Abstract
Introduction
Several different forms of automated insulin delivery systems (AID systems) have recently been developed and are now licensed for type 1 diabetes (T1D). We undertook a systematic review of reported trials and real-world studies for commercial hybrid closed-loop (HCL) systems.
Methods
Pivotal, phase III and real-world studies using commercial HCL systems that are currently approved for use in type 1 diabetes were reviewed with a devised protocol using the Medline database.
Results
Fifty-nine studies were included in the systematic review (19 for 670G; 8 for 780G; 11 for Control-IQ; 14 for CamAPS FX; 4 for Diabeloop; and 3 for Omnipod 5). Twenty were real-world studies, and 39 were trials or sub-analyses. Twenty-three studies, including 17 additional studies, related to psychosocial outcomes and were analysed separately.
Conclusions
These studies highlighted that HCL systems improve time In range (TIR) and arouse minimal concerns around severe hypoglycaemia. HCL systems are an effective and safe option for improving diabetes care. Real-world comparisons between systems and their effects on psychological outcomes require further study.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13300-023-01394-5.
Keywords: Automated insulin delivery system, Hybrid closed loop, T1D
Key Summary Points
| Advances in diabetes technologies have led to the development of hybrid closed-loop systems |
| We undertook a systematic review of the available evidence for these systems |
| We included 62 clinical studies relating to six different hybrid closed-loop systems |
| The studies demonstrated a beneficial impact of hybrid closed-loop systems on glycaemic parameters |
| Further work is needed to understand their impact on psychological aspects of diabetes |
Introduction
Despite advances in the management of type 1 diabetes (T1D), the majority of people with T1D continue to remain outside the recommended target range for glycaemic control [1, 2]. The 2018 Type 1 Diabetes Exchange registry found that only 21% of Americans with T1D were achieving their target glycated haemoglobin (HbA1c) level, and similarly, in 2019, the National Diabetes Audit found that less than a third of people in the United Kingdom (UK) with T1D achieved their HbA1c targets [3, 4]. There is therefore a need for further improvements in diabetes care in order to help people with diabetes to attain glycaemic control within the recommended range.
Automated insulin delivery (AID) systems have been designed to improve glycaemic control and reduce the burden for people with T1D [3, 5]. One form of these is referred to as ‘closed-loop’ systems or ‘artificial pancreas’ devices; these systems essentially consist of three components: an insulin pump, a computer or smartphone-based algorithm, and a continuous glucose monitor (CGM) [3]. These systems aim to help people with T1D achieve as near-normal regulation of their glucose as possible through glucose monitoring and insulin delivery every few minutes, with minimal intervention from the user [5].
Currently, most AID systems are hybrid closed-loop (HCL) systems, whereby basal insulin is automatically determined and delivered, but mealtime insulin boluses must be managed manually, with people with diabetes also required to provide information about the sizes and times of meals [6–9] (Fig. 1). These systems are generally single hormone, delivering insulin only [8–10]. Ideally, AID systems would instead be fully closed-loop systems that were completely automated, requiring minimal user input and with no need for prior warning of mealtimes or exercise, as required by hybrid systems [9–11]. The sensor lag time and delays in insulin action times have been some of the barriers to achieving this, although progress in this regard has been noted in some open-source AID systems, based on testing in animal models and anecdotal real-world experiences in clinics [12]. An ideal AID system would also be a dual-hormone system in order to more closely mimic a biological pancreas and reduce the risk of hypoglycaemia by countering aggressive insulin delivery through the delivery of glucagon in addition to insulin [13]. However, the cost and complexity of dual-hormone systems have thus far limited their development [14, 15].
Fig. 1.
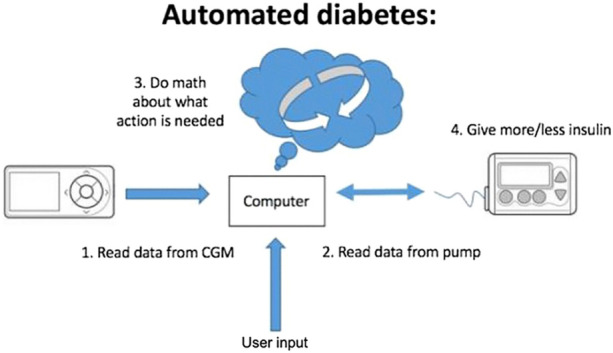
Components required for hybrid closed-loop systems. Figure taken from [21].
AID systems can broadly be divided into two categories: commercial and open-source automated insulin delivery (OS-AID) or ‘do-it-yourself’ (DIY) systems. It is estimated that, globally, around 10,000 people are using some form of OS-AID system [16]. Like commercial HCL systems, OS-AID systems are based on an algorithm, CGM, and insulin pump [14]. However, unlike commercial AID systems, OS-AID user-led DIY systems are not regulated and do not have medical approval, although they have a significant body of real-world and recent randomised controlled trial (RCT) data supporting their use [14, 16–18]. Alongside a responsive online community, agility in improving the algorithm and safety testing without incurring delays from having to meet regulations or undergo lengthy clinical trials means that OS-AID systems can be tested and modified far more quickly than commercial AID systems [14]. The recent consensus in medical practice has been detailed elsewhere [16].
By comparison, there is an appreciably greater evidence base of clinical trials for commercial HCL systems that are given industry funding. Commercial HCL systems have been shown to increase the proportion of time that users spend within a target glycaemic range, both overnight and over a 24-h period [19]. Additionally, they have been found to lower mean glucose levels and lower HbA1c [5, 20]. Clinical trials have also demonstrated that commercial HCL systems do not increase the time spent in hypoglycaemia or increase the occurrence of hypoglycaemia, and in some studies the systems have been found to reduce hypoglycaemia [11]. Although commercial systems are comparable in that they are all regulated, they are not homogeneous; each system has its own algorithm, the settings and features available differ between systems, and the devices the systems are compatible with also vary [16].
Devices Being Assessed
The HCL systems that are being reviewed in this study are all commercial hybrid closed-loop systems that have published trial data and have received CE or United States Food and Drug Agency (FDA) approval for use in type 1 diabetes (Table 1).
Table 1.
