Abstract
Introduction
Cervical disc arthroplasty (CDA) has been established as an effective treatment for cervical disc degeneration or herniation in the general population. Return to sport (RTS) outcomes in athletes remain unclear.
Objective
The purpose of this review was to evaluate RTS following single-level, multi-level, or hybrid CDA, with additional return to activity context provided by return to duty (RTD) outcomes in active-duty military.
Methods
Medline, Embase, and Cochrane were searched through August 2022 for studies that reported RTS/RTD after CDA in athletic or active-duty populations. Data was extracted on the following topics: surgical failures/reoperations, surgical complications, RTS/RTD, and postoperative time to RTS/RTD.
Results
Thirteen papers covering 56 athletes and 323 active-duty members were included. Athletes were 59% male with a mean age of 39.8 years and active-duty members were 84% male with a mean age of 40.9 years. Only 1 of 151 cases required reoperation and only 6 instances of surgical complications were reported. Classified as return to general sporting activity, RTS was observed in 100% of patients (n = 51/51) after an average of 10.1 weeks to training and 30.5 weeks to competition. RTD was observed in 88% of patients (n = 268/304) after an average of 11.1 weeks. Average follow-up was 53.1 months for athletes and 13.4 months for the active-duty population.
Conclusion
CDA displays excellent RTS and RTD rates in physically demanding populations at rates superior or equivalent to alternative treatments. Surgeons should consider these findings when determining the optimal cervical disc treatment approach in active patients.
Keywords: Cervical disc replacement, Cervical disc arthroplasty, Return to sport, Return to duty
Highlights
-
•
Systematic review identified 13 studies with 56 athletes and 323 active-duty service members with cervical disc arthroplasty.
-
•
Only 1 of 151 reported cases required reoperation and 6 of these reported surgical complications.
-
•
Return to Sport (RTS) observed in 100% of athletes (n=51/51); Return to Duty (RTD) observed in 88% of military (n=268/304).
1. Introduction
Cervical disc arthroplasty (CDA) is an effective operative treatment for cervical radiculopathy secondary to disc herniation or spondylosis.1,2 Prior to the development of CDA, cervical spondylosis was treated with anterior cervical discectomy and fusion (ACDF) and disc herniation with either ACDF or posterior foraminotomy (PF). Both procedures have been previously established to produce good clinical outcomes in a general population.3, 4, 5, 6 CDA, however, consists of replacing the pathological disc with an artificial disc, and thus eliminates the need for vertebral fusion or foraminotomy. Compared to the commonly used ACDF, CDA trials produced better or equivalent surgical outcomes with respect to rates of operative success, improvement of symptoms, and restoration of function in the general population.1,2,7,8 While the fusion procedure leads to a subsequent loss of joint space motion, CDA maintains joint space motion and is associated with lower risks of degenerative changes adjacent to the implant.9, 10, 11
Although CDA has been deemed effective for the general population, athletes require unique treatment considerations with return to play as a primary goal.12 Long term spinal flexibility, reaction times, and paraspinal muscle strength after CDA may effect key outcomes for active patients such as rate of return to sport, career length, and performance, each of which are not critical to the general patient population.6,13 Further, the type of sport being played may be associated with better or worse outcomes.12 Similar to competitive athletes, active-duty military are also exposed to increased physical demands and elevated vertebral forces which introduce unique circumstances when evaluating surgical outcomes.14 Therefore, CDA outcomes in active-duty military populations may help guide treatment decisions for athletes.12
Operative management for cervical disc pathology in athletic and active-duty military populations has previously been established as effective, but insufficient data exists regarding CDA.15 ACDF and PF both showed significant improvements in return to sport (RTS) rates compared to nonoperative management in professional American football players, while also allowing longer athletic careers post-surgery.13 ACDF and PF have been established as viable options for management of cervical disc herniations in professional athletes, with PF leading to quicker and higher rates of RTS but higher reoperation rates than ACDF.6,15 Prior studies have shown successful return to duty (RTD) outcomes in military populations after CDA,16,17 and one study found CDA to lead to quicker RTD as compared to ACDF.14
To our knowledge, no systematic review has evaluated return to activity outcomes in athletes and active-duty military following CDA. While a prior review attempted to compare CDA, ACDF, and PF for cervical disc herniations in professional athletes, insufficient evidence was available for patients undergoing CDA.15 This systematic review aims to evaluate CDA outcomes associated with return to sport or duty in athletes and active duty military, respectively, with the intent of providing more information to improve physicians’ decision making when treating active patients with cervical disc pathologies.
