Abstract
The mortality rate of non-communicable diseases (NCDs) contributes more in low-income and middle-income countries, also among individuals with lower socioeconomic status in high-income countries, making NCDs a big hurdle to minimizing global and national health disparities. Among 55 million fatalities worldwide in 2019, NCDs accounted for about 41 million (71%) deaths. The purpose of this scoping review was to comprehend the available literature on the burden of NCDs in India. This review included the studies that have been published between the period of 2009–2020. For this review, 18 full-text articles have been selected. A preliminary search was done to obtain articles from the search engines such as PubMed, Google Scholar, web of science, and Scopus. Our scoping review was focused on five major NCDs which are cardiovascular, hypertension, diabetes, cancer, and stroke. In 2019, around 17.9 million individuals died from cardiovascular disease (CVD), which is accounting for 32% of all deaths. As compared to Chandigarh and Jharkhand (0.12 million and 0.96 million, respectively) Tamil Nadu and Maharashtra (4.8 million and 9.2 million, respectively) have a higher percentage of the population affected by diabetes. In India, stroke is the fifth-significant cause of disability and the fourth-leading cause of fatality, which is accounting for 3.5 percent of all disabilities. India should construct a higher-level coordinating framework and devise an overarching policy or strategy tailored to NCDs. To limit risk factor exposure, it is necessary to emphasize health promotion and preventive actions.
Keywords: Burden, disability, policy
Introduction
Non-communicable diseases (NCDs) are a huge group of illnesses that comprise chronic respiratory illnesses (asthma, COPD), malignant growth, diabetes, and cardiovascular ailments (including stroke and respiratory failures). The mortality rate of NCDs is considerably higher in low-income and middle-income countries (LICs and MICs), which makes NCDs a tremendous barrier to reducing developing and developed nations' health disparities.[1] Overall, in the world, NCDs are the prime determinant of disability and mortality. Out of 55 million fatalities in the world in 2019, about 41 million (around 71%) were caused by NCDs.[2] Over 5.8 million Indians lose their lives each year to NCDs like diabetes, cancer, heart disease, and stroke (WHO report, 2015). In other words, one out of four Indians has the highest probability of dying from NCDs before reaching the age of 70 years.[2] Because of the harm, they do to the nation's socioeconomic development and even the human anguish they bring, NCDs are a significant public health problem in the twenty-first century.[3] Long-term development is in danger due to the global non-communicable disease pandemic. NCDs are also encompassed by Sustainable Development Goal (SDG) 3.4, which aims to reduce non-communicable disease-related premature death by one-third by 2030, as well as seeks to promote mental health and well-being through the use of prevention and treatment.[4] Furthermore, NCDs are addressed in three of the SDG's nine health targets. World Health Organization (WHO) presented a Global Strategy for the Prevention and Control of NCDs Action Plan at the World Health Assembly. Chronic diseases such as chronic respiratory disease, malignant growth, CDV, and cancer are the four diseases that account for more than 80% of all early NCD fatalities (According to World Health Organization 2021). Following the adoption of Resolution 66.10 of the World Health Assembly, India was the first country in the world to create its National NCD Monitoring Framework, which includes country-specific key performance indicators, and has pledged to achieve 10 goals and 21 bench markers by 2025. NCDs are perceived as ailments in which microbial interference is alienated in favor of lifestyle factors, and environmental genetical factors, with a few accompanied risk factor consequences, such as increased industrialization and urbanization, changes in lifestyle habits, and longer life expectancy, the prevalence of the non-communicable disease is predicted to be raised in the coming years.[5,6] Tobacco use and alcoholism, sedentary behavior, being overweight or obese, intake of fruits, and vegetables insufficient, having higher blood pressure (BP), blood glucose, and cholesterol levels, and consuming excessive fat and sodium, seem to be biological and behavioral risk factors that are contributing to the development of NCDs.[7] Non-communicable illnesses (NCDs) such as diabetes mellitus, hypertension, pulmonary (COPD/bronchial asthma), and heart disease have been known to enhance susceptibility to Covid-19 disease among individuals.[8] The Government of India has begun “Population-based screening of major NCDs” at the community and primary healthcare level to battle diabetes, hypertension, and the three most prevalent cancers—oral, breast, and cervical cancers.[9]
Study novelty
The included paper has been adequately verified and of them were evaluated guidelines. Scoping review method has been adapted to summarize the burden of NCDs. By the application of text and descriptive result extraction method, we overlooked all the possible previous research. Recent epidemiological data show that NCDs and multimorbidity were significantly prevalent and it is increasingly the norm for patients in high-income contexts. Even though there is literature on NCDs and their numerous risk factors, to alleviate the burden of NCDs, a comprehensive understanding of the disease burden is required, which will aid in the development of effective intervention strategies. Hence this scoping review aims to comprehend the available literature on the burden of NCDs.
