Abstract
Policy Points.
The US public heath infrastructure is in disrepair and building a sustainable system is the central challenge for the nation.
Doing so in a highly patrician environment is the mission for the next ten years.
Keywords: public health infrastructure, legal authorities, data and surveillance systems
The public health infrastructure in the united states is in disrepair. In fact, it has never truly been adequate to meet the needs of the nation and our nation's role in global affairs. In 1988 the Institute of Medicine of the National Academies of Sciences published the results of a consensus study entitled “The Future of Public Health.” 1 This report found the nation's public health system to be in disarray and that the nation had lost sight of its public health needs. Since that time the nation has struggled to address this finding and to build a system that can adequately address the ever‐growing needs of the population. Infrastructure is defined as “the resources (such as personnel, buildings, or equipment) required for an activity.” 2 In fact, there is growing evidence that the basic infrastructure of the public health system in the nation has continued to erode to the point that its capacity and capabilities to adequately protect the nation are in doubt. 1
A Ten‐Year Look Into the Future
Imagine a system that is comprehensive enough to address all health threats from emerging or reemerging infectious diseases, acute and chronic diseases, severe weather from climate change, product contamination, epidemics of injuries both intentional and unintentional, toxic exposure, and terrorism.
Such a system could for example address a cluster of asthma cases that resulted in ten children presenting to several community emergency departments on a single day. These cases were severe enough that the children had to be absent from school. The children all went to the same school, but were from different homes, were seen at different hospitals and were in different insurance plans. No single source other than the health department in partnership with the local hospitals and the school system would have been able to put the cluster together. The data systems in the community were robust enough that they identified this cluster and reported them to the health department. The health department was resourced and skilled enough to do a rapid, high quality epidemiological assessment. In the end this outbreak identified the one common cause for these children's respiratory distress—they all rode on the same school bus. An inspection of the bus revealed a broken tail pipe. The broken tail pipe allowed noxious fumes to enter the bus and stimulated significant asthma attacks in the children over the next couple of days. The school system was notified, the buses inspected, the tail pipe fixed, and the problem solved. Future health problems prevented, emergency health care costs avoided and the transportation system safer. This system requires strong partnerships, data systems, and a robust infrastructure. This is indeed the public health system of the future.
To see how we get here let's first explore what we have today.
The 2023 Operating Environment
The operating environment for the public health system today recognizes that we are in a globalized world with a renewed focus on infectious diseases driven most recently by the emergence of SARS‐Cov‐2, the virus that caused the COVID‐19 pandemic. In addition, there are continued concerns about the need to address chronic diseases more completely and inadequate support for addressing acute preventable injury from a public health perspective. Rapidly changing demographics in the nation and the peaking of the baby boom generation means the public health system needs to continually adapt to address the diverse needs of the population. This can be done in equitable and culturally sensitive ways as well as meeting the needs of a society that is unprepared for the tsunami of individuals in need of population‐based long‐term supportive care.
There is a growing understanding of the fundamental role that the social determinants play in health outcomes and the central role of policy decisions in impacting these determinants. This environment includes an abundance of disruptive technologies, such as the internet and social media, that now drive health behavior and new technologies like e‐cigarettes that have undermined our years‐long efforts to address tobacco use. Public health practice that in the past was invisible is now highly visible. This visibility in an increasingly partisan world has made health policy a target for political activism and threatens the very authorities under which public health works. 3 , 4
The future operating environment cannot be predicted with precision; however, it seems clear that the partisan divide will continue for some time with its different views on the role of government and that public health will have to navigate building a modernized infrastructure within an ever‐evolving operating environment that is subject to partisan political scrutiny.