2. Materials and methods
2.1. Literature and database search
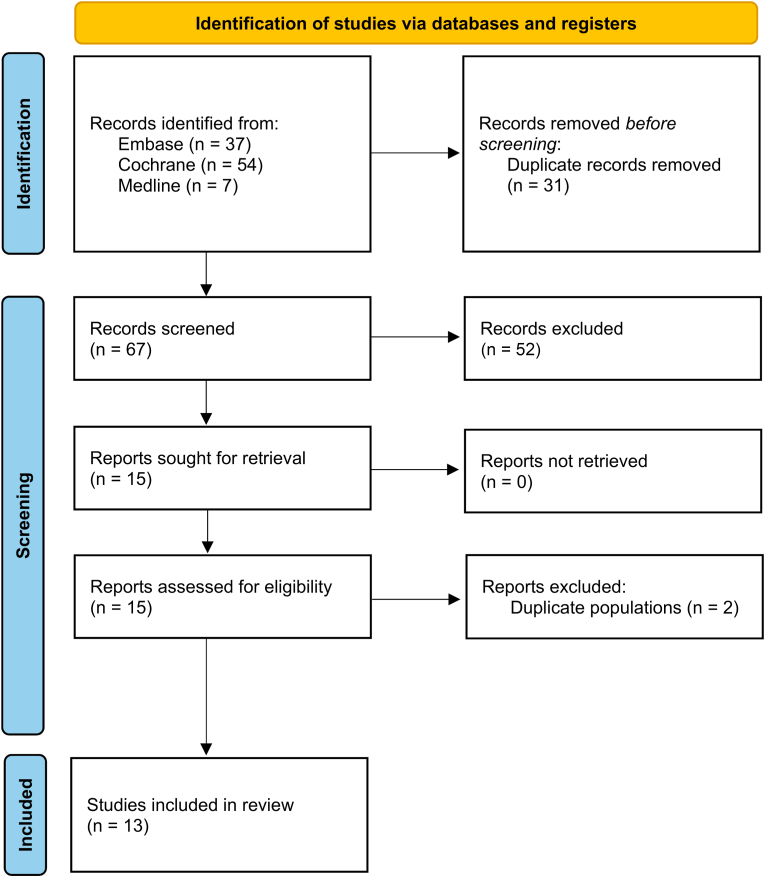
A systematic search of peer-reviewed, published literature was conducted with a research librarian in Medline (Ovid), Embase (Ovid), and Cochrane from inception of the database to August 2022. The search consisted of a combination of keywords and controlled vocabulary for the following concepts: cervical disc arthroplasty, athletes, active-duty military, return to sport, and return to duty. The full details of the search strategy for Medline, Embase, and Cochrane can be seen in Appendices A, Table A.1, Table A.2, Table A.3, respectively. All identified records were imported into Endnote reference management software (Clarivate, https://endnote.com/) and duplicate references were removed (Fig. 1). The remaining references were exported and uploaded to Rayyan (Rayyan, https://www.rayyan.ai/) for collaboration of manual screening. The literature search and subsequent review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting standards.18
Fig. 1.
PRISMA 2020 flow diagram for systematic reviews which included searches of databases and registers only.
2.2. Eligibility criteria and study selection
Two blind reviewers (CN, CR) manually screened titles and abstracts to identify records that primarily investigated cervical disc arthroplasty and return to sport or duty outcomes in athletic or active-duty military populations (Fig. 1). Studies investing single level, multi-level, or hybrid CDA were all included. Case reports, case series, cohort studies, and randomized controlled trials published prior to database search were included for evaluated for inclusion; abstracts, reviews, technical notes, letters to the editor, and surgical technique papers were not included. Studies were excluded if they did not directly report return to sport in athletes or return to duty in active-duty service members. Additionally, reviews, cadaveric studies, non-human studies, and non-English studies were excluded. Included records underwent a full-text review for the same criteria to exclude additional studies as needed. Any conflicts between reviewers were resolved through third-party consultations with a senior author (JS). Full details of the protocol for this systematic review were prospectively registered on PROSPERO and may be accessed at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=353235.
2.3. Methodological quality assessment
Methodological quality of included studies was assessed using the JBI protocol checklist for cohort studies, case series, and case reports, respectively.19 Each criterion possesses a unique set of questions to evaluate the validity of methods, quality of analysis and presentation for each study type. Two reviewers (CR, CN) each reviewed the included studies and discussed discrepancies to reach a consensus. Any disputes were settled by a third reviewer (JS).
2.4. Data extraction
For each included study, one of two authors (CN, CR) independently extracted data into a Google Sheets spreadsheet (Google LLC, Mountain View, California, United States). A second review of the data extraction was performed by the opposite reviewer, with any discrepancies between reviewers being resolved through third-party consultation with a senior author (JS). Data points for extraction from each study included the following: study type, level of evidence, number of cases, sex, mean age, athlete or active-duty, sport and level, military occupation, surgical indication, implant type, follow-up duration, surgical failures or reoperations, surgical complications, RTS or RTD, and postoperative time to RTS or RTD.
2.5. Statistical analysis
Categorical variables were summated and presented as counts or proportions, and continuous variables were calculated as patient means. Outcomes of interest were tabulated to highlight the outcomes of individual reports. A meta-analysis was not performed, and individual participant data was not collected.
3. Results
3.1. Literature search and screening
The initial search of the three databases yielded a combined total of 67 studies after duplicates were removed. After screening titles and abstracts, 15 records were found that met the initial review criteria for inclusion. Of the included studies, 2 were removed after full-text screening due to duplicate subject populations, leaving 13 reports for data extraction. Data extraction was performed on 12 studies with Level IV evidence, of which 3 were case reports and 9 were case series, and 1 retrospective cohort study with Level III evidence. All results were reported per the PRISMA reporting standards.18
3.2. Methodological quality assessment
Two reviewers (CN, CR) analyzed studies according to JBI Clinical Appraisal tools for each study type. Three case reports20, 21, 22 had a mean score of 8 out of 8. Nine case series6,10,16,17,23, 24, 25, 26, 27, 28, 29 had a mean score of 9.1 out of 10. The only retrospective cohort study14 had a score of 11 out of 11. All 13 studies were determined to have adequate methodology to be included in the review.
