Abstract
The mental health of young people (YP) is a major public health concern that has worsened during the COVID-19 pandemic. Whilst engaging with culture and the arts may have mental health benefits there is a dearth of experimental research regarding the impact of online arts and culture on depression and anxiety in YP. In particular online interventions, which may improve accessibility.
Objective:
We aimed to compare a co-produced online intervention encompassing the diverse human stories behind art and artefacts, named Ways of Being (WoB), with a typical museum website, the Ashmolean (Ash) on negative affect (NA), positive affect (PA) and psychological distress (K10).
Methods:
In this parallel group RCT, 463 YP aged 16-24 were randomly assigned, 231 to WoB and 232 to Ash.
Results:
Over the intervention phase (an aggregate score including all post-allocation timepoints to day-five) a group difference was apparent in favour of WoB for NA (WoB-Ash n=448, NA -0.158, p=0.010) but no differences were detected for PA or K10 and differences were not detected at week six. Group differences in NA in favour of WoB were detected in specific subgroups, e.g. ethnic minorities and males. Across participants (from both groups) mean K10 and NA improved between baseline and six weeks despite increased COVID-19 restrictions. Trial recruitment was rapid, retention high and feedback positive with broad geographical, occupational and ethnic diversity.
Conclusions:
Online engagement with arts and culture has the potential to impact on mental health in a measurable way in YP with high unmet mental health needs.
Keywords: Depression, anxiety, youth, experimental medicine
Introduction
Three-quarters of mental health problems emerge before the age of 25, yet people aged 16–24 years are the least likely age group to seek help (Andrews et al., 2001; Olfson and Klerman, 1992). Mental health problems in young people (YP) have long-term sequelae throughout the lifespan (Kieling et al., 2011; Lewinsohn et al., 2000) with significant direct and indirect costs (Knapp et al., 2016). COVID-19 restrictions have disproportionately impacted on the lives of YP with evidence of higher rates of depression (Gray et al., 2020; Nochaiwong et al., 2021; Pierce et al., 2020; Williams et al., 2021). Some YP have been affected more than others, including marginalised groups such as ethnic minorities (Abramovich et al., 2021; Bray et al., 2021; Proto and Quintana-Domeque, 2021).
Only around 35% of YP with mental health problems seek professional help (Zachrisson et al., 2006), the main barriers being lack of recognition, lack of awareness and stigma (Gulliver et al., 2010; Radez et al., 2021a, 2021b; Rickwood and Braithwaite, 1994; Rickwood et al., 2007; Rowe et al., 2014; Stunden et al., 2020). Moreover, YP most in need of mental health support, such as ethnic minorities, are the least likely to seek help (Cauce et al., 2002; Gulliver et al., 2010; Oksanen et al., 2017; Rickwood et al., 2007; Rowe et al., 2014). Thus, there is a compelling need for evidence-based, accessible, acceptable and engaging resources to support the mental health of YP during and beyond the COVID-19 pandemic.
There is evidence that engagement with culture and the arts is good for mental health and well-being (Callinan and Coyne, 2020; Camic and Chatterjee, 2013; Coles and Harrison, 2018; Fancourt et al., 2021; Fancourt and Finn, 2019; Van Lith et al., 2013). The proposed mechanisms include emotional activation, aesthetic engagement, social interaction, cognitive stimulation, sensory activation and imagination (Callinan and Coyne, 2020; Coles and Harrison, 2018; Fancourt et al., 2019). However, some commentators have reservations about the potential broader benefits, citing major inequalities in access (Bourdieu, 1984; Brook, 2016; Brook and O’Brien, 2020) potentially serving to reinforce health inequalities.
There are significant research gaps regarding the impact of arts and culture on mental health. While many epidemiological studies have demonstrated associations between engagement with arts and culture and improved health and even longevity (Bygren et al., 1996; Cuypers et al., 2012; Johansson et al., 2001; Konlaan et al., 2000; Väänänen et al., 2009), most are confounded by the sociodemographic determinants of health (Browne Gott, 2020) such as income, which are positively associated both with positive health outcomes and engagement with culture and the arts. In addition, many qualitative studies have explored the relationship between arts and culture and mental health, predominantly in clinical populations (Ander et al., 2013; Coles and Harrison, 2018; Morse et al., 2022; Plumb, 2012; Stickley and Hui, 2012a, 2012b; Thomson et al., 2020; Todd et al., 2017). While this evidence base appears to be growing (Bungay and Clift, 2010; Camic and Chatterjee, 2013; Fancourt and Finn, 2019; Van Lith et al., 2013), people with the greatest mental health needs, such as YP, often have the poorest access to health services (Vijayaraghavan et al., 2012) and are underrepresented in clinical research.
We previously conducted a series of studies to identify the potential mental health benefits of engaging with online arts and culture on mental health. Previous research has used such broad definitions of online arts and culture that the mental health impact has been unclear (Browne Gott, 2020). We define online arts and culture as online resources from museums, theatres, art galleries, libraries, archives and natural heritage organisations (Syed Sheriff et al., 2021a) rather than broader definitions used by others which have included gaming, streamed and social media (NESTA, 2020).
We commenced a preregistered evidence synthesis (Syed Sheriff et al., 2020) of trials evaluating community resources including engagement with arts and culture on anxiety and depression. To date, we have screened 15,534 titles and abstracts and have found no trials evaluating the effectiveness of online arts and culture for depression and anxiety in YP.
We conducted an online survey of the self-reported benefits of engaging with online arts and culture which took place in the context of the first UK COVID-19 lockdown (Syed Sheriff et al., 2021a). In total, 1056 people completed the survey. A high proportion of participants reported engaging with online arts culture as being helpful for their mental health. Those under 25 years old were less likely to be regular users of online culture or to have increased their use during lockdown.
We then conducted a qualitative interview study, which is described in detail elsewhere (Syed Sheriff et al., 2022). In brief, individual semi-structured interviews were conducted with 13 participants aged 16–24 who were socio-demographically diverse and varied in their use of online arts and culture and mental health status. Participants were asked about the potential benefits of online arts and culture for mental health. Descriptions of themes and subthemes were returned to participants for comment. Participants described that the features of online arts and culture most likely to benefit mental health were diverse human stories and a variety of viewpoints, with which they could connect on a human level, bringing a sense of perspective and opportunities for reflection, learning, escapism, creativity, exploration and discovery. Perceived impacts on mental health included disruption of negative thought patterns, lifted mood and increased feelings of calm and proactivity.
Aims and objectives
The Online Active Community Engagement Proof of Principle Study (O-ACE POP) is a two-arm randomised controlled trial (RCT) comparing a co-produced online cultural experience named Ways of Being (WoB), encompassing the diverse human stories behind art and artefacts and a variety of alternative viewpoints, to a typical museum website (Ashmolean) on negative affect (NA), positive affect (PA) and psychological distress in YP. This proof-of-principle trial was designed to test impact over a short intervention phase for signal detection to determine the utility of developing this approach further. To the best of our knowledge, this is the first experimental study of online cultural experiences for mental health in YP and as such aimed to elucidate efficacy and potential mechanisms of action.