Summary of currently available commercial systems
| System name | Medtronic 670G/770G | Medtronic 780G | Tandem Control-IQ | CamAPS FX | Diabeloop DBLG1 | Diabeloop DBLG Hu | Omnipod 5 |
|---|---|---|---|---|---|---|---|
| Algorithm |
SmartGuard™ Minimed 670G/770G 3.0 HCL |
SmartGuard™ Minimed 780G 4.0 Advanced Hybrid Closed-Loop |
Control IQ 1.0 | CamAPS FX | DBLG1 | DBLG Hu | SmartAdjust™ |
|
User interface |
Insulin pump 770G only: Android or Apple phone (view only) |
Insulin pump, Android or Apple phone (view only) |
Insulin pump, and Android or Apple phone app (t:connect Mobile for view and mobile bolus in US) | Android phone | Separate handheld device or Android or Apple phone app | Separate handheld device |
System “Controller” (locked down Android-based device) Or smartphone app available on certain android phones |
| Compatible CGMs | Guardian Link 3 |
Guardian Link 3 Guardian Link 4 |
Dexcom G6 |
Dexcom G6 Libre 3a |
Dexcom G6 | Dexcom G6 | Dexcom G6 |
|
Compatible insulin pumps |
Medtronic 670G/780G pump | Medtronic 780G pump | Tandem t:slim X2 | DANA Diabecare RS; DANA-i; Ypsomed Ypsopump |
Kaliedo patch AccuChek Insight; Dana-i pump; EOFlow |
Kaliedo patch AccuChek Insight; Dana-i pump; EOFlow |
Omnipod 5 patch pumps |
|
FDA approval |
Age ≥ 7 years | Age ≥ 6 years | Age ≥ 2 years | ||||
| CE mark | Age ≥ 7 years | Age ≥ 7 years | Age ≥ 6 years | Age ≥ 1 year | Adults | Adults | Age ≥ 2 years |
aIn selected European countries
Medtronic 670G/770G
The Medtronic MiniMed 670G was the first hybrid AID system to be available commercially after it was licensed by the United States Food and Drug Agency (FDA) in 2017, and then became available in Europe the following year, for use in people aged 7 and above [5, 11]. Currently, the system is available in the US, Canada, and some countries in Europe, the Middle East, and Hong Kong. It uses the MiniMed 670G insulin pump along with the Medtronic Guardian Sensor 3 CGM and an algorithm called SmartGuard, which is embedded in the insulin pump [11, 22]. The Guardian Sensor 3 CGM can be used for 7 days and requires between two and four calibrations each day [22]. In ‘auto mode’, the 670G automates control of basal insulin delivery every 5 min based on the measured glucose values, but it also takes into consideration the insulin delivery history of the user over the previous 2–6 days [5]. A ‘manual mode’ allows the system to be used as a sensor-augmented (with a predictive low-glucose suspend) or stand-alone pump [22]. The device also has integrated safety features, such as the system being able to revert to manual mode if insulin delivery is approaching a maximum or minimum or if the CGM signal is lost [23]. In the US, the 770G offers the same algorithm and sensor use as 670G; however, it utilises an improved 780G pump device which has Bluetooth connectivity and the ability to receive software updates.
Medtronic 780G
The other Medtronic AID system being assessed is the MiniMed 780G. Also known as the Advanced Hybrid Closed Loop (AHCL), the 780G is an upgraded version of the 670G with Bluetooth connectivity and remote software updates added [22]. The ability of the system to automatically deliver correction boluses was also added [22]. The 780G system uses the Medtronic 780G insulin pump, and, similarly to the 670G AID system, the 780G is compatible with the Medtronic Guardian 3 CGM and the more recently launched Medtronic Guardian 4 CGM [22]. Like the 670G, the algorithm used by the 780G is built into the insulin pump [22]. The 780G has received its CE mark and is currently available in some European countries; however, FDA approval is still pending.
Tandem Control-IQ
The Tandem Control-IQ hybrid closed-loop consists of the Tandem t:slim X2 insulin pump, the Dexcom G6 CGM, and Control-IQ technology [22]. The Dexcom G6 can be used for 10 days [24]. The Control-IQ algorithm within the insulin pump predicts glucose 30 min in advance and correspondingly modifies insulin delivery [24]. As with all of the other systems being explored in this project, the Control-IQ allows for higher glucose targets to be set for announced exercise. The Control-IQ also allows an additional target to be set at night-time [24]. Unlike the other AID systems discussed here, this system relies on setting a basal program which is used by the algorithm to adjust insulin delivery. The system was approved by the FDA in 2019 for use in people with T1D aged 14 and above and was given CE marking for use in people with T1D aged older than 6 years [24]. Currently, the Control-IQ is available in the US, Canada, and some European countries.
CamAPS FX
The CamAPS FX is a HCL system compatible with the Dexcom G6 and Libre 3 CGM devices and the DANA Diabecare RS, DANA-i, and Ypsomed Ypsopump insulin pumps. The CamAPS FX has CE marking for use in people with T1D aged 1 and above, and is available in select European countries [24]. It allows for multiple glucose targets that can be set at different times. The CamAPS FX is currently the only commercial AID system licensed for use during pregnancy [24]. As the CamAPS FX is an Android app, a compatible Android smartphone is required to use the system in order for glucose levels to be managed through Bluetooth connected to a compatible pump and sensor [24]. Whereas the other AID systems being evaluated in the real-world study are only compatible with rapid-acting insulin, the CamAPS FX is also compatible with ultra-rapid insulin [24].
Diabeloop Generation 1 (DBLG1)
The Diabeloop Generation 1 (DBLG1) system integrates a Kaliedo insulin patch pump, Dexcom G6 CGM, and a command module which hosts the system’s algorithm [25, 26]. As with the other AID systems being explored in this project, the DBLG1 is a hybrid closed-loop system that requires mealtime announcement of carbohydrate intake [27]. The DBLG1 provides users with the ability to access a real-time overview of their glucose sensor data through the web-based platform MyDiabeloop [25]. The DBLG1 has received the CE mark for use in adults with T1D and is available in some countries in Europe [28].
Diabeloop for Highly Unstable Type 1 Diabetes (DBLHU)
The Diabeloop for Highly Unstable Type 1 Diabetes (DBLHU) is an AID system derived from the DBLG1 that has recently received the CE mark for the indication of unstable diabetes [29, 30].
Omnipod 5
The Omnipod 5 consists of a tubeless insulin pump, a wireless handheld device used to operate the pump, and the Dexcom G6 CGM [31]. Unlike most AID systems, there are no tubes connecting the infusion site to the Omnipod 5 [31]. The system delivers insulin micro-boluses every 5 min and, similarly to the other AID systems, requires the user to deliver mealtime boluses [31]. Following the pivotal study as well as further study data, it received FDA approval and a CE mark for use in type 1 diabetes in individuals aged 2 years or older [32].
The Need for Real-World Evidence
Evidence from the real-world use of commercial AID systems is needed because of the limitations of randomised controlled trials (RCTs). Inclusion criteria used in RCTs are typically very restrictive and often exclude people with comorbidities [24]. By comparison, real-world studies usually have fewer restrictions on population inclusion and can therefore capture information about groups that are often underrepresented in trials, as well as populations not studied in clinical trials, and provide information about potential interactions with comorbidities [33]. If trials for diabetes interventions only include participants with good baseline blood glucose control, these participants may engage differently with the intervention being trialled than participants with poor initial baseline glycaemic control, making the RCT results less generalisable. Less restrictive inclusion criteria in real-world studies can help to ascertain more generalisable data [24].
Moreover, the ‘trial effect’ of RCTs may unduly influence the measured benefit of an intervention; the follow-up of participants in RCTs is generally far more rigorous than in clinical practice, and as a result, adherence to the intervention being trialled may be greater than it would be outside of the trial setting, leading to misleading results [24]. Real-world studies lacking the same level of follow-up as RCTs may therefore provide a more realistic estimate of the treatment effect of an intervention.
RCTs are also hindered by the long duration of time they take to complete, which, as well as being frustrating for people, can slow the pace of developments [33]. Adjustments to or advances in interventions being investigated are delayed by the time taken for RCTs to be conducted and for the results to be published. Conversely, real-world studies can generally be completed more quickly, helping to overcome these issues.
Evaluating Glycaemic Outcomes
Although previously there were inconsistencies between the thresholds for and the reporting of target glycaemic ranges, an international consensus has since been reached [22]. The target threshold for glucose levels in this project has been chosen in order to reflect the international consensus. The use of TIR as an outcome in this project can be deemed a valid outcome as it has been found that TIR is a metric that matters to people with T1D; an analysis survey of 4,268 people with diabetes found that the greatest incentive participants had to choose one therapy over another was the share of time in the ideal glucose range for ‘most of the day’ [5, 20]. Furthermore, TIR has been found to have a strong association with risk for microvascular complications and can therefore be justified as a valid endpoint [11].