3.3. Patient demographics
Six studies focused on athletes and included 56 cases of cervical disc arthroplasty (Table 1). There were 33 males and 23 females with an average age of 39.8 years. The sports participation included the following: running (n = 18, 32%), mountain sports (n = 12, 21%), unspecified ball sports (n = 11, 20%), cycling (n = 10, 18%), general fitness (n = 9, 16%), Nordic walking (n = 6, 11%), surfing/sailing (n = 3, 5%), baseball (n = 3, 5%), and other (n = 13, 23%). Subject level of sports participation consisted of 6 professional (11%), 20 semiprofessional (36%), 25 recreational (45%), and 5 low level (9%) athletes.
Table 1.
Details, patient demographics, surgery, and return to sport in athlete studies.
| Study | LoE | N | M/F | Mean Age | Sport | Level of Sport | Surgical Indication | Levels | Implant | Avg. FU (months) | Reop. | Surgical Comp. | RTS | Avg. Time to RTS (weeks) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lindi-Sugino (2021)20 | Case Report (IV) | 1 | 0/1 | 34 | Kickboxing (1) | Professional (1) | Disc Herniation with Radiculopathy | Single (1) | – | 84 | 0/1 | None | 1/1 | Training: 3 Competition: 13 |
| Mai (2018)6 | Case Series (IV) | 2 | 2/0 | Unclear | Baseball (2) | Professional (2) | Disc Herniation | – | – | 73 | 0/2 | – | 2/2 | Competition: 36.2 |
| Reinke (2017)10 | Case Series (IV) | 50 | 28/22 | 40a (21–56) | Running (16), Mountain Sports (12), Ball Sports (11), Cycling (10), Fitness (9), Swimming (8), Nordic Walking (6), Surfing/Sailing (3), Other (13) | Professional (2), Semiprofessional (20), Recreational (24), Low Level (5) | Disc Herniation with Radiculopathy | Single (50) | Prestige LP (50) | 53 (26–96) | 0/50 | Unclear | 45/45 | Training: 10 (1–80) Competition (n = 7): 32 (8–68) |
| Roberts (2011)26 | Case Series (IV) | 1 | 1/0 | 31 | Baseball (1) | Professional (1) | Disc Herniation | Single (1) | – | – | 0/1 | None | 1/1 | – |
| Shah (2021)27 | Case Series (IV) | 1 | 1/0 | Unclear | Running (1) | Professional (1) | Not Reported | Single (1) | – | 45 | 0/1 | None | 1/1 | Training: 10 Competition: 26 |
| Siddiqui (2015)21 | Case Report (IV) | 1 | 1/0 | 47 | Running (1) | Recreational (1) | Radiculopathy | Multi (1) | Prestige LP (50) | 24 | 0/1 | Dural Tear (1) | 1/1 | Training: 26 |
Abbreviations: LoE, level of evidence; N, number of cases; M/F, male to female ratio; Avg., average; FU, follow-up; Reop., reoperation; Comp., complications; RTS, return to sport.
Median.
Seven active-duty military studies were included with 323 service members and an average age of 40.9 years (Table 2). Male and female demographic data was only available for 95 patients of which there were 80 males and 15 females. Military occupation was reported for 114 patients as follows: combat arms (n = 28, 25%), combat support (n = 14, 12%), combat service support (n = 34, 30%), fighter pilot (n = 19, 17%), Navy SEAL (n = 7, 6%), high ranking officer (n = 3, 2%), Army helicopter pilot (n = 1, 1%), Marine (n = 1, 1%), and landing craft air cushioning engineer (n = 1, 1%).
Table 2.
Details, patient demographics, surgery, and return to duty in active-duty military studies.
