Abstract
Social media has changed the way we communicate and interact. Unsurprisingly, it has also changed how we teach and learn. Younger generations of learners have transitioned from traditional educational sources to digital ones. Medical educators need to adapt to trends in medical education and develop fluency in the digital methods used by medical learners today. This is part two of a two-part series on social media and digital education in neurology. This article provides an overview of how social media can be used as a teaching tool in medical education and provides an overview in which it is grounded. We offer practical strategies on how social media can promote lifelong learning, educator development, educator support, and foster educator identity with accompanying neurology-specific examples. We also review considerations for incorporating social media into teaching and learning practices and future directions for integrating these tools in neurology education.
Keywords: social media, curriculum, medical education, pandemic, neurology education, COVID-19, Twitter, Instagram, child neurology, information dissemination
Introduction
Social media (SoMe) has changed the way we communicate and interact. Unsurprisingly, it has also changed how we teach and learn. Younger generations of learners have transitioned from traditional educational sources to those within the digital realm, and these learning behaviors persist when this generation transitions to attending and faculty roles.1,2 Digital education, a subset of technology-enhanced learning (TEL) that takes place exclusively in a virtual environment, has expanded in popularity over the past decade for teaching and learning. Digital education often involves SoMe but encompasses other ancillary digital resources like podcasts, streaming videos, blogs, gamification, and virtual reality.
The pandemic forced many medical educators to rapidly adapt to the digital learning environment, which supported existing medical education trends.3–5 As a result, the Association of American Medical Colleges (AAMC) expects future medical educators to have competency in content curation, learner-centric coaching, learning environment pioneering, and technology adaptation. 3 These align with ACGME competencies in practice-based education, improvement, and the trend of learners becoming prosumers (both consumers and producers of content). This role increases motivation, responsibility, self-evaluation, and promotion of their learning. 4 The effectiveness of such strategies has been reported, 5 and are preferred by current learners as learner-centric and customized approaches to education.6,7
Digital skills are already integrated into residency curriculums to prepare the next generation of medical educators.5–13 However, current medical educators must learn these skills independently, which creates variability in content quality and practices. Missteps in SoMe can alienate students, negatively affect a career path, and increasing educators’ anxiety about using digital education. Additionally, mastering new digital educator skills can seem overwhelming, time-consuming, and burdensome.
As medical educators, we need to adapt to trends in medical education and develop fluency in the methods and tools learners use. In addition, understanding how digital education trends are grounded in adult learning theory can help promote the acceptance and legitimization of non-traditional educational methods.
Part 1 of this series provided a broad overview of how to use SoMe for career development as clinicians, scientists, and advocates. 14 We also reviewed the challenges of SoMe, including professionalism best practices, Health Insurance Portability and Accountability Act (HIPAA) compliance, time commitment, and conversational limitations. These remain important considerations when using SoMe as a medical educator. The objective of this article (part 2 of 2) is to introduce how SoMe is a subset of TEL and the educational theory supporting its use. Additionally, we offer practical strategies to leverage SoMe in medical education, lifelong learning, educator development, educator support, and foster educator identity. The broader topic of TEL will be covered in additional companion articles.
1. Terminology
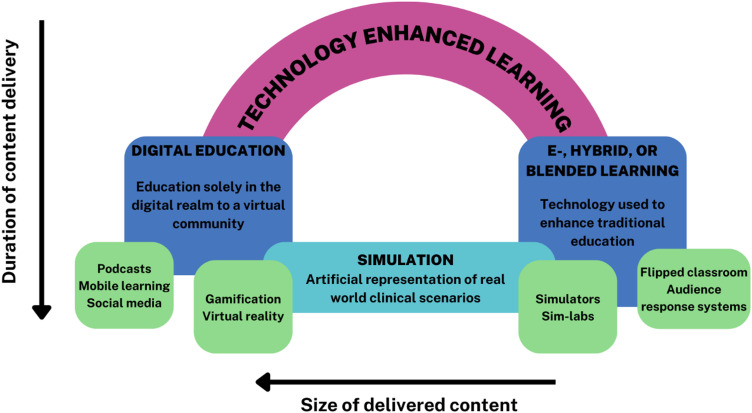
Multiple terms describe technology-enhanced learning, some with overlapping definitions, creating a confusing nomenclature (Figure 1). TEL is an umbrella term encompassing all forms of teaching and learning that use technology. 15 Implicit in the word is the recognition that technology is a vehicle through which learning occurs and should augment, not distract from, the exchange between teacher and learner.
Figure 1.
Technology-Enhanced Learning (TEL) encompasses learning that occurs solely in the digital realm (Digital Education) and the use of technology within a traditional learning environment (E, Hybrid, or Blended Learning).
Digital education refers to education solely occurring in a virtual environment. Digital education often involves SoMe but encompasses other digital resources like podcasts, streaming videos, blogs, gamification, and virtual reality.
Microlearning refers to the delivery of teaching in bite-sized lessons, courses, or content. It is intended to reinforce other educational methods and is specifically characterized by the content's size. It gives the learner flexibility and control in how and when they learn. It also provides learning in brief intervals (seconds to minutes), a concept known as just-in-time learning. Microlearning and just-in-time learning are emerging medical education trends that rely heavily on digital education skills and comfort with technology.
SoMe is a collective term referring to platforms that facilitate communication, community-building, creation, curation, and sharing of content through participation in a user-created social network. 16 As a subset of digital education, SoMe facilitates teaching within the virtual community of a SoMe platform such as Twitter, Facebook, Instagram, YouTube, WhatsApp®, and TikTok. Each platform includes unique parameters of how the users connect, communicate, and share content allowing individuals to leverage different platforms for different purposes and reach a broader, more diverse group of learners and educators. As a result, familiarity with the other SoMe platforms and how they can be used in medical education is crucial for neurology educators today.
