This cohort study examines whether skilled nursing facility (SNF) episode volume and Medicare spending on SNF care changed after introduction of the public health emergency waiver during the COVID-19 pandemic among long-term care residents and other Medicare beneficiaries.
Key Points
Question
Did skilled nursing facility (SNF) care volume and characteristics change when the public health emergency (PHE) waiver for 3-day qualifying hospitalization was introduced in March 2020?
Findings
In this cohort study of SNF care provided for 4 299 863 Medicare fee-for-service beneficiaries from January 2018 to September 2021, waiver episodes without preceding acute care increased from 3% to 18% during the PHE in 2020 to 2021. Among long-term care residents, such waiver episodes increased from 4% to 49%, with 62% of episodes provided for residents with COVID-19.
Meaning
This study found that the use of SNF care for long-term care beneficiaries without a preceding qualifying hospitalization increased markedly during the PHE, primarily for care for patients with COVID-19.
Abstract
Importance
In response to the COVID-19 pandemic, Medicare introduced a public health emergency (PHE) waiver in March 2020, removing a 3-day hospitalization requirement before fee-for-service beneficiaries could receive skilled nursing facility (SNF) care benefits.
Objective
To assess whether there were changes in SNF episode volume and Medicare spending on SNF care before and during the PHE among long-term care (LTC) residents and other Medicare beneficiaries.
Design, Setting, and Participants
This retrospective cohort study used Medicare fee-for-service claims and the Minimum Data Set for Medicare beneficiaries who were reimbursed for SNF care episodes from January 2018 to September 2021 in US SNFs.
Exposures
The prepandemic period (January 2018-February 2020) vs the PHE period (March 2020-September 2021).
Main Outcomes and Measures
The main outcomes were SNF episode volume, characteristics, and costs. Episodes were defined as standard (with a preceding 3-day hospitalization) or waiver (with other or no acute care use).
Results
Skilled nursing facility care was provided to 4 299 863 Medicare fee-for-service beneficiaries. Medicare beneficiaries had on average 130 400 monthly SNF episodes in the prepandemic period (mean [SD] age of beneficiaries, 78.9 [11.0] years; 59% female) and 108 575 monthly episodes in the PHE period (mean [SD] age of beneficiaries, 79.0 [11.1] years; 59% female). All waiver episodes increased from 6% to 32%, and waiver episodes without preceding acute care increased from 3% to 18% (from 4% to 49% among LTC residents). Skilled nursing facility episodes provided for LTC residents increased by 77% (from 15 538 to 27 537 monthly episodes), primarily due to waiver episodes provided for residents with COVID-19 in 2020 and early 2021 (62% of waiver episodes without preceding acute care). Skilled nursing facilities in the top quartile of waiver episodes were more often for-profit (80% vs 68%) and had lower quality ratings (mean [SD] overall star rating, 2.7 [1.4] vs 3.2 [1.4]; mean [SD] staffing star rating, 2.5 [1.1] vs 3.0 [1.2]) compared with SNFs in the other quartiles. Monthly Medicare spending on SNF care was $2.1 billion before the pandemic and $2.0 billion during the PHE. For LTC residents, monthly SNF spending increased from $301 million to $585 million while spending on hospitalizations remained relatively stable.
Conclusions and Relevance
This cohort study found that the PHE waiver for SNF care was associated with a marked increase in the prevalence of SNF episodes without a preceding hospitalization, especially in the first year of the COVID-19 pandemic. The waiver was used primarily among certain types of facilities and for LTC residents with COVID-19. Although the effect of the waiver cannot be differentiated from that of the pandemic, overall SNF care costs did not increase substantially; for LTC residents, the waiver was applied primarily for COVID-19 care, suggesting the waiver’s successful implementation.
Introduction
The COVID-19 pandemic placed strain on the US health care system, overwhelming hospital capacity in early 20201 and exposing the vulnerability of long-term care (LTC) residents in skilled nursing facilities (SNFs).2 In response, the Centers for Medicare & Medicaid Services (CMS) implemented a set of waivers of rules governing reimbursement for Medicare beneficiaries during the public health emergency (PHE), effective March 1, 2020.3,4
One of the PHE waivers removed a requirement that SNF stays be preceded by a 3-day hospitalization in fee-for-service Medicare plans to be reimbursed.5,6 Under the waiver, hospitalized patients could be discharged on the first or second day of their hospitalization to continue their care in an SNF or avoid hospitalization completely through an admission to an SNF directly from the community or an emergency department. Long-term care nursing home residents newly requiring skilled nursing services (eg, for a new COVID-19 diagnosis) could receive Medicare-reimbursed SNF care without transfer to a hospital, staying in the same location and preventing costly hospitalization and potential further COVID-19 transmission.7,8 This waiver also allowed a new SNF benefit period to start without the previously required 60-day break in SNF services between benefit periods.4
The waiver of the 3-day rule during the PHE had the potential to increase SNF care, particularly among LTC residents. Because the majority of long-stay residents have their stay covered by Medicaid at a significantly lower rate than Medicare reimbursement for post–acute care, shifting residents to skilled status was an opportunity to increase revenue to the nursing facility as well as a chance to get more intensive care for residents who may have needed it.9,10 However, to date, the frequency with which and the population for whom the PHE waivers were used are unknown. Historically, the effects of waiving a 3-day hospitalization requirement for Medicare coverage of SNF care (a pilot project in Oregon and Massachusetts in 1978-198011 and a temporary waiver in 198812,13) have been inconsistent. In this study, we examined 4 questions: Did the proportion of SNF episodes without a 3-day hospitalization change during the PHE? Was the waiver associated with different changes in SNF care patterns for Medicare beneficiaries in LTC vs those living in the community? What types of SNFs were more likely to take advantage of the waiver? Did Medicare spending on SNF care change after the PHE waiver was introduced?
