Abstract
This cross-sectional study estimates trends in stroke prevalence representative of the noninstitutionalized civilian population of US adults 20 years and older using data from the 1999 to 2018 National Health and Nutrition Examination Surveys.
Representative estimates of stroke prevalence inform public health interventions and guide resource allocation. There is a need for updated data on stroke prevalence among community-dwelling individuals in the US. We present data from the 1999 to 2018 National Health and Nutrition Examination Surveys (NHANES) to estimate trends in stroke prevalence representative of the noninstitutionalized civilian population of US adults 20 years and older.
Methods
The NHANES is a series of nationally representative cross-sectional surveys administered biennially.1 Participants are selected from among the noninstitutionalized US population using a complex, stratified, multistage, probability-clustered sampling design. This analysis includes all (n = 2197) participants from the 1999-2018 survey cycles 20 years and older who self-reported a history of stroke, ascertained using the question, “Has a doctor or other health professional ever told you that you had a stroke?”2 The NHANES are approved by the National Center for Health Statistics Ethics Review Board.
Data were grouped into 4-year epochs to improve the precision of estimates.1 Within each epoch, stroke prevalence was calculated overall and stratified by sex, self-reported race and ethnicity, and age group. Prevalence estimates were age-standardized to the 2017 to 2018 American Community Survey–Public Use Microdata Sample (ACS-PUMS) using the following age categories: 20 to 39 years, 40 to 59 years, and 60 years or older. We applied our stroke prevalence estimates to the Current Population Surveys and the ACS-PUMS to calculate the number of affected individuals with stroke. P values for linear trend over time were calculated using logistic regression models. In accordance with NHANES recommendations, analyses incorporated survey weights to account for the sampling design and the Taylor series (linearization) method was used to obtain standard errors.1 A 2-tailed P value less than .05 was considered statistically significant, and all analyses were performed using Stata SE version 17 (StataCorp).
Results
From 1999 to 2018, the overall crude and age-standardized prevalence of stroke was 2.84% (95% CI, 2.67-3.02) and 3.10% (95% CI, 2.92-3.29), respectively. This corresponds to an estimated 7.3 million (95% CI, 6.9 million-7.8 million) affected individuals. The overall prevalence of stroke was stable from 1999-2002 to 2015-2018 (Table). Crude estimates of the number of affected individuals with stroke increased over time, while age-standardized estimates were stable (Figure).
Table. Self-Reported Stroke Prevalence Overall and Stratified by Sex, Race and Ethnicity, and Age Group.
| Measure | Prevalence (95% CI) | P for trenda | |||||
|---|---|---|---|---|---|---|---|
| Overall, 1999-2018 | 1999-2002 | 2003-2006 | 2007-2010 | 2011-2014 | 2015-2018 | ||
| Unweighted total, No. | 2197 | 394 | 405 | 485 | 431 | 482 | NA |
| Overall | |||||||
| Crude | 2.84 (2.67-3.02) | 2.50 (2.18-2.87) | 2.82 (2.39-3.31) | 2.91 (2.52-3.36) | 2.86 (2.53-3.23) | 3.05 (2.68-3.47) | .07 |
| Age standardizedb | 3.10 (2.92-3.29) | 2.95 (2.56-3.38) | 3.27 (2.85-3.73) | 3.23 (2.80-3.72) | 3.02 (2.69-3.39) | 3.08 (2.72-3.48) | |
| Stratified by sex | |||||||
| Men | |||||||