Aim
This systematic review will explore the existing literature for commercial hybrid HCL systems that have published data and have received CE or United States Food and Drug Agency (FDA) approval for use in type 1 diabetes to help understand the literature for HCL systems as a whole and allow comparisons between the different systems. Psychosocial outcomes will also be investigated separately.
Methods
Systematic Review
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used to plan, devise, and report the systematic review [34].
Study Design
The search strategy was based on search terms describing the names of the different commercial AID systems that are currently licensed or being licensed for use: the Medtronic 670G; the Medtronic 780G/Advanced Hybrid Closed Loop; the Control-IQ; the CamAPS FX; the DBLG1; the DBLHU; and the Omnipod 5. In order to further refine the searches, in some instances the Boolean operators ‘AND’ and ‘OR' were used. The literature search was conducted using PubMed from inception to October 2022. The search using PubMed, which is an interface that can search the Medline database as well as additional content, was also supplemented by searches of system manufacturer websites which had collections of publications relating to their AID systems.
Titles, abstracts, and full-text articles were screened. After the removal of duplicate results and papers that did not meet the inclusion criteria, the relevant data were extracted from each of the papers included in the final review. These data were recorded in an Excel spreadsheet before being analysed by two independent reviewers.
Eligibility Criteria
The following inclusion criteria for the systematic review were used: papers focused on single-hormone commercial hybrid AID systems; participants with T1D; studies with endpoints relating to glycaemic control; and the study design was either a randomised controlled trial, a crossover trial, an observational/real-world study, a feasibility study, or a pilot study. Studies with solely psychosocial endpoints were collated and analysed separately from the systematic review. Studies with glycaemic and psychosocial endpoints were included in both the systematic review and the analysis of psychosocial outcomes.
The following exclusion criteria were used: studies less than 4 weeks in duration (unless they were real-world, feasibility, or pilot studies); studies published after July 2022 in peer-reviewed journals; studies not published in English; studies that focused on DIY, dual-hormone, or non-hybrid systems. There were no restrictions on age or pregnancy status.
The eligibility criteria were chosen with the intention of being broad to maximise the available literature on the subject of commercial AID systems.
Endpoints
The following endpoints were the main focus of the systematic review: the percentage of TIR; the change in TIR; HbA1c; and the incidence of severe hypoglycaemia, diabetic ketoacidosis (DKA), or serious adverse events.
Psychosocial outcomes for the separate review included quality of life (QoL) measures, patient-reported outcome measures (PROMs), patient-reported experience measures (PREMs), validated psychological, sleep, and treatment satisfaction scores, and qualitative data.
Data Collection and Analysis
For each of the included papers, the following data were extracted: the study duration; the number of participants; the eligibility criteria; the study type; the country the study was conducted in; the primary and secondary endpoints; the methods; the results; and the limitations of the study.
Data from studies ≥ 4 weeks long waere analysed; for AID systems with multiple papers of this duration, findings were reported from studies of the longest duration and/or with the highest number of participants. Data from studies ≥ 4 weeks in duration were tabulated and full details of the research are included in the Supplementary Material.
Studies with psychosocial endpoints and results were analysed separately, and psychosocial outcomes were summarised from the studies.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
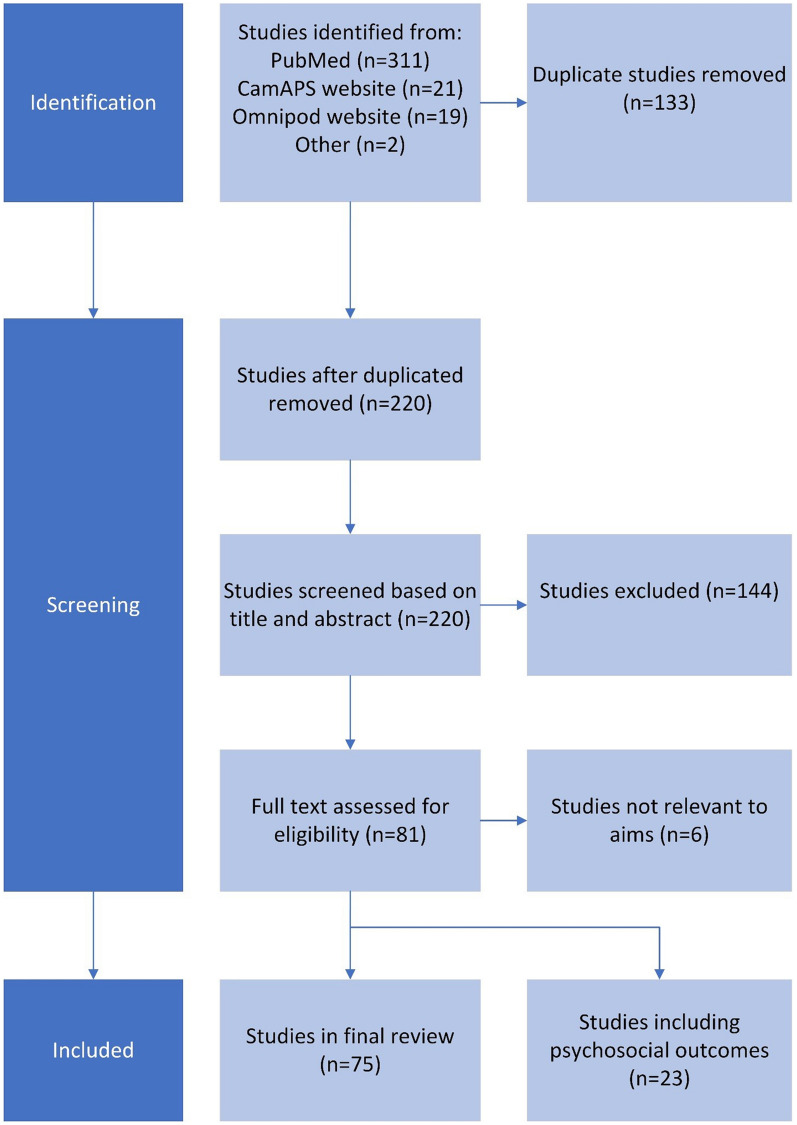
In total, 353 search results were identified. After duplicates and papers that did not meet the inclusion criteria were excluded, a total of 75 papers were included in the final review. The full selection process is shown in Fig. 2. The following number of studies were included for each HCL system: 19 papers for Medtronic 670G; eight for Medtronic 780G; 11 for Control-IQ; 14 for CamAPS FX; three for DBLG1; one for DBLHU; and three for Omnipod 5. In addition to six studies that were also included in the systematic review, 17 articles were identified as having psychosocial outcomes. These 23 studies were analysed separately to the systematic review.
Fig. 2.
Systematic review flowchart
Medtronic 670G
In total, 19 studies were included: 11 real-world studies (Table 1 in the Supplementary Information); five trials; two pilot studies; and one analysis of trial data (Table 2 in the Supplementary Information) [35–53]. Thirteen studies included participants under 18 years. Twelve of the studies were conducted in the United States of America (USA), two in Israel and the USA, two in Europe, two in Qatar, and one in Australia. The 670G AID system was in use for the following time periods: 1 month (two studies); 3 months (11 studies); 6 months (four studies); 1 year (two studies).