Technology blended with traditional elements is referred to as e-learning or blended learning. It employs technology or digital tools to enhance traditional teaching methods (ie, flipped classrooms and audience response systems). Simulation refers to learning experiences with an artificial representation of real-world scenarios to allow the development of clinical reasoning, clinical skills, and procedures. Simulation can be accomplished entirely in the digital realm, for example, using gamification and virtual reality or as part of a hybrid laboratory experience using high-fidelity simulators or standardized patients in an in-person setting. Augmented reality (AR) is the hybrid experience that adds a virtual layer to physical reality. In addition to its application to simulations, AR can create a more immersive experience for neuroscience education, including neuroanatomy and histology.17,18
II. Conceptual Frameworks
Conceptual frameworks provide a scaffold for approaching an educational problem by allowing consideration of multiple factors that will contribute to the curricular outcome. By rooting an educational experience within a framework, the optimal teaching approach to achieve desired outcomes is more readily identified.19–21 Different conceptual frameworks can be considered to address the same educational need resulting in a unique design of learning experiences using shared tools. 19 Incorporation of SoMe into medical education is rooted in several complementary frameworks that inform its use in different contexts: constructivism, connectivism, and communities of practice. 20
Constructivism
Constructivist learning theory is a commonly encountered conceptual framework in SoMe curricula. Constructivist theories are learner-focused, centered on the learning process rather than on the instructor's transmission of information. By shifting focus to the learning process, responsibility transitions to the learner. The role of the teacher then evolves into a facilitator for the “construction of knowledge.” 20 Inherent in constructivism is the critical importance of the social context of learning: learners construct their knowledge through interactions and explorations with peers and those with more expertise (either peers or teachers). At its core, education must be internally driven with the ability for self-direction facilitated by the learning environment created by the teacher. 20
Connectivism
Complementary to constructivism, connectivism is a new theoretical framework for understanding how learning occurs in the digital age. Particularly relevant to SoMe, connectivism describes learning as a fundamentally social, active, and reflective process shaped by technology. The framework highlights technology's impact on learning and building learning communities, where learners connect on shared topics of interest, making knowledge together. 22
Community of Practice
Leveraging SoMe platforms allows the intentional and unintentional development of communities of practice (CoP). Social learning occurs among individuals with a common interest as they collaborate to share ideas and knowledge and develop solutions and innovations.23–25 The CoP conceptual framework is particularly well suited for SoMe platforms, whose emphasis is social connection.26,27 In the pre-SoMe era, the CoP conceptual framework centered on the template of learning that occurs informally in social communities. Initially focused on interactions between novices and experts, this framework later evolved to consider the trajectory of an individual's participation in a group from a peripheral to a core role. The concept continues to grow and integrate work examining professional identity formation. At its core, a community of practice encompasses three key elements: 1) Domain, the area of knowledge on which the community is focused; 2) Community, the people who are brought together around the shared domain and 3) Practice, which refers to the work the community does to further their shared goals which are centered on the domain. 24 CoP frameworks are leveraged by medical educators to create virtual communities on SoMe to collaborate, network, and create around shared interests and goals (domains) to enhance their outreach and impact.27–29
III. Lifelong Learning
As discussed in the initial article, SoMe is a valuable tool for continuing medical education (CME) and promoting lifelong learning. Specific CME opportunities occur within SoMe, such as a monthly webinar series through the Women's Neurologist Group (WNG), BlackInNeuro, or NeuroBytes. 14 In addition, other TEL, such as podcasts or mobile learning, can be advertised through SoMe to reach a broader audience.
Tweetorials, questions of the day, and online journal clubs also present an opportunity for promoting lifelong learning without CME. However, becoming a prosumer (both consumer and content producer) facilitates responsibility and motivation that supports your education. Content creation thus can serve a dual purpose as a tool for teaching and learning.
IV. Educator Development: Building a Teaching Portfolio with SoMe
Teaching with SoMe
SoMe platforms can be used strategically by neurology educators to disseminate educational materials digitally. Twitter remains the most utilized platform for SoMe teaching, delivering content through Tweetorials, journal clubs, daily teaching pearls, interactive electroencephalogram (EEG) cases, clinical cases, and morning reports. In addition, visually-driven platforms like Instagram and TikTok can be used to teach clinical skills, anatomy, and more through high-yield images. Finally, videos can be strategically paired with discussion threads in the comments using hashtags to direct content toward the intended learner audience.
Tweetorials
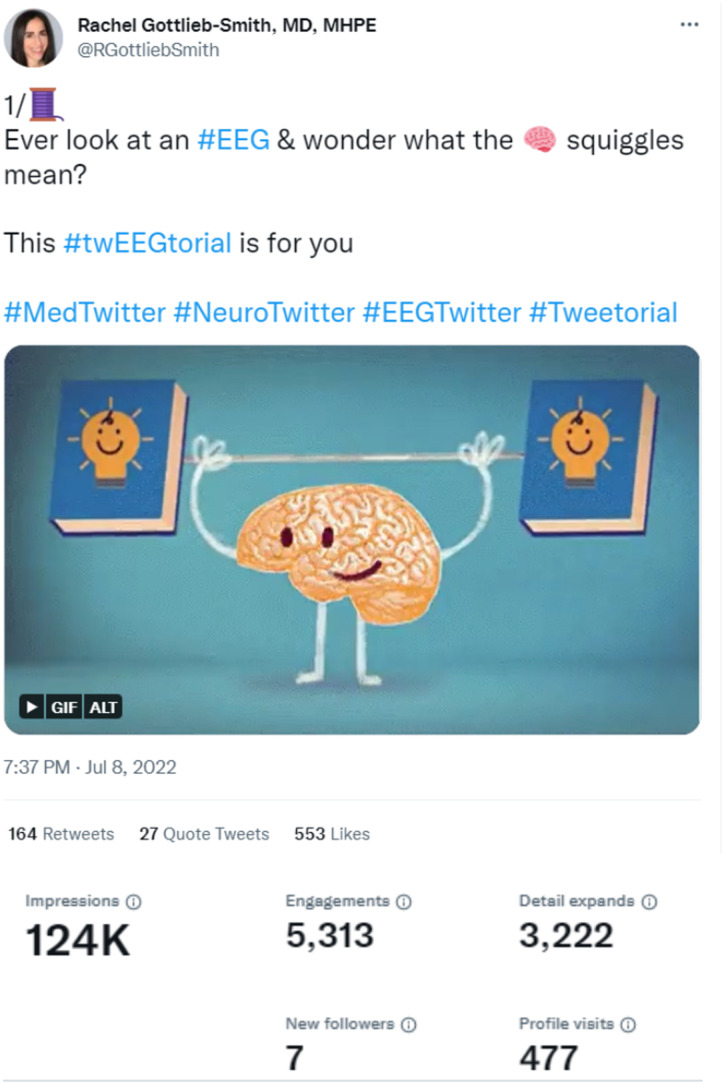
Tweetorials, a combination of a tweet and tutorial, are synchronous posts designed to deliver engaging educational content (Figure 2).30,31 Since they were first introduced in 2008, tweetorials have become a powerful tool in medical education. Common elements of a successful tweetorial include a defined educational goal, a highly engaging first tweet to “hook” the learner, interactive components, and succinct messaging. 30 Strategic integration of hashtags (such as #Tweetorials) or tags can amplify the reach of a tweetorial, aiding in broadening one's network, influence, and educational portfolio.31,32
Figure 2.