Methods
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects were approved by the University of Oxford Central University Research Ethics Committee (CUREC), approval reference number R70187/RE007.
Study design and participants
The design was a parallel-group RCT with a 1:1 allocation ratio, conducted entirely online. The trial was submitted to the trial registry in its current form prior to the first participant being recruited (official registration date shortly after this, but no substantive change in the planned trial; this reflects administration time at the trial registry and academic institution). The Trial Steering Committee included three Public and Patient Involvement (PPI) members aged 16–24, and met at planning and pre-recruitment phases and prior to completion. The protocol and SPIRIT checklist for this trial are described in detail elsewhere (Syed Sheriff et al., 2021b).
We included people aged 16–24 years in the United Kingdom or 18–24 if based overseas (due to local ethical guidance restricting the use of the term ‘competent youth’ to those aged 16–17 years located within the United Kingdom) and with access to a desktop or laptop computer running a recent browser (Edge or Chrome on Windows, and Safari or Chrome on a Mac). There were no exclusions according to current mental health status. We recruited people of the target age through social media (Facebook and Instagram), student organisations (e.g. Student Unions) and schools (e.g. via the online publication, The Day) with a link to Participant Information and e-consent procedures for those who fulfilled inclusion criteria and consented to entering their email address. Informed consent was obtained and recorded electronically from all participants prior to entering the trial.
Randomisation and masking
Participants were randomised using computer-generated random sequencing in blocks of six stratified by gender with an equal allocation ratio. Participants were allocated by a researcher blinded to all study data except gender during the entire randomisation and allocation procedure. The allocation was emailed to the participant with joining instructions and therefore the participants were aware of the name of the online cultural intervention to which they had been allocated but did not know which was the ‘control’ condition. The interventions and all measures were online and self-report and therefore blinding procedures for care providers and outcome assessors were not relevant. Baseline and outcome data remained blinded for all researchers and analysts throughout the intervention phase.
Procedures
Trial procedures were trialled on 11 volunteers and detailed feedback was taken prior to the trial to ensure the integrity of all procedures. Baseline and subsequent assessments were completed and stored securely in the Gorilla platform during the study period. The Gorilla Experiment Builder (www.gorilla.sc) is a cloud-based research platform that allows researchers to design and administer behavioural experiments online.
Consenting participants entered an online questionnaire including items for gender, ethnicity, isolation status, income, relationship status, use of online culture, education, current employment, current and previous mental health and COVID-19 status. Participants were then emailed a unique ID number and requested to complete a baseline assessment on a computer, including self-report measures and online tasks. They were then randomised to WoB or Ash.
Participants had the option of consenting to text messages to remind them to complete the twice-daily measures each day of the 3-day intervention phase. There was also an email reminder (and text message reminder for all those who consented) to all participants to complete the measures on exit of the intervention phase (day 5) and for the 6-week follow-up. In addition, participants were offered Amazon vouchers as a thank you for their time at day 5 and week 6.
Interventions
Co-production of the intervention occurred over an intense 3-month period (September–November 2020) in an iterative process involving small- and large-scale production, co-production sprints and refinement with constant feedback. Co-production was preceded by a stakeholder workshop with YP, service users above the target age range and museum curators, youth engagement and education officers. Throughout co-production, weekly meetings were attended with Imagineear (www.imagineear.com), a production company experienced in content creation and platform provision for museums and art galleries as well as health services.
Youth preference took precedence in the development of WoB. YP were involved in five workshops and gave regular feedback in groups or via direct messaging (zoom and email) with comments, edits, suggestions and viewpoints for the developing intervention. The 12 YP aged 16–24 involved in co-production were selected to represent a diversity of viewpoints and were recruited from youth PPI groups (three YP), volunteers from university staff and students with specific expertise, for example, one works in a voluntary role with young refugees (three YP) and a selection of those involved in the qualitative interview study (six YP).
Stages of co-production included selection of stories, generation of viewpoints, determination of audio-visual preferences, navigation and optimisation of the online platform. The co-production process revealed the importance of authenticity, diversity, accessible language and a rich tapestry of stories to encourage exploration and discovery. A more detailed description of the co-production process has been described previously (Adams et al., 2021) and will be described in more detail in a report (currently being co-produced with the YP) elsewhere.
The co-produced online intervention, called WoB, was designed to be entered at a time and place convenient to the individual on their own device. Introductory pages illustrated the features of WoB. A non-hierarchical menu page gave the choice of 11 diverse ‘stories’, each of which encompassed a visual and a title, e.g. ‘Being Ibrahim’. Once entered, these led into a long-form story (which could be listened to or read) interspersed with visual media and then further ‘deeper’ stories which were interconnected. Alongside the stories was a comments tool that enabled participants to add their own viewpoint to a variety of viewpoints prepopulated during co-production, enabling participants to express their responses anonymously which were then redisplayed within WoB. The features of WoB are illustrated in a video walk-through (www.youtube.com/watch?v=mQLFL4Tm-v8). A TIDieR checklist has been completed (see Supplementary Material 6).
Participants were requested to engage with WoB at least once a day for at least three consecutive days from the day following allocation, for around 30 minutes a day. The duration and intensity of the requested engagement was chosen in discussion with YP during co-production and trial planning to balance the content available on WoB with a realistic and non-onerous engagement requirement at sufficient dose to evaluate proof of principle over the intervention phase.
The Ashmolean Website (Ash) is a typical museum website owned by the Ashmolean Museum of Art and Archaeology at the University of Oxford. Participants who were allocated to Ash were directed towards the Ashmolean from Home webpage (https://ashmolean.org/ashmoleanfromhome). This section of the Ashmolean Website was specifically created as an online substitute for the museum visit and material curated by museum specialists with a focus on art movements or styles. Unlike WoB, the emphasis is on the objects themselves rather than human stories. Participants allocated to Ash were asked to engage with its content in line with the engagement requirement for WoB.
Outcomes
The primary outcomes were NA and PA, both measured via the Positive and Negative Affect Scale (PANAS) (Watson et al., 1988b), and psychological distress, measured via the Kessler Psychological Distress Scale (K10) (Kessler et al., 2002). The ‘intervention phase’ was an aggregate of scores at all time points post-allocation including day 5. The only other time point was at 6 weeks which was included to determine whether early differences in the performance of cognitive tasks predicted changes at 6 weeks (Syed Sheriff et al., 2021b). Therefore, intervention phase NA, PA and K10 are reported as the primary outcomes.