Medtronic 780G
A total of eight studies were included (Table 3 in the Supplementary Information): five trials and three real-world studies [54–61]. Three included participants under 18 years old. One study was conducted in Spain, one in France, two in Italy, one in New Zealand, one in the USA, and two multicentre studies involving Belgium, the Netherlands, Finland, Italy, Qatar, and the UK and involving France, Germany, and the UK, respectively. The studies were of a varied duration: 4 weeks (two studies); 8 weeks (one study); 12 weeks (one study); 3 months (one study); 6 months of use (one study).
Control-IQ
In total, 11 studies were included (Table 4 in the Supplementary Information), one of which was a pilot study, five were trials, two were analyses of trial data, two were real-world studies, and one was an analysis of real-world data [23, 62–71]. Eight of the studies included participants under 18 years old. Ten were conducted in the USA and one in France. The duration of the studies varied from 4 weeks (two studies) to 7 weeks (one study), 3 months (one study), 6 months (three studies), 7 months (one study), 9 months (one study), and 1 year (two studies).
CamAPS FX
A total of 14 studies were included (Table 5 in the Supplementary Information): 11 trials, two analyses of trial data, and one real-world study [10, 72–84]. Four of the studies included participants under 18 years old, one included only participants over 60 years old, and two of the studies included pregnant women. Six of the studies were conducted in the UK, seven in both the UK and Europe, and one in the UK and USA. The duration of the studies varied from 4 weeks (six studies) to 6 weeks (two studies with two 3-week crossover arms), 8 weeks (one study); 12 weeks (three studies), 6 months (one study), and 8 months (one study).
DBLG1
Of the three studies included, one was a real-world study and two were trials (Table 6 in the Supplementary Information). One of the studies included children, and all six of the studies were conducted in France. All studies were greater than 4 weeks in duration: one real-world study where the AID system was used for 6 months and two trials where the AID system was used for 12–13 weeks [26, 33, 85].
DBLHU
Only one study pertaining to the DBLHU was included in the systematic review—a trial with an adult population conducted in France (Table 6 in the Supplementary Information) [29]. One of its two crossover periods was 4 weeks dedicated to DBLHU use. This study found that TIR was higher with DBLHU (73.3% ± 1.7%) compared with a Predictive Low Glucose Suspend (PLGS) system (43.5% ± 1.7%; P < 0.0001) [29]. No device-related adverse events occurred [29]. The study was limited by its very small sample size (n = 5) [29].
Omnipod 5
Of the three studies included, two were trials and one was a real-world study (Table 7 in the Supplementary Information) [32, 86, 87]. Two of the three included participants under 18 years old, and all three were conducted in North America: two in the USA and one in Canada. The duration of the studies varied from 3 months (one study) to 4 months (one study) and 6 months (one study).
Psychosocial Outcomes
A total of 23 studies were identified in the literature search as having psychosocial endpoints (Table 8 in the Supplementary Information) [23, 29, 38, 41, 44, 66, 67, 76, 83, 88–101]. These were analysed separately to the 59 papers included in the systematic review, although eight of the 23 studies were also featured in the systematic review with a focus on their glycaemic endpoints. Of the 23 studies, seven assessed the 670G, two assessed the 780G, five assessed the Control-IQ, eight assessed the CamAPS FX, and one assessed the DBLHU.
Discussion
Findings
Findings suggest that HCL systems are generally safe to use and improve users’ TIR without increasing hypoglycaemia. The Omnipod and Diabeloop systems have relatively little published literature but are comparatively newer than the other AID systems explored. In contrast, the 670G, the first commercial hybrid AID system, currently has the greatest amount of evidence regarding its performance.
Although more studies are needed, psychosocial outcomes with these systems have thus far been generally positive, with no suggestion that AID systems worsen psychosocial outcomes, and in some instances AID systems have demonstrated an improvement in psychosocial outcomes, such as satisfaction.
Implications
The majority of existing evidence regarding the performance of commercial AID systems has demonstrated their effectiveness and safety within the setting of pilot and feasibility studies and trials. Real-world evidence has largely come from insurance-driven systems, and this may alter the characteristics of the participants, who may come from a higher socio-economic status as compared to publicly funded systems and therefore have higher levels of health and digital literacy as well as engagement with self-management.
People with poor baseline control are typically underrepresented in existing literature about AID systems, with eligibility criteria from studies across the different systems typically excluding participants with a high HbA1c and those with a recent history of severe hypoglycaemia or DKA [24, 26, 49, 52, 67, 79].
Improvement of TIR with HCL systems is an important finding, as it has been found that for every 10% absolute change in TIR, there is a 0.8% (9 mmol/mol) change in HbA1c [102]. This is significant, as lower HbA1c levels are correlated with a reduced risk of complications from diabetes [103]. Further study is needed to ascertain whether improvements in TIR with HCL systems are sustained over time.
Strengths and Limitations
The strengths of this review include a comprehensive analysis of the evidence relating to commercial HCL systems with an objective, replicable methodology. At present there is no recent systematic review on commercial AID systems and hence this work may provide a valuable addition to the understanding of HCL systems.
However, there are some limitations to this systematic review. Many of the participants in the studies included had optimal baseline TIR and HbA1c and may have been of high socioeconomic status. Furthermore, the majority of the studies were conducted in the USA, so the results may be less generalisable to different healthcare systems or populations with different demographics. Due to the differences in study designs and trial populations between the various AID systems, it was not possible to conclusively determine differences between them.
Moreover, a meta-analysis was not conducted, and statistical tests were not used, as the broad inclusion criteria and heterogeneity of the included papers meant that this was not possible. Hence, it was also difficult to compare the performance of different systems with regard to improvements in time in range. It should also be noted that HbA1c was not used as an outcome in some studies due to their durations being less than 3 months. It is also possible that duplication of data may have occurred as a result of individual data being replicated in different studies.
As search terms specific to psychosocial studies were not included in the literature search, studies with psychosocial endpoints may have been missed inadvertently. Many studies included psychosocial outcomes, although many of these did not have sufficient sample sizes or sufficient duration for a statistical analysis of their results, meaning that there is a limit to the conclusions that can be drawn from the analysis of these papers. There was also a lot of heterogeneity in how psychosocial outcomes are measured and reported, with no international consensus on how to measure these in technology studies.
Another limitation of the review is that most of the studies were affiliated with HCL system companies; many studies received industry funding, with some authors being company employees, receiving grants during the studies, or owning shares in the company. Whilst in the vast majority of cases the companies were not involved in the study design or the writing of the manuscript, this was not always the case.
Recommendations
Future studies should include more diverse populations, with a greater range of ages, ethnicities, and socioeconomic statuses. More research is also needed on the performance of HCL systems in people with poor baseline HbA1c and TIR to provide a more representative intervention effect size.
As newer commercial HCL systems are developed, more independent evaluations are needed for comparisons between the different systems, in addition to more real-world studies, studies that are longer in duration, and independently financed studies.
Finally, meta-analyses, cost-effectiveness analyses, and further research on the effects of HCL systems on psychosocial outcomes such as quality of life, diabetes-related distress, diabetes burden, and fear of hypoglycaemia are needed.
Conclusions
The results of this systematic review demonstrate that commercial HCL systems can be used effectively to improve TIR in type 1 diabetes, including in real-world settings. Findings further support the efficacy of commercial AID systems in improving glycaemic control and exemplify their safety by showing that they can be used without increasing the incidence of severe hypoglycaemia. More real-world studies are needed, particularly with regard to more diverse participant populations and for comparing recent commercial HCL systems. Additional research is needed to evaluate differences between HCL systems and the cost-effectiveness and psychosocial impact of these systems so that their role in T1D management can be further established.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
No specific funding has been received related to the publication of this article.