Example tweetorial focused on the basics of EEG interpretation—courtesy of Dr Rachel Gottlieb-Smith.
Specific SoMe user communities may be targeted, often using hashtags to highlight content for identified users. For example, content shared on Twitter relevant to the neurology community may be tagged with #neurotwitter. More than one hashtag can be used simultaneously, allowing a broader reach of material within multiple communities on a single platform simultaneously. 30 In addition, creating a Tweetorial can serve as a learning opportunity, offering unique opportunities to integrate the strategy into medical education.
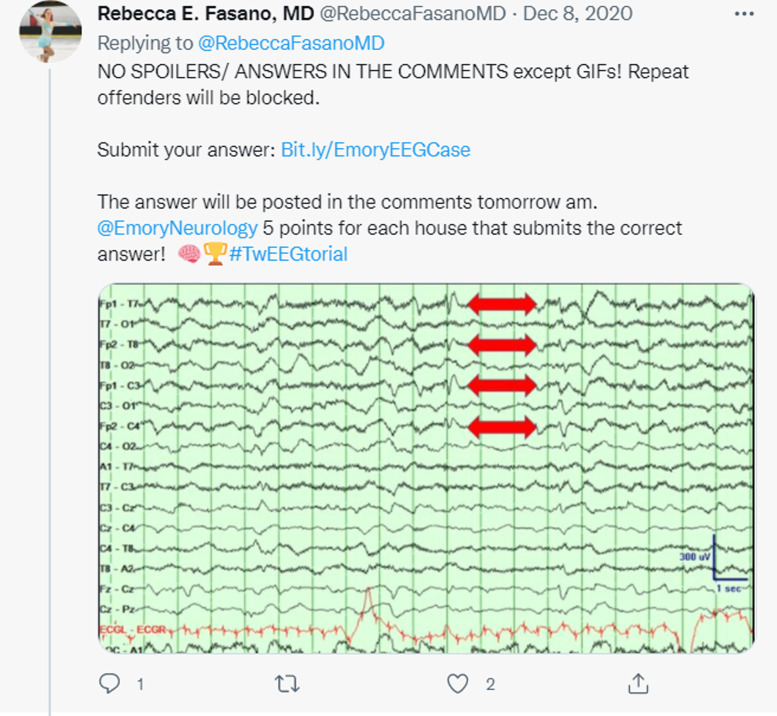
Instagram, a primarily visual SoMe platform centered on sharing images with a caption and comments section, is particularly well suited for teaching topics such as anatomy or radiology through high-yield photos and graphics (Figure 3). Through short videos, reels, or photographs, educators can post visual content centered on a single teaching pearl highlighting key anatomical, surgical, pathology, radiology, or physiology concepts. In addition, learners can interact in comments extending the discussion beyond a passive review of the material to a more interactive discussion. Unlike Twitter or Facebook, the adoption of Instagram as a SoMe medical education tool has been slower; however, the visual nature provides opportunities for innovative approaches to teaching. In addition, limited video length and pictures make the platform particularly well-suited for micro-learning strategies.33,34
Figure 3.
Example of an Image of the Day. Learners are asked to submit their answers to a question identifying a finding or diagnosis based on an image. While points are awarded to participants from the specific residency program, learners worldwide can engage with the content and learn the targeted teaching concept—image Courtesy of Dr Rebecca Fasano.
Journal Clubs
Like their traditional in-person counterpart, the medical Twitter community has readily adopted Twitter virtual journal clubs as an opportunity to learn and discuss current literature, build community, and grow networks. While offering many of the benefits of a traditional journal club, including providing a format to critically review and discuss literature as well implications for clinical practice, Twitter-based journal clubs offer some additional unique aspects that can enhance the experience for participants. Twitter Journal clubs facilitate broader conversations, a more comprehensive selection of articles, author participation, cross-specialty collaboration, and content curation for later reference.33–35 Journal clubs are hosted by societies, such as the Neurocritical Care Society Journal Club (@neurocritical; #NCSTJC) or Alliance for Clinical Education (@MedEdChat, #mededchat), or virtual communities of practice. Formats can vary, but often the journal club occurs at a specific recurring time centered on a single article or topic of discussion. Moderated questions can generate a conversation that occurs through threads and use tools such as hashtags and reply/quote replies to build dialogue. Transcripts can be saved on websites for easy review or reference.
TikTok Teaching
TikTok is a SoMe platform using short videos to create and share content. A relatively newer platform, there is growing interest in leveraging these short videos for medical education, patient education, and advocacy. Short videos are centered on a specific learning objective. They can teach clinical skills, such as physical exam maneuvers and history-taking skills, or highlight a particular learning objective in a visual, conversational manner. The video-based platform is particularly well suited for creating micro-learning content which can be accessed in a “just in time” manner. 36 Hashtags guide interested users to content and can be used strategically to create a thread of related videos that build upon one another, similar to a tweetorial but in a video format. A comments section allows educators to engage with their learners to clarify questions or continue the discussion beyond what is highlighted in a short video clip.