The PANAS is a widely used scale of emotion and comprises 20 items, 10 measuring NA, upset, afraid etc., on a Likert-type scale of 1 (very slightly) to 5 (extremely), and 10 measuring PA, excited, inspired etc. The PANAS was administered with reference to the previous 7 days at baseline and 6 weeks, the previous 3 days at day 5 and at that precise moment twice daily during the 3-day intervention period.
The NA scale is highly internally consistent, largely uncorrelated and stable. Low NA reflects a state of calmness and serenity. High NA is related to self-reported stress and difficulty coping with negative events. Lower scores reflect lower levels of NA. The PA scale is valid and reliable with high internal consistency. High PA is characterised by energy, concentration and engagement (Watson et al., 1988b). In this study, individual mean PA scores were used to indicate PA at each time point and individual mean NA scores were used to indicate NA at each time point.
Psychological distress was used to ascertain the level of anxiety and depressive symptoms at baseline, day 5 and 6 weeks. The K10 is one of the most widely used mental health screening instruments (Andrews and Slade, 2001) and demonstrates good properties with regard to validity, reliability (Andrews and Slade, 2001) and sensitivity to change (Perini et al., 2006). The K10 strongly discriminates between community cases and non-cases of mental disorders identified by a structured clinical interview (Kessler et al., 2002). The K10 was asked with reference to the previous 4 weeks at baseline and 6 weeks and the previous 3 days at day 5. Each item was rated on a 5-point Likert scale (1 = none of the time to 5 = all of the time) and scores added to a possible range of 10 to 50, with higher scores reflecting higher levels of distress (Andrews and Slade, 2001).
There was also a detailed feedback survey at 6 weeks based on the NIHR Research Experience checklist (www.nihr.ac.uk/documents/optimising-the-participant-in-research-experience-checklist/21378?diaryentryid=60465) (see Figure 1).
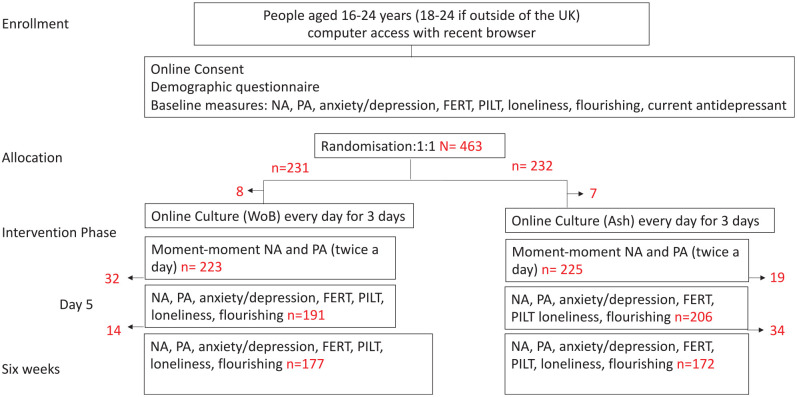
Figure 1.
Participant flow chart.
NA: Negative Affect, PA: Positive Affect, FERT: Facial Expression Recognition Task, PILT: Probabilistic Instrumental Learning Task
The analyses of the primary outcomes are reported here. Secondary outcomes are described elsewhere (Syed Sheriff et al., 2021b) and the analyses included in the Supplementary Files (Supplementary Material 1). The data and code underlying these analyses are available from https://www.glam.ox.ac.uk/oace-project. The analyses of cognitive measures and a full description of the embedded qualitative study will be reported separately.
Sample size calculation
We approximated the statistical power to detect a significant effect of WoB on PANAS scores by assuming an effect size of 0.3 standard deviations of group (WoB vs Ashmolean Website). With 200 participants in each group, and no pre-intervention differences, a Welch’s t test would have 85% probability of rejecting the null hypothesis under these parameters.
Statistical analysis
A descriptive analysis was performed for the whole population and each group (WoB and Ash). Categorical variables are described, presenting the numbers and frequency of each. Quantitative variables are described using usual positional and dispersion parameters.
We performed an intention-to-treat analysis to include all participants with any outcome data. Participants continued to be invited for assessment regardless of whether they used the allocated intervention. Missing item responses were not possible by design. Missing data, if any, happened was due to participants discontinuing with outcome assessments. However, data for timepoints prior to that were included in the multilevel model, so no additional methodological steps were required regarding missing data.
For primary outcomes (NA, PA and K10), we separately regressed the subscale means on baseline score (day 1 measurement) (Twisk et al., 2018), an indicator for Group (Ash/WoB), and contrast coded age group, sex, ethnicity (White/Other), relationship status (In/Not in relationship or other) and current antidepressant use (Yes/No). We also included time (Intervention phase [all time points post-allocation including day 5]/Week 6 follow-up) and its interactions with all other predictors in the model. We included random intercepts for participants. We performed a similar analysis for the K10 and secondary outcomes (flourishing and loneliness are reported in the supplementary analysis).
We conducted subgroup analyses based on age group (16–17 or 18–24), sex, ethnicity, baseline probable moderate-severe mental disorder, antidepressant use and previous regular use of online culture (more or less than once a month). We hypothesised that those with mental disorder at baseline, those not on antidepressants and regular users of culture would be more likely to demonstrate group differences. All analyses were conducted in the R programming language (R Core Team, 2019).
Changes to protocol
Many participants started the intervention following randomisation rather than after the second PANAS measurement (as per protocol) and therefore the baseline measurement only includes the baseline PANAS rather than the first two PANAS measurements.
Availability of data
The study data and coding used for the main analysis are available on the Open Science Framework https://osf.io/9wt8d/.
Results
Main findings
In total, 463 people aged 16–124 were randomised, 232 to Ash and 231 to WoB, 276 (60%) were female, 422 (91%) were 18–24 years old and 360 (78%) identified as White British, Irish or other. At baseline, 245 (52.9%) reported having a current mental disorder and 413 (89.2%) had clinically significant symptoms according to their K10 score (see Table 1).
Table 1.