Author Contributions
Sufyan Hussain designed the study. Sofia Peacock conducted the analysis. Sofia Peacock and Sufyan Hussain co-authored the first draft of the manuscript. Isolda Frizelle supported further analysis and a further review of the manuscript. All authors critically reviewed and approved the final version of the manuscript. Sufyan Hussain is the guarantor of the work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures
Sufyan Hussain is a recipient of a Medical Research Council Clinical Academic Partnership award (MR/W030004/1). Sofia Peacock and Isolda Frizelle have no conflicts of interest to declare.
Compliance and Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data availability
Datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request from qualified researchers.
References
- 1.Ramli R, Reddy M, Oliver N. Artificial pancreas: current progress and future outlook in the treatment of type 1 diabetes. Drugs. 2019;79:1089–1101. doi: 10.1007/s40265-019-01149-2. [DOI] [PubMed] [Google Scholar]
- 2.Castle JR, DeVries JH, Kovatchev B. Future of automated insulin delivery systems. Diabetes Technol Ther. 2017;19:S67–S72. doi: 10.1089/dia.2017.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jennings P, Hussain S. Do-it-yourself artificial pancreas systems: a review of the emerging evidence and insights for healthcare professionals. J Diabetes Sci Technol. 2019 doi: 10.1177/1932296819894296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.NHS Digital. National Diabetes Audit, 2017–18. Report 1: Care processes and treatment targets, full report 2019, England and Wales, 13th June 2019. Leeds: NHS Digital; 2019.
- 5.Kesavadev J, Saboo B, Krishna MB, Krishnan G. Evolution of insulin delivery devices: from syringes, pens, and pumps to DIY artificial pancreas. Diabetes Ther. 2020;11:1251–1269. doi: 10.1007/s13300-020-00831-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weisman A, Bai JW, Cardinez M, Kramer CK, Perkins BA. Effect of artificial pancreas systems on glycaemic control in patients with type 1 diabetes: a systematic review and meta-analysis of outpatient randomised controlled trials. Lancet Diabetes Endocrinol. 2017;5:501–512. doi: 10.1016/S2213-8587(17)30167-5. [DOI] [PubMed] [Google Scholar]
- 7.Bekiari E, Kitsios K, Thabit H, Tauschmann M, Athanasiadou E, Karagiannis T, Haidich AB, Hovorka R, Tsapas A. Artificial pancreas treatment for outpatients with type 1 diabetes: systematic review and meta-analysis. BMJ (Online) 2018 doi: 10.1136/bmj.k1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown SA, Kovatchev BP, Raghinaru D, et al. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med. 2019;381:1707–1717. doi: 10.1056/NEJMoa1907863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tauschmann M, Allen JM, Wilinska ME, Thabit H, Stewart Z, Cheng P, Kollman C, Acerini CL, Dunger DB, Hovorka R. Day-and-night hybrid closed-loop insulin delivery in adolescents with type 1 diabetes: a free-living, randomized clinical trial. Diabetes Care. 2016;39:1168–74. [DOI] [PMC free article] [PubMed]
- 10.Thabit H, Tauschmann M, Allen JM, et al. Home use of an artificial beta cell in type 1 diabetes. N Engl J Med. 2015 doi: 10.1056/nejmoa1509351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saunders A, Messer LH, Forlenza GP. MiniMed 670G hybrid closed loop artificial pancreas system for the treatment of type 1 diabetes mellitus: overview of its safety and efficacy. Exp Rev Med Dev. 2019;16:845–853. doi: 10.1080/17434440.2019.1670639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lal RA, Maikawa CL, Lewis D, et al. Full closed loop open-source algorithm performance comparison in pigs with diabetes. Clin Transl Med. 2021 doi: 10.1002/ctm2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alexander CM, Amiel S, Beck R, et al. Need for regulatory change to incorporate beyond A1C glycemic metrics. Diabetes Care. 2018 doi: 10.2337/dci18-0010. [DOI] [PubMed] [Google Scholar]
- 14.Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the International Consensus on Time in Range. Diabetes Care. 2019;42:1593–603. [DOI] [PMC free article] [PubMed]
- 15.Gabbay MAL, Rodacki M, Calliari LE, et al. Time in range: a new parameter to evaluate blood glucose control in patients with diabetes. Diabetol Metab Syndr. 2020 doi: 10.1186/s13098-020-00529-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braune K, Lal RA, Petruželková L, et al. Open-source automated insulin delivery: international consensus statement and practical guidance for health-care professionals. Lancet Diabetes Endocrinol. 2022 doi: 10.1016/S2213-8587(21)00267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burnside MJ, Lewis DM, Crocket HR, et al. Open-source automated insulin delivery in type 1 diabetes. N Engl J Med. 2022;387:869–881. doi: 10.1056/NEJMoa2203913. [DOI] [PubMed] [Google Scholar]
- 18.Knoll C, Peacock S, Wäldchen M, Cooper D, Aulakh SK, Raile K, Hussain S, Braune K. Real-world evidence on clinical outcomes of people with type 1 diabetes using open-source and commercial automated insulin dosing systems: a systematic review. Diabet Med. 2022 doi: 10.1111/dme.14741. [DOI] [PubMed] [Google Scholar]
- 19.Beck RW, Bergenstal RM, Riddlesworth TD, Kollman C, Li Z, Brown AS, Close KL. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019 doi: 10.2337/dc18-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schliess F, Heise T, Benesch C, et al. Artificial pancreas systems for people with type 2 diabetes: conception and design of the European CLOSE Project. J Diabetes Sci Technol. 2019 doi: 10.1177/1932296818803588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall DC, Holloway M, Korer M, Woodman J, Brackenridge A, Hussain S. Do-it-yourself artificial pancreas systems in type 1 diabetes: perspectives of two adult users, a caregiver and three physicians. Diabetes Ther. 2019 doi: 10.1007/s13300-019-00679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sherwood JS, Russell SJ, Putman MS. New and emerging technologies in type 1 diabetes. Endocrinol Metab Clin N Am. 2020;49:667–678. doi: 10.1016/j.ecl.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pinsker JE, Müller L, Constantin A, Leas S, Manning M, McElwee Malloy M, Singh H, Habif S. Real-world patient-reported outcomes and glycemic results with initiation of control-IQ technology. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2020.0388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forlenza GP, Buckingham BA, Brown SA, et al. First outpatient evaluation of a tubeless automated insulin delivery system with customizable glucose targets in children and adults with type 1 diabetes. Diabetes Technol Ther. 2021 doi: 10.1089/dia.2020.0546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Benhamou PY, Huneker E, Franc S, Doron M, Charpentier G. Customization of home closed-loop insulin delivery in adult patients with type 1 diabetes, assisted with structured remote monitoring: the pilot WP7 Diabeloop study. Acta Diabetol. 2018 doi: 10.1007/s00592-018-1123-1. [DOI] [PubMed] [Google Scholar]
- 26.Benhamou PY, Franc S, Reznik Y, et al. Closed-loop insulin delivery in adults with type 1 diabetes in real-life conditions: a 12-week multicentre, open-label randomised controlled crossover trial. Lancet Digit Health. 2019 doi: 10.1016/S2589-7500(19)30003-2. [DOI] [PubMed] [Google Scholar]