| Study | LoE | N | M/F | Mean Age | Military Occupation | Surgical Indication | Levels | Implant | Avg. FU (months) | Reoperations | Surgical Complications | RTD | Avg. Time to RTD (weeks) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cleveland (2015)16 | Case Series (IV) | 34 | 28/6 | 36.3 (6.8) | Combat Arms (14), Combat Support (6), Combat Service Support (14) | – | Single (34) | ProDisc-C (23), Prestige (11) | 21.4 (10.1) | 0/34 | Dural Tear (1), Adjacent Level Fusion (2) | 30/34 | 8.5 (8.0) |
| Cleveland (2016)23 | Case Series (IV) | 30 | 24/6 | 39.7 (8.0) | Combat Arms (9), Combat Support (5), Combat Service Support (16) | – | Hybrid (30) | ProDisc-C (29), Prestige (1) | 16.1 (7.7) | 0/30 | Vocal Cord Injury (1) | 24/30 | 15.6 (14.4) |
| Cody (2014)24 | Case Series (IV) | 209 | Unclear | 42.1 (8.4) | – | Myelopathy, Radiculopathy and Myeloradiculopathy, or Neck Pain | Unclear | Unclear | 11.2 (11.0) | Unclear | Unclear | 189/209 | – |
| Miller (2018)25 | Case Series (IV) | 19 | Unclear | 41.7 (32.7–52.5) | Fighter Pilot (19) | Spondylosis | Single (14), Multi (3), Hybrid (2) | Bryan (5), Prestige (9), Prestige LP (3) ProDisc-C (1) |
12.3 | Unclear | Unclear | 9/19a | 39.6a |
| Spinelli (2016)22 | Case Report (IV) | 1 | 1/0 | 36 | Army Helicopter Pilot (1) | Radiculopathy, Spondylosis, or Disc Herniation | Single (1) | Prestige (1) | 12 | 0/1 | None | 1/1 | – |
| Tumialán (2010)14 | Retrospective Cohort (III) | 12 | 12/0 | 36.5 | Navy SEAL (7), Marine (1), Landing Craft Air Cushioning Engineer (1), High Ranking Officer (3) | Herniation, Spondylosis, or Loss of Disc Height | Single (12) | ProDisc-C (12) | 12.2 (3–26) | 1/12 | None | 12/12 | 10.3 (7–13) |
| Zarkadis (2017)29 | Case Series (IV) | 18 | 15/3 | 40.0 (5.8) | Combat Arms (5), Combat Support (3), Combat Service Support (4) | Spondylosis with Radiculopathy | Multi (18) | Mobi-C (13), ProDisc-C (4), Secure-C (1) | 21.4 (11.1) | 0/18 | Upper Extremity Paresthesia (1) | 12/18 | 9.6 (11.7) |
Abbreviations: LoE, level of evidence; N, number of cases; M/F, male to female ratio; Avg., average; FU, follow-up; Reop., reoperation; Comp., complications; RTD, return to duty.
Reported as return to flight duty, which includes stricter requirements than RTD.
3.4. Surgical indications, levels, and implants
In the athlete studies, surgical indication was reported in all but one study27 (Table 1). Two studies reported disc herniation as the indication for surgery6,26 and two studies reported disc herniation with radiculopathy as surgical indication.10,20 One study reported only radiculopathy as the indication for surgery21 and the remaining study did not specify a surgical indication.27 Implant types were reported for 51 out of 56 patients with all 51 operations using Prestige LP implants. Of these procedures, 53 (95%) were single level CDA, one (2%) was multi-level CDA, and one (2%) procedure was not specified. Average follow-up duration was 53.1 months postoperatively.
In the military studies, surgical indications included combinations of disc herniation, spondylosis, radiculopathy, myelopathy, myeloradiculopathy, loss of disc height, or neck pain (Table 2). Implant types included: ProDisc-C (n = 69, 61%), Prestige (n = 22, 19%), Mobi-C (n = 13, 12%), Bryan (n = 5, 4%), Prestige LP (n = 3, 3%), and Secure-C (n = 1). Amongst these procedures, 61 (54%) were single level arthroplasty, 21 (18%) were multi-level, and 32 (28%) were hybrid. Average follow-up duration was 13.4 months postoperatively.
3.5. Reoperations and surgical complications
In total, only 1 out of 151 cases required reoperation due to a failed CDA (Table 3). The single reoperation case occurred in an active-duty patient who displayed progressive osteolysis from the rostral keel and required removal of the implant and conversion to ACDF. The authors suspect this complication was due to an immune-mediated reaction to the device.14 Surgical complications were reported in 9 studies with 99 patients (Table 1, Table 2). Complications included Dural tear (2, 2%), vocal cord injury (1, 1%), upper extremity paresthesia (1, 1%), and subsequent adjacent level fusion (2, 2%).
Table 3.
Summary outcomes after cervical disc arthroplasty.
| Outcome | Athletes | Active-Duty |
|---|---|---|
| Reoperation (%) | 0/56 (0%) | 1/95 (1.1%) |
| RTS/RTD (%) | 51/51 (100%) | 268/304 (88%)a |
| Time to RTS/RTD (weeks) | Training: 10.1 Competition: 30.5 |
11.1a |
Abbreviations: RTS, return to sport; RTD, return to duty.
Does not include 19 fighter pilots as Return to Flight Duty involves stricter requirements than typical RTD.
3.6. Return to sport
Return to sport was classified as return to general sporting activity, regardless of return to preinjury level of performance. All 51 (100%) athletes returned to sport following CDA (Table 3). The average time to RTS was 10.1 weeks for training and 30.5 weeks for competition.
3.7. Return to duty
277 of 323 (86%) active-duty service members achieved RTD at an average of 14.1 weeks (Table 2). However, one study25 included all fighter pilots and subsequently reported return to flight duty rather than just RTD. Return to flight duty requires a stricter set of criteria to be achieved than does the typical RTD.25 Removing these cases from the analysis produced a RTD rate of 268 out of 304 (88%) active-duty service members at an average of 11.1 weeks (Table 3).
4. Discussion
The primary objective of this systematic review was to evaluate return to sport in athletes after cervical disc arthroplasty, while also providing additional context with return to duty in active-duty military. Our review of 13 studies produced exceptional return to activity rates with a perfect 100% RTS rate in athletes and an 88% RTD rate in active-duty service members. Athletes were able to return to training at 10.1 weeks (2.3 months) and competition at 30.5 weeks (6.9 months) while active-duty members returned at 11.1 weeks (2.6 months) on average.