V. Educator Support: SoMe as Part of the Flipped Classroom and Microlearning
Flipped classrooms have long been identified as a superior method for knowledge transfer compared to traditional educational methods. Flipped Classroom is an instructional method focused on interactive learning by “flipping” independent learning and classroom activities. Learners are asked to prepare for a didactic session by reviewing material independently before class time is spent applying the concepts through interactive activities.37,38 Digital educational resources, including podcasts, streaming videos, SoMe, online quizzing tools, and student response systems, play an essential part in the flipped classroom process and are already commonly used by health professions education. 39 However, increased clinical duties for postgraduate trainees often “crowd out” educational activities. Therefore, microlearning and microteaching with digital educational resources have been advanced as possible interventions. 40 In particular, microlearning improves knowledge retention, builds procedural skills, and encourages learners to participate in collaborative education. 5
VI. Educator Identity: SoMe for Professional Growth
SoMe is a powerful tool for medical educators to connect around shared interests to collaborate, create and build networks. SoMe platforms are particularly well suited to support such communities of practice (CoP) and bring together individuals from diverse backgrounds, experiences, and geographic locations on shared interests. As such, it is vital in academic collaboration and mentorship in the twenty-first century. The Women's Neurologist Group (WNG) is an example of a community of practice that uses a closed Facebook group platform to house a community of women neurologists who network, support, collaborate and learn together. Facebook Groups create a protected space in which individuals come together. To allow this, group administrators create criteria for community entry and outline rules for interactions within the group, which are then moderated.
Networking and participation in communities of practice also take place on Twitter, which distinctly supports these interactions from Facebook Groups. Hashtags (denoted by #) link and highlight (or tag) conversations on a specific topic of interest to a particular community. Clever use of hashtags such as #meded, #neurotwitter, and #mededtwitter, allows individuals to follow and engage in conversations on topics of interest. These interactions do not occur behind a “closed door” of the Facebook group and can allow for broader networking outside of an individual's usual professional circles. In addition to growing one's professional network, Twitter offers many opportunities to highlight and virtually sponsor the work of others by retweeting, quote tweeting, and engaging with tweets highlighting the content of interest.
Instant messaging apps, such as WhatsApp®, can provide another platform for community building, engagement, and networking. WhatsApp® can be used as a secure educational tool due to end-to-end encryption, two-way opt-in for all users, and the ability for user activity and message reading to be monitored. 41 Integration of WhatsApp® into hybrid learning models to extend discussion past the classroom has been used, as well as the ability to house an online space for a designated group of individuals to share experiences, resources, and advice. The virtual platform can allow the development of digital professional communities of practice, mainly supporting isolated healthcare professionals such as those working in more rural communities or undergoing career transitions.
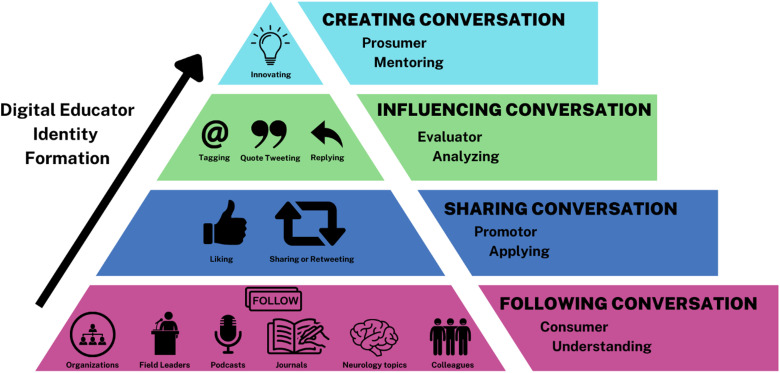
Engagement on SoMe platforms allows educators to network within communities broader than their institution or professional societies elevating their impact and reputation as medical educators. 42 Through this process, educators shift from consumers to prosumers while simultaneously forming and internalizing their digital educator identity (Figure 4). Additionally, educators reach more learners. For example, traditional grand rounds or lectures reach less than a hundred individuals, and national conference speaker perhaps reaches less than a thousand individuals; however, on SoMe, an educator can get thousands or hundreds of thousands of individuals rapidly.
Figure 4.
Proposed framework for consideration of digital educator formation, with individuals moving from a novice level, engaging primarily as a consumer or bystander to an expert, creating content, and considering innovative strategies for incorporating SoME in teaching and mentoring others in use.
Engaging in education using SoMe has impacted the relationship between educators and their learners, with studies noting that learners feel more comfortable asking questions of their peers and appreciate the opportunity to hear responses from a diverse network when able to pose those questions on SoMe platforms. The ability for SoMe networks to “flatten” traditional academic hierarchies has increased learner comfort in engaging with their educators, collaborating with their peers, and engaging with the material. The opportunity to extend the conversation on SoMe beyond the classroom has allowed for ongoing communication and collaboration outside traditional methods. As these educator-learner relationships evolve through the use of SoMe, intentional education related to the professional use of SoMe is needed for all, with attention to topics such as accountability, confidentiality, professional boundaries, and personal digital health.43–45
The broader impact of SoMe activities can be captured for academic portfolios using alternative metrics such as Altmetrics and Symplur Analytics. 46 In addition, other digital educational resources, such as podcasts or streaming videos, have easily accessible usage metrics. While not uniformly accepted in the promotion process, there is a growing movement toward formal recognition of these metrics in scholarly activities and products, mainly as they are situated within social learning theories, which emphasize the importance of social connectivity as part of the learning process.32,47–50
VII. Considerations for Incorporating SoMe as a Neurology Educator
SoMe and Neurophobia
SoMe offer a unique opportunity for neurology educators to extend their reach, educating a broad community and creating opportunities to reduce neurophobia, provide exposure to the field and further develop a pipeline for recruiting diverse, engaged students into neurology. Neurophobia, the fear of neurology among medical students and non-neurologist physicians, is well documented and has practical implications, including fewer students pursuing careers in neurology and reduced confidence in patients presenting with neurological conditions leading to increased patient referrals to neurology.51,52 Additionally, the shortage of neurologists in the face of an increasing number of patients with chronic neurological disorders can overwhelm the current workforce and further aggravate neurophobia.53,54 SoMe offer a unique opportunity for neurology educators to combat neurophobia in an accessible, digestible, interactive, and supportive manner.9,55 Uniquely, SoMe can invite a broad range of medical professionals to the conversation, such as with the Neurocritical Care Society (NCS) Twitter journal club, which draws neurologists, pharmacists, nurse practitioners, nurses, and trainees into the bimonthly discussion. The NCS has also collaborated with other societal groups to host article discussions across subspecialties, expanding the conversation outside neurology.