Demographics.
| Characteristic | Overall, N = 463 a | Ash, N = 232 a | WoB, N = 231 a |
|---|---|---|---|
| Age | |||
| 16–17 | 41 (8.9%) | 15 (6.5%) | 26 (11%) |
| 18–24 | 422 (91%) | 217 (94%) | 205 (89%) |
| Gender | |||
| Female | 276 (60%) | 138 (59%) | 138 (60%) |
| Male | 179 (39%) | 90 (39%) | 89 (39%) |
| Other/prefer not to say | 8 (1.7%) | 4 (1.7%) | 4 (1.7%) |
| Ethnicity | |||
| Asian British (Indian Pakistani or Bangladeshi) | 33 (7.1%) | 18 (7.8%) | 15 (6.5%) |
| Black/Black British (Caribbean African or Other) | 22 (4.8%) | 11 (4.7%) | 11 (4.8%) |
| Chinese/Chinese British | 10 (2.2%) | 5 (2.2%) | 5 (2.2%) |
| Mixed race (Other) | 17 (3.7%) | 6 (2.6%) | 11 (4.8%) |
| Mixed race (White and Black/Black British) | 15 (3.2%) | 9 (3.9%) | 6 (2.6%) |
| Other/prefer not to say | 6 (1.3%) | 3 (1.3%) | 3 (1.3%) |
| White (British Irish or Other) | 360 (78%) | 180 (78%) | 180 (78%) |
| Occupation | |||
| At school | 48 (10%) | 23 (9.9%) | 25 (11%) |
| In full-time employment (not studying) | 113 (24%) | 64 (28%) | 49 (21%) |
| In part-time employment (not studying) | 84 (18%) | 45 (19%) | 39 (17%) |
| On furlough (not studying) | 14 (3.0%) | 4 (1.7%) | 10 (4.3%) |
| Other | 27 (5.8%) | 13 (5.6%) | 14 (6.1%) |
| Studying and not working | 113 (24%) | 56 (24%) | 57 (25%) |
| Studying and working | 64 (14%) | 27 (12%) | 37 (16%) |
| Relationship | |||
| In a relationship/Living with partner | 85 (18%) | 43 (19%) | 42 (18%) |
| In a relationship/Not living with partner | 146 (32%) | 74 (32%) | 72 (31%) |
| Other | 6 (1.3%) | 2 (0.9%) | 4 (1.7%) |
| Single | 226 (49%) | 113 (49%) | 113 (49%) |
| Household income | |||
| £16,000–£29,999 a year | 81 (17%) | 44 (19%) | 37 (16%) |
| £30,000–£59,999 a year | 144 (31%) | 67 (29%) | 77 (33%) |
| Less than £16,000 a year | 88 (19%) | 44 (19%) | 44 (19%) |
| More than £60,000 a year | 115 (25%) | 62 (27%) | 53 (23%) |
| Prefer not to say | 35 (7.6%) | 15 (6.5%) | 20 (8.7%) |
| OCC engagement frequency | |||
| Between once a month and once a year | 156 (34%) | 76 (33%) | 80 (35%) |
| More than once a month (but less than once a week) | 115 (25%) | 59 (25%) | 56 (24%) |
| Once a week or more | 123 (27%) | 62 (27%) | 61 (26%) |
| Rarely/Never (No more than once a year) | 69 (15%) | 35 (15%) | 34 (15%) |
| Current mental health | |||
| No | 218 (47%) | 114 (49%) | 104 (45%) |
| Yes | 245 (53%) | 118 (51%) | 127 (55%) |
| Current health | |||
| No | 393 (85%) | 202 (87%) | 191 (83%) |
| Yes | 70 (15%) | 30 (13%) | 40 (17%) |
| COVID-19 diagnosis | |||
| No | 367 (79%) | 190 (82%) | 177 (77%) |
| Suspected and recovered | 43 (9.3%) | 10 (4.3%) | 33 (14%) |
| Suspected and still ill | 22 (4.8%) | 11 (4.7%) | 11 (4.8%) |
| Yes diagnosed and recovered | 24 (5.2%) | 18 (7.8%) | 6 (2.6%) |
| Yes diagnosed and still ill | 7 (1.5%) | 3 (1.3%) | 4 (1.7%) |
| Isolation Status | |||
| I am leaving the house as normal | 64 (14%) | 31 (13%) | 33 (14%) |
| I am leaving the house for work/essential responsibilities but practising social distancing where possible | 183 (40%) | 87 (38%) | 96 (42%) |
| I am leaving the house only for essential supplies and daily exercise | 149 (32%) | 75 (32%) | 74 (32%) |
| I am not leaving the house at all and have no access to outside space | 22 (4.8%) | 14 (6.0%) | 8 (3.5%) |
| I am not leaving the house at all but have access to outside space (e.g. garden) | 45 (9.7%) | 25 (11%) | 20 (8.7%) |
| Antidepressant | |||
| No | 363 (78%) | 175 (75%) | 188 (81%) |
| Yes | 100 (22%) | 57 (25%) | 43 (19%) |
| Baseline mild MH b | |||
| No | 355 (77%) | 172 (74%) | 183 (79%) |
| Yes | 108 (23%) | 60 (26%) | 48 (21%) |
| Baseline moderate MH b | |||
| No | 327 (71%) | 167 (72%) | 160 (69%) |
| Yes | 136 (29%) | 65 (28%) | 71 (31%) |
| Baseline severe MH b | |||
| No | 294 (63%) | 146 (63%) | 148 (64%) |
| Yes | 169 (37%) | 86 (37%) | 83 (36%) |
n (%).
Mild, moderate and severe mental disorder: A score of 20–24 was defined as being consistent with probable mild disorder, 25–29 with a probable moderate disorder and 30 and over with a probable severe disorder.
Fifteen participants (eight from WoB and seven from Ash) dropped out after randomisation but prior to any outcome assessments and were therefore not included in the analyses. Overall, 349 (75%) completed assessments to 6 weeks. There was no difference between groups in the proportion of dropouts (Ash = 59, WoB = 55) (see Figure 1). Baseline mean K10 was non-significantly higher in trial completers (27.2, 95% confidence interval [CI] = [25.8, 28.0]) than non-completers (26.9, 95% CI = [26.6, 27.8]).
Of the 336 trial completers who reported location, 8 were located overseas and the others came from across regions of the United Kingdom including small towns, villages and rural areas (see Supplementary Materials 3 and 4, Location type and region). Imagineear set up a method for recording use of WoB using unique login ID numbers; however, it transpired that this did not log use reliably as it depended on the security settings of participants’ devices and therefore is not used in these analyses.
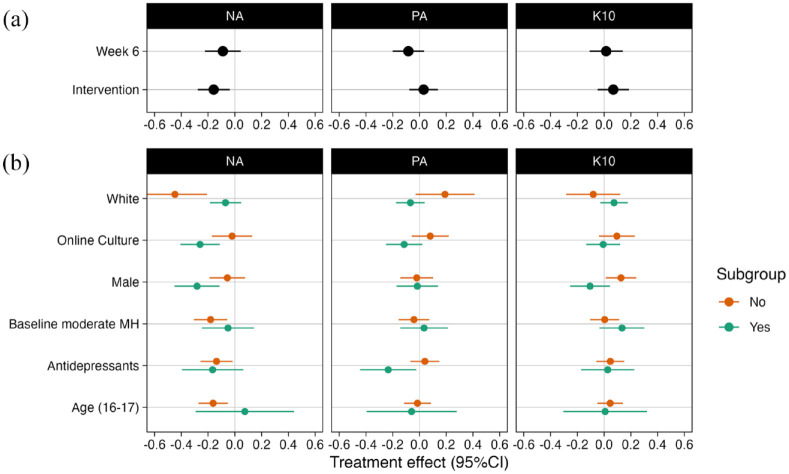
Group differences
NA was lower in the WoB group than in the Ash group during the intervention phase, which is an aggregate score including all time points’ post-allocation until day 5 (see Statistical analysis section). There were no group differences for PA or K10 during the intervention phase. Significant group differences were not detected for NA, PA or K10 at 6 weeks (see Table 2).
