Abstract
Three Colombian patients with chronic HTLV-1 infection and severe intermediate and/or posterior uveitis are described. In one case, retinal ablation was necessary due to extensive peripheral degeneration, while the other two were successfully managed with local anti-inflammatory therapy. Gradual resolution of ocular findings was observed in all three patients on follow-up. Uveitis is a rarely recognized late complication of this infection, which represents a diagnostic and therapeutic challenge for clinicians in endemic countries. The real extension of HTLV-1 prevalence in Colombia and the frequency of its ophthalmologic complications remain to be determined.
Keywords: A report of three cases in Colombia, HTLV-1, posterior uveitis
Introduction
Human T-cell leukemia virus type 1 (HTLV-1), the first human retrovirus to be discovered, is present in diverse regions of the world where its infection is usually underacknowledged in health care settings and by public health authorities. 1
HTLV-1 remains a viral neglected infection in Latin America, which is associated with multiple acute and non-acute consequences, including adult T-lymphocyte leukemia/lymphoma (ATLL) and tropical spastic paraparesis/HTLV-1-associated myelopathy (TSP/HAM). 1
While most HTLV-1 infections are asymptomatic, progress to ATLL is observed in 2–4% of cases and to TSP/HAM in 1–4% of cases.2–9
ATLL is clinically characterized by generalized lymphadenopathy, visceral involvement, skin involvement, hypercalcemia, lytic bone lesions, >5% abnormal T cells with normal counts, and occasionally skin and lung lesions. Chronic manifestations include lymphocytosis > 4 × 109/L, T lymphocytes >3.5 × 109/L, and histologically proven lymphadenopathy in the absence of lymphocytosis. Blood smears show ‘flower cells’, pleomorphic, atypical lymphoid cells with basophilic cytoplasm, and complex nuclei. 7 The prevalence and incidence of arthritis were found to be higher among HTLV-1-infected patients than among uninfected individuals in a cohort study. 9 Although data remain sparse, lifetime risk of associated inflammatory and autoimmune syndromes, such as uveitis, dermatitis, alveolitis/bronchiectasis, arthritis, nephritis, and myositis, may be close to 10%.2–9
Intermediate and posterior uveitis, a disorder that threatens the loss of vision in affected individuals, has also been linked to this condition. Ophthalmoscopy reveals opacities in the vitreous, resulting from moderate to high infiltration of inflammatory cells and retinal vasculitis, particularly near the optic disc and the vascular arcade. 5 After the exclusion of other causes of uveitis, the diagnosis is based on seropositivity for the HTLV-1 virus, although it can also be achieved with the polymerase chain reaction in aqueous humor and/or peripheral blood samples. 6 We discuss herein three confirmed cases of intermediate uveitis seen in patients from separate endemic regions of Colombia.
Case 1
A 38-year-old male patient from Sincelejo, Sucre Department, presented with headache, blurry vision, nausea, facial paresthesia, arthralgias, rigidity and weakness in limbs, and edema in the balanopreputial sulcus (Figure 1(a) and (b)). A comprehensive rheumatological and urological assessment detected a reactive arthritis (Reiter’s syndrome). Western blot (WB) for HTLV-1 was positive (7/10 antigens: 2/3 env, 5/7 gag), but negative for HTLV-2 and HIV. Serial fecal concentration examinations were negative for Strongyloides stercoralis, but revealed Blastocystis hominis cysts. Serial acid-fast stains and O-K cultures were negative for Mycobacteria. On ocular fundus examination, the retina appeared adhered, operculated, and latticed between meridians 12 and 6. A retinologist assessment confirmed large peripheral degeneration of the retina, which required retinal ablation by laser. Ulterior evolution was favorable with a steady improvement of initial clinical findings.
Figure 1.