SoMe Digital Inclusion and Equity
By extending the learning environment beyond the classroom, SoMe allow neurology educators to facilitate a larger, more diverse conversation. It can facilitate access to virtual lecturers with unique areas of expertise, 56 breaking traditional geographic or hierarchal boundaries. While some argue that SoMe mitigate accessibility barriers to high-quality education, mentors, networks, and experiences, the increased utilization of digital education does not address decades of preexisting disparities and inequities. Significant global gaps in the uptake of digital educational resources continue to exist, though culturally- and linguistically-targeted interventions involving local learners and teachers have been effective.57,58
Developing Best Practices for the Incorporation of Technology in Clinical Learning Environments
While the potential of digital education for medical education was enthusiastically and widely embraced during the height of the COVID-19 pandemic, studies are just emerging to evaluate the best ways to leverage this technology as an effective educational tool.45,59 Ongoing education research examining TEL curricula is crucial for developing best practices for incorporation in neurology education. In addition, education for trainees on becoming responsible consumers and stewards of SoMe is essential, as is providing explicit trainee and continuing medical education on professional use of technology and social media, including appropriate timing to use digital tools and technology in clinical spaces or as part of clinical rotations Recognition and discussion of the quality of education received on SoMe, in particular, whether material reviewed provides adequately in-depth instruction on a specific topic requires education of consumers and producers of content on SoMe platforms. A recent systematic review by Maudsley et al summarized identified best practices for the incorporation of mobile technology in clinical rotations, recognizing both the potential benefits technology brings to the clinical learning environment as well as the unintended negative consequences of perceived unprofessionalism, patient privacy/confidentiality, impact on the hidden curriculum and potential to distract from patient care. 60 Evidence-based guidelines for educators incorporating mobile technology and TEL into clinical rotations have been proposed, emphasizing clear goals and intentionally building a technology culture, including clear expectations for use, positive role modeling, and frequent feedback to inform further innovation and address educational gaps when used in professional activities. Evidence supports thoughtful incorporation of mobile technology and digital education in clinical learning spaces as a powerful approach to better quality learning with a recognized need for ongoing rigorous scholarship to delineate best practices further and directly address concerns related to professionalism, confidentiality, and distraction.60,61
Peer Review for Digital Educators
Peer review is crucial to all medical and educational products and scholarships. It refers to how others review an author's work in their field (peers) to ensure accuracy and quality. The lack of formal peer-review mechanisms has long challenged digital educators. 62 Fortunately, as the field matures, review mechanisms appear increasingly common, and many producers of digital educational content have partnered with medical journals and professional societies to grant continuing medical education credits and provide formal peer review.31,63 Despite this, without standards, the responsibility for determining the quality of educational research still largely falls on learner gestalt. Lack of peer review of content and credentials of individual users should be considered when engaging with medical education content to ensure accurate information and reduce the spread of misinformation.16,45,64 As digital education teaching activities are only sometimes financially supported by institutions, many podcasts, and streaming videos take advertising. Financial conflicts of interest appear to be common in digital education, and these conflicts are not frequently disclosed. 63
Becoming proficient in digital education also takes deliberate skill building, though the barriers to entry are lower than most educators think. For example, the skills necessary to create podcasts or infographics can be quickly learned within an afternoon. Residency and fellowship programs are increasingly training future medical educators in digital education, and continuing medical education conferences that focus on practical skills have also proliferated.65–68
VIII. Future Directions
As evidenced above, SoMe can be harnessed to provide asynchronous resources to students, build a teaching portfolio, and network with clinician educators worldwide. However, in each of these domains, there is a rich opportunity to understand better the degree to which SoMe is effective and influential.
Students embrace SoMe education as it is often free, asynchronous, and bite-sized; however, there has yet to be a concerted effort among neurology educators to establish the best practices for SoMe teaching. For example, should all SoMe include links to primary literature and chapters for further reading? Citing relevant peer-reviewed resources may be one way that our field can establish validity for the content posted on social media. Still, more work will be needed: setting verified and trustworthy content in social media is gravely important. Given that social media posts are public and can be discussed in the comments, many inaccuracies posted are debated in real time; however, learners who do not read the comments or dialogue may be left with false impressions, which can contribute to the spread of misinformation and disinformation.
Leaders in this space have formed editorial committees highlighting and fact-checking medically reputable blogs and podcasts and giving approval ratings so that students and trainees know that academic faculty have determined these resources as high-yield and valid. An example of this is Academic Life in Emergency Medicine (ALiEM)'s Approved Instructional Resources (AIR) series which highlights the best FOAM resources each year (https://www.aliem.com/aliem-approved-instructional-resources-air-series/). However, a quality control editorial group like this does not yet exist within Neurology; this will be a crucial vacancy to fill.
More questions remain about what type of posts have the highest educational impact. How long should content be to retain the attention of today's learners? Which platform is most engaged among learners at various levels? Will physicians use it for CME? In undertaking this challenge, educators will benefit from identifying and studying “neurology education influencers,” – such as in General Surgery and Neurosurgery.69,70 What makes their content successful? To what degree does it reflect a constructivist or connectivism educational paradigm? How can it be placed into a more expansive curriculum so students can find comprehensive resources?