Table 2.
Group differences.
| Outcome | Contrast | Time | Estimate | SE | Lower CL | Upper CL | T ratio | p value | N |
|---|---|---|---|---|---|---|---|---|---|
| NA | WoB–Ash | Intervention | −0.158 | 0.061 | −0.278 | −0.038 | −2.592 | 0.010 | 448 |
| NA | WoB–Ash | Week 6 | −0.090 | 0.068 | −0.223 | 0.044 | −1.319 | 0.187 | 448 |
| PA | WoB–Ash | Intervention | 0.031 | 0.055 | −0.076 | 0.139 | 0.569 | 0.570 | 448 |
| PA | WoB–Ash | Week 6 | −0.083 | 0.060 | −0.200 | 0.034 | −1.387 | 0.166 | 448 |
| K10 | WoB–Ash | Intervention | 0.069 | 0.060 | −0.048 | 0.186 | 1.158 | 0.247 | 397 |
| K10 | WoB–Ash | Week 6 | 0.015 | 0.063 | −0.109 | 0.140 | 0.241 | 0.809 | 397 |
NA: negative affect; PA: positive affect.
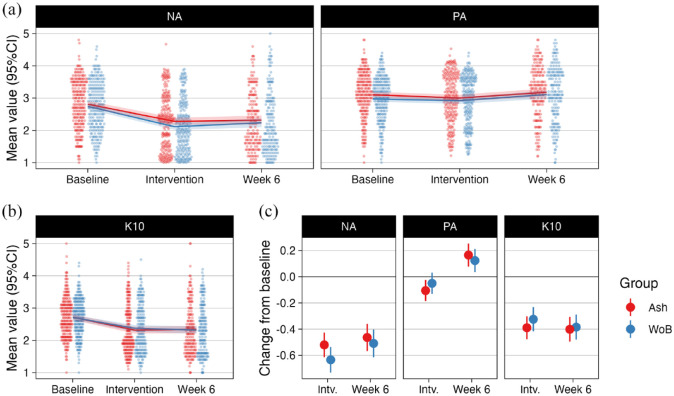
Changes over time
The K10 and NA reduced between baseline and the intervention phase and then remained significantly lower than baseline at 6 weeks in both groups (see Figure 2 and Supplementary Material 1, Table 2).
Figure 2.
Change in primary outcomes from baseline. (a) Mean negative (left) and positive affect (right) at baseline, during the intervention, and at week 6 follow-up. Lines with shades indicate group means and 95%CIs, points indicate individual participants. (b) Same as (a) but for the K10 scale. (c) Parameters indexing change from baseline for each group. Bars indicate 95%CIs. Intv. = Intervention.
Subgroup differences
For NA, the subgroup models indicated that there were statistically significant differences in NA in favour of WoB for the following subgroups, ethnic minorities, males, people aged 18–24, regular users of online culture, those who did not reach the threshold for a moderate–severe disorder at baseline and those not on antidepressants (see Figure 3).
Figure 3.
Subgroups analysis. (a) Group differences (WoB – Ash) during intervention and at week 6 follow-up for negative (left) and positive affect (middle), and K10 (right). (b) Group differences as (a) for different subgroups, but during intervention only..
Self-reported mental health and help-seeking
Of the 313 participants who had clinically significant symptoms at baseline and completed the 6-week follow-up, 22.4% (95% CI = [18.6, 27.3]) had never sought help, 17.3% (95% CI = [13.4, 21.9]) had only ever sought help from within their own friends and family and 32.2% (95% CI = [28.2, 38.7]) had sought help in two or more ways (other than family or friends) (see Supplementary Material 2, Help-seeking table).
Panel 1: Participant comments on Ways of Being.
‘the different variety of artists and the inclusivity, it made it feel, for me personally, because I’m transgender, it made me feel less alone that there was other people who were going through stuff like that so I would come away feeling very positive at the end of it’.
‘It was nice and refreshing to see so many different kinds of people, all presented together equally. And a lot of people I hadn’t heard of, I was really surprised I hadn’t ‘cause I’d studied those periods so it was very interesting’.
‘because it’s not in a therapy setting of someone telling you, this is how you should try and accept yourself and get better . . . I think seeing it in a more of an artistic setting with artists’ works. It took away the mental health focus and let me come to those conclusions by myself’.
‘it got me out of my own head’
‘I would compare it to art therapy but less demanding because it wasn’t forcing me to look inward to create, it was letting me explore other things. I think it was the removal from the self that was quite helpful’.
‘It was something I did at the end of the day and it took my mind off anything that happened during the day and I felt like I had done something to . . . a form of self-care’.
‘I really liked the voice. It was like a really nice calming tone to listen to’.
‘It was distracting because it was immersing me in something else which was positive and it was easy to focus on’
‘I would compare it to group therapy but less sad because it’s like you’ve come together to interpret something in a productive way’
‘I feel that the negative side of accessing content online is the isolation because you’re doing it by yourself. And the other people’s viewpoints kind of combatted that’.
‘because it was so well-made you felt kind of supported in a way’.
Feedback
The study was generally well received with the majority of 371 participants who completed the feedback questionnaire at 6 weeks agreeing or strongly agreeing with statements such as ‘I would consider taking part in research again’ and ‘Taking part was a positive experience’ and responses to online cultural resources were positive (see Supplementary Material 5, Research Feedback Table and Panel 1). Feedback specific to WoB was that participants exhausted the content before the end of the intervention phase and would have appreciated more material.
Discussion
Although it is generally thought that engagement with culture and the arts is good for mental health and well-being, this RCT provides the first reliable experimental evidence lending support for online engagement for depression and anxiety in YP. This report describes an online RCT with 1:1 allocation in which 463 participants aged 16–24 were allocated to WoB, an online experience encompassing the diverse human stories behind art and artefacts and a variety of viewpoints in favour of WoB, or a traditional museum website. Group differences were apparent over the intervention phase for NA but not PA or psychological distress (K10) and group differences were not detected 6 weeks later. In both groups, mean K10 and NA substantially reduced between baseline and the intervention phase and remained low at week 6 despite increased COVID-19 restrictions. There were subgroup differences in NA in favour of WoB in groups in whom help-seeking tends to be low, for example, in ethnic minorities and males. These findings provide early evidence for the potential of online arts and culture in supporting mental health in YP.