Materials and Methods
A preliminary search of PubMed, Google Scholar, web of science, and Scopus revealed that there was no review on the current state of the NCD burden in India. A scoping review technique has been used to assess the magnitude of evidence in this area in India. This analysis adhered to a predetermined structure and set of guidelines. Systematic searches were carried out utilizing electronic information databases, namely, Google Scholar, Scopus, MEDLINE, Embase, Web of Science, and PsycINFO. These search libraries were used because they were most likely to focus on providing relevant and highly effective coverage of the subject, while also limiting the probability of missing publications. The search terms were decided upon collectively by the authors and were generated from keywords associated with the research objective. The studies that have been selected for this review were published between the period of 2009–2020. In each database, the following search string/MESH terms was used: Keywords: Non communicable disease [Title/Abstract] AND (“India” [MeSH Terms] OR “Cardiovascular” [Title/Abstract] OR “NCD's” [All Fields]) AND (“India” [MeSH Terms] OR “hypertension” [Title/Abstract] OR “comorbidity” [MeSH Terms] OR “morbidities” [All Fields]) AND (“Household” [Title/Abstract] OR “India” [All Fields] OR “community” [All Fields]) AND (“India” [MeSH Terms] AND “Diabetes” [Title/Abstract] OR “blood sugar” [MeSH Terms] OR “morbidities” [All Fields]) AND (“Household” [Title/Abstract] AND “Cancer” [Title/Abstract] OR “morbidities” [All Fields]) AND (“Stroke” [Title/Abstract] OR “India” [All Fields].
The inclusion criteria of studies were based on NCDs, Comorbidities, and NCDs. This review included the disease that is most prevalent in NCDs. The studies that are done among communities and the prevalence rate. Initial searches of electronic databases yielded only a few studies. Eligibility criteria were used to choose papers for inclusion in the review. The first choice was picked based on the title, then the abstract, and finally the whole content. The search for and application of inclusion criteria are in Figure 1. Exclusion criteria: Studies of mixed populations (e.g., Hypertension and depression) were excluded unless separate results for people with hypertension could be isolated. We excluded studies that are done on qualitative assessment, review articles, retrospective studies, randomized control trials, etc.,
Figure 1.
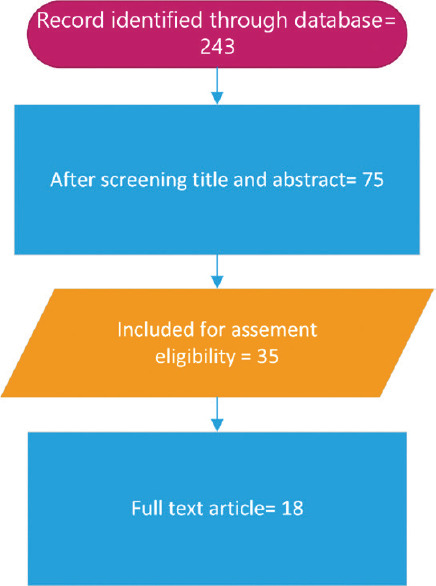
Flowchart (Using Visio software) for review items (Data source: Secondary data) Documenting NCDs in India: A Strategy for Finding articles
Results
Overall, 18 articles were screened for the final review process. These 18 articles concentrated majorly on five NCDs which accounted for the high disease burden. This review explains the burden of cardiovascular, hypertension, diabetes, cancer, and stroke. The burden of each non-communicable disease has been explained henceforth.