Just as educators must establish best practices to promote the longevity of learning from social media, the collective group of health professionals must also set boundaries for teaching in a public domain that can reach millions of viewers worldwide. This is especially crucial around consent for posting. Avital O’Glasser, an internal medicine physician known for tweetorials on peri-operative management, wrote a widely shared tweetorial on the concept of “Post the Pearl, not the patient” (https://twitter.com/aoglasser/status/1236053604080873473) urging all health professionals to think about privacy concerns that extend beyond HIPAA. The advice shared in this thread and similar works (https://www.atsjournals.org/doi/full/10.34197/ats-scholar.2020-0155PS) should be considered mandatory reading for health professionals and trainees that teach through social media. However, there is currently no way to enforce these policies.
Moving beyond the ethics and best practices for creating innovative teaching, more questions and challenges emerge as digital education becomes considered academic scholarship. For educators who use SoMe as part of their teaching portfolio, the major next step for educators is to establish the validity of SoMe teaching and define the merits of digital education as an activity of educational scholarship. That anyone can post educational content on SoMe is a double-edged sword. It is thus imperative, as Cooper and Breu have argued, that medical educators obtain peer-review of their digital teaching material, providing quality assurance. 47 Specialties that were early adaptors have already established precedence for peer review. For example, Sherbino et al, through a consensus process, defined a standard for SoMe-based scholarship, proposing that the content must 1) be original, 2) advance the field of health professions education by building on theory, research or best practice, 3) be archived and disseminated, 4) provide the health professions education community with the ability to comment on and transparently provide feedback. 46
The creation of engaging and factual content is time intensive. Because it is reproducible by other scholars, peer-reviewed SoMe educational content should be treated as education scholarship in Glassick's framework 71 and by Shulman's paradigm, two frameworks that delineate criteria by which a work can be considered a product of scholarship and assessed as such. 72 Educators that invest academic capital into creating SoMe content should be recognized for this work. Emergency medicine educators have established consensus Guidelines for Digital Scholarship in Academic Promotion. 32 However, these have yet to be widely adopted in Neurology. Furthermore, only some metrics can communicate their SoMe productivity to other SoMe creators and even academics unfamiliar with the space.
Specific metrics measuring the impact of an individual author's digital education and social media scholarship have been proposed, modeled on well-established scholarship metrics such as the H-index, which measures an individual author's cumulative scholarly impact based on productivity and citation impact factor. One example of an altmetric proposed to capture digital scholarship impact is “The T-Factor", 68 a metric modeled on the H-index, which combines twitter-specific metrics of the number of tweets and retweets to provide an impact score has not been widely adopted. There is yet to be a validated tool for educators to describe their digital education impact.
To demonstrate value, as for any curricula activity, educators must also study the degree to which SoMe teaching promotes knowledge gain and retention, moving beyond “likes” to demonstrating knowledge growth and, ultimately, change in behavior (reflecting higher Kirkpatrick levels of learning in curriculum assessment). 73 As for many educational initiatives, pinpointing how one initiative leads to behavior change will be challenging but possible with thoughtful SoMe curriculum and pre-/post- curriculum observation. These studies are needed. A similar analysis is necessary to explore how different learners interact and learn from the SoMe curriculum to guide best practices further, ensure equity and inclusivity in digital spaces, and tailor the use of these spaces to individual learners.
Finally, many educators would support that being visible on SoMe leads to career opportunities. But how much and in what way? Longitudinal studies of junior faculty who are both highly visible and invisible in SoMe offer an interesting, albeit confounded, way to begin understanding SoMe's value from a networking and mentoring perspective.
SoMe teaching has the potential to revolutionize teaching and the scholarship of education. However, work is needed within neurology to establish validity, impact, and acceptance of SoMe as a scholastic achievement.
Acknowledgments
We want to thank Rebecca Fasano for allowing us to use her tweet as an example.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jessica Goldstein https://orcid.org/0000-0003-1428-5345
Jaclyn M. Martindale https://orcid.org/0000-0002-4919-8850
Scott Otallah https://orcid.org/0000-0003-0316-6121
References
- 1.Bernstein E, Bhardwaj N, Pfoh ER, Yudelevich E. A nationwide survey of educational resource utilization and perception among internal medicine residents. J Gen Intern Med. 2021;36(6):1598‐1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalnow A, Beck-Esmay J, Riddell J, et al. Continuing medical education delivery preferences among physicians and advanced practice providers in emergency medicine. Cureus. 2021;13(12):e20406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simpson D, Marcdante K, Souza KH, Anderson A, Holmboe E. Job roles of the 2025 medical educator. J Grad Med Educ. 2018;10(3):243‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eno C. Milestones guidebook for residents and fellows. 2020.
- 5.De Gagne JC, Park HK, Hall K, Woodward A, Yamane S, Kim SS. Microlearning in health professions education: Scoping review. JMIR Med Educ. 2019;5(2):e13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han E-R, Yeo S, Kim M-J, Lee Y-H, Park K-H, Roh H. Medical education trends for future physicians in advanced technology and artificial intelligence: An integrative review. BMC Med Educ. 2019;19(1):460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plch L. Perception of technology-enhanced learning by medical students: An integrative review. Med Sci Educ. 2020;30(4):1707‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandrone S, Albert DVF, Dunham SR, et al. Training in neurology: How lessons learned on teaching, well-being, and telemedicine during the COVID-19 pandemic can shape the future of neurology education. Neurology. 2021;96(24):e3007‐e3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chhetri SK. E-learning in neurology education: Principles, opportunities, and challenges in combating neurophobia. J Clin Neurosci. 2017;44:80‐83. [DOI] [PubMed] [Google Scholar]
- 10.Latif MZ, Hussain I, Saeed R, Qureshi MA, Maqsood U. Use of smart phones and social media in medical education: Trends, advantages, challenges and barriers. Acta Inform Med. 2019;27(2):133‐138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheng Y-T, Liu DR, Wang VJ. Teaching splinting techniques using a just-in-time training instructional video. Pediatr Emerg Care. 2017;33(3):166‐170. [DOI] [PubMed] [Google Scholar]
- 12.Buchem I, Hamelmann H. Microlearning: a strategy for ongoing professional development. 2010.