This pattern of results is interesting because some models of psychopathology postulate that NA is a core dimension and may be the key unifying thread in anxiety and depressive disorders (Griffith et al., 2010; Mineka et al., 1998) and psychopathology more broadly (Hinden et al., 1997; Krueger et al., 1996; Watson et al., 1988a) and is a mediator between stress and risk-taking behaviours such as substance misuse and smoking in adolescents (Colder and Chassin, 1993; Doran et al., 2011). Psychological therapies have been shown to reduce NA in the short term (Kring et al., 2007). During the COVID-19 pandemic, NA has been proposed as a mediator between social media use and depression in YP (Zhao and Zhou, 2020). It is possible that online arts and culture could positively impact on mental health via a reduction in NA, particularly at times of psychosocial stress, such as the COVID-19 pandemic or other stressful experiences, perhaps including the transition into adulthood itself. These results offer an intriguing indication that WoB includes elements which may have efficacy to reduce mental health symptoms and/or protect against the evolution of mental disorder and associated poor outcomes and provide an avenue for self-management in YP.
Mental health outcomes appeared to improve in both groups over the period of the trial despite increased COVID-19 restrictions. Many epidemiological studies have demonstrated worsening mental health in YP in the context of the COVID-19 pandemic and associated restrictions (Gray et al., 2020; Pierce et al., 2020; Vizard et al., 2020), whereas we observed that both K10 and NA scores reduced. In fact, there appeared to be a clinically significant improvement. In both groups, over 25% less people reported clinically significant symptoms between baseline and the intervention phase which was sustained at 6 weeks (Supplementary Material 1, Table 3). Across the whole population, the mean K10 reduced from 27.1 (range of moderate disorder) to 23.4 (range of mild disorder) in the intervention phase and remained low at 6 weeks (23.3). It is possible that online arts and culture acted as a protective factor for mental health over this period.
These findings also suggest that online arts and culture has potential as an intervention for YP with high unmet mental health needs. At baseline, a high proportion of trial participants reported levels of distress consistent with disorder compared to other studies conducted at a similar time (Gray et al., 2020). Many of those underserved clinically and underrepresented in research were recruited into this study, such as ethnic minorities, non-students and males (Biddle et al., 2004; Lynch et al., 2018; Memon et al., 2016). Subgroup analyses indicated that those traditionally least likely to seek help, such as males and ethnic minorities had a positive response to WoB. Ethnic minorities, non-students and males are poorly served both clinically (Memon et al., 2016) and by the cultural sector in the United Kingdom (Brook and O’Brien, 2020; Syed Sheriff et al., 2021a). It is encouraging that these YP engaged and benefitted in this online trial.
Strengths
This trial was innovative with rapid recruitment, high retention rates and positive feedback. In contrast to many trials of non-pharmacological interventions, this trial compared two alternative potentially active interventions. This reduced the probability of detecting a difference. This trial was conducted online, was inclusive and reached YP who are conventionally hard to reach which may have been aided by its online setting and non-restrictive inclusion criteria, allowing the inclusion of those who may not have identified as having a current mental health problem. We are not aware of any previous experimental research investigating online arts and culture for anxiety and depression in YP.
Limitations
While the results are promising, it is likely that richer content delivered over a longer period would have had a more sustained effect. In the same vein, the design would have benefitted from a third arm to evaluate efficacy compared to a waitlist control. We decided against this strategy given the mental health need in YP at the time of the trial. In addition, it is not possible to elucidate from this study alone the extent to which these findings are dependent on the context of the psychosocial stress of the COVID-19 pandemic.
Implications
These findings contribute to how we understand the links between the cultural and health sectors suggesting there is untapped potential to reach vulnerable groups through arts and culture, especially YP, many of whom are reluctant help-seekers. More effort is needed to explore how online arts and culture support different vulnerable groups and connect to other types of support.
Conclusion
Although museums seek to broaden their user base (which is 92% White) and push back against traditional cultural approaches (Shaindlin, 2019), development of resources through co-production directly link these efforts to engage more diverse audiences with efforts to promote health and thriving more broadly. Tailoring co-produced cultural resources to optimise efficacy on mental health outcomes may be particularly suited to online engagement and must be capitalised on, given the burden of mental disorder in this age group, particularly as we emerge from the COVID-19 pandemic.
Supplemental Material
Supplemental material, sj-docx-6-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-pdf-1-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-2-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-3-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-4-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-5-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Acknowledgments
We would like to thank the following PPI members for their valuable input on the materials used for this trial: Rebecca Woolford, Tharuka Nanomi Arachchige and Louise Chandler. We would also like to thank the following people who kindly provided assistance in the planning, conduct and/or write up of this trial, Susan McCormack, Richard Addis, Bessie O’Dell, Neginsadat Mirtorabi, Leenah Abuelgasim, Hadassah Buechner, Margaret Glogowska and Farhad Shokraneh.
Footnotes
Author Contributions: Trial design: R.J.S.S., A.K.P., E.R., H.A., C.H. and J.R.G.
Trial implementation: R.J.S.S., E.R. and H.A.
Statistical analysis: M.V., A.K.P.
Manuscript preparation: R.J.S.S., M.V., E.R., C.H., A.P., H.A. and J.R.G.
All authors read and approved the final manuscript.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: A.K.P. and M.V. were supported by a grant provided by the Huo Family Foundation. There are no declarations of interest for any of the other authors.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study is sponsored by the University of Oxford COVID-19 Research Response Fund and supported by the NIHR Oxford Health Biomedical Research Centre, The Westminster Foundation and the Huo Family Foundation. The sponsors did not have a role in designing the study, the collection of the results, in the analysis or interpretation of data, the writing of the manuscript or in the decision to submit for publication. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Dissemination Policy: We plan to publish the results of the study on the Ashmolean and/or Oxford University Department of Psychiatry websites for members of the public. We will present a summary of key findings in a format that is accessible to a wide audience.
ORCID iD: Rebecca J Syed Sheriff  https://orcid.org/0000-0002-5934-6722
https://orcid.org/0000-0002-5934-6722
Data Availability: The data and code underlying these analyses are openly available from https://osf.io/9wt8d/
Supplemental Material: Supplemental material for this article is available online.
