Abstract
Policy Points.
We reviewed some of the recent advances in education and health, arguing that attention to social contextual factors and the dynamics of social and institutional change provide critical insights into the ways in which the association is embedded in institutional contexts.
Based on our findings, we believe incorporating this perspective is fundamentally important to ameliorate current negative trends and inequality in Americans’ health and longevity.
Keywords: education, health, social policy
Greater educational attainment is strongly associated with better health. Research has found this association across many world regions, 1 , 2 , 3 , 4 social contexts, 5 , 6 , 7 , 8 , 9 social groups, 10 , 11 , 12 , 13 and historical periods. 14 , 15 , 16 , 17 , 18 , 19 This association is not limited to one health outcome, but has been documented for an array of important measures, including self‐rated health, biological risk, chronic conditions, mental health, mortality, and physical and cognitive functioning. 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 The evidence has been consistent and voluminous, leading to the wide acceptance of this association as one of the leading social scientific “truths.”
Despite this enormous body of research, the question of how education influences health outcomes continues to generate a significant amount of research interest. In large part, researchers’ attention to this association reflects the growing recognition that the association is highly malleable. Research has shown that while more years of education are associated with better health, the magnitude of the association can vary widely, for example, across countries, within country administrative units such as states and provinces, across race/ethnic and gender groups, and across birth cohorts. 8 , 10 , 12 , 28 , 29 , 30 These differences are leading researchers to consider how and why this malleability exists. Why and how do administrative units and social categories impact the association? Are there mechanisms at the institutional and individual levels (or combinations thereof) that can help us understand this dynamism? How is the education‐health association embedded in nested institutional contexts reflecting families, communities, institutions, and policies? 31 , 32
Historical dynamism and the explosion of knowledge play important roles in understanding the impact of education on health. 14 , 33 Societies are constantly adapting or developing in response to scientific and technological innovations. We have observed this throughout modern history. In fact, technological change and scientific knowledge have been one of the widely recognized precursors to improvements in health. 34 , 35 Since the turn of the twentieth century, significant scientific and technological advancements (e.g., germ theory, development of modern medicine, water filtration systems, and vaccines) have ushered in sweeping improvements in population health such as longer life expectancy and lower infant mortality. Education has increasingly come to play a key role in determining health because of individuals’ ability to use knowledge to garner health advantages.
In this Perspective, we build on this large body of literature by considering how the education‐health association is contingent on combinations of macro influences including institutional context, historical change, and scientific and technological advancements, and we consider how different parts of the educational distribution may be impacted. Throughout this article, we review important conceptual frameworks, which are combined and summarized in Figure 1, and we draw on empirical studies that focus on the US adult population. We largely limit our focus to the US context solely for heuristic purposes and to impose necessary boundary constraints on the discussion. Concomitantly, we also focus exclusively on educational attainment (i.e., years of schooling or degrees obtained). We do, however, recognize the importance of educational quality on health. 36 Adult health has been defined broadly to encompass physical health and functioning as well as mortality.
Figure 1.
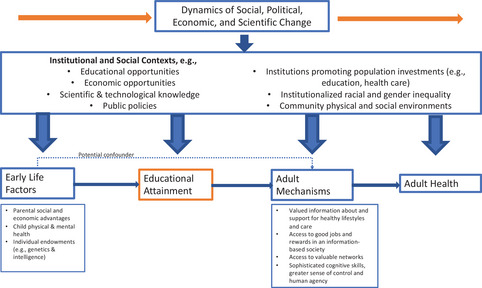
Embedding the Education‐Health Association in a Dynamic Macro Environment [Colour figure can be viewed at wileyonlinelibrary.com]
Lastly, we build on other recent reviews examining the association between education and health. 37 , 38 , 39 Long‐term trends in US mortality relative to other high‐income countries, as well as the growing inequality in health, have alarmed policymakers, public health workers, and health researchers alike. We build on these prior reviews by reemphasizing the dynamic nature of the education‐health association across many different contexts and historical periods. Education has become a core institutional and personal resource to improve health and health inequity, and without understanding this association, future improvements in population health will be threatened.
The Conceptual Ties Between Education and Adult Health
Social science researchers, especially sociologists and economists, have long been interested in the conceptual ties between education and health, with significant development in understanding individual‐level mechanisms. 32 , 40 , 41 , 42 , 43 , 44 Figure 1, in part, graphically summarizes some of these mechanisms. It shows that health is tied to educational attainment through myriad resources, including health literacy that promotes healthier lifestyles, more stable and rewarding employment opportunities, vast social networks, greater sense of control and human agency, and more sophisticated cognitive skills to navigate life. In general, having access to and using these resources promotes greater agency to make choices that benefit one's health throughout life. Differences in ability to access and use resources help explain the persistent health inequality between adults with greater and lower levels of education.
The multiplicity of mechanisms associated with education and health reinforces the association across different contexts. These basic mechanisms are seen as highly flexible, complementary, and often overlapping and can lead to a variety of behaviors and choices over people's lives that benefit—or not—their health. For example, highly educated persons have greater knowledge about factors influencing health conditions; they are connected to supportive social networks; they have the knowledge, sense of personal control, and motivation to be proactive in minimizing exposures and enhancing behaviors that lead to good health; they work in jobs that provide greater economic resources that can be deployed to minimize risk (e.g., neighborhood choices); and they also work in jobs with greater intrinsic rewards and control over work activities that reduce stress. Less‐educated persons often lack these resources, leading to a persistent gap in educational differences in health and mortality.
The fact that education may be associated with health through many mechanisms points to the importance of education as a linchpin in population health over time and across populations. 40 , 41 , 42 It also signifies the importance of education as a fundamental cause of disease, which allows education to be connected to health even when mechanisms may change or differ across contexts. 45 , 46 As such, one intervention alone cannot reduce health inequality across education groups. It is for this reason that education, as a cause of causes, is often considered a fundamental cause of disease and disability. 45 , 46 In the discussion that follows, we examine more closely how contextual factors may be impacting these connections.
The Dynamic Nature of the Education‐Health Association
The dynamic nature of the association between education and health can be readily observed in the United States since the mid‐20th century. For example, while Kitagawa and Hauser's important work documented the educational gradient in mortality for the 1960 US population, 47 they also noted that this gradient was surprisingly absent in one demographic group: men aged 65 years and older. Since their landmark study, a number of studies have documented the widening of the educational gradient in US adult mortality in the latter half of the 20th century and into the 21st century, 21 , 48 , 49 , 50 , 51 although the trends differed for racial/ethnic subgroups and by gender and region. 46 , 49 , 52 , 53
Through much of the latter part of the 20th century, the widening gradient generally reflected improved mortality for highly educated persons, with mortality rates being relatively stable or slightly increasing among less‐educated persons. 30 , 48 This pattern was mirrored for adult health. 54 Toward the end of the 20th century, however, while the educational gap continued to widen, the reasons for the widening changed. Highly educated persons continued to experience declines in mortality while less‐educated persons began to experience absolute increases in mortality rates. 21 , 50 , 53 , 55 This challenges the idea that a “rising tide” of improvements in health and longevity over time are shared—even differentially across educational groups. Indeed, as the evidence shows, less‐educated persons are falling behind in their health and longevity in absolute as well as relative terms regardless of continued improvements in scientific knowledge and technology.
Life expectancy trends since the 1990s are shown in Figure 2 to illustrate the changing association between educational attainment and mortality. This figure highlights three important issues. First, the growing inequality in life expectancy between the lowest and highest educated more than doubled from 1990 to 2010. This held true across race and gender groups. Second, the national trends in life expectancy are being affected by the education‐specific trends. The stagnation and recently observed declines in life expectancy among Whites, for example, was a product of stagnation followed by absolute declines in life expectancy for people with less than a college education. 21 , 51 , 56 Although national trends did not look favorable for the overall population, college‐educated adults have continued to see improvements in life expectancy. Third, declines in life expectancy were observed among adults without a college degree at different periods. Adults with a high school diploma or less were the first group to experience declines in life expectancy around 1990. Adults with some college (but no bachelor's degree) started to experience life expectancy declines around 2010. College‐educated adults have been spared (for the time being). This has led some researchers to suggest that high levels of education act as a “personal firewall” to suboptimal conditions. 57 , 58 Compared to less‐educated adults, more‐educated adults have the personal resources to either compensate or overcome hazardous conditions (e.g., COVID‐19) or completely avoid them.
Figure 2.
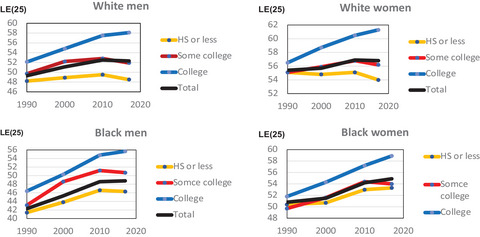
Life Expectancy at Age 25 [LE(25)] by Education, Sex, and Race, 1990–2017 [Colour figure can be viewed at wileyonlinelibrary.com]
We note that the educational distribution has not remained constant since 1990, with fewer persons having a high school degree or less and a substantial growth in the prevalence of persons with a bachelor's degree. One might expect that the two ends of the education distribution would both be increasingly negatively select since 1990. Yet, as Case and Deaton noted, real wages among the bachelor's degree group actually rose over the period, 56 the opposite of what one would expect given selection. Moreover, Montez and colleagues provided evidence consistent with the argument that the increasing mortality of less‐educated persons reflected higher rates of mortality among persons living in states where less‐educated persons are the least select and more subject to adverse state policies. 57 Although selection cannot be completely ruled out, most of the evidence runs counter to what one would expect given negative selectivity.
The dynamic nature of education‐health can also be observed in changes in the functional form of the association between education and mortality since the 1960s. Functional form analysis evaluates how mortality risk changes at different years of education. Researchers have elaborated on two potential explanations that describe the functional form of the education‐health association: credentialism and human capital. 32 , 59 Credentialism proposes that mortality will decrease at specific years of education because of the resources that those credentials bring: for education‐health in the latter part of the 20th century, a high school diploma (at 12 years) and a college degree (at 16 years) were two of the most important points. Human capital proposes a continuous decline in mortality risk across all years of education. These explanations are not mutually exclusive but can be combined.
From 1960 to 1990, the association between education and mortality largely reflected a “credentialist” explanation with significant declines in mortality risk at 12 years of education and 16 years of education. 47 , 60 Over the 30‐year period, the declines in mortality associated with 12 and 16 years of education increased, while little change in mortality rates was observed between these watershed points within the educational distribution. The credentalist pattern and the changes over time point to the importance of labor market mechanisms as explanations for the growing educational gap in mortality in the latter half of the 20th century.
Since 1990, however, changes in the functional form point to the increasing importance of a combined “credentialist/human capital” explanation for changes in the educational gradient. After 12 years of education, mortality rates now decline in almost a dose‐response pattern with each year of education, and the slope has steepened since the beginning of the 21st century. 32 , 59
The changing functional form between education and mortality since the 1960s points to the importance of historical changes in the macro context. Through the 1960s to the 1990s, credentialism most likely reflected the labor market mechanisms that arose during the post–World War II economic boom and rise of manufacturing. Blue‐collar work and unionization provided stable employment and access to good housing. 61 This period was also punctuated by vast social programs and resources to improve health and well‐being in the population (we elaborate on this in the following section). Since the 1990s, social and economic conditions have changed. Advances in educational attainment stalled, and persons with only a high school education found it difficult to secure access to stable employment, good housing, or other types of resources. 62 , 63 Moreover, health advantages associated with higher levels of education today also reflect a host of personal behaviors, such as being a nonsmoker, having a body mass index at or below 30, doing vigorous activity, exhibiting low rates of excessive drinking, having had colorectal screening, having had a mammogram, regularly wearing a seat belt, and having working smoke detectors in the home. 43 These associations between education and health behaviors, in combination with growing socioeconomic resources over the period among better‐educated people, 32 strongly suggest that advanced education is associated with a growing portfolio of personal resources that can be deployed to garner good health.
The importance of personal resources (and behaviors) for health across the education distribution can also be observed in the clustering of mortality risk. Less‐educated adults are not only more likely to die at younger ages, but most deaths occur across a wider range of ages. 50 , 64 The wider range of deaths reflects greater uncertainty in their lives, as well as larger variability in exposures. For well‐educated adults, mortality has a much narrower range of deaths at later ages, reflecting greater certainty and lower variability. 50 Well‐educated adults have similar health profiles. In the discussion that follows, we turn to possible reasons for these bifurcated patterns in health at the ends of the education distribution.
The Role of Context in Educational Disparities and Trends in Health and Longevity
Several studies have offered insights into the role of “social context” for understanding trends and disparities in the association between education and health. Figure 1 provides a partial list of some of the key contextual factors that have been identified in the literature. Contextual factors range from specific policy environments to geopolitical boundaries. Avendano and Kawachi provide a review of the ways in which a variety of upstream policies may be contributing Americans’ health disadvantages across the life course. 65 Other studies have focused on contexts referenced by neighborhoods, 66 racialized environmental conditions such segregation, 67 and policy and institutional contexts defined by geopolitical boundaries. 7 , 8 , 68 , 69 Zajacova and Lawrence provide an excellent overview of the scientific terrain in these areas. 38 Very few studies, however, have examined how contextual factors may be influencing changes in the association between education and health. However, research has started to move into this area. A recent example is a study of how policy changes are associated with educational disparities in mortality across US states. 57
Most studies that have sought to empirically explain changes in the association have largely focused their attention on changes in behavioral risk factors and the economic conditions of persons’ lives. 15 , 70 , 71 Cutler and his colleagues noted, for example, that changes in behavioral risk factors, while important, fall short of explaining the growing educational divide in health and longevity. 15 Montez and Zajacova considered health risk behaviors, economic resources (employment, occupation, poverty income, asset wealth, and home ownership), and social psychological factors (e.g., marriage and psychological distress) as potential explanations for the increased educational gradient in adult women's mortality. 70 , 71 They observed that increases in the gradient for women largely reflected the combination of health risk behaviors and economic conditions, and they hypothesized that the level of clustering of these resources and risks factors has become tighter over time.
Changes in the educational gradient with health has led to broader questions about the implications of the growing economic inequality in US society. For example, to answer the question about clustering of opportunities and resources, we need to understand why highly educated people are seeing resources become more readily available, while less‐educated adults have not only fallen behind, but have regressed compared to early historical periods. Why have resources and risks been redistributed to not only advantage the most advantaged, but also be pulled from the least? These conceptual insights will not only help us understand how the association between education and health has developed and changed, but also incorporate the role of context into considering how the associations between education and health are reinforced over time and allow us to reflect on potential pathways that impact either the low or high end of the distribution that contributes to this entrenchment.
In addition to policies, scholars have also attributed some of these changes to technological advancement. More than 50 years ago, Norman Ryder argued that the primary driver of contemporary social change is through technological innovation. 72 This idea of social change tied to technology is a cornerstone in the population health literature. Economic historians, for example, have posited that population's social capacity of health is directly tied to technological change. 33 , 34 , 73 Technological and scientific advances become increasingly embedded in social institutions, defining the institutional and personal resources that individuals in a population, especially educated individuals, can access and act on to enhance health and longevity throughout their lives.
Hayward and Sheehan offer a heuristic timeline of major social, biomedical, and technological changes across the 20th century that have influenced population health. 74 In the first half of the century, for example, a dizzying array of changes occurred such as the establishment of the Public Health Service, enactment of the Meat Inspection Act, the discovery of different blood types, refrigerators for home use, vaccine development for several prevalent infectious diseases, and the discovery of penicillin. The population in this period was also experiencing dramatic improvements in educational attainment, providing increased access and ability to act on institutional and personal resources for better health. High school graduation rates rose from about 10% in 1910, to 30% in 1930, and more than 50% in 1940. 75 Greater education coincided with improved hygienic practices and better health behaviors, mitigating exposures and lowering risk for everyone in the population.
In the 1930s, the New Deal launched a “contract” between the federal government and the population that affected many aspects of Americans’ well‐being. It especially helped to improve the lives of Americans who had the fewest resources, such as rural communities, older adults, and children. For example, the Tennessee Valley Authority and the Rural Electrification Act, the Social Security Act, and the establishment of a minimum wage accompanied additional technological advances such as the shift to hospital deliveries. The 1940s and 1950s brought additional broadening and deepening of the contract between the federal government (e.g., the establishment of the Centers for Disease Control and Prevention) and scientific advances (e.g., the licensing of the polio vaccine, the initiation of water fluoridation, mass production of penicillin, the start of the Interstate Highway System, and the GI Bill, which fueled college attendance). The 1960s witnessed the culmination of the New Deal in the form of the Great Society Programs, briefly cementing the social contract between the US population and the federal government. Not surprisingly, life expectancy substantially increased throughout this period in US history, incomes rose dramatically at about the same rate throughout the income distribution, and prosperity was shared across most of the population (although significant gender and racial inequality continued to exist). 76 These broad historical changes are plausible explanations for the relatively high levels of life expectancy in 1960 and the relatively low levels of inequality between less‐ and well‐educated groups. 47 Institutional investments in the population were broad, scientific and technological changes were accessible to most people, and prosperity was shared across a large swath of the population.
The dramatic improvements in health and reduction of inequality across education groups, however, came to an end. Since 1970, educational inequality in health and mortality has grown. Coincident with the growing educational inequality in health, income and wealth inequality also increased while economic growth rates stabilized. Additionally, while macroeconomic forces lead to concentrated wealth, health behaviors started to contribute more toward the growing inequality. For example, following the Surgeon General's Report in 1964, 77 smoking declined among well‐educated people, contributing to a long‐term decline in this risky behavior that is often associated with a host of chronic conditions and death. While smoking also declined among the less educated, the rate of decline was much smaller, leading to a growing educational gap in smoking. 48 , 78 , 79 Moreover, medical technology, health information, and the technological ways to access these advances exploded but was most used by well‐educated persons. 80 , 81 Other trends also point to the concentration of resources shown in Figure 1 among well‐educated persons (e.g., economic returns to a bachelor's degree, higher rates of marriage and family stability among well‐educated persons). 32 The concentration of resources and the mitigation of risks through the end of the 20th century and beginning of the 21st century have allowed well‐educated adults to live longer and in better health.
Although these trends provide some evidence that the concentrated health improvements among the well educated accounts for the widening educational gap in health, it is less clear how or whether these trends in health‐related resources played a role in the widening variability of life chances among less‐educated persons. Note that related research on the changing relationship between income and US mortality has also documented a trend in the widening of variability in mortality among low‐income persons as well. 82 However, research outside the US also suggests that increased variability at the low end of the educational (or income) distribution is not necessarily a consequence of widening inequality in mortality. 83
The growing variability in mortality for less‐educated adults has been recently linked to changes in the balance of US federal and state policies and institutional factors and their growing influence in more recent decades. 7 , 57 , 58 , 68 , 69 , 84 , 85 Although it is impossible in this short review to go into detail regarding the sociohistorical reasons that led to the growing variability, the reasons can be summarized under the umbrella of New Federalism—that is, the transfer of federal authority to states for the administration of an array of social welfare programs (also known as devolution), state preemption laws constraining local authority, diverging economic and policy environments across states, and the polarization of state policy contexts along political lines. 57 , 84 , 86 In essence, states have become important institutional drivers of educational differences in health as well as health trends. For example, states that implemented more liberal policies since 1970—policies that expanded economic regulations and protected marginalized groups—saw a rise in their life expectancy, while states that implemented more conservative policies were more likely to see a lowering of life expectancy for its residents. 84 As noted by Montez and colleagues, “[L]ess educated persons possess fewer resources of their own and face greater risks in their daily lives, all of which make the resources, opportunities, and protections provided by their state particularly salient.” 57
Empirically, this body of research makes clear that the educational gradient in health and mortality varies widely across US states. 57 Second, state‐level variability is driven almost entirely by state differences in the health of less‐educated persons. The health of highly educated persons is strikingly similar across the states for a number of health outcomes, 8 providing evidence of the outsized role that context has for less‐educated persons compared to well‐educated persons. Finally, variability has grown in recent decades and is showing no sign of stabilizing, partly reflecting the political polarization of state policy contexts and state differences in the investments and deinvestments they make in their populations. State context clearly matters for variability in less‐educated Americans’ health and longevity, and the importance of state context has been growing for decades as the federal government has taken a smaller role in the lives of American adults.
Discussion
We have argued that the association between education and health is dynamic and highly contingent on macro contextual factors. Returning to Figure 1, contingencies include macro, historical changes that have led to the growing importance of education in our society in garnering health advantages via multiple and reinforcing mechanisms. Institutional contexts have also played a critical role in shaping heterogeneity in the association across education groups in a population. We have attempted not only to draw attention to the magnitude of change in the association over time but also to changes in the variation in health and longevity across the education distribution. These contingencies are overlapping and often not independent.
We have made these arguments in large part because much of the literature examining the association ignores these contingencies. The association is often characterized in ahistorical terms, with almost no attention given to how the association has changed and why. This has implications for anticipating future changes in the association and even understanding how inequality is potentially shaping overall population‐level trends in health and longevity. It also has implications for assessing and understanding the causal nature of the association between education and health. Education is far from exogenous in studying health outcomes. This association is embedded in sociohistorical changes and institutional arrangements that are fundamental in understanding the association and its dynamic nature.
The education‐health association is embedded in institutional contexts. Earlier we noted the importance of the embedding of technological and scientific knowledge in societal institutions that improve the social capacity in health at the population level. However, other institutional contexts operating at a subnational level also shape the association. We have illustrated this idea, drawing on the research examining US states as institutional contexts. A value of this example is that it highlights less‐educated individuals may be especially vulnerable to institutional contexts given their lack of personal resources that can be deployed at will and on a daily basis to ensure health and well‐being. It also appears that institutional contexts not only exacerbate the negative consequences of the absence of personal resources but also may mitigate the negative consequences of the absence of personal resources. For example, the educational gradient in health can be quite narrow (and has become narrower) in US states with robust social welfare policies and policies that invest in their population. Institutional contexts can provide compensating mechanisms for less‐educated persons that mitigate the negative health consequences of the lack of personal resources.
In thinking about future research on this topic, it is important to move beyond thinking of the association in simplistic “relative risk” or “causal effect” terms. For example, what do changes in the relative risk of mortality mean if one ignores how (and why) risks are changing at different points in the education distribution? What does a causal analysis mean without a careful conceptual analysis of education's links to specific mechanisms that garner health advantages in a population? Why might the association strengthen or subside over time? What lies behind differences in “uncertainty” in health across the education distribution? Addressing these questions by embedding the association in institutional contexts is vital to finding answers.
We acknowledge that contexts are not easy to define. Here, we have focused on national and state‐level institutional factors that have been shaping the association between education and health, but there are clearly other contextual influences to consider. A major challenge is how to conceptualize contextual factors in terms of the key actors, institutions, policies, the economic system, social norms, and more in which the association between education and health is embedded. 31 Increasingly, researchers are turning their attention to the National Research Council report 87 to develop hypotheses and expand conceptual frameworks to better understand major trends and disparities in the association between education and health. A recent example is the work by Montez and colleagues, which highlights the importance of macro contextual influences in the form of policies, politics, and profits. 69 Although a thorough review of these conceptual advances is beyond the scope of this paper, they represent important steps in developing a more sophisticated understanding of the association between education and health.
The association between education and health is central in developing a better understanding of the stagnation, erosion, and recent declines in US health and mortality. Recent empirical research 21 , 56 , 57 , 84 clarifies in significant ways how we got to where we are, but clearly the research record is far from complete. Making strides in reversing these trends will require additional research that incorporates insights about how major dynamic and contextual contingencies influence the association between education and health. The US's recent experiences with the opioid epidemic and the COVID‐19 pandemic have laid bare the disproportionate impact on less‐educated persons and the importance of institutional contexts as battlegrounds in fighting these inequities.
Improving the health of less‐educated groups will require policies that decrease their vulnerability to adverse health outcomes by increasing access to personal and institutional resources. In order to make this happen, it is critical to understand the following issues. First, as described earlier, the battleground for population health in the United States has shifted from the federal to the state level. Without a rebalancing of federal and state responsibilities for social welfare programs and other programs affecting population health (e.g., US Environmental Protection Agency federal and state regulatory bodies), a focus on state policy change is essential. Second, policy discussions should focus on “bundles” of policies that reflect investments in the population rather than a single policy. 84 Conceptually, a bundled approach allows investments in population health across a broad age range, from childhood into old age, with numerous multiplier effects of these investments for well‐being across the entire life course. This approach would undo some of the widespread, systemic changes related to other disinvestment policy bundles that occurred since the 1970s that have undercut health among the most vulnerable groups. Finally, it is important to acknowledge that policy investments and deinvestments do not take place in a vacuum. Instead, politics are increasingly playing an outsized role in policies affecting population health, often for the worst. 69 , 84 , 85 , 88 Policy recommendations must take into account political context and power structures in order to make progress on reducing health inequality in the United States. Policy cannot be devoid of the context in which it operates.
Limitations
While this Perspective provides an empirically informed argument for considering the dynamism between education and health, it is important to note some limitations that could not be fully addressed due to space constraints. First, the association between education and health is also greatly impacted and influenced by race and gender stratification systems. Prior work has found differential returns and pathways. 12 , 89 , 90 , 91 , 92 In keeping with this review, we encourage researchers to consider how context and historical periods may impact the education‐health association across groups, especially when evaluating within group inequality.
Second, we have focused almost exclusively on US studies. Numerous studies outside of the US have shown a positive association between education and health, but the mechanisms or degree of inequality may differ. 93 , 94 , 95 Incorporating a global perspective will undoubtedly provide additional evidence of dynamic changes in the education‐health association, especially as it relates to policy environments and other more macro social, political, and economic conditions. Relatedly, when evaluating context, we have incorporated studies that have focused exclusively on US states; however, other institutional contexts, both health and social, also have an important role.
Lastly, although we provide a brief overview of potential individual‐level mechanisms, we do not address causality directly. A number of studies evaluating the association between education and health have undertaken this work, and several others have established the theoretical basis for increased levels of education leading to improved health outcomes. 96 , 97 , 98 Changes to education‐health association most likely reflect changes in causal pathways as well, which will be of interest to researchers and policymakers.
Funding/Support: Partial support for this paper was provided by infrastructure support from the National Institute on Aging (NIA) (P30 AG066614, P30 AG17265 and P30 AG066589) and National Institute on Child Health and Human Development (P2CHD042849), a training grant from NIA (T32 AG000037), and a research grant from NIA (R56 AG057778).
Conflict of Interest Disclosure: None.
Acknowledgments: The authors would like to thank Hyungmin Cha and K. J. Davidson‐Turner at the University of Texas at Austin for their helpful suggestions and comments.
References
- 1. Mackenbach JP, Bos V, Andersen O, et al. Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol. 2003;32(5):830‐837. [DOI] [PubMed] [Google Scholar]
- 2. Vathesatogkit P, Batty GD, and Woodward M. Socioeconomic disadvantage and disease‐specific mortality in Asia: systematic review with meta‐analysis of population‐based cohort studies. J Epidemiol Community Health. 2014;68(4):375. [DOI] [PubMed] [Google Scholar]
- 3. KC S, Lentzner H. The effect of education on adult mortality and disability: a global perspective. Vienna Yearbook Popul Res. 2010;8(1):201‐235. [Google Scholar]
- 4. Sandoval MH, Turra CM, Luz L. The importance of education for middle‐ and old‐age mortality in Chile: estimates from panel data linked to death records. J Aging Health. 2021;34(1):71‐77. [DOI] [PubMed] [Google Scholar]
- 5. Leopold L. Education and physical health trajectories in later life: a comparative study. Demography. 2018;55(3):901‐927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Montez JK, Sheehan C, Zajacova A, Connor D. State‐level variation in the association between educational attainment and sleep. Popul Res Policy Rev. 2021. [Google Scholar]
- 7. Montez JK, Zajacova A, Hayward MD. Disparities in disability by educational attainment across US states. Am J Public Health. 2017;107(7):1101‐1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Montez JK, Hayward MD, Zajacova A. Educational disparities in adult health: US states as institutional actors on the association. Socius. 2019;5:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kemp BR, Montez JK. Why does the importance of education for health differ across the United States? Socius. 2020;6:2378023119899545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ross CE, Masters RK, Hummer RA. Education and the gender gaps in health and mortality. Demography. 2012;49(4):1157‐1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kimbro RT, Bzostek S, Goldman N, Rodríguez G. Race, ethnicity, and the education gradient in health. Health Aff (Millwood). 2008;27(2):361‐372. [DOI] [PubMed] [Google Scholar]
- 12. Everett BG, Rehkopf DH, and RG Rogers. The nonlinear relationship between education and mortality: an examination of cohort, race/ethnic, and gender differences. Popul Res Policy Rev. 2013;32(6):893‐917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schwandt H, Currie J, Bar M, et al. Inequality in mortality between Black and White Americans by age, place, and cause and in comparison to Europe, 1990 to 2018. Proc Natl Acad Sci U S A. 2021;118(40):e2104684118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baker DP, Leon J, Smith Greenaway EG, Collins J, Movit M. The education effect on population health: a reassessment. Popul Dev Rev. 2011;37(2):307‐332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cutler DM, Lange F, Meara E, Richards‐Shubik S, Ruhm CJ. Rising educational gradients in mortality: the role of behavioral risk factors. J Health Econ. 2011;30(6):1174‐1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lauderdale DS. Education and survival: birth cohort, period, and age effects. Demography. 2001;38(4):551‐561. [DOI] [PubMed] [Google Scholar]
- 17. Lynch SM. Cohort and life‐course patterns in the relationship between education and health: a hierarchical approach. Demography. 2003;40(2):309‐331. [DOI] [PubMed] [Google Scholar]
- 18. Masters RK, Hummer RA, and DA Powers. Educational differences in US adult mortality: a cohort perspective. Am Sociol Rev. 2012;77(4):548‐572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Frase RT, Bauldry S. The expansion of higher education and the education‐health gradient in the United States. Soc Curr. 2021;9(1):70‐86. [Google Scholar]
- 20. Chiu C‐T, Hayward M, Saito Y. A comparison of educational differences on physical health, mortality, and healthy life expectancy in Japan and the United States. J Aging Health. 2016;28(7):1256‐1278. [DOI] [PubMed] [Google Scholar]
- 21. Sasson I, Hayward MD. Association between educational attainment and causes of death among white and Black US adults, 2010–2017. JAMA. 2019;322(8):756‐763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cantu PA, Sheehan CM, Sasson I, Hayward MD. Increasing education‐based disparities in healthy life expectancy among US non‐Hispanic whites, 2000–2010. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):319‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med. 2008;66(6):1334‐1345. [DOI] [PubMed] [Google Scholar]
- 24. Hansen T, Slagsvold B, Veenstra M. Educational inequalities in late‐life depression across Europe: results from the generations and gender survey. Eur J Ageing. 2017;14(4):407‐418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Farina MP, Zhang YS, Kim JK, Hayward MD, Crimmins EM. Trends in dementia prevalence, incidence, and mortality in the United States (2000‐2016). J Aging Health. 2022;34(1):100‐108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Farina MP, Hayward MD, Kim JK, Crimmins EM. Racial and educational disparities in dementia and dementia‐free life expectancy. J Gerontol B Psychol Sci Soc Sci. 2020;75(7):e105‐e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988‐1994). Soc Sci Med. 2008;66(1):72‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. von dem Knesebeck O, Verde PE, Dragano N. Education and health in 22 European countries. Soc Sci Med. 2006;63(5):1344‐51. [DOI] [PubMed] [Google Scholar]
- 29. Mackenbach JP, Kulhánová I, Bopp M, et al. Variations in the relation between education and cause‐specific mortality in 19 European populations: a test of the “fundamental causes” theory of social inequalities in health. Soc Sci Med. 2015;127:51‐62. [DOI] [PubMed] [Google Scholar]
- 30. Miech R, Pampel F, Kim J, Rogers RG. The enduring association between education and mortality: the role of widening and narrowing disparities. Am Sociol Rev. 2011;76(6):913‐934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zimmerman E, Woolf SH. Understanding the relationship between education and health. In: NAM Perspectives. Washington, DC: National Academy of Medicine; 2014. [Google Scholar]
- 32. Hayward MD, Hummer RA, Sasson I. Trends and group differences in the association between educational attainment and US adult mortality: implications for understanding education's causal influence. Soc Sci Med. 2015;127:8‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Deaton A. The Great Escape: Health, Wealth, and the Origins of Inequality. Princeton, NJ: Princeton University Press; 2014. [Google Scholar]
- 34. Cutler D, Deaton A, Lleras‐Muney A. The determinants of mortality. J Econ Perspect. 2006;20(3):97‐120. [Google Scholar]
- 35. Cutler D, Miller G. The role of public health improvements in health advances: the twentieth‐century United States. Demography. 2005;42(1):1‐22. [DOI] [PubMed] [Google Scholar]
- 36. Walsemann KM, Gee GC, Ro A. Educational attainment in the context of social inequality: new directions for research on education and health. Am Behav Sci. 2013;57(8):1082‐1104. [Google Scholar]
- 37. Hummer RA, Hernandez EM. The effect of educational attainment on adult mortality in the United States. Popul Bull. 2013;68(1):1‐16. [PMC free article] [PubMed] [Google Scholar]
- 38. Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273‐289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Montez JK, Chapter Brooks JD. 6: Educational attainment and adult health. In: Ferraro KF, Carr D, eds. Handbook of Aging and the Social Sciences. 9th ed. Cambridge, MA: Academic Press; 2021:83‐98. [Google Scholar]
- 40. Ross CE, Wu CL. Education, age, and the cumulative advantage in health. J Health Soc Behav. 1996;37(1):104‐120. [PubMed] [Google Scholar]
- 41. Ross CE, Mirowsky J. Refining the association between education and health: the effects of quantity, credential, and selectivity. Demography. 1999;36(4):445‐460. [PubMed] [Google Scholar]
- 42. Mirowsky J, Ross CE. Education, Social Status, and Health. New York, NY: Aldine De Gruyter; 2003. [Google Scholar]
- 43. Cutler DM, Lleras‐Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29(1):1‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cutler DM, Lleras‐Muney A. Education and Health: Evaluating Theories and Evidence. National Bureau of Economic Research working paper 12352. https://www.nber.org/papers/w12352. Published July 2006. Accessed November 9, 2022.
- 45. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;Spec No:80‐94. [PubMed] [Google Scholar]
- 46. Masters RK, Link BG, Phelan JC. Trends in education gradients of “preventable” mortality: a test of fundamental cause theory. Soc Sci Med. 2015;127:19‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kitagawa EM, Hauser PM. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- 48. Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff (Millwood). 2008;27(2):350‐360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Montez JK, Hummer RA, Hayward MD, Woo H, Rogers RG. Trends in the educational gradient of US adult mortality from 1986 to 2006 by race, gender, and age group. Res Aging. 2011;33(2):145‐171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sasson I. Trends in life expectancy and lifespan variation by educational attainment: United States, 1990–2010. Demography. 2016;53(2):269‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sasson I. Diverging trends in cause‐specific mortality and life years lost by educational attainment: evidence from United States vital statistics data, 1990–2010. PLoS One. 2016;11(10):e0163412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lin SF, Beck AN, Finch BK, Hummer RA, Masters RK. Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health. 2012;102(11):2157‐2163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Montez JK, Berkman LF. Trends in the educational gradient of mortality among US adults aged 45 to 84 years: bringing regional context into the explanation. Am J Public Health. 2014;104(1):e82‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Goesling B. The rising significance of education for health? Social Forces. 2007;85(4):1621‐1644. [Google Scholar]
- 55. Olshansky SJ, Antonucci T, Berkman L, et al. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff (Millwood). 2012;31(8):1803‐1813. [DOI] [PubMed] [Google Scholar]
- 56. Case A, Deaton A. Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed. Proc Natl Acad Sci U S A. 2021;118(11):e2024777118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Montez JK, Zajacova A, Hayward MD, Woolf SH, Chapman D, Beckfield J. Educational disparities in adult mortality across US states: how do they differ, and have they changed since the mid‐1980s? Demography. 2019;56(2):621‐644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Montez JK, Hayward MD, Wolf DA. Do US states’ socioeconomic and policy contexts shape adult disability? Soc Sci Med. 2017;178:115‐126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Montez JK, Hummer RA, Hayward MD. Educational attainment and adult mortality in the United States: a systematic analysis of functional form. Demography. 2012;49(1):315‐336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Backlund E, Sorlie PD, Johnson NJ. A comparison of the relationships of education and income with mortality: the National Longitudinal Mortality Study. Soc Sci Med. 1999;49(10):1373‐1384. [DOI] [PubMed] [Google Scholar]
- 61. Goldin CD, Katz LF. The Race Between Education and Technology. Boston, MA: Harvard University Press; 2009. [Google Scholar]
- 62. Kalleberg AL. Precarious work, insecure workers: employment relations in transition. Am Sociol Rev. 2009;74(1):1‐22. [Google Scholar]
- 63. Bowen WG, Chingos MM, McPherson M. Crossing the Finish Line: Completing College at America's Public Universities. Princeton, NJ: Princeton University Press; 2009. [Google Scholar]
- 64. Brown DC, Hayward MD, Montez JK, Hummer RA, Chiu CT, Hidajat MM. The significance of education for mortality compression in the United States. Demography. 2012;49(3):819‐840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Avendano M, Kawachi I. Why do Americans have shorter life expectancy and worse health than do people in other high‐income countries? Annu Rev Public Health. 2014;35:307‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wight RG, Aneshensel CS, Miller‐Martinez D, Botticello AL, Cummings JR, Karlamangla AS, Seeman TE. Urban neighborhood context, educational attainment, and cognitive function among older adults. Am J Epidemiol. 2006;163(12):1071‐1078. [DOI] [PubMed] [Google Scholar]
- 67. Glymour MM, Manly JJ. Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychol Rev. 2008;18(3):223‐254. [DOI] [PubMed] [Google Scholar]
- 68. Montez JK, Zajacova A, Hayward MD. Explaining inequalities in women's mortality between US states. SSM Popul Health. 2016;2:561‐571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Montez JK, Hayward MD, Zajacova A. Trends in US population health: the central role of policies, politics, and profits. J Health Soc Behav. 2021;62(3):286‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Montez JK, Zajacova A. Explaining the widening education gap in mortality among US white women. J Health Soc Behav. 2013;54(2):166‐182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Montez JK, Zajacova A. Why is life expectancy declining among low‐educated women in the United States? Am J Public Health. 2014;104(10):e5‐e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ryder NB. The cohort as a concept in the study of social change. Am Sociol Rev. 1965;30(6):843‐861. [PubMed] [Google Scholar]
- 73. Easterlin RA. Growth Triumphant: The Twenty‐First Century in Historical Perspective. Ann Arbor, MI: University of Michigan Press; 1997. [Google Scholar]
- 74. Hayward MD, Sheehan CA. Does the body forget: adult health, life course dynamics, and social change. In: Shanahan MJ, Mortimer J, Johnson M, eds. Handbook on the Life Course. 2nd ed. New York, NY: Springer Press; 2016. [Google Scholar]
- 75. Goldin C. America's graduation from high school: the evolution and spread of secondary schooling in the twentieth century. J Econ History. 1998;58(2):345‐374. [Google Scholar]
- 76. Stone C, Trisi D, Sherman A, Beltran J. A guide to statistics on historical trends in income inequality. Center on Budget and Policy Priorities. https://www.cbpp.org/research/poverty‐and‐inequality/a‐guide‐to‐statistics‐on‐historical‐trends‐in‐income‐inequality. Updated January 13, 2020. Accessed November 7, 2022.
- 77. Surgeon General's Advisory Committee on Smoking and Health . Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Public Health Service; 1964. [Google Scholar]
- 78. Pampel FC. Age and education patterns of smoking among women in high‐income nations. Soc Sci Med. 2003;57(8):1505‐1514. [DOI] [PubMed] [Google Scholar]
- 79. Denney JT, Rogers RG, Hummer RA, Pampel FC. Education inequality in mortality: the age and gender specific mediating effects of cigarette smoking. Soc Sci Res. 2010;39(4):662‐673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Martin SP, Robinson JP. The income digital divide: trends and predictions for levels of internet use. Social Problems. 2007;54(1):1‐22. [Google Scholar]
- 81. Brodie M, Flournoy RE, Altman DE, Blendon RJ, Benson JM, Rosenbaum MD. Health information, the Internet, and the digital divide. Health Aff (Millwood). 2000;19(6):255‐265. [DOI] [PubMed] [Google Scholar]
- 82. Brønnum‐Hansen H, Östergren O, Tarkiainen L, et al. Changes in life expectancy and lifespan variability by income quartiles in four Nordic countries: a study based on nationwide register data. BMJ Open. 2021;11(6):e048192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Permanyer I, Spijker J, Blanes A, Renteria E. Longevity and lifespan variation by educational attainment in Spain: 1960–2015. Demography. 2018;55(6):2045‐2070. [DOI] [PubMed] [Google Scholar]
- 84. Montez JK, Beckfield J, Cooney JK, et al. US state policies, politics, and life expectancy. Milbank Q. 2020;98(3):668‐699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Montez JK. Deregulation, devolution, and state preemption laws’ impact on US mortality trends. Am J Public Health. 2017;107(11):1749‐1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Riley AR, Collin D, Grumbach JM, Torres JM, Hamad R. Association of US state policy orientation with adverse birth outcomes: a longitudinal analysis. J Epidemiol Community Health. 2021;jech‐2020‐214858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Institute of Medicine and National Research Council . US Health in International Perspective: Shorter Lives, Poorer Health. Steven HW, Laudan A, eds. Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 88. Grumbach JM. Laboratories Against Democracy: How National Parties Transformed State Politics. Princeton, NJ: Princeton University Press; 2022. [Google Scholar]
- 89. Leive AA, Ruhm CJ. Education gradients in mortality trends by gender and race. J Human Capital. 2021;16(1):47‐72. [Google Scholar]
- 90. Bartle‐Haring S, Whiting R. Structural racism and the education gradient for early all‐cause mortality. SSM Popul Health. 2022;17:101076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Geronimus AT, Bound J, Waidmann TA, Rodriguez JM, Timpe B. Weathering, drugs, and whack‐a‐mole: fundamental and proximate causes of widening educational inequity in US life expectancy by sex and race, 1990–2015. J Health Soc Behav. 2019;60(2):222‐239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Ross CE, Masters RK, Hummer RA. Education and the gender gaps in health and mortality. Demography. 2012;49(4):1157‐1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Bambra C. Health inequalities and welfare state regimes: theoretical insights on a public health “puzzle.” J Epidemiol Community Health. 2011;65(9):740‐745. [DOI] [PubMed] [Google Scholar]
- 94. Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med. 2012;75(4):761‐769. [DOI] [PubMed] [Google Scholar]
- 95. Beckfield J, Bambra C, Eikemo T, et al. An institutional theory of welfare state effects on the distribution of population health. Soc Theory Health. 2015;13(3):227‐244. [Google Scholar]
- 96. Conti G, Heckman J, Urzua S. The education‐health gradient. Am Econ Rev. 2010;100(2):234‐238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Clark D, Royer H. The effect of education on adult mortality and health: evidence from Britain. Am Econ Rev. 2013;103(6):2087‐2120. [DOI] [PubMed] [Google Scholar]
- 98. Davies NM, Dickson M, Davey Smith G, van den Berg GJ, Windmeijer F. The causal effects of education on health outcomes in the UK Biobank. Nat Hum Behav. 2018;2(2):117‐125. [DOI] [PMC free article] [PubMed] [Google Scholar]