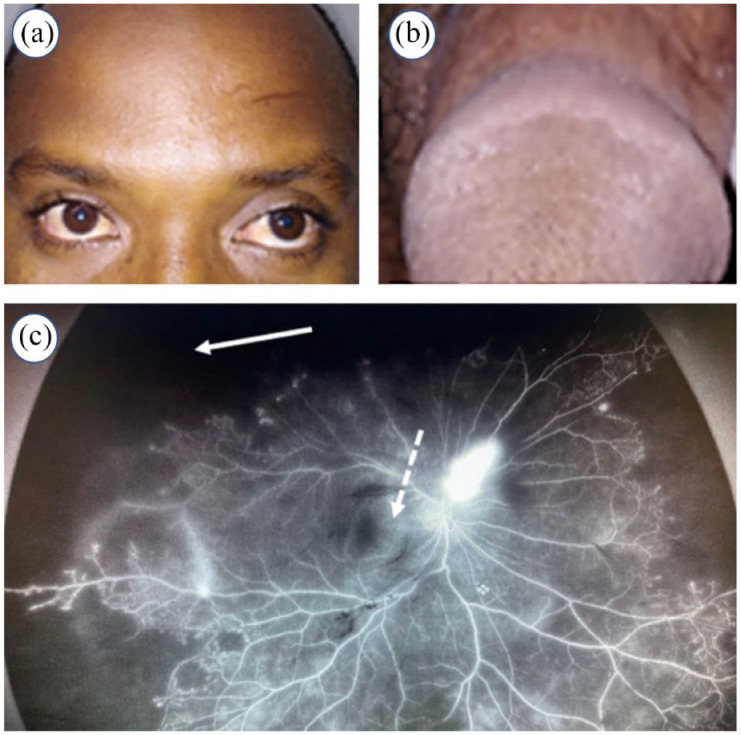
Relevant clinical findings in two patients with HTLV-1-related uveitis. Case 1 exhibited bilateral conjunctival hyperemia (a) and chronic balanopreputial sulcus edema (b). Right fundus fluorescein angiography of case 3 showing extensive peripheral retinal ischemia in 360 degrees (white solid arrow), macular edema (white dash arrow), and widespread retinal neovascularization (c).
Case 2
A 55-year-old male was evaluated because of a 1-year history of bilateral hand distal interphalangeal arthralgia and elbow joint inflammation, accompanied by morning stiffness, fatigue, and myalgias in the lower extremities. Physical examination revealed enanthem on the soft palate and multiple posterior cervical inflammatory lymphadenopathies, bilaterally. He had a history of chikungunya fever, Plasmodium vivax malaria, and gonococcal urethritis. The patient had moved back to Colombia 4 years earlier, after living in Venezuela for 35 years. As part of a clinical protocol for evaluation of patients with suspected chikungunya infection seen at Hospital Universitario de Sincelejo, a detailed ophthalmologic examination was performed. Ocular fundus findings were compatible with bilateral intermediate uveitis, which was treated with local corticosteroid administration. A WB for HTLV-1 was positive, but negative for HTLV-2 and HIV. Sequential stool examinations for Strongyloides stercoralis were negative. Serial acid-fast stains and O-K sputum cultures were negative for Mycobacteria. Clinical evolution was satisfactory with marked gradual improvement.
Case 3
A 12-year-old Afro-descendant female patient from Cali, Valle del Cauca Department, was admitted because of 9 days of fever, intense otalgia, rhinorrhea, conjunctival injection, and general malaise. Physical examination on admission did not reveal a source of infection. Relevant laboratory results included a normal blood count, elevated C-reactive protein, negative procalcitonin, and normal urinalysis. Chest X-ray and paranasal sinuses tomography did not show any pathological finding. After several days afebrile, the patient exhibited a sudden decrease in visual acuity to the point of presenting amaurosis. A pediatric neurology assessment confirmed bilateral loss of vision, predominantly central and of color. A lumbar puncture was performed, revealing cerebrospinal fluid pleocytosis (CSF) at the expense of lymphocytes, proteinorhachia, and hypoglycorrhachia. Gram staining of CSF, bacterial cultures, and a FilmArray® Meningitis/Encephalitis panel test were negative for microorganisms.
Further ophthalmologic evaluation showed bilateral posterior uveitis, with severe peripheral vasculitis, more intense on the right eye, extensive peripheral retinal ischemia, macular edema, and wide retinal neovascularization (Figure 1(c)). Therefore, management with atropine, ophthalmic prednisolone, and immunomodulation therapy with cyclophosphamide was started. Antibodies against HTLV types 1 and 2 and a confirmatory WB test for HTLV-1 were both positive.