Non-communicable diseases
Cardiovascular
Currently, CVD has emerged as one of the most prominent and preferred fields globally. From Figure 2 all over the world, CVD is the foremost leading cause of death across the world, followed by other NCDs, namely, injuries, chronic respiratory diseases, cancer, and diabetes. In 2019, worldwide 17.9 million people died as a result of CVD, which is accounting for 32% of all deaths. In 2019, out of these 17 million premature fatalities (before reaching the age of 70) owing to NCDs, 85% of these deaths were caused by strokes and heart attacks, and 38% were related to CVD.[10] In India, the estimated annual number of deaths due to CVD is predicted to increase from 2.26 million (1990) to 4.77 million (2020).[11] In India, the mortality rate of CVD increased by 34% from 1990 to 2016.[12] A study by Dosi et al. revealed that the prevalence of coronary artery disease was 38% among postmenopausal women.[13] Across India, Punjab, Kerala, and Tamil Nadu are having the highest rate of CVD, besides that, these states also have the highest prevalence of high cholesterol and raised BP.[12] Evidence from LASI wave 1 shows that the overall self-reported prevalence of CVD was 29.4% among older adults who are aged 45 and above. The prevalence rate was increased among ages from 22% among 45–54 years to 38% among 70 years and above, and the study also shows that the prevalence of CVD is higher among women when compared with men and it is also higher among individuals who are residing in urban areas when compared to rural areas. The increasing trend of cardiovascular risk factors among Indians has been attributed to urbanization and higher living conditions. As can be seen from Table 1, there is a rise in the prevalence rate, death, disability-adjusted life year (DALY), years of life lost, and years lived with disabilities, as well as when compared to both gender prevalence and death are increased among males when compared to females. CVD is both extremely debilitating and proactive, with numerous external and internal factors influencing its exacerbation and improvement, and these characteristics also have an impact on patients quality of life and impose enormous costs on the healthcare systems of a country.[14] A significant portion of CVD conditions can be mitigated by addressing behavioral risk factors such as the usage of tobacco, alcohol abuse, inappropriate eating habit, obesity, and inadequate physical inactivity. CVD and their consequences are generally preventable, however, a lack of patient knowledge, attitude, and practice can be significant factors influencing the selection and adoption of health-promoting behavior to achieve a healthy lifestyle.[15] It is indeed extremely important to diagnose cardiovascular illness as soon as possible so that counseling and medication therapies can be started to treat the illness.
Figure 2.
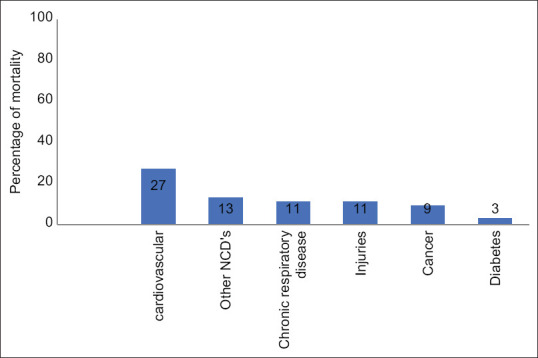
Percentage of NCDs mortality in India in 2016 (Source: WHO Non-communicable disease India profile 2018)
Table 1.