These results indicate equivalent or better return to sport when compared to alternative treatments, ACDF, PF, and nonoperative management. Leider et al.15 conducted a SR of cervical disc surgery in elite athletes and reported return to play (RTP), or return to competition, rates ranging from 68% to 87% following ACDF or PF. Mai et al.6 found 68% of National Football League (NFL), Major League Baseball (MLB), National Hockey League (NHL), and National Basketball Association (NBA) players returned to play for 2.6 years following ACDF and 83% RTP for 4.3 years following PF. Hsu13 showed 72% RTP in NFL players following ACDF or PF compared to 46% RTP with nonoperative management. Watkins et al.30 investigated single level ACDF in NFL, NHL, MLB, and NBA players elicited 81% RTP with return at 9.5 months postoperatively. Maroon et al.31 found an 87% RTS rate in NFL players and professional wrestlers after ACDF. Tumialán et al.32 found quicker RTD after PF than ACDF in an active-duty population with RTD at 4.8 weeks and 19.6 weeks, respectively.
Our findings also produced similar return to sport and duty rates as lumbar disc surgery. In professional athletes with lumbar discectomies, RTS rates have ranged from 74% to 89%.10,31,33, 34, 35 Similarly, young athletes returned to sport at a 94% rate after lumbar disc arthroplasty and ultimately achieved peak performance after 5.2 months.10,36 Lumbar disc arthroplasty RTD rates have been reported as slightly lower than RTS rates at 83% after an average of 22.6 weeks.10,14 The results of our study similarly found comparable RTS and RTD rates also with RTD being lower than of RTS. The active-duty cohort, however, returned to duty at a substantially quicker rate, 11.1 weeks, than reported in the lumbar arthroplasty study.
The RTS data presented in this study needs to be taken into context when comparing rates to prior research, however. We defined RTS as a return to general sporting activity, without requiring a return to preinjury level of play. RTS is reported variably across sports medicine literature, with a majority of studies defining RTS as a return to competition and many other studies requiring return to preinjury competition level or simply a return to general training.37 Across the included athlete studies, those that included only professional athletes tended to report return to play, whereas those with lower-level athletes utilized a more general RTS definition. Return to competitive play of the professional baseball players in Mai et al.,6 for example, is likely not equivalent to a recreational distance runner returning to training.21 Postoperative sport performance data would have helped to elucidate these differences, but only one study6 reported meaningful performance metrics, reporting a 5.8% increase in postoperative statistical performance.
Much like the level of sport needs to be taken into consideration when interpreting this data, the sport and position played should be considered when making individual RTS recommendations. As this was not an individual participant data (IPD) study, we did not attempt to make any conclusions about sport- or position-specific outcomes following CDA. While the included athletes participated in a variety of sports ranging from recreational runners to a professional kickboxer, more research is needed to determine whether CDA is more or less effective for different types of athletes. Practitioners are still advised to evaluate each athlete with regards to their unique physical demands, especially when treating contact sport athletes who are routinely at risk of head and neck trauma.12 Prior studies have suggested differing cervical spine surgery outcomes depending on sport or position. NFL defensive backs had worse performance outcomes than other position groups, only returning for an average of 10 games over 1.2 years postoperatively.13,15 A group of MLB pitchers were able to RTP after ACDF or CDA, but upon return, pitched significantly fewer innings per year.15,26 Similarly, all 8 starting pitchers returned to play in Mai et al.6 after cervical spine surgery, but 3 of the 8 moved to relief roles post-surgery.15
Active-duty service members were included in this study to provide a secondary patient population that, similar to athletes, are exposed to vertebral column forces that would not be expected in a less active, civilian population. While RTD involves a return to physical activity, it is not equivalent to RTS, and the differing criteria likely explains the lower RTD than RTS rates in our findings. For example, Tumialán et al.14 described their RTD recommendations as return to nonimpact training at patient's preference, light impact and weight training in the 2nd postoperative month, and high impact training by the 3rd month. To be cleared for RTD, patients had to show preservation of motion on flexion/extension radiographs, complete resolution of symptoms, and absence of hardware complications. In most cases, RTD involves a higher standard to be met and requires all patients to meet extreme physical demands such as parachute jumping or high-impact water entries.14 A recent study advised against using RTD as a surrogate marker for RTS, citing that amongst RTD patients, roughly two-thirds reported lower levels of activity and one-third reported being nondeployable.38 However, other authors have acknowledged the similar physical demands amongst active-duty military and elite athletes,12,39 therefore making RTD rates at least reasonable to consider when treating athletes.
The low reoperation rate (1%) and minimally reported surgical complications suggest successful CDA surgical outcomes in active patients. This compares to the 1% reoperation rate observed in professional athletes following ACDF, and substantially lower than a 46.2% reoperation rate seen after PF.6,12 However, with an average follow-up duration of only 13.4 months in the military population and 53.1 months in the athlete population, it was not possible to come to conclusions regarding the long-term efficacy of the disc implants in these populations. Regarding surgical complications, a small minority of patients presented with Dural tears or vocal cord injury, while two patients required adjacent level fusions. Prior research has established CDA as presenting with lower risks of adjacent disc degeneration, likely due to the restoration of range of motion at the disc space that is eliminated in fusion surgeries.9, 10, 11
This study is largely limited by the heterogeneity of available patient data between studies. Some studies grouped outcome data between active and non-active populations or CDA and ACDF together, thus making some data entries unclear. Because of this, many of the analyses were not able to include the entire included patient population. Additionally, the generalizability of the findings is limited by the ages of the patients, particularly in the military studies. The average age in the military studies was almost 40 years and therefore the RTD was likely negatively influenced by age-related factors, such as near retirement. Similarly, the RTS findings are limited by the lack of performance data upon return and broad spectrum of athletic levels included. Further, without individual patient data, the influence of likely confounders, such as age, level(s) of replacement, and implant type could not be determined.