This evolving operating environment means that building community resilience to withstand the emergence of new health threats as well as the reemergence of diseases long thought under control or conquered is an essential component of the public health infrastructure of the future. “Community resilience is the sustained ability of communities to withstand, adapt to, and recover from adversity,” as defined by the Assistant Secretary for Preparedness and Response of the US Department of Health and Human Services (HHS). 5
The Structure of Today's US Public Health System
Unlike many other high‐income countries, the United States does not have a system of universal health care, nor does it have a unified health care and public health system. 6 To that end, the public health system is separate in many aspects of its functioning including its core infrastructure. It is a partnership between the federal, state, and local governments with strong support from many private nonprofit organizations. These private organizations consist of both for‐profit and not‐for‐profit organizations that provide a range of direct and indirect public health services and programs. For example, the Association of Public Health Laboratories (APHL), whose mission is to “strengthen laboratory systems, serving the public health of the United States and globally,” serves as the organizing entity to coordinate and address the nation's governmental public health laboratory needs in support of the mission of the Centers for Disease Control and Prevention (CDC) at the state and local level and often is an interface to private sector laboratories. It also plays an enormous role in building public health laboratory capacity in under‐resourced countries. The Health Resources and Services Administration (HRSA) provides both clinical services to the underserved through their nationwide community health centers, as well as a suite of programs to support targeted populations to address maternal and child health, HIV/AIDS, rural populations, and programs to strengthen the health workforce of the United States. Other examples include the National Network for Public Health Institutes, the Association of Maternal and Child Health Programs (AMCHIP), the American Public Health Association (APHA,) and the National Association of City and County Health Officials (NACCHO), which provide numerous trainings to develop and maintain the skills of public health workers.
The public health system in the United States developed over time in a random way as new health needs were identified, and resources found to partially address them. This piecemeal approach has resulted in a patchwork of programs and funding streams that partially address health promotion, disease prevention, and health protection. Thus, the public health system today is not well designed or adequately resourced to meet the strategic needs of the nation nor to support the building of resilient communities.
Historically, the federal public health services originated from the nation's system of marine hospitals that were founded in 1798. Over time this system became the Public Health Service as we know it today, fully integrated into the US Department of Health and Human Services. This creates some confusion as we think about the public health infrastructure because although people often refer to the CDC and occasionally HRSA when thinking about public health, in reality all the agencies of HHS and several operating entities of other federal agencies are part of the public health system. For example, the Occupational Safety and Health Agency (OSHA) in the US Department of labor, the Environmental Protection Agency, and the National Highway Traffic Safety Administration (NHTSA) in the Department of Transportation are clearly public health entities.
Because of the US concept of federalism, the public health system is governed locally and managed as a partnership with a range of private sector organizations as noted above. The governmental public health system is the entity that has the legal responsibility for the health of the community but relies on its private sector partners to expand its operational and early warning capacities.
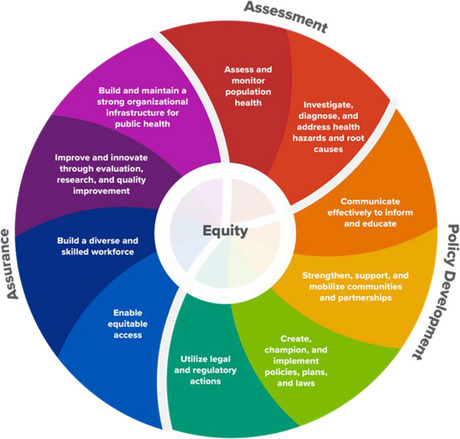
There are four models of organizational structures of public health systems at the state and local level: centralized, shared, mixed, and decentralized (Figure 1). 7 Each of these state organizational governance models have benefits and weaknesses but in general are tailored to the desires of their local officials. In many ways this mix and match of organizational structures creates confusion and complicates the management of health threats on a national basis. 8 The work that public health does is defined under a framework known as the ten essential services. These services were recently updated and recognize equity at the center of public health practice (Figure 2). 9 These ten services are organized under three core functions: to assess the health of the community on an ongoing and recurrent basis; to develop policy to address the health needs identified through the assessments; and to assure that the activities put in place have a positive health impact on the population. These three core functions of assessment, policy development, and assurance are functions of all three levels of government and provide an organizing framework for the infrastructure needs of the governmental public health system.
Figure 1.
State public Health Organizational and Governance Models. [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.

Ten Essential Public Health Services. [Colour figure can be viewed at wileyonlinelibrary.com]
After publishing its 1988 report, the Institute of Medicine convened a committee known as the Committee on Public Health Strategies to Improve Health, which produced three reports to again look at how best to invest in and modernize the nation's public health system. One of these reports published in 2012 was titled “For the Public's Health: Investing in a Healthier Future.” 10 This report built on a series of other studies including the ten essential services framework and explored the need to provide sustainable funding for the public health system. It defined a minimum package of services, programs, and skills that every state or local department must have to provide the foundational capacities all communities should have. This set of capacities created a framework that would allow one to estimate the cost to provide adequate public health services for all communities. 11 , 12
A real problem is the large number of small local health departments that do not have a minimum capacity to provide the health protections their communities deserve. Solutions have been debated to include consolidation of agencies across jurisdictional lines, partnership agreements, and even redefining the responsibilities of state versus local agencies to rationalize the system. The federal government could bring together the various parties to come to agreement on ways to improve the alignment and structures of the nation's public health system. However, total standardization of the national structure and legal framework of the public health system would require a major revamping of the role of federalism because of our unique federal, state, and local governance structure that is built into the US Constitution. This would require a constitutional convention and is unlikely to occur.
The Infrastructure Now and In the Future
The public health infrastructure consists of the legal basis for its work, adequate numbers of well‐trained workers, modern technologies, robust data systems, communications capacity, and the ability to engage partners. This infrastructure must be adequately resourced and financed using performance standards and accountability to the public and policymakers.
Legal Authorities
The legal basis for public health at the federal level is defined in the Public Health Services Act. 13 It has been amended over the years to provide the legal basis for many public health authorities including disease reporting, prevention, and control. At the state and local level additional authorities govern the legal basis for public health practice. Most recently, many of these authorities are under threat and their future is unclear. Public health authorities do need to be strengthened, modernized, and better understood by both policymakers and the public. 14
Funding
Funding for the public health system has been a significant challenge. It is generally accepted that the proportion of funding for the public health represent only 2.4% of the overall $4 trillion in spending for health in the United States 15 or $286 per capita overall in 2018. State contributions for public health is highly variable. In 2020 state funding ranged from $18.44 per capita for residents in the state of New Jersey to $69.25 for residents in the state of Alaska. 16 A recent study reported that the system needs a boost of $4.5 billion annually 17 in federal funding for state, local and territorial agencies to achieve a funding level that can support core capacities.
It is also known that public health operates in an incongruent fiscal environment. Major increases in funding occur in cycles usually when a significant health threat enters the population. Funding is then allocated by various levels of government—often delayed and in inadequate amounts which are then diminished too early and with a performance expectation that far exceeds the resources provided. Often these funds are provided in ways that do not build long‐term infrastructure and creates a boom and bust administrative and programmatic process. The reasons for the lack of will to create a robust and long‐term infrastructure is astounding and poorly understood by the average citizen.
The current funding is highly dependent on federal funding principally from the CDC, HRSA and SAMSA. Other federal agencies like the National Highway Traffic and Safety Administration provide targeted funding for programs as well. Local funding support is highly variable and comes from inspection fees, clinical services, and state or local funding for specific programs, but the bulk of the funding comes from the federal level.
Workforce
The workforce for public health is also inadequate today and needs to be rebuilt in terms of number of workers and their skills for the future work. Since 2008 there has been a loss of more than 50,000 public health workers overall. A recent assessment of workforce needs found that a total of 80,000 full time equivalates are needed to get the system to an adequate state. 18 A 2021 assessment of the epidemiological needs for state health departments conducted by the Council of State and Territorial Epidemiologists (CSTE) showed that 2,196 additional positions were needed to provide basic public health work. This was despite a 23% increase in staffing that occurred primarily during the COVID‐19 pandemic. 19 Because the bulk of the funding for these positions are from federal funds there is a great deal of concern that the current capacity cannot be maintained after the pandemic surge of funds. The other concern is that this assessment is only an estimate of the needs at state health departments and does not represent the need for epidemiologists in other federal health agencies.
The public health workforce is ill defined in terms of numbers and what jobs are included. It currently consists of more than 30 different job categories and has people with a range of skills. There is an urgent need to better define the public health workforce by having the federal government create a Standard Operational Classification (SOC) for public health. By creating a SOC, the nation will be better able to define public health workers and enumerate the level of workers for future workforce planning.
Workforce Skills
Historically, public health skills included competencies in epidemiology, statistics, environmental health, health policy and management, and social and behavioral health. Specialized skills in maternal and child health, global health, infectious disease, injury control, health education, chronic diseases, and emergency preparedness are also commonly acquired. Skills needed for the future modern workforce include enhanced scientific and technical skills in molecular, genetic, and forensic microbiology for laboratorians and disease surveillance workers as well as enhanced skills in disease modelling and tracking. These skillsets will need to be applied for the full range of diseases of public health concern.
New and enhanced leadership skills to be more adept at operating in a highly politized environment across the full spectrum of political ideologies is needed for all program managers. Managing through influence will be a strongly needed skillset best exemplified by the concept of meta‐leadership. 20 Meta‐leadership is a concept of successfully managing up and down ones organizational structure as well as across organizational silos, often using influence and persuasion and not command authority to accomplish your goals.
People with skills in community and private sector engagement will be in extreme demand. Partnering is not a natural act and requires work, especially because the future work of public health increasingly will include multisectoral partnerships outside the health sector. Skills such as coalition building, conflict resolution, and organizational development will be essential in building an effective public health infrastructure. Building exceptional communication skills across the full range of platforms from public speaking and social media to public writing and visual media (TV and radio) at many levels of the organization below the chief executive level will be vital. Experience at testifying at legislative hearings, townhalls, and other public events under both calm and hostile environments is an essential skill for the future. Becoming adept at risk communication is a specialized skillset for all future public health practitioners in any level of management role. This skillset must be capable of enabling public trust in science and government while helping to improve public science literacy. Finally, becoming an effective advocate—building an advocacy agenda and a following that agenda—will give the practitioners of the future the capacity to get others to adopt their health recommendations.
Data Systems
Public health is a data driven discipline which prides itself on its strong use of the scientific methods and evidence. Unfortunately, the health threats that exist today are more complex, evolve at a rapid pace and are better understood on a timeline that requires greater analytic speed than the system currently has. The opioid epidemic, the COVID‐19 pandemic, and the growing number of foodborne outbreaks all demonstrate the need for more robust and timely data systems. A radical transformation and full integration of the US public health and health care system data infrastructures is needed now. Defining a new health technology highway is essential, much like the Federal‐Aid Highway Act of 1956 defined a national highway infrastructure and laid the way for our rationalized and interconnected national highway system. The challenges of health disparities, maternal mortality, and climate change all represent ongoing challenges to the public health system's need to have more robust and timely access to data at a granular enough level to do a proper assessment of the risks and craft solutions to them. Developing a single patient identifier would be an important first step. A data and surveillance modernization effort to build out the disease tracking and reporting system of the future is also drastically needed.
Governance of these systems needs to be enhanced because of the patchwork of data systems in existence today. This is essential to provide the utmost in data privacy and security. Cybersecurity of health data needs to be improved at all levels and training of the entire workforce is essential in line with the emerging threat environment.
Technology
Data systems are only the beginning. The public health infrastructure needs to be on the cutting edge of the use of genetic technology for forensic disease tracking. It also needs to have top‐of‐the‐line laboratory and analytical capabilities in every state health department. The system must have the comprehensive capacity to rapidly track and evaluate pathogenic organisms using next generation genetic tools. The system must also have a robust methodology to forecast disease as a tool for prevention and early intervention. This disease modelling capability must be state of the art and achieve world class status over the next ten years.
Partnerships
Building partnerships across the public health sector as well as across other sectors both domestically and globally is imperative. Strong multisectoral partnerships create an infrastructure collaborative that creates resiliency in the public health system by building business interdependencies to address a broad range of community needs. It leverages the strengths and bolsters the weaknesses of entities in the partnership and allows for stronger programmatic engagement. It also has the potential to make a political powerhouse that can support community needs when a health threat arrives. Potential partners include the private business, academic, faith, and education communities at a minimum.
Accountability
In everyday practice governmental public health systems have strong oversight through the various legislative bodies, auditing entities, and public advisory boards. They also have several entities in the private sector that provide voluntary and standard setting accreditation throughout the system. For the educational component there is the Council on Education for Public Health (CEPH). CEPH provides accreditation for programs and schools of public health. This accreditation sets a framework for certification and is overseen by the US Department of Education. CEPH accreditation provides assurance that the training received by people receiving public health education in the United States is of a high quality. All CEPH accredited schools and programs undergo a reaccreditation process every five years.
For people who receive training in public health, a National Board Exam also exists by the National Board of Public Health Examiners (NBPHE). While voluntary and relatively new, this certification is growing in importance as the benchmark for graduates of CEPH‐accredited schools and programs of public health. Recently the NBPHE has allowed people with a minimal set of practice experiences to sit for the exam and if they pass become certified in public health. Recertification is required every ten years to demonstrate continued competency in public health as well as continuing education credits to foster and demonstrate lifelong learning.
The Public Health Accreditation Board provides accreditation for governmental public health agencies. To date 80% of the population is covered by an accredited health department. However, this figure is deceptive since it does not include many of the smaller health departments. Accreditation has been shown to make a difference in improvements in quality and enhanced awareness of strengths and weaknesses. 21 Accreditation should continue to be promoted for all governmental agencies to achieve and maintain. A ten‐year goal would be to have this as the standard for all governmental public health agencies.
Accountability includes a robust public health systems research program. The capacity to do assessment and evaluation of all aspects of the performance of the public health agency and its programs is essential for any learning health system. The goal must be to understand the past as well as be prepared to anticipate the future through data driven program management.
Advocacy and Driving the Agenda
Having the capacity to make the case for the resources, tools, and programs to improve the public's health is an important capacity and one that goes beyond the material aspects of infrastructure. Governmental public health by its very nature improves health through policy development and service provision when needed. But the public support to provide for policy change and the resources for programs does not come with out effort. That effort to educate, advocate, and build support in a constructive way is required to drive a pro‐health agenda. Optimal health requires a population health approach and the ability to influence others to support the infrastructure to achieve it.
Conclusion
The central challenge for the nation is to structure and resource the nation's health and public health system to meet the strategic needs of the nation to perform its health security mission and build a next generation public health system. Public health leaders must see themselves as the chief health strategist for their community as described in the Public Health 3.0 concept. 22 The governmental agency should be structured and resources to deliver the ten essential / functional health services. Such as system must have powerful data systems to deliver timely and actionable information that is interoperable across the entire health system. It should also have the capacity to incorporate data streams from other aspects of society as needed. Adequate and sustainable funding streams and accountable accredited systems are essential to ensure the ability to document the return on investment for the public's investment. An essential goal over the next ten years will be to harmonize statutory authorities across jurisdictions and rationalize disease reporting systems. All systems must have vibrant, cross‐sector partnerships as well. No community can be considered prepared or resilient without a robust public health system.
References
- 1. The Institute of Medicine . The Future of Public Health. National Academy Press; 1988. [Google Scholar]
- 2. Merriam‐Webster . Definition of infrastructure. https://www.merriam‐webster.com/dictionary/infrastructure. Accessed April 7, 2022.
- 3. Oliver T. The politics of public health policy. Ann. Rev. Public Health. 2006;27:195‐233 [DOI] [PubMed] [Google Scholar]
- 4. Hall MA, Mello MM, Studdert DM. The legal authority for States’ stay‐at‐home orders. N Engl J Med. 2020; 383:e29. [DOI] [PubMed] [Google Scholar]
- 5. Community resilience . Public Health Emergency website. Office of the Assistant Secretary for Preparedness and Response. https://www.phe.gov/Preparedness/planning/abc/Pages/community‐resilience.aspx. Accessed March 15, 2023.
- 6. Woolf SH, Aron L, eds. U.S. Health in International Perspective: Shorter Lives, Poorer Health. National Research Council and Institute of Medicine, National Academies Press; 2013. [PubMed] [Google Scholar]
- 7. ASTHO . State and Local Health Department, Governance Classification System. https://www.astho.org/Research/Data‐and‐Analysis/State‐and‐Local‐Governance‐Classification‐Tree/. Published 2014. Accessed October 29, 2020.
- 8. DeSalvo K, Hughes B, Bassett M, Benjamin G, Fraser M, Galea S, Garcia N, Howard J. Public health COVID‐19 impact assessment: lessons learned and compelling needs. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. April 7, 2021. 10.31478/202104c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. CDC . Health Professionals Gateway: 10 Essential Public Health Services. US Department of Health and Human Services; 2021. https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html. Accessed March 15, 2023.
- 10. Committee on Public Health Strategies to Improve Health; Institute of Medicine . For the Public's Health: Investing in a Healthier Future. National Academies Press; 2012. [PubMed] [Google Scholar]
- 11. Public Health National Center for Innovations . Foundational public health services in action. PHNCI. https://phnci.org/national‐frameworks/fphs. Published November 2018.
- 12. Foundational public health services . Resolve website. https://www.resolve.ngo/site‐healthleadershipforum/defining‐and‐constituting‐foundational‐capabilities‐and‐areas.htm#. Accessed March 15, 2023.
- 13. US Congress . (1952) United States Code: The Public Health Service, 42 U.S.C. §§ 201‐291n . [Periodical] Retrieved from the Library of Congress, https://www.loc.gov/item/uscode1952‐004042006a/.
- 14. Goodman RA, Moulton A, Matthews G, Shaw F, Kocher P, Mensah G, Zaza S, Besser R, Centers for Disease Control and Prevention . Law and public health at CDC. Morb Mortal Wkly Rep. 2006;55(2):29‐33 [PubMed] [Google Scholar]
- 15. Himmelstein DU, Woolhandler S. Public health's falling share of US health spending. Am J Public Health. 2016;106(1):56‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Trust for America's Health . The impact of chronic underfunding on America's public health system: Trends, risks, and recommendations, https://www.tfah.org/report‐details/publichealthfunding2020/. Published April 2020. Accessed March 15, 2023.
- 17. Developing a finance system to support public health infrastructure . Resolve website. https://www.resolve.ngo/site‐healthleadershipforum/developing‐a‐financing‐system‐to‐upportpublic‐health‐infrastructure.htm. Accessed April 4, 2022.
- 18. de Beaumont Foundation . Staffing Up: Workforce Levels Needed to Provide Basic Public Health Services for All Americans. https://debeaumont.org/wp‐content/uploads/2021/10/Staffing‐Up‐FINAL.pdf. Published October 2021. Accessed March 15, 2023.
- 19. Arrazola J, Auer S. Assessment of epidemiology capacity in state health departments — United States, 2021. MMWR Morb Mortal Wkly Rep. 2022;71:484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marcus LJ, Dorn BC, Henderson JM. Meta‐leadership and national emergency preparedness: A model to build government connectivity. Biosecur Bioterror. 2006;4(2):128‐34. [DOI] [PubMed] [Google Scholar]
- 21. Kronstadt J, Meit M, Siegfried A, Nicolaus T, Bender K, Corso L. Evaluating the impact of national public health department accreditation ― United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:803‐806. 10.15585/mmwr.mm6531a3externalicon. [DOI] [PubMed] [Google Scholar]
- 22. DeSalvo KB, Wang YC, Harris A, Auerbach J, Koo D, O'Carroll P. Public Health 3.0: A call to action for public health to meet the challenges of the 21st century. Prev Chronic Dis. 2017;14:170017. [DOI] [PMC free article] [PubMed] [Google Scholar]