Prevalence of CVD in India 2009-2019
| Measure | Percent | Number | ||
|---|---|---|---|---|
|
|
|
|||
| 2009 | 2019 | 2009 | 2019 | |
| Death | ||||
| Male | 0.23386 | 0.28511 | 1124779 | 1427542 |
| Female | 0.20119 | 0.26113 | 773860 | 1146867 |
| YLLs (Years of Life Lost) | ||||
| Male | 0.15294 | 0.21281 | 30411969 | 35849607 |
| Female | 0.11616 | 0.18334 | 18873574 | 25680328 |
| DALYs (Disability- Adjusted Life Years) | ||||
| Male | 0.15574 | 0.12096 | 31563163 | 37466406 |
| Female | 0.12163 | 0.08604 | 20133820 | 27480063 |
| YLDs (Years Lived with Disability) | ||||
| Male | 0.01895 | 0.02241 | 1151194 | 1616798 |
| Female | 0.01758 | 0.02062 | 1260246 | 1799735 |
| Prevalence | ||||
| Male | 0.04399 | 0.05377 | 26631881 | 37084040 |
| Female | 0.04145 | 0.05096 | 24020119 | 34046289 |
Source: GHDx healthdata.org
Hypertension
In India as well as globally, hypertension has emerged to be the most important cause of death and disability. Heart failure, ischemic heart disease, chronic renal disease, and stroke are all linked to the development of hypertension. According to estimates, hypertension is attributed to 57% of strokes and 24% of coronary artery disease fatalities.[16,17] In 2017, according to the global burden of disease report, about 1.54 million deaths were because by hypertension in India and worldwide hypertension has caused 10.4 million fatalities; global hypertension has led to 220.0 million disability-adjusted life years, whereas in India it is 38.1 million disability-adjusted life. The global burden of hypertension climbed from 594 million people in 1975 to 1.13 billion in 2015. According to the recent report of the national family health survey-5 elevated BP (Systolic ≥140 mm of Hg and/or Diastolic ≥90 mm of Hg) or under medication for the control of hypertension was about 21.3% among women and 24.0% among men. In south Asian regions, hypertension is regarded as the third-most significant risk factor for the burden of disease.[15] The prevalence of hypertension was about 31.5% in urban areas and 26.2% in rural areas as shown in the ICMR INDIAB study. A study by Geevar, Zachariah, et al. conducted in Kerala among young adults aged 20–39 years shows that the prevalence of hypertension was about 11.2% and it also showed a prehypertension prevalence of 33.3%.[18] Evidence from the literature shows that the prevalence of hypertension in the urban areas in India is about 20% to 40% and 13% to 17% in rural areas. Due to a wide range of factors, hypertension is progressively very prevalent in both advanced countries and developing countries and is attributed to a sudden transition in lifestyle behaviors and patterns in developing countries like India, in addition, there is an increase in the older population due to a rise in life expectancy.[19] uncontrolled hypertension is a significant risk factor for CVD complications, which is accounting for 70% of the Asian-Pacific region's CVD burden.[20] Likewise, a higher BMI, alcohol consumption, poor eating habits, and a sedentary lifestyle are all key contributors to India's increased prevalence of hypertension. The potential for community-based preventative interventions that concentrate on both healthcare and lifestyle-related issues, such as medical counseling, suitable dietary habits, and cultural perceptions of healthy lives. To track the progress of interventions, high-prevalence districts from available national-level data should have universal BP screening. When it comes to interventions, the focus should be on hypertension prevention at primary levels and policy measures should be done to ameliorate the poor's hazardous working circumstances and the growing social constraints of survival responsible for “lifestyle” modifications like high-calorie eating and alcohol usage.
Diabetes
The threat that diabetes poses to both public health and socioeconomic development makes it one of the most severe public health crises in the world.[21] It is considered to be one of the leading causes of mortality.[22] Diabetes mellitus had long been seen to be a disease of the privileged, but current epidemiological evidence reveals that diabetes mellitus is becoming most significant among both urban India's middle and working classes and rural communities, By 2025, a globally agreed target is to halt the rise in diabetes and obesity. According to the International Diabetes Federation, in 2017 it is estimated that approximately 451 million adults worldwide have diabetes, and that number is anticipated to rise to 693 million by 2045 if effective prevention strategies are not adopted.[23] With more than 74 million people diagnosed with diabetes in India, the disease is quickly becoming an epidemic.[24] There are regional disparities in diabetes prevalence within India. The disparity across regions ranges from 3.85% to 21%.[14,25] According to baseline study findings of a huge community survey performed by the Indian Council of Medical Research (ICMR), which is a phase 1 survey from these survey the Northern Indian states of Chandigarh and Jharkhand are affected with 0.12 and 0.96 million populations affected with diabetes, which has a lower portion of the population affected by diabetes when compared with the southern Indian states of Tamil Nadu and Maharashtra (which accounts for 9.2 million and 4.8 million, respectively).[26,27] According to the National family health survey-5, the overall percentage of glucose levels—high or very high (>140 mg/dl) or under medication to control glucose levels was 13.5% among women and 15.6% among men. Because of these startling levels, the economic effect of diabetes mellitus throughout India is ranked among the highest in the world.[28] The outbreak of diabetes mellitus proportion has been increasing in India, with this rise the prevalence of diabetes is shifting from urban to rural areas, from wealthy to the less privileged, and from older persons to younger persons, and physical activities have decreased as a result of increased wealth, a less rigorous lifestyle and sophisticated facilities.[29] In comparison to HICs, metropolitan Indians have an unacceptably high risk of developing diabetes at any age and BMI.[30,31] Greater availability of the food like fast foods and junk foods adds fire to the fuel of diabetes.