5. Conclusion
Surgical considerations for cervical disc degeneration or herniation in athletes or active-duty military involves a complex decision-making equation that considers not only symptom relief and restoration of function, but also return to activity ability, quickness of return, and long-term postoperative performance. This systematic review displays excellent return to sport and duty after cervical disc arthroplasty at rates equivalent or superior to treatment alternatives previously described in the literature. On average, patients can return to training in less than 3 months, competition in under 7 months, or active duty in under 3 months removed from CDA. Further, the short-term risk of operative failure or surgical complications appears to be low in these physically active populations. While further research is necessary to evaluate longer-term success and postoperative physical performance, surgeons should consider these findings when determining the optimal cervical disc treatment approach in active patients.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
Charles R. Reiter: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Roles/Writing – original draft, Writing – review & editing. Chase T. Nelson: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Roles/Writing – original draft, Writing – review & editing. James R. Satalich: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. Conor N. O'Neill: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. John W. Cyrus: Data curation, Investigation, Methodology, Resources, Software, Writing – review & editing. Robert S. O'Connell: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. Alexander R. Vap: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Declaration of competing interest
None.
Acknowledgments
None.
APPENDIX A.
Table A.1.
Search Strategy for Medline (Ovid) on August 18th, 2022
| ID | Strategy | Hits |
|---|---|---|
| 1 | (athlete or athletes or player or players or sport or sports or athletic or athletics or military personnel or military or armed forces or army or air force or navy or marine or marines or coast guard or service member or service members or active duty).tw. | 362468 |
| 2 | exp sport/or exp athlete/or exp military personnel/ | 256023 |
| 3 | 1 or 2 | 520417 |
| 4 | exp cervical vertebrae/or (cervical or spinal or spine).tw. | 590346 |
| 5 | exp total disc replacement/or (artificial disc* or artificial disk*).tw. | 1307 |
| 6 | ((disc or disk) adj5 (replacement or arthroplasty)).tw. | 2426 |
| 7 | cervical arthroplast*.tw. | 271 |
| 8 | 5 or 6 | 2709 |
| 9 | 4 and 8 | 2001 |
| 10 | 7 or 9 | 2080 |
| 11 | 3 and 10 | 37 |
Table A.2.
Search Strategy for Embase (Ovid) on August 18th, 2022
| ID | Strategy | Hits |
|---|---|---|
| 1 | (athlete or athletes or player or players or sport or sports or athletic or athletics or military personnel or military or armed forces or army or air force or navy or marine or marines or coast guard or service member or service members or active duty).tw. | 423993 |
| 2 | exp sport/or exp athlete/or exp military personnel/ | 238863 |
| 3 | 1 or 2 | 544412 |
| 4 | exp cervical vertebra/or (cervical or spinal or spine).tw. | 754098 |
| 5 | exp total disc replacement/or (artificial disc* or artificial disk*).tw. | 1778 |
| 6 | ((disc or disk) adj5 (replacement or arthroplasty)).tw. | 3423 |
| 7 | cervical arthroplast*.tw. | 409 |
| 8 | 5 or 6 | 3788 |
| 9 | 4 and 8 | 2878 |
| 10 | 7 or 9 | 2998 |
| 11 | 3 and 10 | 54 |
Table A.3.