References
- Abramovich A, Pang N, Moss A, et al. (2021) Investigating the impacts of COVID-19 among LGBTQ2S youth experiencing homelessness. PLoS ONE 16: e0257693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams H, Syed Sheriff R, Cooper-Hammond C. (2021) Optimising online cultural content to positively impact mental health in young people. Museweb 2021. https://mw21.museweb.net/paper/optimising-online-cultural-content-to-positively-impact-mental-health-in-young-people/ [Google Scholar]
- Ander ET, Thomson LB, Blair K, et al. (2013) Using museum objects to improve wellbeing in mental health service users and neurological rehabilitation clients. British Journal of Occupational Therapy 76: 208–216. [Google Scholar]
- Andrews G, Slade T. (2001) Interpreting scores on the Kessler Psychological Distress Scale (K10). Australian and New Zealand Journal of Public Health 25: 494–497. [DOI] [PubMed] [Google Scholar]
- Andrews G, Issakidis C, Carter G. (2001) Shortfall in mental health service utilisation. The British Journal of Psychiatry: The Journal of Mental Science 179: 417–425. [DOI] [PubMed] [Google Scholar]
- Biddle L, Gunnell D, Sharp D, et al. (2004) Factors influencing help seeking in mentally distressed young adults: A cross-sectional survey. The British Journal of General Practice: The Journal of the Royal College of General Practitioners 54: 248–253. [PMC free article] [PubMed] [Google Scholar]
- Bourdieu P. (1984) Distinction: A Social Critique of the Judgment of Taste. Cambridge, MA: Harvard University Press. [Google Scholar]
- Bray MJC, Daneshvari NO, Radhakrishnan I, et al. (2021) Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry 78: 444–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook O. (2016) Spatial equity and cultural participation: How access influences attendance at museums and galleries in London. Cultural Trends 25: 21–34. [Google Scholar]
- Brook O, O’Brien D. (2020) Culture Is Bad for You: Inequality in the Cultural and Creative Industries. Manchester: Manchester University Press. [Google Scholar]
- Browne Gott H. (2020) Exploring the Relationship between Culture and Well-Being. Cardiff: Welsh Government. [Google Scholar]
- Bungay H, Clift S. (2010) Arts on prescription: A review of practice in the U.K. Perspectives in Public Health 130: 277–281. [DOI] [PubMed] [Google Scholar]
- Bygren LO, Konlaan BB, Johansson SE. (1996) Attendance at cultural events, reading books or periodicals, and making music or singing in a choir as determinants for survival: Swedish interview survey of living conditions. BMJ 313: 1577–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callinan J, Coyne I. (2020) Arts-based interventions to promote transition outcomes for young people with long-term conditions: A review. Chronic Illness 16: 23–40. [DOI] [PubMed] [Google Scholar]
- Camic PM, Chatterjee HJ. (2013) Museums and art galleries as partners for public health interventions. Perspectives in Public Health 133: 66–71. [DOI] [PubMed] [Google Scholar]
- Cauce AM, Domenech-Rodriguez M, Paradise M, et al. (2002) Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology 70: 44–55. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L. (1993) The stress and negative affect model of adolescent alcohol use and the moderating effects of behavioral undercontrol. Journal of Studies on Alcohol 54: 326–333. [DOI] [PubMed] [Google Scholar]
- Coles AH, Harrison F. (2018) Tapping into museums for art psychotherapy: An evaluation of a pilot group for young adults. International Journal of Art Therapy 23: 115–124. [Google Scholar]
- R Core Team (2019) A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing. [Google Scholar]
- Cuypers K, Krokstad S, Holmen TL, et al. (2012) Patterns of receptive and creative cultural activities and their association with perceived health, anxiety, depression and satisfaction with life among adults: The HUNT study, Norway. Journal of Epidemiology and Community Health 66: 698–703. [DOI] [PubMed] [Google Scholar]
- Doran N, Sanders PE, Bekman NM, et al. (2011) Mediating influences of negative affect and risk perception on the relationship between sensation seeking and adolescent cigarette smoking. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco 13: 457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D, Finn S. (2019) What is the evidence on the role of the arts in improving health and well-being? A scoping review. Health Evidence Network (HEN) synthesis report 67. Copenhagen: WHO Regional Office for Europe. [PubMed] [Google Scholar]
- Fancourt D, Aughterson H, Finn S, et al. (2021) How leisure activities affect health: A narrative review and multi-level theoretical framework of mechanisms of action. The Lancet Psychiatry 88: 329–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D, Garnett C, Spiro N, et al. (2019) How do artistic creative activities regulate our emotions? Validation of the Emotion Regulation Strategies for Artistic Creative Activities Scale (ERS-ACA). PLoS ONE 14: e0211362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray NS, O’Connor C, Knowles J, et al. (2020) The influence of the COVID-19 pandemic on mental well-being and psychological distress: Impact upon a single country. Frontiers in Psychiatry 11: 594115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, et al. (2010) Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine 40: 1125–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H. (2010) Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 10: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinden BR, Compas BE, Howell DC, et al. (1997) Covariation of the anxious-depressed syndrome during adolescence: Separating fact from artifact. Journal of Consulting and Clinical Psychology 65: 6–14. [DOI] [PubMed] [Google Scholar]
- Johansson SE, Konlaan BB, Bygren LO. (2001) Sustaining habits of attending cultural events and maintenance of health: A longitudinal study. Health Promotion International 16: 229–234. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, et al. (2002) Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 32: 959–976. [DOI] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham, Belfer HM, et al. (2011) Child and adolescent mental health worldwide: Evidence for action. The Lancet 378: 1515–1525. [DOI] [PubMed] [Google Scholar]
- Knapp M, Ardino V, Brimblecombe N, et al. (2016) Youth Mental Health: New Economic Evidence. London: London School of Economics and Political Science. [Google Scholar]
- Konlaan BB, Bygren LO, Johansson SE. (2000) Visiting the cinema, concerts, museums or art exhibitions as determinant of survival: A Swedish fourteen-year cohort follow-up. Scandinavian Journal of Public Health 28: 174–178. [PubMed] [Google Scholar]
- Kring AM, Persons JB, Thomas C. (2007) Changes in affect during treatment for depression and anxiety. Behaviour Research and Therapy 45: 1753–1764. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, et al. (1996) Personality traits are differentially linked to mental disorders: A multitrait-multidiagnosis study of an adolescent birth cohort. Journal of Abnormal Psychology 105: 299–312. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, et al. (2000) Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. The American Journal of Psychiatry 157: 1584–1591. [DOI] [PubMed] [Google Scholar]
- Lynch L, Long M, Moorhead A. (2018) Young men, help-seeking, and mental health services: Exploring barriers and solutions. American Journal of Men’s Health 12: 138–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memon A, Taylor K, Mohebati LM, et al. (2016) Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: A qualitative study in Southeast England. BMJ Open 6: e012337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. (1998) Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology 49: 377–412. [DOI] [PubMed] [Google Scholar]
- Morse N, Thomson LJ, Elsden E, et al. (2022) Exploring the potential of creative museum-led activities to support stroke in-patient rehabilitation and wellbeing: A pilot mixed-methods study. Arts and Health. Epub ahead of print 30January. DOI: 10.1080/17533015.2022.2032224. [DOI] [PubMed] [Google Scholar]