Cancer
Cancer is a wide concept that would encircle a wide range of ailments that could impact any portion of the human body. A few other terminologies that are used to specify cancer were neoplasms and malignant tumors. Globally, cancer is the significant underlying cause of fatalities, by 2030 approximately 10 million mortalities were expected.[32] Even though there are several types of cancer that have been defined, colorectal, liver, stomach, lungs, gastric, esophagus, cervix, and breasts were the prime sites of cancer tumors in the human body in 2020.[32,33] Over 70% of cancer fatalities were accounted from LICs and MICs.[34] Use of tobacco, a high BMI, consumption of alcohol and drug usage, a lack of fruit and vegetable intake, and a lack of physical activity are accounted for almost one-third of cancer-related deaths.[33] With rising life expectancy and changes in lifestyles linked with economic growth, India's cancer burden is already high (about 1 million new cases in 2012) and is predicted to rise even more.[35] The number of individuals living with the disease is estimated to be over 2.25 million. In India, there have been 7,84,821 cancer-related deaths.[36,37] From 1990 to 2016, India's cancer mortality rate more than doubled.[38] Cancer's estimated burden is enormous, and it has been steadily rising at an alarming frequency of 93.0% among men in India.[39] According to the ICMR, Indians who are suffering from cancer is projected to increase from 26.7 million in 2021 to 29.8 million in 2025 and it also shows the seven cancers which are accounted for more than 40% of the total disease burden, the report indicated the percentage of different cancer rate, lung (10.6%), breast (10.5%), esophagus (5.8%), mouth (5.7%), stomach (5.2%), liver (4.6%), and cervix (4.3%). In India, one woman dies of cervical cancer every 8 min, one woman dies from breast cancer for every two newly diagnosed women and the death rate from tobacco usage is estimated to be around 3500 people per day.[32] According to the population-based cancer registry of 2012–2014, Delhi (19746), Thiruvananthapuram district (15640), Mumbai (13357), Chennai (11659), and Kollam (11012) were the top five PBCRs with the most cases.[40] Treatment for pediatric cancers is still minimal, and overall survival in India is lower than in more developed nations.[41] At the time of diagnosis, over 75–80% of individuals had advanced disease (Stage 3–4).[40,42] In various parts of the country, a lifestyle shift has occurred that is reflecting a rising incidence of various associated cancers such as prostate, breast, colon-rectum, and corpus-uteri. The most concerning factor in India is, that there is rising in the critical risk factors which are contributing to the development of various malignant tumors, the factors such as obesity or overweight, physically inactive, and consumption of alcohol.[37]
Stroke
In countries all over the world, stroke is a primary cause of disability and mortality, over 13 million new cases per year have been registered and post-stroke treatment, it had significant financial implications.[43,44] According to GBD, global burden of disease, injuries, and risk factors study 2017, as estimated by DALYs stroke was the third-most prominent reason for disability and mortality, and it is the second most prime factor of mortality around the world. Stroke is the fourth foremost cause of fatalities and in addition, stroke is the fifth contributing factor of morbidity, which is accounting for 3.5% of DALY.[45] According to the study evidence, in India, the incidence rate of stroke ranges from 116 to 163 per 100,000 people. A stroke is a life-altering event that impacts not only the disabled individual but also their family and careers.[46] Rural India has a greater rate of stroke-related mortality than urban India. Stroke claimed the lives of an estimated 375,000 Indians aged 30 to 69 years old in 2015. About 66 percent of the population resides in the rural areas of India, among those rural inhabitants, about 71% of stroke deaths have occurred, which is indicating disproportionately high numbers of moralities.[47] The prevalence rate ranged between 44.54 and 150 per 100,000.