- 27.Quemerais MA, Doron M, Dutrech F, et al. Preliminary evaluation of a new semi-closed-loop insulin therapy system over the prandial period in adult patients with type 1 diabetes: the WP6.0 diabeloop study. J Diabetes Sci Technol. 2014 doi: 10.1177/1932296814545668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boughton CK, Hovorka R. New closed-loop insulin systems. Diabetologia. 2021 doi: 10.1007/s00125-021-05391-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benhamou PY, Lablanche S, Vambergue A, Doron M, Franc S, Charpentier G. Patients with highly unstable type 1 diabetes eligible for islet transplantation can be managed with a closed-loop insulin delivery system: a series of N-of-1 randomized controlled trials. Diabetes Obes Metab. 2021 doi: 10.1111/dom.14214. [DOI] [PubMed] [Google Scholar]
- 30.Tubiana-Rufi N, Schaepelynck P, Franc S, et al. Practical implementation of automated closed-loop insulin delivery: a French position statement. Diabetes Metab. 2020 doi: 10.1016/j.diabet.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Cobry EC, Berget C, Messer LH, Forlenza GP. Review of the Omnipod®5 automated glucose control system powered by Horizon™ for the treatment of type 1 diabetes. Ther Deliv. 2020 doi: 10.4155/tde-2020-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown SA, Forlenza GP, Bode BW, et al. Multicenter trial of a tubeless, on-body automated insulin delivery system with customizable glycemic targets in pediatric and adult participants with type 1 diabetes. Diabetes Care. 2021 doi: 10.2337/dc21-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amadou C, Franc S, Benhamou P-Y, Lablanche S, Huneker E, Charpentier G, Penfornis A. Diabeloop DBLG1 closed-loop system enables patients with type 1 diabetes to significantly improve their glycemic control in real-life situations without serious adverse events: 6-month follow-up. Diabetes Care. 2021;44:844–6. [DOI] [PubMed]
- 34.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Petrovski G, al Khalaf F, Campbell J, Umer F, Almajaly D, Hamdan M, Hussain K. One-year experience of hybrid closed-loop system in children and adolescents with type 1 diabetes previously treated with multiple daily injections: drivers to successful outcomes. Acta Diabetol. 2020 doi: 10.1007/s00592-020-01607-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Salehi P, Roberts AJ, Kim GJ. Efficacy and safety of real-life usage of MiniMed 670G automode in children with type 1 diabetes less than 7 years old. Diabetes Technol Ther. 2019 doi: 10.1089/dia.2019.0123. [DOI] [PubMed] [Google Scholar]
- 37.Stone MP, Agrawal P, Chen X, Liu M, Shin J, Cordero TL, Kaufman FR. Retrospective analysis of 3-month real-world glucose data after the minimed 670G system commercial launch. Diabetes Technol Ther. 2018 doi: 10.1089/dia.2018.0202. [DOI] [PubMed] [Google Scholar]
- 38.Beato-Víbora PI, Gallego-Gamero F, Lázaro-Martín L, del Romero-Pérez M. Prospective analysis of the impact of commercialized hybrid closed-loop system on glycemic control, glycemic variability, and patient-related outcomes in children and adults: a focus on superiority over predictive low-glucose suspend technology. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2019.0400. [DOI] [PubMed] [Google Scholar]
- 39.Akturk HK, Giordano D, Champakanath A, Brackett S, Garg S, Snell-Bergeon J. Long-term real-life glycaemic outcomes with a hybrid closed-loop system compared with sensor-augmented pump therapy in patients with type 1 diabetes. Diabetes Obes Metab. 2020 doi: 10.1111/dom.13933. [DOI] [PubMed] [Google Scholar]
- 40.Usoh CO, Johnson CP, Speiser JL, Bundy R, Dharod A, Aloi JA. Real-world efficacy of the hybrid closed-loop system. J Diabetes Sci Technol. 2021 doi: 10.1177/1932296820985103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lal RA, Basina M, Maahs DM, Hood K, Buckingham B, Wilson DM. One year clinical experience of the first commercial hybrid closed-loop system. Diabetes Care. 2019 doi: 10.2337/dc19-0855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lepore G, Scaranna C, Corsi A, Dodesini AR, Trevisan R. Switching from suspend-before-low insulin pump technology to a hybrid closed-loop system improves glucose control and reduces glucose variability: a retrospective observational case-control study. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2019.0302. [DOI] [PubMed] [Google Scholar]
- 43.Faulds ER, Zappe J, Dungan KM. Real-world implications of hybrid close loop (HCl) insulin delivery system. Endocr Pract. 2019 doi: 10.4158/EP-2018-0515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berget C, Messer LH, Vigers T, Frohnert BI, Pyle L, Wadwa RP, Driscoll KA, Forlenza GP. Six months of hybrid closed loop in the real-world: an evaluation of children and young adults using the 670G system. Pediatr Diabetes. 2020 doi: 10.1111/pedi.12962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duffus SH, al Ta’ani Z, Slaughter JC, Niswender KD, Gregory JM. Increased proportion of time in hybrid closed-loop “auto mode” is associated with improved glycaemic control for adolescent and young patients with adult type 1 diabetes using the MiniMed 670G insulin pump. Diabetes Obes Metab. 2020 doi: 10.1111/dom.13912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Petrovski G, al Khalaf F, Campbell J, Fisher H, Umer F, Hussain K. 10-day structured initiation protocol from multiple daily injection to hybrid closed-loop system in children and adolescents with type 1 diabetes. Acta Diabetol. 2020. 10.1007/s00592-019-01472-w. [DOI] [PMC free article] [PubMed]
- 47.Hsu L, Buckingham B, Basina M, Ekhlaspour L, von Eyben R, Wang J, Lal RA. Fast-acting insulin aspart use with the MiniMedTM670G system. Diabetes Technol Ther. 2021 doi: 10.1089/dia.2020.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Forlenza GP, Pinhas-Hamiel O, Liljenquist DR, et al. Safety evaluation of the MiniMed 670G system in children 7–13 years of age with type 1 diabetes. Diabetes Technol Ther. 2019 doi: 10.1089/dia.2018.0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garg SK, Weinzimer SA, Tamborlane W, et al. Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Diabetes Technol Ther. 2017 doi: 10.1089/dia.2016.0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Messer LH, Forlenza GP, Sherr JL, Wadwa RP, Buckingham BA, Weinzimer SA, Maahs DM, Slover RH. Optimizing hybrid closed-loop therapy in adolescents and emerging adults using the Mini Med 670G system. Diabetes Care. 2018. 10.2337/dc17-1682. [DOI] [PMC free article] [PubMed]
- 51.McAuley SA, Lee MH, Paldus B, et al. Six months of hybrid closed-loop versus manual insulin delivery with fingerprick blood glucose monitoring in adults with type 1 diabetes: a randomized controlled trial. Diabetes Care. 2020 doi: 10.2337/dc20-1447. [DOI] [PubMed] [Google Scholar]