Methods
Data Source
This cohort study used 100% fee-for-service SNF and inpatient claims files for Medicare beneficiaries from January 1, 2017, to December 31, 2021, to identify SNF care episodes and preceding acute care. We used the Medicare Master Beneficiary Summary File to identify beneficiaries and obtain their demographic data and the Minimum Data Set from January 1, 2017, to December 31, 2021, to identify LTC residents (ie, beneficiaries with long-term residence at a nursing facility14,15). We used the Medicare Nursing Home Compare16 data set for SNF characteristics. This study was approved by the Office of Human Research Administration at Harvard Medical School. The requirement for informed consent was waived because the data were deidentified. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
Our primary unit of observation was the SNF episode. Following the CMS definition of SNF benefit period and its rules for SNF care reimbursement before the PHE, we grouped adjacent SNF stays into a single episode if a subsequent Medicare-covered SNF stay started within 60 days of the prior stay discharge date, even if only partially reimbursed. We considered an episode as ended when a beneficiary spent 60 or more days without Medicare-reimbursed SNF or inpatient care. More details are provided in eAppendix 1 in Supplement 1.
The study population included all patients enrolled in Medicare fee-for-service Part A with at least 1 Medicare-reimbursed SNF episode recorded in Medicare Part A claims and initiated between January 2018 and September 2021. We excluded episodes starting in October to December 2021 because they were likely to extend to 2022, and thus, we would not capture the full episode length and cost. We assigned the full episode to the SNF and the month in which it was initiated. We excluded SNFs that were not operational both before and during the PHE and excluded SNF episodes in hospital swing beds. A flowchart documenting how SNF episodes were constructed and the exclusion due to missing information is shown in eFigure 1 in Supplement 1.
Outcome Measures
Our primary outcome was a monthly count of SNF episodes, grouped into 3 categories. First, any SNF episode with a qualifying hospitalization of at least 3 days occurring within 30 days before the SNF episode was referred to as a standard episode. The second group consisted of any SNF episodes with other acute care use, such as a 1- to 2-day hospitalization, observational stay, or emergency department visit, within 30 days before the episode. The final group consisted of SNF episodes without acute care in the prior 30 days. We refer to the latter 2 categories as waiver episodes regardless of whether they occurred before or during the PHE (waiver episodes could happen before PHE, for example, for disaster relief or in accountable care organizations). As the periods before and during the PHE were of different lengths, we calculated both total and average total monthly counts of episodes within the period by dividing the total by the number of calendar months in the period (26 before the PHE and 19 during the PHE).
As a secondary outcome, we examined Medicare Part A spending for standard and waiver SNF episodes before and during the PHE (total, total divided by the number of months in the period, and per episode). We also compared monthly Medicare Part A spending on SNF care with that for hospitalizations and Part B spending on emergency department visits and observational hospital stays among all Medicare beneficiaries who were LTC residents in SNFs. We calculated the proportion of SNF episodes without any acute care among LTC residents that happened at the same SNF as their LTC (identified by the CMS certification number of their last Minimum Data Set assessment within 365 days before the SNF episode). Finally, we compared the 10 most frequent primary diagnoses in SNF episodes before and during the PHE stratified by beneficiary LTC status.
Descriptive Variables
We used Medicare files to capture beneficiary characteristics: age, sex, race and ethnicity, presence of Alzheimer disease or other dementia (defined using a Chronic Conditions Data Warehouse flag for the year prior to the SNF episode),17,18 number of chronic conditions (of 27 Chronic Conditions Data Warehouse flags),18 and dual eligibility for Medicaid status (defined as at least 1 month of Medicaid eligibility in the year of the SNF episode). Race and ethnicity were self-reported at the time of Medicare enrollment as Black, White, or other (including Asian, Hispanic, North American Native, other, and missing) and were included to identify potential disparities in SNF care use.
We also identified whether the beneficiary was an LTC resident at an SNF at the time of episode initiation using an established algorithm (a previous continuous SNF stay of at least 100 days as documented in Minimum Data Set records).14,15 We also examined 90-day mortality for the beneficiary from the SNF episode start.
We examined SNF episode length (ie, SNF care utilization days) and flagged episodes from March 1, 2020, to September 30, 2021, that had a COVID-19 diagnosis recorded in the claim (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code U07.1). We also examined SNF characteristics, including number of beds, overall and staffing star ratings, ownership type (government, for-profit, or nonprofit), and chain membership. The location of the SNF was defined by the Rural-Urban Commuting Area data set as metropolitan (primary codes 1-3), micropolitan (primary codes 4-6), or rural (primary codes 7-10) based on the SNF’s zip code.19
Statistical Analysis
The main unit of analysis was the SNF episode. Episode counts were aggregated monthly and divided according to whether they were preceded by 3-day hospitalizations, other acute care, or no acute care. The counts were then plotted, stratified by beneficiary group (LTC residents or other beneficiaries), episode type (standard or waiver), and COVID-19 diagnosis in any of the Part A claims of the episode.
Characteristics of the SNF episodes were described according to the period (before or during the PHE), episode type, and beneficiary group. If multiple SNF episodes were provided for the same beneficiary from January 2018 to September 2021, the beneficiary was included multiple times. eAppendix 2 in Supplement 1 shows the results of restricting the analysis to a single SNF episode per beneficiary per year to assess whether individuals with multiple episodes disproportionately influenced the distribution of the characteristics of SNF care episodes. To examine the characteristics of SNFs providing more waivered SNF care, we compared SNFs in the top quartile by the proportion of waiver episodes provided during the PHE in that SNF with other SNFs. We calculated total, average monthly, and median episode Medicare spending on SNF episodes before and during the PHE overall and among LTC residents. We used Pearson χ2 tests for comparing categorical variables, t tests to compare means of continuous variables, and multivariate analysis of variance tests for comparing race and ethnicity distributions. Differences were considered statistically significant with 2-sided P ≤ .05. Analyses were performed in SAS, version 9.4 (SAS Institute Inc).