- 13.Trivedi S, Saunders S, Rodman A. Strategies for designing a health professions digital education curriculum. Clin Teach. 2021;18(4):336‐340. [DOI] [PubMed] [Google Scholar]
- 14.Martindale JM, Goldstein J, Xixis K, et al. Be in the digital room where it happens, part I: Tweeting & technology for career development. Child Neurol Open. 2022;9:2329048X221106843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellaway R. Chapter 10: technology-enhanced learning. 3rd ed. Association for the Study of Medical Education (ASME): John Wiley & Sons Ltd; 2019. [Google Scholar]
- 16.D'Souza F, Shah S, Oki O, Scrivens L, Guckian J. Social media: Medical education's double-edged sword. Future Healthc J. 2021;8(2):e307‐e310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dhar P, Rocks T, Samarasinghe RM, Stephenson G, Smith C. Augmented reality in medical education: Students’ experiences and learning outcomes. Med Educ Online. 2021;26(1):1953953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandrone S, Carlson CE. Future of neurology & technology: Virtual and augmented reality in neurology and neuroscience education: Applications and curricular strategies. Neurology. 2021;97(15):740-744. [DOI] [PubMed] [Google Scholar]
- 19.Zackoff MW, Real FJ, Abramson EL, Li ST, Klein MD, Gusic ME. Enhancing educational scholarship through conceptual frameworks: A challenge and roadmap for medical educators. Acad Pediatr. 2019;19(2):135‐141. [DOI] [PubMed] [Google Scholar]
- 20.Flynn L, Jalali A, Moreau KA. Learning theory and its application to the use of social media in medical education. Postgrad Med J. 2015;91(1080):556‐560. [DOI] [PubMed] [Google Scholar]
- 21.Mann KV. Theoretical perspectives in medical education: Past experience and future possibilities. Med Educ. 2011;45(1):60‐68. [DOI] [PubMed] [Google Scholar]
- 22.Goldie JGS. Connectivism: A knowledge learning theory for the digital age? Med Teach. 2016;38(10):1‐6. [DOI] [PubMed] [Google Scholar]
- 23.Buckley H, Steinert Y, Regehr G, Nimmon L. When I say … community of practice. Med Educ. 2019;53(8):763‐765. [DOI] [PubMed] [Google Scholar]
- 24.Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: Implications for medical education. Acad Med. 2018;93(2):185‐191. [DOI] [PubMed] [Google Scholar]
- 25.Li LC, Grimshaw JM, Nielsen C, Judd M, Coyte PC, Graham ID. Evolution of Wenger's concept of community of practice. Implement Sci. 2009;4(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaw L, Jazayeri D, Kiegaldie D, Morris M. Virtual communities of practice to improve clinical outcomes in healthcare: Protocol for a 10-year scoping review. BMJ Open. 2021;11(7):e046998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roland D, Spurr J, Cabrera D. Preliminary evidence for the emergence of a health care online community of practice: Using a netnographic framework for Twitter hashtag analytics. J Med Internet Res. 2017;19(7):e252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keir A, Bamat N, Hennebry B, et al. Building a community of practice through social media using the hashtag #neoEBM. PLoS One. 2021;16(5):e0252472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ting DK, Thoma B, Luckett-Gatopoulos S, et al. CanadiEM: Accessing a virtual community of practice to create a Canadian national medical education institution. AEM Educ Train. 2019;3(1):86‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Albin C, Berkowitz AL. #Neurotwitter 101: A tweetorial on creating tweetorials. Pract Neurol. 2021;21(6):539‐540. [DOI] [PubMed] [Google Scholar]
- 31.Breu AC, Abrams HR, Manning KD, Cooper AZ. Tweetorials for medical educators. J Grad Med Educ. 2021;13(5):723‐725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Husain A, Repanshek Z, Singh M, et al. Consensus guidelines for digital scholarship in academic promotion. West J Emerg Med. 2020;21(4):883‐891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shafer S, Johnson MB, Thomas RB, Johnson PT, Fishman EK. Instagram as a vehicle for education: What radiology educators need to know. Acad Radiol. 2018;25(6):819‐822. [DOI] [PubMed] [Google Scholar]
- 34.Douglas NKM, Scholz M, Myers MA, et al. Reviewing the role of Instagram in education: Can a photo sharing application deliver benefits to medical and dental anatomy education? Med Sci Educ. 2019;29(4):1117‐1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daneshjou R, Adamson AS. Twitter journal clubs: Medical education in the era of social media. JAMA Dermatol. 2020;156(7):729‐730. [DOI] [PubMed] [Google Scholar]
- 36.Comp G, Dyer S, Gottlieb M. Is TikTok the next social media frontier for medicine? AEM Educ Train. 2021;5(3):1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blair RA, Caton JB, Hamnvik OR. A flipped classroom in graduate medical education. Clin Teach. 2020;17(2):195‐199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585‐597. [DOI] [PubMed] [Google Scholar]
- 39.Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med Educ. 2018;18(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thillainadesan J, Le Couteur DG, Haq I, Wilkinson TJ. When I say … microlearning. Med Educ. 2022;56(8):791‐792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Coleman E, O’Connor E. The role of WhatsApp® in medical education; a scoping review and instructional design model. BMC Med Educ. 2019;19(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luo T, Freeman C, Stefaniak J. “Like, comment, and share”—professional development through social media in higher education: A systematic review. Educ Technol Res Dev. 2020;68(4):1659‐1683. [Google Scholar]
- 43.Guckian J, Utukuri M, Asif A, et al. Social media in undergraduate medical education: A systematic review. Med Educ. 2021;55(11):1227‐1241. [DOI] [PubMed] [Google Scholar]