- 52.Bergenstal RM, Nimri R, Beck RW, et al. A comparison of two hybrid closed-loop systems in adolescents and young adults with type 1 diabetes (FLAIR): a multicentre, randomised, crossover trial. Lancet. 2021 doi: 10.1016/S0140-6736(20)32514-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forlenza GP, Ekhlaspour L, DiMeglio LA, et al. Glycemic outcomes of children 2–6 years of age with type 1 diabetes during the pediatric MiniMed™ 670G system trial. Pediatr Diabetes. 2022 doi: 10.1111/pedi.13312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Collyns O, Meier R, Betts Z, et al. 199-OR: improved glycemic outcomes with medtronic Minimed advanced hybrid closed-loop delivery: results from a randomized crossover trial comparing automated insulin delivery with predictive low glucose suspend in people with type 1 diabetes. Diabetes. 2020 doi: 10.2337/db20-199-or. [DOI] [PubMed] [Google Scholar]
- 55.Pintaudi B, Gironi I, Nicosia R, Meneghini E, Disoteo O, Mion E, Bertuzzi F. Minimed Medtronic 780G optimizes glucose control in patients with type 1 diabetes mellitus. Nutr Metab Cardiovasc Dis. 2022;32:1719–1724. doi: 10.1016/j.numecd.2022.03.031. [DOI] [PubMed] [Google Scholar]
- 56.Beato-Víbora PI, Gallego-Gamero F, Ambrojo-López A, Gil-Poch E, Martín-Romo I, Arroyo-Díez FJ. Amelioration of user experiences and glycaemic outcomes with an advanced hybrid closed loop system in a real-world clinical setting. Diabetes Res Clin Pract. 2021 doi: 10.1016/j.diabres.2021.108986. [DOI] [PubMed] [Google Scholar]
- 57.Schiaffini R, Deodati A, Nicoletti MC, et al. Comparison of two advanced hybrid closed loop in a pediatric population with type 1 diabetes: a real-life observational study. Acta Diabetol. 2022;59:959–964. doi: 10.1007/s00592-022-01886-z. [DOI] [PubMed] [Google Scholar]
- 58.Thivolet C, Gaudilliere M, Villar Fimbel S, Bendelac N, Mestre B, Protsenko N, Brunot S, Nicolino M. Hybrid closed loop improved glucose control compared to sensor-augmented pumps in outpatients with type 1 diabetes in real-life conditions with telehealth monitoring. Acta Diabetol. 2022;59:395–401. doi: 10.1007/s00592-021-01820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.da Silva J, Lepore G, Battelino T, Arrieta A, Castañeda J, Grossman B, Shin J, Cohen O. Real-world performance of the MiniMed™ 780G system: first report of outcomes from 4120 users. Diabetes Technol Ther. 2022;24:113–119. doi: 10.1089/dia.2021.0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Carlson AL, Sherr JL, Shulman DI, et al. Safety and glycemic outcomes during the MiniMed™ advanced hybrid closed-loop system pivotal trial in adolescents and adults with type 1 diabetes. Diabetes Technol Ther. 2022;24:178–189. doi: 10.1089/dia.2021.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Choudhary P, Kolassa R, Keuthage W, et al. Advanced hybrid closed loop therapy versus conventional treatment in adults with type 1 diabetes (ADAPT): a randomised controlled study. Lancet Diabetes Endocrinol. 2022;10:720–731. doi: 10.1016/S2213-8587(22)00212-1. [DOI] [PubMed] [Google Scholar]
- 62.Kanapka LG, Wadwa RP, Breton MD, et al. Extended use of the control-IQ closed-loop control system in children with type 1 diabetes. Diabetes Care. 2021 doi: 10.2337/dc20-1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.O’Malley G, Messer LH, Levy C, et al. Clinical management and pump parameter adjustment of the control-IQ closed-loop control system: results from a 6-month multicenter randomized clinical trial. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2020.0472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brown SA, Beck RW, Raghinaru D, et al. Glycemic outcomes of use of CLC versus PLGS in type 1 diabetes: a randomized controlled trial. Diabetes Care. 2020;43:1822–8. [DOI] [PMC free article] [PubMed]
- 65.Isganaitis E, Raghinaru D, Ambler-Osborn L, et al. Closed-loop insulin therapy improves glycemic control in adolescents and young adults: outcomes from the International Diabetes Closed-Loop Trial. Diabetes Technol Ther. 2021 doi: 10.1089/dia.2020.0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bisio A, Brown SA, McFadden R, et al. Sleep and diabetes-specific psycho-behavioral outcomes of a new automated insulin delivery system in young children with type 1 diabetes and their parents. Pediatr Diabetes. 2020 doi: 10.1111/pedi.13164. [DOI] [PubMed] [Google Scholar]
- 67.Bisio A, Gonder-Frederick L, McFadden R, Cherñavvsky D, Voelmle M, Pajewski M, Yu P, Bonner H, Brown SA. The impact of a recently approved automated insulin delivery system on glycemic, sleep, and psychosocial outcomes in older adults with type 1 diabetes: a pilot study. J Diabetes Sci Technol. 2021 doi: 10.1177/1932296820986879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Breton MD, Kovatchev BP. One year real-world use of the control-IQ advanced hybrid closed-loop technology. Diabetes Technol Ther. 2021;23:601–608. doi: 10.1089/dia.2021.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Akturk HK, Snell-Bergeon J, Shah VN. Efficacy and safety of tandem control IQ without user-initiated boluses in adults with uncontrolled type 1 diabetes. Diabetes Technol Ther. 2022;24:779–783. doi: 10.1089/dia.2022.0162. [DOI] [PubMed] [Google Scholar]
- 70.Renard E, Tubiana-Rufi N, Bonnemaison E, et al. Outcomes of hybrid closed-loop insulin delivery activated 24/7 versus evening and night in free-living prepubertal children with type 1 diabetes: a multicentre, randomized clinical trial. Diabetes Obes Metab. 2022;24:511–521. doi: 10.1111/dom.14605. [DOI] [PubMed] [Google Scholar]
- 71.Ekhlaspour L, Raghinaru D, Forlenza GP, et al. Outcomes in pump- and CGM-baseline use subgroups in the International Diabetes Closed-Loop (iDCL) Trial. J Diabetes Sci Technol. 2022:193229682210893. [DOI] [PMC free article] [PubMed]
- 72.Boughton CK, Hartnell S, Thabit H, et al. Hybrid closed-loop glucose control with faster insulin aspart compared with standard insulin aspart in adults with type 1 diabetes: a double-blind, multicentre, multinational, randomized, crossover study. Diabetes Obes Metab. 2021 doi: 10.1111/dom.14355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tauschmann M, Allen JM, Nagl K, et al. Home use of day-and-night hybrid closed-loop insulin delivery in very young children: a multicenter, 3-week, randomized trial. Diabetes Care. 2019 doi: 10.2337/dc18-1881. [DOI] [PubMed] [Google Scholar]
- 74.Ruan Y, Bally L, Thabit H, et al. Hypoglycaemia incidence and recovery during home use of hybrid closed-loop insulin delivery in adults with type 1 diabetes. Diabetes Obes Metab. 2018 doi: 10.1111/dom.13304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bally L, Thabit H, Ruan Y, et al. Bolusing frequency and amount impacts glucose control during hybrid closed-loop. Diabet Med. 2018 doi: 10.1111/dme.13436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tauschmann M, Bally HTL, Allen JM, et al. Closed-loop insulin delivery in suboptimally controlled type 1 diabetes: a multicentre, 12-week randomised trial. Yearb Paediatr Endocrinol. 2019 doi: 10.1530/ey.16.10.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tauschmann M, Allen JM, Wilinska ME, Thabit H, Acerini CL, Dunger DB, Hovorka R. Home use of day-and-night hybrid closed-loop insulin delivery in suboptimally controlled adolescents with type 1 diabetes: a 3-week, free-living, randomized crossover trial. Diabetes Care. 2016 doi: 10.2337/dc16-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bally L, Thabit H, Kojzar H, et al. Day-and-night glycaemic control with closed-loop insulin delivery versus conventional insulin pump therapy in free-living adults with well controlled type 1 diabetes: an open-label, randomised, crossover study. Lancet Diabetes Endocrinol. 2017 doi: 10.1016/S2213-8587(17)30001-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thabit H, Lubina-Solomon A, Stadler M, et al. Home use of closed-loop insulin delivery for overnight glucose control in adults with type 1 diabetes: a 4-week, multicentre, randomised crossover study. Lancet Diabetes Endocrinol. 2014 doi: 10.1016/S2213-8587(14)70114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Stewart ZA, Wilinska ME, Hartnell S, O’Neil LK, Rayman G, Scott EM, Barnard K, Farrington C, Hovorka R, Murphy HR. Day-and-night closed-loop insulin delivery in a broad population of pregnant women with type 1 diabetes: A randomized controlled crossover trial. Diabetes Care. 2018 doi: 10.2337/dc17-2534. [DOI] [PubMed] [Google Scholar]
