv Surg Tech. 2021;32:137–41. [DOI] [PubMed] [Google Scholar]
- 12. Parshad R, Nanjakla Jayappa S, Bhattacharjee HK, et al. Comparison of three‐dimensional (3D) endovision system versus ultra‐high‐definition 4K endovision system in minimally invasive surgical procedures: a randomized‐open label pilot study. Surg Endosc. 2022;36(2):1106–1116. [DOI] [PubMed] [Google Scholar]
- 13. Aokage K, Saji H, Suzuki K, Mizutani T, Katayama H, Shibata T, et al. A non‐randomized confirmatory trial of segmentectomy for clinical T1N0 lung cancer with dominant ground glass opacity based on thin‐section computed tomography (JCOG1211). Gen Thorac Cardiovasc Surg. 2017;65(5):267–72. [DOI] [PubMed] [Google Scholar]
- 14. Tsuboi M. A phase III randomized trial of lobectomy versus limited resection for small‐sized peripheral non‐small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol. 2010;40(3):271–4. [DOI] [PubMed] [Google Scholar]
- 15. Kohman LJ, Gu L, Altorki N, et al. Biopsy first: lessons learned from cancer and leukemia group B (CALGB) 140503. J Thorac Cardiovasc Surg. 2017;153(6):1592–1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheng K, Zheng B, Zhang S, et al. Feasibility and learning curve of uniportal video‐assisted thoracoscopic segmentectomy. J Thorac Dis. 2016;8:S229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Qiu B, Ji Y, He H, Zhao J, Xue Q, Gao S. Three‐dimensional reconstruction/personalized three‐dimensional printed model for thoracoscopic anatomical partial‐lobectomy in stage I lung cancer: a retrospective study. Transl Lung Cancer Res. 2020;9(4):1235–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.