- 44.Vukušić Rukavina T, Viskić J, Machala Poplašen L, et al. Dangers and benefits of social media on E-professionalism of health care professionals: Scoping review. J Med Internet Res. 2021;23(11):e25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sterling M, Leung P, Wright D, Bishop TF. The use of social Media in graduate medical education: A systematic review. Acad Med. 2017;92(7):1043‐1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sherbino J, Arora VM, Van Melle E, Rogers R, Frank JR, Holmboe ES. Criteria for social media-based scholarship in health professions education. Postgrad Med J. 2015;91(1080):551‐555. [DOI] [PubMed] [Google Scholar]
- 47.Breu AC, Cooper AZ. Tweetorials: Digital scholarship deserving of inclusion in promotion portfolios. Med Teach. 2022;44(4):450‐452. [DOI] [PubMed] [Google Scholar]
- 48.Cabrera D, Roy D, Chisolm MS. Social media scholarship and alternative metrics for academic promotion and tenure. J Am Coll Radiol. 2018;15(1, Part B):135‐141. [DOI] [PubMed] [Google Scholar]
- 49.Acquaviva KD, Mugele J, Abadilla N, et al. Documenting social media engagement as scholarship: A new model for assessing academic accomplishment for the health professions. J Med Internet Res. 2020;22(12):e25070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cabrera D, Vartabedian BS, Spinner RJ, Jordan BL, Aase LA, Timimi FK. More than likes and tweets: Creating social Media portfolios for academic promotion and tenure. J Grad Med Educ. 2017;9(4):421‐425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zinchuk AV, Flanagan EP, Tubridy NJ, Miller WA, McCullough LD. Attitudes of US medical trainees towards neurology education: “Neurophobia” - a global issue. BMC Med Educ. 2010;10(2010):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Abulaban AA, Obeid TH, Algahtani HA, et al. Neurophobia among medical students. Neurosciences (Riyadh). 2015;20(1):37‐40. [PMC free article] [PubMed] [Google Scholar]
- 53.Majersik JJ, Ahmed A, Chen IA, et al. A shortage of neurologists we must act now: A report from the AAN 2019 transforming leaders program. Neurology. 2021;96(24):1122-1134. [DOI] [PubMed] [Google Scholar]
- 54.Burton A. How do we fix the shortage of neurologists? Lancet Neurol. 2018;17(6):502‐503. [DOI] [PubMed] [Google Scholar]
- 55.Abushouk AI, Duc NM. Curing neurophobia in medical schools: Evidence-based strategies. Med Educ Online. 2016;21:32476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weber DJ, Albert DVF, Aravamuthan BR, Bernson-Leung ME, Bhatti D, Milligan TA. Training in neurology: Rapid implementation of cross-institutional neurology resident education in the time of COVID-19. Neurology. 2020;95(19):883‐886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodman A, Abrams HR, Watto M, et al. Medical podcasting in low- and middle-income countries: A needs assessment and vision for the future. Teach Learn Med. 2021;33(4):416‐422. [DOI] [PubMed] [Google Scholar]
- 58.Alemán MJ, Nematollahi S, Berkowitz AL. Expanding global access to neurology education. JAMA Neurol. 2021;78(10):1173‐1174. [DOI] [PubMed] [Google Scholar]
- 59.Katz M, Nandi N. Social media and medical education in the context of the COVID-19 pandemic: Scoping review. JMIR Med Educ. 2021;7(2):e25892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maudsley G, Taylor D, Allam O, Garner J, Calinici T, Linkman K. A Best Evidence Medical Education (BEME) systematic review of: What works best for health professions students using mobile (hand-held) devices for educational support on clinical placements? BEME Guide No. 52. Med Teach. 2019;41(2):125‐140. [DOI] [PubMed] [Google Scholar]
- 61.Deutsch K, Gaines JK, Hill JR, Nuss MA. Ipad experience during clinical rotations from seven medical schools in the United States: Lessons learned. Med Teach. 2016;38(11):1152‐1156. [DOI] [PubMed] [Google Scholar]
- 62.Krishnan K, Thoma B, Trueger NS, Lin M, Chan TM. Gestalt assessment of online educational resources may not be sufficiently reliable and consistent. Perspect Med Educ. 2017;6(2):91‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang E, Trad N, Corty R, Zohrob D, Trivedi S, Rodman A. How podcasts teach: A comprehensive analysis of the didactic methods of the top hundred medical podcasts. Med Teach. 2022;44(10):1146‐1150. [DOI] [PubMed] [Google Scholar]
- 64.Park JH, Christman MP, Linos E, Rieder EA. Dermatology on Instagram: An analysis of hashtags. J Drugs Dermatol. 2018;17(4):482‐484. [PMC free article] [PubMed] [Google Scholar]
- 65.Cooper AZ, Rodman A, Simpson D. Visual media in medical education. J Grad Med Educ. 2021;13(3):417‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Trivedi SP, Chin A, Ibrahim A, Ou A. Infographics and visual abstracts. J Grad Med Educ. 2021;13(4):581‐582.34434520 [Google Scholar]
- 67.Berk J, Watto M, Williams P. Twelve tips for creating a medical education podcast. Med Teach. 2020;42(11):1221‐1227. [DOI] [PubMed] [Google Scholar]
- 68.Ramakrishnan M, Sparks MA, Farouk SS. Training the public physician: The nephrology social media collective internship. Semin Nephrol. 2020;40(3):320‐327. [DOI] [PubMed] [Google Scholar]
- 69.Elson NC, Le DT, Johnson MD, et al. Characteristics of general surgery social media influencers on Twitter. Am Surg. 2021;87(3):492‐498. [DOI] [PubMed] [Google Scholar]
- 70.Riccio I, Dumont AS, Wang A. The top 100 social media influencers in neurosurgery on Twitter. Interdiscip Neurosurg. 2022;29(2022):101545. [Google Scholar]
- 71.Glassick CE, Huber MT, Maeroff GI. Scholarship assessed: evaluation of the professoriate. Jossey-Bass; 1997. [Google Scholar]
- 72.Hutchings P, Shulman LS. The scholarship of teaching: New elaborations, new developments. Change: Magazine Higher Learn. 1999;31(5):10‐15. [Google Scholar]
- 73.Kirkpatrick D. The four levels of evaluation: measurement and evaluation. American Society for Training & Development; 2007. [Google Scholar]