Results
Beneficiary and Episode Characteristics
There were 4 299 863 Medicare fee-for-service beneficiaries with SNF episodes from January 2018 to September 2021. There were 3 390 406 SNF episodes in the prepandemic period (mean [SD] age of beneficiaries, 78.9 [11.0] years; 59% female and 41% male) and 2 062 932 SNF episodes in the PHE period (mean [SD] age of beneficiaries, 79.0 [11.1] years; 59% female and 41% male). In the prepandemic period, 11% of Medicare beneficiaries were Black, 81% were White, and 9% were in the other race and ethnicity category. During the PHE period, 11% of Medicare beneficiaries were Black, 80% were White, and 9% were in the other race and ethnicity category. Table 1 shows the characteristics of SNF episodes before and during the PHE. During the PHE, substantially more episodes were delivered among dual-eligible beneficiaries (45% vs 36%) and those diagnosed with dementia (30% vs 24%). The share of SNF episodes provided for LTC residents increased from 12% to 25%.
Table 1. Skilled Nursing Facility Episode Characteristics and Spending Before and During the COVID-19 PHEa.
| Characteristic | Before the PHEb | During the PHEc | P valued |
|---|---|---|---|
| SNF episodes | |||
| Total (N = 5 453 338) | 3 390 406 (62) | 2 062 932 (38) | NA |
| Average monthly episodes | |||
| Overall | 130 400 | 108 575 | NA |
| Standard with qualifying hospitalization | 122 514 (94) | 74 487 (69) | <.001 |
| Waiver with other acute care use | 3493 (3) | 14 840 (14) | |
| Waiver without acute care | 4394 (3) | 19 248 (18) | |
| Time receiving skilled care per episode, median (IQR), d | 25 (15-46) | 27 (15-50) | <.001 |
| Beneficiariese | |||
| Age, mean (SD), y | 78.9 (11.0) | 79.0 (11.1) | .001 |
| Comorbidities, mean (SD), No. | 7.5 (4.3) | 7.6 (4.4) | <.001 |
| Within average monthly episodes | |||
| Sex | |||
| Female | 77 466 (59) | 64 490 (59) | .79 |
| Male | 52 934 (41) | 44 085 (41) | |
| Race and ethnicity | |||
| Black | 13 988 (11) | 12 141 (11) | <.001 |
| White | 105 216 (81) | 86 531 (80) | |
| Otherf | 11 196 (9) | 9904 (9) | |
| Dual eligible for Medicaid | 46 351 (36) | 48 493 (45) | <.001 |
| With dementia | 31 920 (24) | 33 085 (30) | <.001 |
| With LTC in SNFs | 15 538 (12) | 27 537 (25) | <.001 |
| Medicare spending on SNF care, $ | |||
| All Medicare beneficiaries | |||
| Average total monthlyg | 2 079 544 017 | 2 027 349 143 | NA |
| Per episode, median (IQR) | 12 450 (7537-20 730) | 14 407 (8819-24 399) | <.001 |
| Total | 54 068 144 436 | 38 519 633 712 | NA |
| LTC residents | |||
| Average total monthlyg | 301 472 968 | 585 141 783 | NA |
| Per episode, median (IQR) | 15 093 (8450-27 026) | 16 487 (9574-28 957) | <.001 |
| Total | 7 838 297 168 | 11 117 693 884 | NA |
Abbreviations: LTC, long-term care; NA, not applicable; PHE, public health emergency; SNF, skilled nursing facility.
Data are presented as number (percentage) of episodes unless otherwise indicated.
January 2018 to February 2020.
March 2020 to September 2021.
We used Pearson χ2 test for comparing categorical variables and t test to compare means of continuous variables.
In cases of multiple episodes per beneficiary, characteristics are counted multiple times.
Other race and ethnicity includes Asian, Hispanic, North American Native, other, and missing.
Calculated by dividing the total number during the period by the number of calendar months in the period (26 before the PHE period and 19 during the PHE period).
During the PHE, 386 785 SNF episodes (19%) were for patients with COVID-19. Of those, 226 351 (59%) were provided for LTC residents compared with 296 845 non–COVID-19 episodes (18%) (eTable 1 in Supplement 1). The most frequent primary diagnoses in SNF episodes during the PHE overlapped with those before the PHE, with the notable addition of COVID-19 among LTC residents (23.5% of episodes) and other beneficiaries (5.3% of episodes) (eTable 2 in Supplement 1).
Volume of Standard and Waiver SNF Episodes
On average, 130 400 SNF episodes were initiated monthly between January 2018 and February 2020 and 108 575 monthly between March 2020 and September 2021, a relative monthly decrease of 17% (Figure 1, Table 1, and eTable 3 in Supplement 1). The proportion of waiver episodes without a preceding 3-day hospitalization was stable at roughly 6% from January 2018 through February 2020 and increased to 32% in March 2020 to September 2021. Waiver episodes with other acute care use increased from 3% to 14%, and waiver episodes without any acute care increased from 3% to 18% (Table 1).
Figure 1. Number of Skilled Nursing Facility (SNF) Episodes With a Qualifying Hospitalization, Other Preceding Acute Care Use, and No Prior Acute Care.