- 81.Stewart ZA, Wilinska ME, Hartnell S, et al. Closed-loop insulin delivery during pregnancy in women with type 1 diabetes. N Engl J Med. 2016 doi: 10.1056/nejmoa1602494. [DOI] [PubMed] [Google Scholar]
- 82.Ware J, Boughton CK, Allen JM, et al. Cambridge hybrid closed-loop algorithm in children and adolescents with type 1 diabetes: a multicentre 6-month randomised controlled trial. Lancet Digit Health. 2022;4:e245–e255. doi: 10.1016/S2589-7500(22)00020-6. [DOI] [PubMed] [Google Scholar]
- 83.Ng SM, Katkat N, Day H, Hubbard R, Quinn M, Finnigan L. Real-world prospective observational single-centre study: hybrid closed loop improves HbA1c, time-in-range and quality of life for children, young people and their carers. Diabet Med. 2022 doi: 10.1111/dme.14863. [DOI] [PubMed] [Google Scholar]
- 84.Boughton CK, Hartnell S, Thabit H, et al. Hybrid closed-loop glucose control compared with sensor augmented pump therapy in older adults with type 1 diabetes: an open-label multicentre, multinational, randomised, crossover study. Lancet Healthy Longev. 2022;3:e135–e142. doi: 10.1016/S2666-7568(22)00005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kariyawasam D, Morin C, Casteels K, et al. Hybrid closed-loop insulin delivery versus sensor-augmented pump therapy in children aged 6–12 years: a randomised, controlled, cross-over, non-inferiority trial. Lancet Digit Health. 2022;4:e158–e168. doi: 10.1016/S2589-7500(21)00271-5. [DOI] [PubMed] [Google Scholar]
- 86.Brown RE, Vienneau T, Aronson R. Canadian real-world outcomes of omnipod initiation in people with type 1 diabetes (COPPER study): evidence from the LMC Diabetes Registry. Diabet Med. 2021 doi: 10.1111/dme.14420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sherr JL, Bode BW, Forlenza GP, et al. Safety and glycemic outcomes with a tubeless automated insulin delivery system in very young children with type 1 diabetes: a single-arm multicenter clinical trial. Diabetes Care. 2022;45:1907–1910. doi: 10.2337/dc21-2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Messer LH, Berget C, Vigers T, Pyle L, Geno C, Wadwa RP, Driscoll KA, Forlenza GP. Real world hybrid closed-loop discontinuation: predictors and perceptions of youth discontinuing the 670G system in the first 6 months. Pediatr Diabetes. 2020 doi: 10.1111/pedi.12971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Grando MA, Bayuk M, Karway G, Corrette K, Groat D, Cook CB, Thompson B. Patient perception and satisfaction with insulin pump system: pilot user experience survey. J Diabetes Sci Technol. 2019 doi: 10.1177/1932296819843146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cobry EC, Hamburger E, Jaser SS. Impact of the hybrid closed-loop system on sleep and quality of life in youth with type 1 diabetes and their parents. Diabetes Technol Ther. 2020 doi: 10.1089/dia.2020.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cobry EC, Kanapka LG, Cengiz E, et al. Health-related quality of life and treatment satisfaction in parents and children with type 1 diabetes using closed-loop control. Diabetes Technol Ther. 2021 doi: 10.1089/dia.2020.0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Musolino G, Dovc K, Boughton CK, et al. Reduced burden of diabetes and improved quality of life: experiences from unrestricted day-and-night hybrid closed-loop use in very young children with type 1 diabetes. Pediatr Diabetes. 2019 doi: 10.1111/pedi.12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lawton J, Blackburn M, Rankin D, et al. Participants’ experiences of, and views about, daytime use of a day-and-night hybrid closed-loop system in real life settings: longitudinal qualitative study. Diabetes Technol Ther. 2019 doi: 10.1089/dia.2018.0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Barnard KD, Wysocki T, Ully V, et al. Closing the loop in adults, children and adolescents with suboptimally controlled type 1 diabetes under free living conditions: a psychosocial substudy. J Diabetes Sci Technol. 2017 doi: 10.1177/1932296817702656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Barnard KD, Wysocki T, Thabit H, et al. Psychosocial aspects of closed- and open-loop insulin delivery: closing the loop in adults with type 1 diabetes in the home setting. Diabet Med. 2015 doi: 10.1111/dme.12706. [DOI] [PubMed] [Google Scholar]
- 96.Abraham MB, de Bock M, Smith GJ, et al. Effect of a hybrid closed-loop system on glycemic and psychosocial outcomes in children and adolescents with type 1 diabetes. JAMA Pediatr. 2021;175:1227. doi: 10.1001/jamapediatrics.2021.3965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kudva YC, Laffel LM, Brown SA, et al. Patient-reported outcomes in a randomized trial of closed-loop control: the pivotal International Diabetes Closed-Loop Trial. Diabetes Technol Ther. 2021 doi: 10.1089/dia.2021.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gianini A, Suklan J, Skela-Savič B, Klemencic S, Battelino T, Dovc K, Bratina N. Patient reported outcome measures in children and adolescents with type 1 diabetes using advanced hybrid closed loop insulin delivery. Front Endocrinol (Lausanne) 2022 doi: 10.3389/fendo.2022.967725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Petrovski G, al Khalaf F, Campbell J, Day E, Almajaly D, Hussain K, Pasha M, Umer F, Hamdan M, Khalifa A. Glycemic outcomes of advanced hybrid closed loop system in children and adolescents with type 1 diabetes, previously treated with multiple daily injections (MiniMed 780G system in T1D individuals, previously treated with MDI) BMC Endocr Disord. 2022 doi: 10.1186/s12902-022-00996-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hood KK, Garcia-Willingham N, Hanes S, et al. Lived experience of CamAPS FX closed loop system in youth with type 1 diabetes and their parents. Diabetes Obes Metab. 2022;24:2309–2318. doi: 10.1111/dom.14815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.de Beaufort C, Schierloh U, Thankamony A, et al. Cambridge hybrid closed-loop system in very young children with type 1 diabetes reduces caregivers’ fear of hypoglycemia and improves their well-being. Diabetes Care. 2022;45:3050–3053. doi: 10.2337/dc22-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Vigersky RA, McMahon C. The relationship of hemoglobin A1C to time-in-range in patients with diabetes. Diabetes Technol Ther. 2019 doi: 10.1089/dia.2018.0310. [DOI] [PubMed] [Google Scholar]
- 103.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request from qualified researchers.