Discussion
Since 1981, a high prevalence of TSP/HAM has been recognized in the Southern Pacific lowlands of Colombia, particularly in the locality of Tumaco Island, Nariño Department, where rates as high as 98/100,000 have been reported.10–12 Of note, the local ratio of TSP cases per HTLV-I carriers is unusually high, and the prevalence rate of HTLV-I antibodies in the general population reaches 2.8%. Being female aged above 40 years and a history of intravenously administered medications are associated with a higher probability of being an HTLV-I carrier. 13 Nevertheless, the real extent of the spread of the virus in Colombia remains to be defined.2,3
HTLV-1 uveitis (HU) is more commonly observed in the endemic regions of Japan, Central and Equatorial Africa, Oceania, and South America. In the latter, it has been reported in Amerindian populations of Argentina, Paraguay, Chile, Bolivia, and Peru, as well as in Afro-American populations of Brazil, French Guyana, Suriname, Colombia, and Peru and in Japanese migrants in Bolivia. 6
Intermediate uveitis associated with HTLV-1 infection in Peruvian patients may account for up to 29.4% of all cases of this entity, being only second in frequency to idiopathic intermediate uveitis. In patients aged above 50 years, HU accounted for 45.5% of cases. 6
HU is twice as frequent in women as in men, and although the syndrome mostly affects adults, it has been described in children too. In more than half of the cases, HU is an intermediate uveitis. Bilateral inflammation is as frequent as unilateral; however, some authors report a higher proportion of patients with unilateral uveitis.5,6,14
The management of case 1 involved laser ablation because of the severity of retinal involvement. An effective therapeutic alternative in less complicated patients is the administration of immunomodulators or periocular injections of depot corticosteroids (triamcinolone or methylprednisolone).5,6,14
Differential diagnosis of posterior and intermediate HU must include other infective causes, such as toxoplasmosis, toxocariasis, tuberculosis (TB), histoplasmosis, syphilis, bartonella, herpes simplex, varicella zoster, cytomegalovirus, and HIV, as well as many non-infective causes. 14 After taking into consideration seroepidemiological and clinical studies, the diagnosis of HU should be based on seropositivity for HTLV-1 and exclusion of other uveitis entities with defined causes.5,6,14
While the initial prognosis of HU in most patients is good, with spontaneous resolution within weeks or after the administration of local and/or systemic corticosteroids, more than 90% of cases may recur within 3 years. The mean interval between episodes is 16 months.5,6,14 Corticosteroid is the only effective treatment for HU to suppress the cytokines produced by infiltrating HTLV-1-infected cells. 15 As observed in two of our patients, sight-threatening complications may occur in severe cases. They include retinochoroidal degeneration, glaucoma, and corticosteroid-induced cataracts, among others.9,15
Case 3 was partially described in a recent report on pediatric manifestations of HTLV-1 in Colombia. 16 However, ophthalmological manifestations were not described in detail then, and images of retinal lesions were not included in the original report. The patient was later classified as having Vogt–Koyanagi–Harada syndrome in relation to HTLV-1 infection. We are not aware of any previous instance of such comorbid association.
Although the development of a vaccine for HTLV-1 is considered feasible, no such product is currently available. Therefore, prevention of transmission depends on safe alternatives to breastfeeding, the major route of transmission worldwide. Unfortunately, these options are difficult to provide in many resource-limited endemic areas. 9 For that purpose, it is necessary to improve the awareness of the infection among populations at risk and clinicians in endemic areas. 4
Since HU may be a cause of severe morbidity and sequelae in patients with HTLV-1 infection, surveillance of this important, yet underrecognized complication should be enhanced in Colombia, as there is a scarcity of studies and reports on the subject.
Research Data
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-1-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-2-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-3-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease
Acknowledgments
The authors are grateful to Dr Diana Libreros, an ophthalmologist from Cali. Colombia, for sharing the retinal image of patient 3. These cases were presented at the IX Colombian Symposium of Virology and V Latin American Congress of Virology, November 17–19, 2021.
Footnotes
ORCID iD: Wilmer Villamil-Gomez  https://orcid.org/0000-0002-5492-3455
https://orcid.org/0000-0002-5492-3455
Contributor Information
Wilmer Villamil-Gomez, Centro de Investigación en Ciencias de la Vida, Grupo de expertos Clinicos , Secretaria de salud de Barranquilla, Universidad Simón Bolívar, Barranquilla, Colombia.
Jaime R. Torres, Infectious Diseases Section, Tropical Medicine Institute, Universidad Central de Venezuela, Caracas, Venezuela
Juan Rojas-Hernández, GRINPED Research Group, Universidad Libre Seccional Cali, Cali, Colombia.
Torés Jose Reston, Dirección Científica, Clinica Oftalmologica de la Costa, Sincelejo, Colombia.
Jairo Vergara-Corena, Departamento de Medicina Interna, Universidad de Sucre, Sincelejo, Colombia.
Patricia Salgado, Infectious Diseases and Infection Control Research Group, Hospital Universitario de Sincelejo, Sincelejo, Colombia.
Jorge Viloria-Ruiz, Facultad de Medicina, Universidad de Sucre, Sincelejo, Colombia.
Alvaro Castro, Departamento de Patología, Universidad de Sucre, Sincelejo, Colombia.
Andrés Mauricio Cabrera Lasso, Infectious Diseases and Infection Control Research Group, Hospital Universitario de Sincelejo, Sincelejo, Colombia.
Eduardo Gotuzzo, Universidad Peruana Cayetano Heredia, Lima, Peru.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Written informed consent for publication was obtained from the patients. With regard to case 3, written informed consent for publication was obtained from the patient’s parents.
Author contributions: Wilmer Villamil-Gomez: Investigation; Methodology; Writing – original draft.
Jaime R. Torres: Investigation; Writing – review & editing.
Juan Rojas-Hernández: Conceptualization; Funding acquisition; Investigation.
Torés Jose Reston: Funding acquisition; Investigation.