| Crude | 2.55 (2.36-2.77) | 2.29 (1.94-2.71) | 2.32 (1.88-2.85) | 2.62 (2.26-3.05) | 2.53 (2.06-3.11) | 2.94 (2.50-3.46) | .04 |
| Age standardizedb | 2.95 (2.73-3.18) | 2.91 (2.49-3.39) | 2.96 (2.50-3.49) | 3.03 (2.65-3.48) | 2.81 (2.27-3.46) | 3.08 (2.63-3.60) | |
| Women | |||||||
| Crude | 3.10 (2.85-3.37) | 2.69 (2.21-3.28) | 3.28 (2.73-3.93) | 3.18 (2.58-3.92) | 3.17 (2.69-3.72) | 3.15 (2.62-3.79) | .39 |
| Age standardizedb | 3.24 (2.99-3.52) | 2.99 (2.46-3.63) | 3.56 (3.03-4.19) | 3.39 (2.74-4.18) | 3.22 (2.76-3.76) | 3.09 (2.57-3.71) | |
| Stratified by race and ethnicity | |||||||
| Mexican American | |||||||
| Crude | 1.51 (1.28-1.78) | 1.09 (0.81-1.46) | 1.62 (1.1-2.36) | 1.29 (0.83-2.00) | 1.94 (1.31-2.86) | 1.51 (1.15-1.99) | .15 |
| Age standardizedb | 2.60 (2.28-2.97) | 2.58 (2.12-3.14) | 3.22 (2.37-4.35) | 2.29 (1.67-3.14) | 2.94 (2.07-4.17) | 2.25 (1.82-2.78) | |
| Non-Hispanic Asianc | |||||||
| Crude | 1.34 (0.96-1.85) | NA | NA | NA | 1.68 (1.10-2.57) | 1.04 (0.64-1.68) | NA |
| Age standardizedc | 1.74 (1.29-2.35) | NA | NA | NA | 2.32 (1.62-3.32) | 1.28 (0.81-2.03) | |
| Non-Hispanic Black | |||||||
| Crude | 3.82 (3.49-4.17) | 3.38 (2.73-4.17) | 3.38 (2.71-4.21) | 4.12 (3.44-4.92) | 3.70 (3.01-4.55) | 4.39 (3.69-5.21) | .05 |
| Age standardizedb | 4.66 (4.29-5.01) | 4.45 (3.60-5.49) | 4.60 (3.80-5.54) | 4.99 (4.18-5.94) | 4.39 (3.59-5.36) | 4.91 (4.21-5.73) | |
| Non-Hispanic White | |||||||
| Crude | 2.95 (2.72-3.18) | 2.59 (2.17-3.07) | 2.94 (2.44-3.55) | 3.09 (2.56-3.72) | 2.95 (2.57-3.39) | 3.14 (2.62-3.75) | .18 |
| Age standardizedb | 2.92 (2.71-3.16) | 2.81 (2.34-3.37) | 3.11 (2.63-3.67) | 3.11 (2.57-3.75) | 2.81 (2.47-3.19) | 2.84 (2.39-3.37) | |
| Otherd | |||||||
| Crude | 2.46 (2.00-3.02) | 2.03 (1.22-3.34) | 2.14 (1.18-3.86) | 1.87 (1.28-2.70) | 2.69 (1.81-3.97) | 3.48 (2.29-5.25) | .08 |
| Age standardizedb | 3.47 (2.84-4.23) | 2.66 (1.60-4.39) | 3.62 (2.10-6.17) | 2.91 (2.06-4.09) | 3.89 (2.73-5.51) | 4.26 (2.80-6.43) | |
| Stratified by age, ye | |||||||
| 20-39 | 0.42 (0.33-0.54) | 0.46 (0.27-0.79) | 0.41 (0.23-0.75) | 0.46 (0.27-0.80) | 0.38 (0.23-0.64) | 0.38 (0.21-0.68) | .60 |
| 40-59 | 2.01 (1.77-2.29) | 1.67 (1.19-2.34) | 1.91 (1.36-2.68) | 2.11 (1.67-2.66) | 1.97 (1.48-2.61) | 2.37 (1.82-3.07) | .14 |
| ≥60 | 7.71 (7.22-8.24) | 7.54 (6.59-8.61) | 8.41 (7.36-9.60) | 7.99 (6.69-9.51) | 7.54 (6.60-8.61) | 7.28 (6.28-8.42) | .35 |
Abbreviation: NA, not applicable.
P values for linear trend across 4-year epochs from logistic regression models.
Age standardized to the 2017-2018 American Community Survey–Public Use Microdata Sample using the following age categories: 20 to 39 years, 40 to 59 years, and 60 years and older.
Representative information for Asian American individuals available from 2011 to 2018.
The other category includes other Hispanic and other race, including multiracial.
Crude and age-standardized estimates are equivalent when age stratified using the categories of 20 to 39 years, 40 to 59 years, and 60 years and older.
Figure. Crude and Age-Standardized Estimated Number of US Adults 20 Years or Older With Self-Reported Stroke.
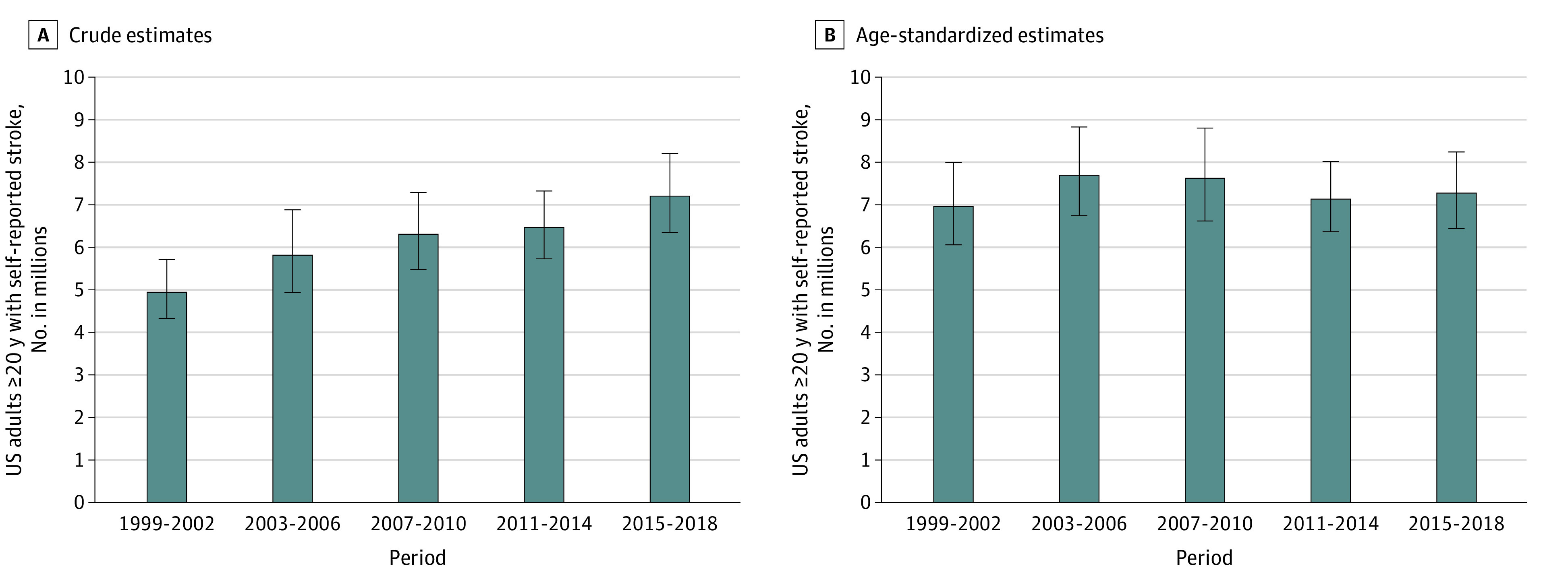