Search Strategy for Cochrane on August 18th, 2022
| ID | Strategy | Hits |
|---|---|---|
| #1 | MeSH descriptor: [Sports] explode all trees | 17233 |
| #2 | MeSH descriptor: [Athletes] explode all trees | 1165 |
| #3 | MeSH descriptor: [Military Personnel] explode all trees | 1063 |
| #4 | athlete* OR player* OR sport* OR athletic* OR “military personnel” OR military OR “armed forces” OR army OR “air force” OR navy OR marine OR marines OR “coast guard” OR “service member” OR “service members” OR “active duty” | 47515 |
| #5 | #1 OR #2 OR #3 OR #4 | 56627 |
| #6 | ((disc or disk) near/5 (replacement or arthroplasty or arthroplasties)) | 524 |
| #7 | artificial disc or “artificial disk” or “artificial discs” or “artificial disks" | 155 |
| #8 | MeSH descriptor: [Total Disc Replacement] explode all trees | 73 |
| #9 | #6 OR #7 OR #8 | 556 |
| #10 | MeSH descriptor: [Cervical Vertebrae] explode all trees | 1039 |
| #11 | cervical or spinal or spine | 63713 |
| #12 | #10 OR #11 | 63713 |
| #13 | #9 AND #12 | 532 |
| #14 | cervical arthroplasty or “cervical arthroplasties" | 72 |
| #15 | #13 OR #14 | 551 |
| #16 | #15 AND #5 | 9* |
| *7 exported (not protocols) |
References
- 1.Mummaneni P.V., Amin B.Y., Wu J.C., Brodt E.D., Dettori J.R., Sasso R.C. Cervical artificial disc replacement versus fusion in the cervical spine: a systematic review comparing long-term follow-up results from two FDA trials. Evid Base Spine Care J. Feb 2012;3(S1):59–66. doi: 10.1055/s-0031-1298610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sasso R.C., Smucker J.D., Hacker R.J., Heller J.G. Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine. Dec 15 2007;32(26):2933–2940. doi: 10.1097/BRS.0b013e31815d0034. ; discussion 2941-2. [DOI] [PubMed] [Google Scholar]
- 3.Bohlman H.H., Emery S.E., Goodfellow D.B., Jones P.K. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. Sep 1993;75(9):1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Henderson C.M., Hennessy R.G., Shuey H.M., Jr., Shackelford E.G. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery. Nov 1983;13(5):504–512. doi: 10.1227/00006123-198311000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Herkowitz H.N., Kurz L.T., Overholt D.P. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine. Oct 1990;15(10):1026–1030. doi: 10.1097/00007632-199015100-00009. [DOI] [PubMed] [Google Scholar]
- 6.Mai H.T., Chun D.S., Schneider A.D., Hecht A.C., Maroon J.C., Hsu W.K. The difference in clinical outcomes after anterior cervical fusion, disk replacement, and foraminotomy in professional athletes. Clin Spine Surg. Feb 2018;31(1):E80–E84. doi: 10.1097/BSD.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 7.Mummaneni P.V., Burkus J.K., Haid R.W., Traynelis V.C., Zdeblick T.A. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. Mar 2007;6(3):198–209. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 8.Murrey D., Janssen M., Delamarter R., et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. Apr 2009;9(4):275–286. doi: 10.1016/j.spinee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Auerbach J.D., Anakwenze O.A., Milby A.H., Lonner B.S., Balderston R.A. Segmental contribution toward total cervical range of motion: a comparison of cervical disc arthroplasty and fusion. Spine. Dec 1 2011;36(25):E1593–E1599. doi: 10.1097/BRS.0b013e31821cfd47. [DOI] [PubMed] [Google Scholar]
- 10.Reinke A., Behr M., Preuss A., Villard J., Meyer B., Ringel F. Return to sports after cervical total disc replacement. World Neurosurg. Jan 2017;97:241–246. doi: 10.1016/j.wneu.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 11.Rollinghoff M., Zarghooni K., Hackenberg L., Zeh A., Radetzki F., Delank K.S. Quality of life and radiological outcome after cervical cage fusion and cervical disc arthroplasty. Acta Orthop Belg. Jun 2012;78(3):369–375. [PubMed] [Google Scholar]
- 12.Pahapill R.R., Hsu W.K. Controversies in the management of cervical spine conditions in elite athletes. Orthopedics. Jul 1 2019;42(4):e370–e375. doi: 10.3928/01477447-20190624-05. [DOI] [PubMed] [Google Scholar]
- 13.Hsu W.K. Outcomes following nonoperative and operative treatment for cervical disc herniations in National Football League athletes. Spine. May 1 2011;36(10):800–805. doi: 10.1097/BRS.0b013e3181e50651. [DOI] [PubMed] [Google Scholar]
- 14.Tumialan L.M., Ponton R.P., Garvin A., Gluf W.M. Arthroplasty in the military: a preliminary experience with ProDisc-C and ProDisc-L. Neurosurg Focus. May 2010;28(5):E18. doi: 10.3171/2010.1.FOCUS102. [DOI] [PubMed] [Google Scholar]
- 15.Leider J., Piche J.D., Khan M., Aleem I. Return-to-Play outcomes in elite athletes after cervical spine surgery: a systematic review. Sport Health. Sep-Oct 2021;13(5):437–445. doi: 10.1177/19417381211007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cleveland A., Herzog J., Caram P. The occupational impact of single-level cervical disc arthroplasty in an active duty military population. Mil Med. Nov 2015;180(11):1196–1198. doi: 10.7205/MILMED-D-14-00702. [DOI] [PubMed] [Google Scholar]
- 17.Kang D.G., Lehman R.A., Tracey R.W., Cody J.P., Rosner M.K., Bevevino A.J. Outcomes following cervical disc arthroplasty in an active duty military population. J Surg Orthop Adv. Spring. 2013;22(1):10–15. doi: 10.3113/jsoa.2013.0010. [DOI] [PubMed] [Google Scholar]
- 18.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. Mar 29 2021:372. doi: 10.1136/bmj.n71. n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moola S., Munn Z., Tufanaru C., et al. In: JBI Manual for Evidence Synthesis. Aromataris E., Munn Z., editors. JBI; 2020. Chapter 7: systematic reviews of etiology and risk. chap. 7. [Google Scholar]
- 20.Lindi-Sugino R., Hartl R., Klezl Z. Cervical arthroplasty in a professional kick-boxing fighter, 7 years follow-up. Acta Ortop Mex. May-Jun 2021;35(3):282–285. Artroplastia cervical en un luchador profesional de kick-boxing, 7 anos de seguimiento. [PubMed] [Google Scholar]
- 21.Siddiqui A., Wickham N., Hulme C. Painless squeaking following cervical disc replacement: a case report. Internet J Spine Surg. 2015;9:44. doi: 10.14444/2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spinelli J., Neal C.J., Rosner M.K. Performance of cervical arthroplasty at a pseudarthrosed level of a MultiLevel anterior cervical discectomy and fusion: case report. Mil Med. Jun 2016;181(6):e621–e624. doi: 10.7205/MILMED-D-15-00322. [DOI] [PubMed] [Google Scholar]
- 23.Cleveland A., Herzog J., Caram P. Occupational impact of multilevel cervical disease treated with hybrid cervical disc arthroplasty in active duty military population. J Surg Orthop Adv. summer. 2016;25(2):110–113. [PubMed] [Google Scholar]
- 24.Cody J.P., Kang D.G., Tracey R.W., Wagner S.C., Rosner M.K., Lehman R.A., Jr. Outcomes following cervical disc arthroplasty: a retrospective review. J Clin Neurosci. Nov 2014;21(11):1901–1904. doi: 10.1016/j.jocn.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Miller C.A., Boulter J.H., Coughlin D.J., Rosner M.K., Neal C.J., Dirks M.S. Return-to-active-duty rates after anterior cervical spine surgery in military pilots. Neurosurg Focus. Dec 1 2018;45(6):E10. doi: 10.3171/2018.9.FOCUS18380. [DOI] [PubMed] [Google Scholar]
- 26.Roberts D.W., Roc G.J., Hsu W.K. Outcomes of cervical and lumbar disk herniations in Major League Baseball pitchers. Orthopedics. Aug 2011;34(8):602–609. doi: 10.3928/01477447-20110627-23. [DOI] [PubMed] [Google Scholar]
- 27.Shah K., Bharuka A., Gadiya A., Nene A. Assessment of outcomes of spine surgery in Indian athletes involved in high-end contact sports. Asian Spine J. Apr 2021;15(2):192–199. doi: 10.31616/asj.2019.0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tracey R.W., Kang D.G., Cody J.P., Wagner S.C., Rosner M.K., Lehman R.A., Jr. Outcomes of single-level cervical disc arthroplasty versus anterior cervical discectomy and fusion. J Clin Neurosci. Nov 2014;21(11):1905–1908. doi: 10.1016/j.jocn.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Zarkadis N.J., Cleveland A.W., Kusnezov N.A., Dunn J.C., Caram P.M., Herzog J.P. Outcomes following multilevel cervical disc arthroplasty in the young active population. Mil Med. Mar 2017;182(3):e1790–e1794. doi: 10.7205/MILMED-D-16-00085. [DOI] [PubMed] [Google Scholar]
- 30.Watkins RGt, Chang D., Watkins R.G., 3rd Return to play after anterior cervical discectomy and fusion in professional athletes. Orthop J Sports Med. Jun 2018;6(6) doi: 10.1177/2325967118779672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maroon J.C., Bost J.W., Petraglia A.L., et al. Outcomes after anterior cervical discectomy and fusion in professional athletes. Neurosurgery. Jul 2013;73(1):103–112. doi: 10.1227/01.neu.0000429843.68836.91. ; discussion 112. [DOI] [PubMed] [Google Scholar]
- 32.Tumialan L.M., Ponton R.P., Gluf W.M. Management of unilateral cervical radiculopathy in the military: the cost effectiveness of posterior cervical foraminotomy compared with anterior cervical discectomy and fusion. Neurosurg Focus. May 2010;28(5):E17. doi: 10.3171/2010.1.FOCUS09305. [DOI] [PubMed] [Google Scholar]
- 33.Anakwenze O.A., Namdari S., Auerbach J.D., et al. Athletic performance outcomes following lumbar discectomy in professional basketball players. Spine. Apr 1 2010;35(7):825–828. doi: 10.1097/BRS.0b013e3181d3cf45. [DOI] [PubMed] [Google Scholar]
- 34.Hsu W.K., McCarthy K.J., Savage J.W., et al. The Professional Athlete Spine Initiative: outcomes after lumbar disc herniation in 342 elite professional athletes. Spine J. Mar 2011;11(3):180–186. doi: 10.1016/j.spinee.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Savage J.W., Hsu W.K. Statistical performance in National Football League athletes after lumbar discectomy. Clin J Sport Med. Sep 2010;20(5):350–354. doi: 10.1097/JSM.0b013e3181efc259. [DOI] [PubMed] [Google Scholar]
- 36.Siepe C.J., Wiechert K., Khattab M.F., Korge A., Mayer H.M. Total lumbar disc replacement in athletes: clinical results, return to sport and athletic performance. Eur Spine J. Jul 2007;16(7):1001–1013. doi: 10.1007/s00586-006-0257-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doege J., Ayres J.M., Mackay M.J., et al. Defining return to sport: a systematic review. Orthop J Sports Med. Jul 2021;9(7) doi: 10.1177/23259671211009589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zalneraitis B.H., Drayer N.J., Nowak M.J., et al. Is self-reported return to duty an adequate indicator of return to sport and/or return to function in military patients? Clin Orthop Relat Res. Nov 1. 2021;479(11):2411–2418. doi: 10.1097/CORR.0000000000001840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cochran J., Baisden J., Yoganandan N., Pintar F. Effects of treatment for cervical disc degenerative disease in military populations. ASME. 2011;2doi doi: 10.1115/IMECE2011-63919. [DOI] [Google Scholar]