[48] Studies that included people of all ages showed that the stroke prevalence rates in urban regions ranged from 45 to 487 per 100,000 people, according to research that included people of all ages. Stroke prevalence rates in urban regions ranged from 45 to 487 per 100,000 people.[49,50] The prevalence rates of stroke in rural India were found in studies that included people of all ages, and the rates ranged from 55 to 388.4 per 100,000 people,[49] In terms of DALYs, gradual changes in demography, economy, and lifestyle have pushed the disease from 12th place in 1990 to 5th place in 2016.[51] India's solution to the uphill task offered by NCDs was the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS), which was established in the year 2010, Health promotion, referral, screening, and treatment for early diagnosis are all included in the program.[52]
Discussion
The paper reviews the magnitude of NCDs in a detailed way. The global epidemic of NCDs offers a challenge to all countries' health systems, while the challenges differ. The burden of disease in India has changed through the years, with a relatively big decline in communicable diseases and an increase in non-communicable disorders (NCDs). To control the rising magnitude of NCDs in LICs and MICs, proper monitoring systems must be established, and the data gathered must be used to enhance or implement control plans, although NCDs are complicated diseases, the majority of them may be controlled.[53] In addition, the majority of the efforts are focused on discovering cures. NCDs are the primary cause of disability, illness, and mortality, and across the countries, the prevalence rate is anticipated to rise unless interventions are implemented on a wide range.[54] A high level of coordinating framework and devising an overarching policy or strategy tailored to NCDs should be constructed in India. Non-health sectors such as agronomics, regional development, education, and trade have underlying indicators of NCDs. To build an enabling environment that supports healthy lifestyles, cross-sectoral coordination is required. To limit risk factor exposure, it is necessary to emphasize health promotion and preventive actions. The National Multisectoral Action Plan for the Prevention and Control of Common NCDs (2017–2022) is the nationwide conceptual model which will guide the nation's initiatives to deal with the rising magnitude of NCDs in the aspect of the country's healthcare systems, cultural and socioeconomic status. The lack of reliable NCD surveillance and research data is a major impediment to effective NCD prevention and control planning and implementation. It is necessary to build a robust surveillance system capable of providing precise and timely facts on NCD problems, quality of healthcare, and healthcare costs. Because of their limited scope of implementation, currently deployed NCD programs have not been able to alleviate the burden.
Conclusion
The government should consider strategic investments and efforts to prevent and regulate NCDs and their risk factors, and also concrete actions at the individual and community levels, primary prevention through screening and enhanced diagnostic facilities, improved management capacities, and universal access to health services. Integrated management, a solid surveillance system, and a public awareness campaign are required for the program to be successful and for services to be extensively available across the country.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Ms. Dhasarathi for her useful feedback and review. We would like to thank the dean and faculty of SRM school of public health for their support
References
- 1.Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, et al. NCD Countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392:1072–88. doi: 10.1016/S0140-6736(18)31992-5. [DOI] [PubMed] [Google Scholar]
- 2.WHO non-communicable Key facts. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicablediseases .
- 3.NDP India, Healthy living>Non-communicable disease. Available from: Non-communicable Diseases | National Health Portal Of India (nhp.gov.in)
- 4.UN Sustainable goals. Available from: Health – United Nations Sustainable Development.