A, Crude stroke prevalence estimates were applied to the 1999 to 2002 Current Population Survey (CPS), 2003 to 2006 CPS, 2007 to 2010 CPS and American Community Survey–Public Use Microdata Sample (ACS-PUMS), 2011 to 2014 ACS-PUMS, and 2015 to 2018 ACS-PUMS to calculate the number of affected individuals with stroke in each 4-year epoch. B, Stroke prevalence estimates were age-standardized to the 2017-2018 ACS-PUMS using the following age categories: 20 to 39 years, 40 to 59 years, and 60 years and older. Age-standardized stroke prevalence estimates were then applied to the 2017-2018 ACS-PUMS to calculate the age-standardized number of affected individuals with stroke in each 4-year epoch. Error bars indicate 95% CIs.
The age-standardized prevalence of stroke was higher among non-Hispanic Black individuals compared with other racial and ethnic groups and was similar by sex. The prevalence was higher among older compared with younger individuals. The prevalence of stroke in each age and racial and ethnic group was stable from 1999-2002 to 2015-2018 but increased over time among men (from 2.29% [95% CI, 1.94-2.71] in 1999-2002 to 2.94% [95% CI, 2.50-3.46] in 2015-2018; P for trend = .04) (Table).
Discussion
Using a nationally representative sample of community-dwelling adults, we show that the prevalence of self-reported stroke remained stable in the US between 1999 and 2018 overall and by racial and ethnic group and age group and increased among men. Estimates herein underestimate the total burden of stroke in the US as NHANES does not include individuals residing in rehabilitation, long-term care, or other institutional settings. Stroke was self-reported in NHANES, which has high negative predictive value but modest positive predictive value3,4; it is possible that the validity of self-reported stroke has changed over time. Importantly, we presented both crude and age-standardized prevalence estimates to account for changes in the age structure of the US population over the study period.
We report a crude stroke prevalence of 2.8% and an age-standardized stroke prevalence of 3.1% from 1999 to 2018, which is slightly higher than the 2006 to 2010 prevalence data from the Behavioral Risk Factor Surveillance System (BRFSS; 2.6% to 2.7%).5 Both prevalence estimates, that of our study and BRFSS, are higher than the 1973 to 1991 NHANES estimates, which showed that prevalence increased from 1.41% to 1.87%.6 Taken together, although the burden of stroke has increased since 1973 to 1991, it has stabilized in recent years.
Data Sharing Statement
References
- 1.Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999-2010. Vital Health Stat 2. 2013;(161):1-24. [PubMed] [Google Scholar]
- 2.National Health and Nutrition Examination Survey . 2017-2018 Data Documentation, Codebook, and Frequencies. Accessed March 13, 2023. https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/MCQ_J.htm#MCQ160f
- 3.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: the Tromso Study. Stroke. 2000;31(7):1602-1607. doi: 10.1161/01.STR.31.7.1602 [DOI] [PubMed] [Google Scholar]
- 4.Reitz C, Schupf N, Luchsinger JA, et al. Validity of self-reported stroke in elderly African Americans, Caribbean Hispanics, and Whites. Arch Neurol. 2009;66(7):834-840. doi: 10.1001/archneurol.2009.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fang J, Shaw KM, George MG; Centers for Disease Control and Prevention (CDC) . Prevalence of stroke—United States, 2006-2010. MMWR Morb Mortal Wkly Rep. 2012;61(20):379-382. [PubMed] [Google Scholar]
- 6.Muntner P, Garrett E, Klag MJ, Coresh J. Trends in stroke prevalence between 1973 and 1991 in the US population 25 to 74 years of age. Stroke. 2002;33(5):1209-1213. doi: 10.1161/01.STR.0000015031.57955.D1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement