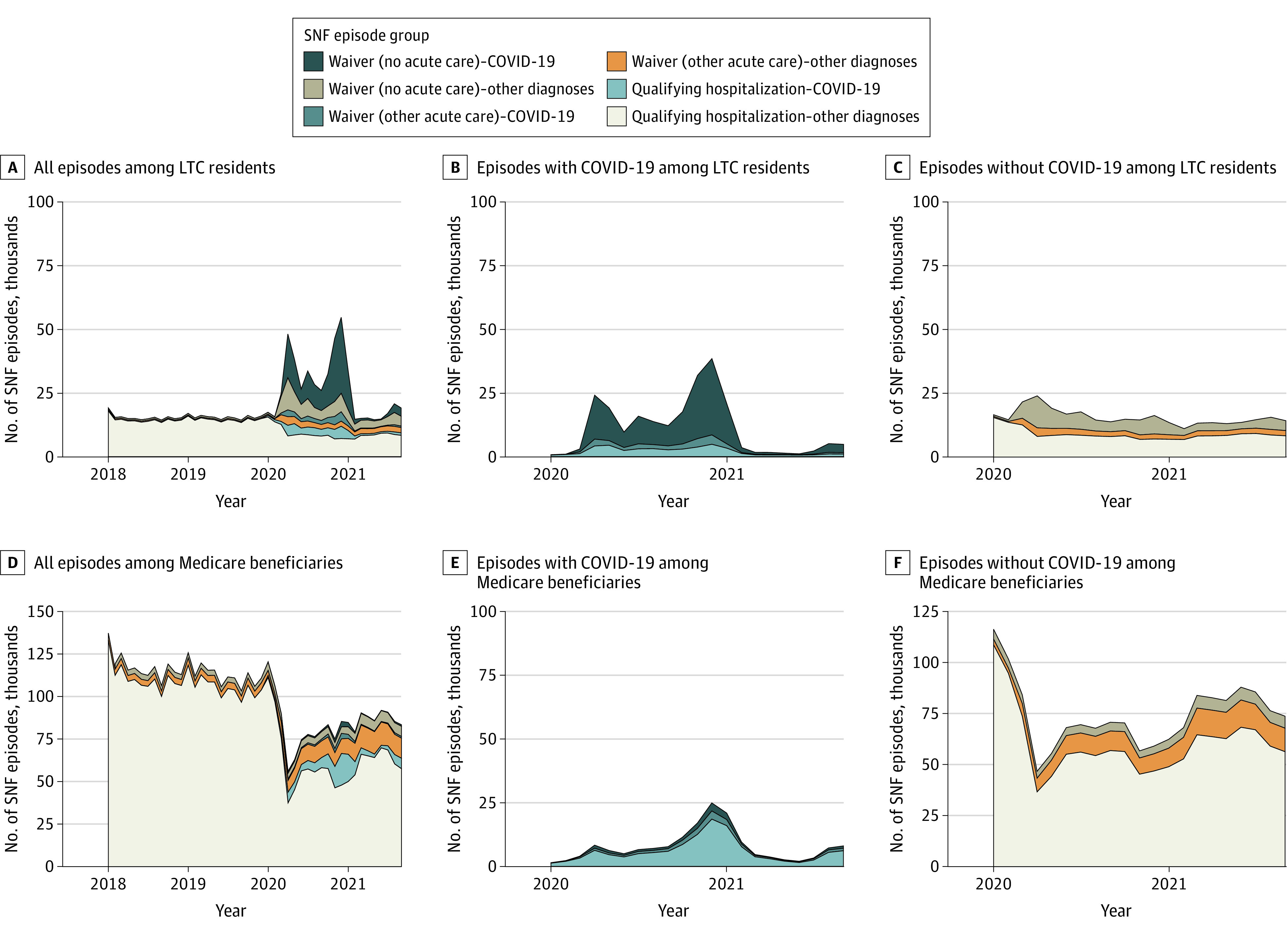
The prepandemic period was from January 2018 to February 2020, and the public health emergency period was from March 2020 to September 2021. LTC indicates long-term care.
Volume of SNF Episodes for LTC Residents and Other Beneficiaries
The number of monthly SNF episodes among LTC residents increased, on average, from 15 538 before the PHE to 27 537 during the PHE (relative increase of 77%) (Figure 1A). The increase was primarily due to waiver episodes without any acute care in 2020 and early 2021 (an increase from 4% to 49% of all SNF episodes from the prepandemic to PHE periods), the majority of which were provided for patients with COVID-19 (ranging from 11% in June 2021 to 81% in November 2020; overall, 62% of such episodes were during the PHE period) (Figure 1B). The overall number of SNF episodes decreased to roughly the prepandemic level starting in February 2021 (Figure 1A).
Among beneficiaries not in LTC (Figure 1D), the average number of monthly episodes decreased from 114 862 to 81 039 (a relative decrease of 29%). The number of waiver episodes increased less than for the LTC residents, and the majority of episodes with COVID-19 diagnoses had a qualifying hospitalization (Figure 1E). Results were similar when considering only the first SNF episode for a beneficiary per year (eAppendix 2 in Supplement 1).
Characteristics of Standard and Waiver SNF Episodes During the PHE
During the PHE, waiver episodes without acute care vs episodes with either qualifying hospitalization or other acute care for LTC residents were shorter (27 vs 36 and 44 days), were more likely to be associated with a COVID-19 diagnosis (62% vs 21% and 38%), and were provided for patients with fewer comorbidities (Table 2). Among LTC residents, 70% of waiver SNF episodes without any acute care were in the same SNF as their LTC. The episodes without prior acute care were shorter for residents with COVID-19 vs without COVID-19 (median, 24 days [IQR, 14-47 days] vs 30 days [IQR, 14-61 days]), while episodes with a qualifying hospitalization (median, 42 days [IQR, 21-78 days] vs 35 days [IQR, 19-67 days]) or other acute care (median, 51 days [IQR, 26-87 days] vs 40 days [IQR, 21-76 days]) were longer for residents with COVID-19 (eTable 4 in Supplement 1).
Table 2. Characteristics of Standard and Waiver Skilled Nursing Facility Episodes During the COVID-19 Public Health Emergency From March 2020 to September 2021 by LTC Statusa.
| Characteristic | Episodesb | ||
|---|---|---|---|
| Standard with qualifying hospitalization | Waiver with other acute care use | Waiver without acute care | |
| Episodes among LTC residents (n = 523 196) | |||
| Total | 201 899 (39) | 65 594 (13) | 255 703 (49) |
| Time receiving skilled care, median (IQR), d | 36 (19-70) | 44 (22-81) | 27 (14-52) |
| Beneficiaryc | |||
| Age, mean (SD), y | 76.5 (12.0) | 78.0 (11.9) | 79.7 (11.9) |
| Race and ethnicity | |||
| Black | 36 467 (18) | 10 242 (16) | 34 725 (14) |
| White | 143 508 (71) | 47 700 (73) | 189 996 (74) |
| Otherd | 21 924 (11) | 7652 (12) | 30 982 (12) |
| Dual eligible | 177 441 (88) | 58 619 (89) | 228 927 (90) |
| COVID-19 diagnosis | 41 993 (21) | 24 747 (38) | 159 611 (62) |
| With dementia | 113 974 (56) | 38 967 (59) | 158 050 (62) |
| Comorbidities, mean (SD), No. | 9.9 (4.2) | 9.6 (4.2) | 8.5 (4.1) |
| 90-d Mortality | 36 274 (18) | 7939 (12) | 33 131 (13) |
| Episodes among beneficiaries not in LTC (n = 1 539 736) | |||
| Total | 1 213 354 (79) | 216 370 (14) | 110 012 (7) |
| Time receiving skilled care, median (IQR), d | 26 (15-46) | 26 (15-46) | 24 (14-47) |
| Beneficiaryc | |||
| Age, mean (SD), y | 79.1 (10.8) | 81.2 (10.4) | 78.1 (10.7) |
| Race and ethnicity | |||
| Black | 116 593 (10) | 16 164 (7) | 16 481 (15) |
| White | 997 607 (82) | 184 618 (85) | 80 662 (73) |
| Otherd | 99 154 (8) | 15 588 (7) | 12 869 (12) |
| Dual eligible | 349 496 (29) | 62 312 (29) | 44 578 (41) |
| COVID-19 diagnosis | 122 010 (10) | 20 145 (9) | 18 279 (17) |
| With dementia | 247 798 (20) | 51 526 (24) | 18 300 (17) |
| Comorbidities, mean (SD), No. | 7.3 (4.2) | 7.1 (4.1) | 4.0 (4.5) |
| 90-d Mortality | 210 616 (17) | 24 079 (11) | 16 342 (15) |
Abbreviation: LTC, long-term care.
We used Pearson χ2 test for comparing categorical variables and t test to compare means of continuous variables. P values for all comparisons were <.001.
Data are presented as number (percentage) of episodes unless otherwise indicated.
In cases of multiple episodes per beneficiary, characteristics are counted multiple times.
Other race and ethnicity includes Asian, Hispanic, North American Native, other, and missing.
Among SNF episodes involving beneficiaries not in LTC, the number of skilled care days was overall lower and more similar across episode types, and COVID-19 diagnoses were less frequent than among LTC residents (Table 2). The differences in length of stay were smaller between patients with COVID-19 and other beneficiaries (eTable 4 in Supplement 1).
Characteristics of SNFs With High Waiver Use
The proportion of SNF episodes delivered through the waiver varied broadly across SNFs (median, 31.0% [IQR, 20.5%-43.4%]) (eFigure 2 in Supplement 1). Skilled nursing facilities in the top quartile (>43.4%) by the proportion of waiver episodes served a larger share of dual-eligible beneficiaries, LTC residents, and beneficiaries with dementia compared with SNFs in the other quartiles (Table 3). They were also more likely to be for-profit institutions (80% vs 68%) and situated in rural areas (22% vs 15%) and had more months during the PHE providing SNF care for at least 1 beneficiary with a COVID-19 diagnosis (mean [SD], 7.0 [3.4] months vs 6.6 [3.8] months). The mean (SD) overall star rating (2.7 [1.4] vs 3.2 [1.4]) and mean (SD) staffing star rating (2.5 [1.1] vs 3.0 [1.2]) were lower in SNFs providing a higher proportion of waiver episodes.
Table 3. Baseline Characteristics of SNFs, Stratified by Waiver Use During the COVID-19 PHE From March 2020 to September 2021a.
| Characteristic | Proportion of waiver episodes during the PHEb | P valuec | |
|---|---|---|---|
| Top quartile | Other | ||
| Total, No. | 3852 | 10 931 | NA |
| Beds, median (IQR), No.d | 100 (73-129) | 100 (65-128) | <.001 |
| SNF beneficiaries, median (IQR), %d,e | |||
| Dual eligible for Medicaid | 59 (43-75) | 40 (22-57) | <.001 |
| In long-term care | 27 (16-40) | 12 (5-24) | <.001 |
| Race and ethnicity | |||
| Black | 5 (0-17) | 4 (0-14) | <.001 |
| White | 85 (62-96) | 90 (75-96) | |
| Otherf | 4 (0-15) | 3 (1-8) | |
| With dementia | 30 (22-39) | 24 (18-32) | <.001 |
| Time with an episode flagged with COVID-19 diagnosis, mean (SD), mog | 7.0 (3.4) | 6.6 (3.8) | <.001 |
| Ownership model, %d,h | |||
| Government | 7 | 5 | .04 |
| Not for profit | 13 | 27 | |
| For profit | 80 | 68 | |
| Chain membership, %h | 73 | 74 | .63 |
| Star rating, mean (SD)d,h | |||
| Overall | 2.7 (1.4) | 3.2 (1.4) | <.001 |
| Staffing | 2.5 (1.1) | 3.0 (1.2) | <.001 |
| Urban or rural setting of zip code, %h,i | |||
| Metropolitan | 62 | 72 | <.001 |
| Micropolitan | 16 | 13 | |
| Rural | 22 | 15 | |
Abbreviations: NA, not applicable; PHE, public health emergency; SNF, skilled nursing facility.
Information was missing for 17 SNFs, which were thus excluded from this table.
Greater than 43.4% of waiver episodes during the PHE indicates the top quartile of SNFs; 43.4% or less indicates other SNFs.
We used Pearson χ2 test for comparing categorical variables, a t test to compare means of continuous variables, and a multivariate analysis of variance test for comparing race distributions.
Eleven SNFs had missing information.
Beneficiary characteristics refer to SNF care beneficiaries covered by Medicare Part A in 2019. In cases of multiple episodes per beneficiary, characteristics are counted multiple times.
Other race and ethnicity includes Asian, Hispanic, North American Native, other, and missing.
A month is counted as having a COVID-19 diagnosis if at least 1 SNF episode with an attached COVID-19 diagnosis was initiated in that SNF in that month.
Skilled nursing facility characteristic refers to July 2019 or the latest month with information available on Medicare’s Nursing Home Compare database.
Twenty-five SNFs had missing zip code information.
Medicare Spending on SNF Care Before and During the PHE
The average monthly Medicare Part A spending on SNF care episodes was $2.1 billion before the PHE and $2.0 billion during the PHE, corresponding to an average relative monthly spending decrease of 3% (Table 1). However, for LTC residents, monthly SNF spending increased from $301 million to $585 million (relative increase of 94%).
Monthly Medicare spending on SNF care for LTC residents was on average less than half (45%) of the spending on hospitalizations before the PHE (Figure 2A). While monthly spending on SNF care increased during the PHE, mostly during the peak months of COVID-19 prevalence, spending on hospitalizations remained more stable so that monthly spending on SNF care was on average 88% of spending on hospitalizations. In contrast, the spending on a single SNF episode or a hospitalization remained relatively stable from 2018 to 2021 (Figure 2B). Total spending and per-episode cost remained stable for emergency department visits and observational stays through 2018 to 2021.
Figure 2. Medicare Spending on Skilled Nursing Facility (SNF) Episodes, Inpatient Stays, Emergency Department (ED) Visits, and Observational Stays in a Hospital Among Long-term Care Residents.
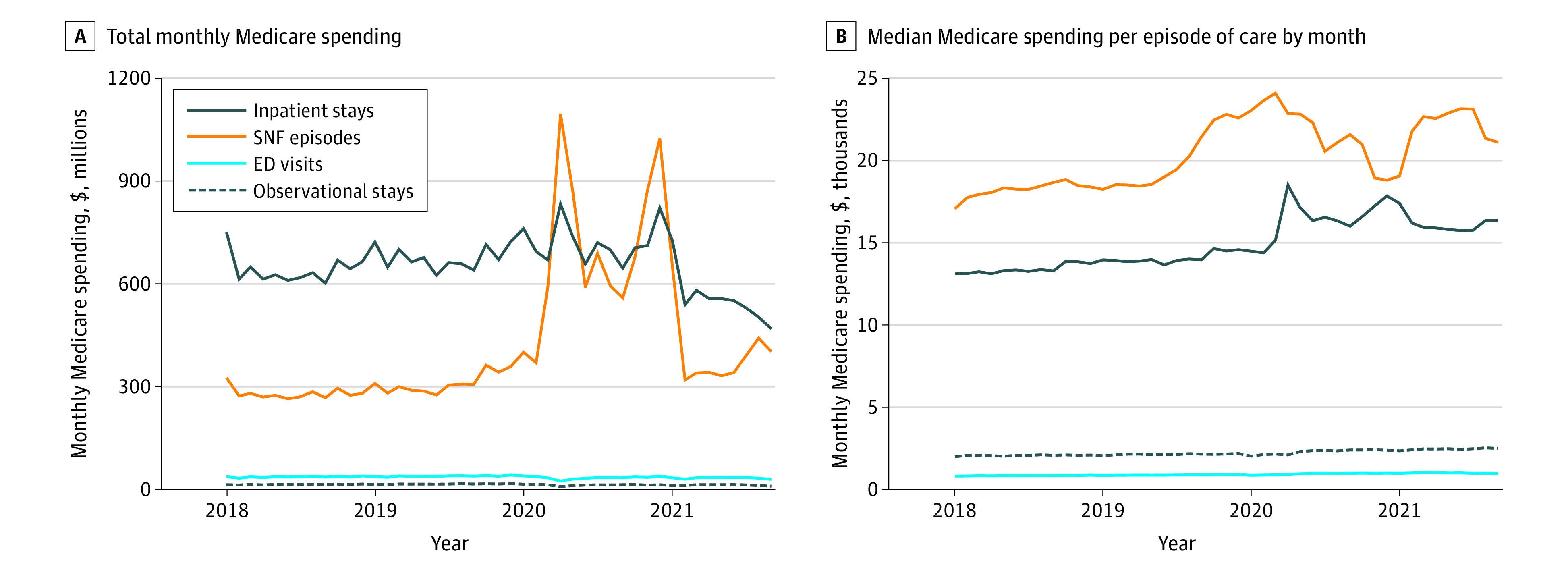
The prepandemic period was from January 2018 to February 2020, and the public health emergency period was from March 2020 to September 2021.
Discussion
In this cohort study of SNF care provided for traditional Medicare beneficiaries from January 2018 to September 2021, we found that SNF episodes for LTC residents increased substantially, primarily due to care for COVID-19 with waiver episodes during the peaks of incidence from April 2020 to March 2021. In contrast, the number of SNF episodes for other beneficiaries decreased and was not offset by waiver-enabled SNF care or care for COVID-19. As a result, average monthly Medicare spending on SNF care decreased but spending on care for LTC residents doubled. Certain SNFs, such as rural and for-profit facilities and those with lower quality ratings, were more likely to provide care under the PHE waiver.
Most community-living beneficiaries who received SNF care during the PHE did so after a hospitalization or other acute care. Skilled nursing facility care supply, limited by a severe shortage of staff,20,21 potentially restricted wider use of SNF care even under the PHE waiver. We cannot know how a 3-day waiver would have changed SNF care in the absence of the other pandemic changes in the health care system and patients’ clinical needs, which are reflected also in changes in the diagnoses of SNF episodes before and during the PHE. Among community-living beneficiaries, the waiver was primarily applied to provide SNF care after less than a 3-day hospitalization rather than without any acute care. Potentially, the waiver enabled faster discharge for some of the beneficiaries. Previously, a number of current Medicare alternative payment models, such as accountable care and bundled payment programs, with a waiver for a qualifying hospitalization led to shorter hospitalizations but not more SNF admissions or longer lengths of stay.22
In contrast, the PHE waiver was frequently used to provide SNF care to LTC residents without a prior hospital visit and without a transfer from the SNF in which they already resided. This practice, termed skilling-in-place by The Medicare Payment Advisory Commission,7 may have enabled access to a broader range of clinical services on site and effectively substituted for a higher-cost hospitalization. Long-term care residents receiving skilling-in-place care rather than SNF care following a hospitalization had fewer comorbidities and spent fewer days in care, meaning that SNFs likely triaged residents with less severe illness to receive direct SNF care rather than a hospital visit. Skilling-in-place primarily served patients with COVID-19 during the peaks of disease prevalence in early 2020 and the winters of 2020 and 2021. These SNF episodes decreased to a stable level once the majority of SNF residents were vaccinated in April 202123 and community prevalence of COVID-19—a major reason for COVID-19 spread in SNFs24—became lower. Unlike for community-dwelling beneficiaries, there may have been fewer barriers to receive SNF care for LTC residents already residing in an SNF. Because skilling-in-place was limited once COVID-19 prevalence became low in 2021, its expansion was likely driven by patient clinical needs.
The complex epidemiological, behavioral, and health care system changes accompanying the early COVID-19 pandemic make it difficult to isolate the effects of the PHE waiver on the care patterns and outcomes of SNF care beneficiaries. However, the waiver was not associated with a substantial increase in the overall SNF care volume and was applied for LTC residents primarily for COVID-19 care, suggesting that the goals for the waiver were successfully achieved.
We found that Medicare spending for hospitalizations among LTC residents stayed relatively stable during the PHE, consistent with another study showing only a slight decrease in the hospitalization rate.25 In contrast, the monthly spending on SNF care among LTC residents almost doubled, primarily due to increased SNF care volume as median spending for a single episode remained stable. Likely, the additional care for residents with COVID-19 helped to divert patients with less severe cases to be treated directly at an SNF rather than a hospital.
The proportion of waiver to standard SNF episodes was highly variable across SNFs. Skilled nursing facilities with a high proportion of waiver episodes were more likely to be for-profit and thus, perhaps, more attentive to the financial incentives embedded in the waiver. They also had more dually eligible beneficiaries and LTC residents, who usually contribute to lower SNF earnings than Medicare-reimbursed care.9 However, these possibilities are countered by the significant reduction in waiver applications once COVID-19 became a smaller threat for residents in April 2021.
Limitations
Our study has limitations. First, it is difficult to disentangle the effect of the waiver from other changes in care due to the pandemic (eg, changes in disease incidence, populations of SNF residents and staff, or resident access to hospitals). Second, relying on claims data precluded direct assessment of the clinical appropriateness of the waiver episodes. While we were able to calculate the cost of SNF episodes to Medicare, we lacked spending data for Medicaid and could not accurately estimate total government spending. The algorithms we applied to identify waiver episodes and LTC residents likely have a degree of misclassification.15 They rely on correctly recorded dates of SNF stays, and their accuracy might be affected by changes in care reimbursement and documentation. We did not have a direct indicator of which SNF stays constituted a single episode and instead defined them based on Medicare rules and observed use pattern in the claims.
Conclusions
In this cohort study, the PHE waiver for SNF care was associated with a marked increase in the prevalence of SNF episodes without a preceding hospitalization, especially in the first year of the COVID-19 pandemic. The waiver was used primarily among certain types of facilities and for LTC residents with COVID-19. Although the effect of the waiver cannot be differentiated from that of the pandemic, overall SNF care costs did not increase substantially, and for LTC residents, the waiver was applied primarily for COVID-19 care, suggesting its successful implementation.
eAppendix 1. Overview of SNF Reimbursement in Medicare
eFigure 1. Flowchart of Analyzed SNF Episodes
eTable 1. SNF Episode Characteristics for Patients With and Without COVID-19 During PHE in March 2020 to September 2021
eTable 2. Most Frequent Diagnoses in SNF Care Episodes Before and During PHE Among Long-term Care Residents and Other Beneficiaries
eTable 3. Number of SNF Episodes With a Qualifying Hospitalization, Other Acute Care Use, and No Acute Care Among Long-term Care Residents and Other Medicare Beneficiaries
eTable 4. Characteristics of SNF Episodes With and Without COVID-19 Diagnosis During PHE in March 2020 to September 2021, by Long-term Care Status and Episode Type
eAppendix 2. Study Results of Restricting the Analysis to a Single SNF Episode per Beneficiary per Year
eFigure 2. Distribution of SNFs by the Proportion of Waiver Skilled Care Episodes Among All Episodes Provided in March 2020 to September 2021
Data Sharing Statement
References
- 1.Tsai TC, Jacobson BH, Orav EJ, Jha AK. Association of community-level social vulnerability with US acute care hospital intensive care unit capacity during COVID-19. Healthc (Amst). 2022;10(1):100611. doi: 10.1016/j.hjdsi.2021.100611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ouslander JG, Grabowski DC. COVID-19 in nursing homes: calming the perfect storm. J Am Geriatr Soc. 2020;68(10):2153-2162. doi: 10.1111/jgs.16784 [DOI] [PubMed] [Google Scholar]
- 3.Grabert L, Makam AN, Grabowski DC. COVID-19 waivers of Medicare post-acute rules increased capacity but should not become permanent. Health Affairs. December 6, 2021. Accessed March 15, 2023. https://www.healthaffairs.org/do/10.1377/forefront.20211202.867311/full/
- 4.Centers for Medicare & Medicaid Services. Coronavirus waivers & flexibilities. Accessed May 17, 2022. https://www.cms.gov/coronavirus-waivers
- 5.Sheehy AM, Locke CFS, Kaiksow FA, Powell WR, Bykovskyi AG, Kind AJH. Improving healthcare value: COVID-19 emergency regulatory relief and implications for post-acute skilled nursing facility care. J Hosp Med. 2020;15(8):495-497. doi: 10.12788/jhm.3482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Health Care Association; National Center for Assisted Living . 3-Day stay and benefit-period waivers for Medicare Part A SNF PPS. Updated January 26, 2023. Accessed March 15, 2023. https://www.ahcancal.org/Survey-Regulatory-Legal/Emergency-Preparedness/Documents/COVID19/3-Day Waiver FAQ.pdf
- 7.The Medicare Payment Advisory Commission Policy. March 2022 report to Congress: Medicare payment policy. March 15, 2022. Accessed July 18, 2022. https://www.medpac.gov/document/march-2022-report-to-the-congress-medicare-payment-policy/
- 8.Levitt AF, Ling SM. COVID-19 in the long-term care setting: the CMS perspective. J Am Geriatr Soc. 2020;68(7):1366-1369. doi: 10.1111/jgs.16562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q. 2007;85(4):579-610. doi: 10.1111/j.1468-0009.2007.00502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grabowski DC. Putting the nursing and home in nursing homes. Innov Aging. 2022;6(4):igac029. doi: 10.1093/geroni/igac029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birnbaum H, Mor V, Stearns S, Sherwood S, Kronick R, Schwartz R. Entry to Skilled Nursing Care: Evaluation of the Prior Hospital Stay Requirement for Medicare SNF Reimbursement. Cambridge; 1982. [Google Scholar]
- 12.Aaronson WE, Zinn JS, Rosko MD. The success and repeal of the Medicare Catastrophic Coverage Act: a paradoxical lesson for health care reform. J Health Polit Policy Law. 1994;19(4):753-771. doi: 10.1215/03616878-19-4-753 [DOI] [PubMed] [Google Scholar]
- 13.Laliberte L, Mor V, Berg K, Intrator O, Calore K, Hiris J. Impact of the Medicare Catastrophic Coverage Act on nursing homes. Milbank Q. 1997;75(2):203-233. doi: 10.1111/1468-0009.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46(1, pt 1):120-137. doi: 10.1111/j.1475-6773.2010.01194.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodwin JS, Li S, Zhou J, Graham JE, Karmarkar A, Ottenbacher K. Comparison of methods to identify long term care nursing home residence with administrative data. BMC Health Serv Res. 2017;17(1):376. doi: 10.1186/s12913-017-2318-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. Provider information. Accessed May 4, 2022. https://data.cms.gov/provider-data/dataset/4pq5-n9py
- 17.Research Data Assistance Center. Alzheimer’s disease and related disorders or senile dementia end-of-year indicator. Accessed January 24, 2023. https://resdac.org/cms-data/variables/mbsf-27-cc/alzheimers-disease-and-related-disorders-or-senile-dementia-end-year-indicator
- 18.Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. Accessed June 24, 2022. https://www2.ccwdata.org/web/guest/condition-categories-chronic
- 19.Economic Research Service, US Department of Agriculture. Rural-urban commuting area codes. Accessed December 14, 2022. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- 20.SteelFisher GK, Epstein AM, Grabowski DC, Joynt Maddox KE, Orav EJ, Barnett ML. Persistent challenges of COVID-19 in skilled nursing facilities: the administrator perspective. J Am Geriatr Soc. 2021;69(4):875-878. doi: 10.1111/jgs.17062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGarry BE, Grabowski DC, Barnett ML. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID-19 pandemic. Health Aff (Millwood). 2020;39(10):1812-1821. doi: 10.1377/hlthaff.2020.01269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grebla RC, Keohane L, Lee Y, Lipsitz LA, Rahman M, Trivedi AN. Waiving the three-day rule: admissions and length-of-stay at hospitals and skilled nursing facilities did not increase. Health Aff (Millwood). 2015;34(8):1324-1330. doi: 10.1377/hlthaff.2015.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Nursing home COVID-19 vaccination data dashboard. Accessed January 13, 2023. https://www.cdc.gov/nhsn/covid19/ltc-vaccination-dashboard.html
- 24.Konetzka RT, White EM, Pralea A, Grabowski DC, Mor V. A systematic review of long-term care facility characteristics associated with COVID-19 outcomes. J Am Geriatr Soc. 2021;69(10):2766-2777. doi: 10.1111/jgs.17434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnett ML, Waken RJ, Zheng J, et al. Changes in health and quality of life in US skilled nursing facilities by COVID-19 exposure status in 2020. JAMA. 2022;328(10):941-950. doi: 10.1001/jama.2022.15071 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Overview of SNF Reimbursement in Medicare
eFigure 1. Flowchart of Analyzed SNF Episodes
eTable 1. SNF Episode Characteristics for Patients With and Without COVID-19 During PHE in March 2020 to September 2021
eTable 2. Most Frequent Diagnoses in SNF Care Episodes Before and During PHE Among Long-term Care Residents and Other Beneficiaries
eTable 3. Number of SNF Episodes With a Qualifying Hospitalization, Other Acute Care Use, and No Acute Care Among Long-term Care Residents and Other Medicare Beneficiaries
eTable 4. Characteristics of SNF Episodes With and Without COVID-19 Diagnosis During PHE in March 2020 to September 2021, by Long-term Care Status and Episode Type
eAppendix 2. Study Results of Restricting the Analysis to a Single SNF Episode per Beneficiary per Year
eFigure 2. Distribution of SNFs by the Proportion of Waiver Skilled Care Episodes Among All Episodes Provided in March 2020 to September 2021
Data Sharing Statement