- NESTA (2020) Digital Culture: Consumption in Lockdown. London: Creative Industries Policy & Evidence Centre. [Google Scholar]
- Nochaiwong S, Ruengorn C, Thavorn K, et al. (2021) Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic A systematic review and meta-analysis. Science Reports 11: 10173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksanen A, Laimi K, Bjorklund K, et al. (2017) A 12-year trend of psychological distress: National study of Finnish University Students. Central European Journal of Public Health 25: 113–119. [DOI] [PubMed] [Google Scholar]
- Olfson M, Klerman GL. (1992) Depressive symptoms and mental health service utilization in a community sample. Social Psychiatry and Psychiatric Epidemiology 27: 161–177. [DOI] [PubMed] [Google Scholar]
- Perini SJ, Slade T, Andrews G. (2006) Generic effectiveness measures: Sensitivity to symptom change in anxiety disorders. Journal of Affective Disorders 90: 123–130. [DOI] [PubMed] [Google Scholar]
- Pierce M, Hope H, Ford T, et al. (2020) Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry 7: 883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plumb S. (2012) Neutral territory: The gallery – A site for artists, young people and older people with dementia to collaborate. Engage 30: 21–31. [Google Scholar]
- Proto E, Quintana-Domeque C. (2021) COVID-19 and mental health deterioration by ethnicity and gender in the UK. PLoS ONE 16: e0244419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radez J, Reardon T, Creswell C, et al. (2021. a) Adolescents’ perceived barriers and facilitators to seeking and accessing professional help for anxiety and depressive disorders: A qualitative interview study. European Child & Adolescent Psychiatry 31: 1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radez J, Reardon T, Creswell C, et al. (2021. b) Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. European Child & Adolescent Psychiatry 30: 183–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickwood DJ, Braithwaite VA. (1994) Social-psychological factors affecting help-seeking for emotional problems. Social Science & Medicine 39: 563–572. [DOI] [PubMed] [Google Scholar]
- Rickwood DJ, Deane FP, Wilson CJ. (2007) When and how do young people seek professional help for mental health problems? Medical Journal of Australia 187: S35–S39. [DOI] [PubMed] [Google Scholar]
- Rowe SL, French RS, Henderson C, et al. (2014) Help-seeking behaviour and adolescent self-harm: A systematic review. Australian and New Zealand Journal of Psychiatry 48: 1083–1095. [DOI] [PubMed] [Google Scholar]
- Shaindlin VB. (2019) Reading museum exhibits: Visitors’ reading of exhibits in cultural heritage institutions and museums. The International Journal of Information, Diversity, and Inclusion 3: 63–79. [Google Scholar]
- Stickley T, Hui A. (2012. a) Social prescribing through arts on prescription in a U.K. city: Participants’ perspectives (part 1). Public Health 126: 574–599. [DOI] [PubMed] [Google Scholar]
- Stickley T, Hui A. (2012. b) Social prescribing through arts on prescription in a U.K. city: Referrers’ perspectives (part 2). Public Health 126: 580–586. [DOI] [PubMed] [Google Scholar]
- Stunden C, Zasada J, Vanheerwaarden N, et al. (2020) Help-seeking behaviors of transition-aged youth for mental health concerns: Qualitative study. Journal of Medical Internet Research 22: e18514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Sheriff R, Adams H, Riga E, et al. (2021. a) Use of online cultural content for mental health and well-being during COVID-19 restrictions: Cross-sectional survey. BJPsych Bulletin. Epub ahead of print 12November. DOI: 10.1192/bjb.2021.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Sheriff R, Bergin L, Bonsaver L, et al. (2022) Digital arts and culture for mental health in people aged 16-24: A qualitative interview study. : https://assets.researchsquare.com/files/rs-1393188/v1/01c66359-86e5-4781-a228-b4a0df60ab6b.pdf?c=1658745935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Sheriff R, Edoardo O, Farhad S, et al. (2020) Active community engagement for anxiety and depression in adults and young people (aged 16 and over): Protocol for a systematic review of primary studies. https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=204471 [Google Scholar]
- Syed Sheriff RJ, Vuorre M, Riga E, et al. (2021. b) A cultural experience to support mental health in people aged 16-24 during the COVID-19 pandemic compared to a typical museum website: Study protocol of an online randomised controlled trial. Trials 22: 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson LJ, Morse N, Elsden E, et al. (2020) Art, nature and mental health: Assessing the biopsychosocial effects of a ‘creative green prescription’ museum programme involving horticulture, artmaking and collections. Perspectives in Public Health 140: 277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd C, Camic PM, Lockyer B, et al. (2017) Museum-based programs for socially isolated older adults: Understanding what works. Health & Place 48: 47–55. [DOI] [PubMed] [Google Scholar]
- Twisk J, Bosman L, Hoekstra T, et al. (2018) Different ways to estimate treatment effects in randomised controlled trials. Contemporary Clinical Trials Communications 10: 80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Väänänen A, Murray M, Koskinen A, et al. (2009) Engagement in cultural activities and cause-specific mortality: Prospective cohort study. Preventive Medicine 49: 142–177. [DOI] [PubMed] [Google Scholar]
- Van Lith T, Schofield MJ, Fenner P. (2013) Identifying the evidence-base for art-based practices and their potential benefit for mental health recovery: A critical review. Disability and Rehabilitation 35: 1309–1323. [DOI] [PubMed] [Google Scholar]
- Vijayaraghavan M, Tochterman A, Hsu E, et al. (2012) Health, access to health care, and health care use among homeless women with a history of intimate partner violence. Journal of Community Health 37: 1032–1099. [DOI] [PubMed] [Google Scholar]
- Vizard T, Davis J, White E, et al. (2020) Coronavirus and depression in adults, Great Britain. In: Office of National Statistics (ed.). Office of National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsgreatbritain/june2020 [Google Scholar]
- Watson D, Clark LA, Carey G. (1988. a) Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology 97: 346–353. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. (1988. b) Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology 54: 1063–1070. [DOI] [PubMed] [Google Scholar]
- Williams T, Davis J, Figueira C, Vizard T. (2021) Coronavirus and depression in adults, Great Britain: January to March 2021. Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsgreatbritain/januarytomarch2021 [Google Scholar]
- Zachrisson HD, Rodje K, Mykletun A. (2006) Utilization of health services in relation to mental health problems in adolescents: A population based survey. BMC Public Health 6: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N, Zhou G. (2020) Social media use and mental health during the COVID-19 pandemic: Moderator role of disaster stressor and mediator role of negative affect. Applied Psychology: Health and Well-Being 12: 1019–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-6-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-pdf-1-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-2-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-3-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-4-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Supplemental material, sj-xlsx-5-anp-10.1177_00048674221115648 for A co-produced online cultural experience compared to a typical museum website for mental health in people aged 16–24: A proof-of-principle randomised controlled trial by Rebecca J Syed Sheriff, Matti Vuorre, Evgenia Riga, Andrew K Przybylski, Helen Adams, Catherine J Harmer and John R Geddes in Australian & New Zealand Journal of Psychiatry
Data Availability Statement
The study data and coding used for the main analysis are available on the Open Science Framework https://osf.io/9wt8d/.