Jairo Vergara-Corena: Conceptualization; Investigation.
Patricia Salgado: Supervision; Validation.
Jorge Viloria-Ruiz: Data curation; Formal analysis.
Alvaro Castro: Conceptualization; Supervision; Validation.
Andrés Mauricio Cabrera Lasso: Funding acquisition; Investigation; Supervision.
Eduardo Gotuzzo: Investigation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: For any inquiries contact the corresponding author.
References
- 1.Gonçalves DU, Proietti FA, Ribas JG, et al. Epidemiology, treatment, and prevention of human T-cell leukemia virus type 1-associated diseases. Clin Microbiol Rev 2010; 23: 577–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cardona-Arias JA, Velez-Quintero C, Calle-Gonzalez OV, et al. Seroprevalence of human T-lymphotropic virus HTLV and its associated factors in donors of a Blood Bank of Medellin-Colombia, 2014–2018. PLoS ONE 2019; 14: e0221060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Domínguez MC, Salcedo M, García-Vallejo F.Serological and virological evaluation of human T-lymphotropic virus type 1 infection in family groups from Tumaco, Colombia. Biomedica 2015; 35: 337–346. [DOI] [PubMed] [Google Scholar]
- 4.Schierhout G, McGregor S, Gessain A, et al. Association between HTLV-1 infection and adverse health outcomes: a systematic review and meta-analysis of epidemiological studies. Lancet Infect Dis 2020; 20: 133–143. [DOI] [PubMed] [Google Scholar]
- 5.Manabu Mochizuki MD, Toshiki Watanabe MD, Kazunari Yamaguchi MD.Uveitis associated with human T-cell lymphotropic virus type 1. Am J Ophthalmol 1992; 114: 123–129. [DOI] [PubMed] [Google Scholar]
- 6.Siverio-Llosa C, Silva-Ocas I, Gálvez-Olórtegui T, et al. Clinical course of HTLV-1 infection associated intermediate uveitis. Arch Soc Esp Oftalmol 2022; 97: 386–390. [DOI] [PubMed] [Google Scholar]
- 7.Murphy EL, Roberta L.Human T-lymphotropic virus (HTLV). In: Mandell GL, Bennett JE. (eds) Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 8th ed.Amsterdam: Elsevier, 2015, pp. 2038–2053.e6. [Google Scholar]
- 8.Mejía-Mertel J, Gómez-Banoy N, Rojas-Hernández JP, et al. Clinical profile of human T-lymphotropic virustype I: a forgotten infection in pediatrics. Infectio 2021; 25: 28–32. [Google Scholar]
- 9.Verdonck K, González E, Van Dooren S, et al. Human T-lymphotropic virus 1: recent knowledge about an ancient infection. Lancet Infect Dis 2007; 7: 266–281. [DOI] [PubMed] [Google Scholar]
- 10.Zaninovic V, Biojó R, Barreto PL.Paraparesia espástica del Pacífico. Colombia Med 1981; 12: lll–117. [Google Scholar]
- 11.Arango C, Concha M, Zaninovic V, et al. Epidemiology of tropical spastic paraparesis in Colombia and associated HTLV I infection. Ann Neurol 1988; 23(Suppl.): S161–S165. [DOI] [PubMed] [Google Scholar]
- 12.Román GC, Román LN, Spencer PS, et al. Tropical spastic paraparesis. A neuroepidemiological study in Colombia. Ann Neurol 1985; 17: 361–365. [DOI] [PubMed] [Google Scholar]
- 13.Trujillo JM, Concha M, Muñoz A, et al. Seroprevalence and cofactors of HTLV-I infection in Tumaco, Colombia. AIDS Res Hum Retroviruses 1992; 8: 651–657. [DOI] [PubMed] [Google Scholar]
- 14.Sudharshan S, Ganesh SK, Biswas J.Current approach in the diagnosis and management of posterior uveitis. Indian J Ophthalmol 2010; 58: 29–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kamoi K, Mochizuki M.HTLV-1 uveitis. Front Microbiol 2012; 243: 270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James IC, Mejía-Mertel J, Gil Artunduaga MA, et al. Case series: pediatric human T-lymphotropic virus type 1 and its clinical expression. Front Trop Dis 2022; 2: 824067. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-1-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-2-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-pdf-3-tai-10.1177_20499361231165864 for HTLV-1 uveitis in Colombia, an underrecognized complication of a hitherto neglected condition: a case series by Wilmer Villamil-Gomez, Jaime R. Torres, Juan Rojas-Hernández, Torés Jose Reston, Jairo Vergara-Corena, Patricia Salgado, Jorge Viloria-Ruiz, Alvaro Castro, Andrés Mauricio Cabrera Lasso and Eduardo Gotuzzo in Therapeutic Advances in Infectious Disease