- 5.Reddy KS, Shah B, Varghese C, Ramadoss A. Responding to the threat of chronic diseases in India. Lancet. 2005;366:1744–9. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 6.Gupta I, Roy A. Economic studies on non-communicable diseases and injuries in India: A systematic review. Appl Health Econ Health Policy. 2018;16:303–15. doi: 10.1007/s40258-018-0370-1. [DOI] [PubMed] [Google Scholar]
- 7.Sarveswaran G, Kulothungan V, Mathur P. Clustering of noncommun icable disease risk factors among adults (18–69 years) in rural population, South-India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;Sep 1;14(5):1005–14. doi: 10.1016/j.dsx.2020.05.042. [DOI] [PubMed] [Google Scholar]
- 8.Geetha K, Kanniammal C, Kumar D. Prevalence of hypertension among economically productive tribal population in Tamilnadu. Indian J Public Health Res Dev. 2020;11:553–6. [Google Scholar]
- 9.INDIA: Grassroots screening to prevent and control non-communicable diseases: (WHO 2021) Available from: INDIA: Grassroots screening to prevent and control non-communicable diseases (WHO)
- 10.WHO Cardiovascular disease. Available from: Cardiovascular diseases (CVDs) (WHO)
- 11.Huffman MD, Prabhakaran D, Osmond C, Fall CH, Tandon N, Lakshmy R, et al. Incidence of cardiovascular risk factors in an Indian urban cohort: Results from the New Delhi Birth Cohort. J Am Coll Cardiol. 2011;57:1765–74. doi: 10.1016/j.jacc.2010.09.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vasan SK, Antonisamy B, Gowri MS, Selliah HY, Geethanjali FS, Jebasingh F, et al. Burden of cardiovascular disease risk factors over 13.5 years in a rural and urban South Indian cohort in comparison with global data. medRxiv. 2020 doi: 10.1136/bmjdrc-2020-001782. doi: 10.1101/2020.07.03.20145599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dosi R, Bhatt N, Shah P, Patell R. Cardiovascular disease and menopause. Journal of clinical and diagnostic research: JCDR. 2014;Feb; 8(2):62. doi: 10.7860/JCDR/2014/6457.4009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shakibazadeh E, Sabouri M, Mohebbi B, Tol A, Yaseri M. Validity and reliability properties of the Persian version of perceived health competence scale among patients with cardiovascular diseases. J Educ Health Promot. 2021;10:19. doi: 10.4103/jehp.jehp_899_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohebbi B, Sabouri M, Tol A. Application of health education and promotion theory-based interventions on patients with cardiovascular disease: A systematic review. J Educ Health Promot. 2021;10:236. doi: 10.4103/jehp.jehp_173_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramakrishnan S, Zachariah G, Gupta K, Rao JS, Mohanan PP, Venugopal K, et al. Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019;71:309–13. doi: 10.1016/j.ihj.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;31(383):1899–911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zachariah G, Harikrishnan S, Krishnan MN, Mohanan PP, Sanjay G, Venugopal K, Thankappan KR. Prevalence of coronary artery disease and coronary risk factors in Kerala, South India: a population survey–design and methods. indian heart journal. 2013;May1;65(3):243–9. doi: 10.1016/j.ihj.2013.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pooja P, Mittal Y. Prevalence of hypertension among rural population of Doiwala block, Dehradun, Uttarakhand India. Recent Res Sci Technol. 2013:5. [Google Scholar]
- 20.Mohebbi B, Tafaghodi B, Sadeghi R, Tol A, Yekanenejad MS. Factors predicting nutritional knowledge, illness perceptions, and dietary adherence among hypertensive middle-aged women: Application of transtheoretical model. J Educ Health Promot. 2021;10:212. doi: 10.4103/jehp.jehp_1434_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin X, Xu Y, Pan X, Xu J, Ding Y, Sun X, et al. Global, regional, and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Sci Rep. 2020;10:14790. doi: 10.1038/s41598-020-71908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO Diabetes. Available from: https://www.who.int/health-topics/diabetes#tab=tab_1 .
- 23.Cho N, Shaw JE, Karuranga S, Huang YD, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 24.International Diabetes Federation (IDF) IDF diabetes atlas eighth edition 2017. [Last accessed on 2021 Dec 21]. Available from: https://www.idf.org/e-library/epidemiology-research/diabetes-atlas/134-idfdiabetes-atlas-8th-edition.html .
- 25.Chauhan S, Gupte SS, Kumar S, Patel R. Urban-rural differential in diabetes and hypertension among elderly in India: A study of prevalence, factors, and treatment-seeking. Diabetes Metab Syndr. 2021;15:102201. doi: 10.1016/j.dsx.2021.102201. [DOI] [PubMed] [Google Scholar]
- 26.Kaveeshwar S, Cornwall J. The current state of diabetes management. Australas Med J. 2014;7:45–8. doi: 10.4066/AMJ.2013.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anjana RM, Ali MK, Pradeepa R, Deepa M, Datta M, Unnikrishnan R, et al. The need for obtaining accurate nationwide estimates of diabetes prevalence in India-rationale for a national study on diabetes. Indian J Med Res. 2011;133:369–80. [PMC free article] [PubMed] [Google Scholar]
- 28.Joshi SR. Diabetes care in India. Ann Glob Health. 2015;81:830–8. doi: 10.1016/j.aogh.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 29.Kaur J, Singh Z. Occurrence of diabetes among rural women. J Dis. 2020;7:33–8. [Google Scholar]
- 30.Luhar S, Kondal D, Jones R, Anjana RM, Patel SA, Kinra S, et al. Lifetime risk of diabetes in metropolitan cities in India. Diabetologia. 2021;64:521–9. doi: 10.1007/s00125-020-05330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desa UN. Revision of world urbanization prospects. UN Department of Economic and Social Affairs. 2018:16. [Google Scholar]
- 32.Schottenfeld D, Beebe-Dimmer JL. Advances in cancer epidemiology: Understanding causal mechanisms and the evidence for implementing interventions. Annu Rev Public Health. 2005;26:37–60. doi: 10.1146/annurev.publhealth.26.021304.144402. [DOI] [PubMed] [Google Scholar]
- 33.Rajpal S, Kumar A, Joe W. Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014. PLoS One. 2018;13:e0193320. doi: 10.1371/journal.pone.0193320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO, Cancer. [Last accessed on 2021 Oct 23]. Available from: Cancer (who.int)
- 35.India fight against cancer, NICPR-ICMR. [Last accessed on 2021 Oct 23]. Available from: India Against Cancer-Cancer Detection, Cancer Prevention and Cancer Treatment in India (cancerindia.org.in)
- 36.India fight against cancer, NICPR-ICMR. [Last accessed on 2021 Oct 23]. Available from: Cancer Statistics-India Against Cancer (cancerindia.org.in)
- 37.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 38.Smith RD, Mallath MK. History of the growing burden of cancer in India: From antiquity to the 21st century. J Glob Oncol. 2019;5:1–5. doi: 10.1200/JGO.19.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mathew A, George PS, KM JK, Vasudevan D, James FV. Transition of cancer in populations in India. Cancer Epidemiol. 2019;58:111–20. doi: 10.1016/j.canep.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 40.NCRP. Three-Year Report of the Population Based Cancer Registries 2012–2014. [Last accessed on 2021 Oct 25]. Available from: Three Year Report of PBCR 2012-2014 (ncdirindia.org)
- 41.Mallath MK, Taylor DG, Badwe RA, Rath GK, Shanta V, Pramesh CS, et al. The growing burden of cancer in India: Epidemiology and social context. Lancet Oncol. 2014;15:e205–12. doi: 10.1016/S1470-2045(14)70115-9. [DOI] [PubMed] [Google Scholar]
- 42.Singh M, Prasad CP, Singh TD, Kumar L. Cancer research in India: Challenges & opportunities. Indian J Med Res. 2018;148:362–5. doi: 10.4103/ijmr.IJMR_1711_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lindsay MP, Norrving B, Sacco RL, Brainin M, Hacke W, Martins S, et al. World Stroke Organization (WSO): Global stroke fact sheet 2019. Int J Stroke. 2022;17:18–29. doi: 10.1177/17474930211065917. [DOI] [PubMed] [Google Scholar]
- 44.Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459–80. doi: 10.1016/S1474-4422(18)30499-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Directorate General of Health Services: Ministry of Health and Family Welfare. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Disease and Stroke. Government of India 2019. [Last accessed on 2021 Oct 28]. Available from: National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS) | Ministry of Health and Family Welfare | GOI (mohfw.gov.in)
- 46.Taylor FC, Suresh Kumar K. Stroke in India Factsheet (updated 2012). South Asia Network for Chronic Disease, IIPH Hyderabad, Public Health Foundation of India. 2012 [Google Scholar]
- 47.Ke C, Gupta R, Xavier D, Prabhakaran D, Mathur P, Kalkonde YV, et al. Divergent trends in ischaemic heart disease and stroke mortality in India from 2000 to 2015: A nationally representative mortality study. Lancet Glob Health. 2018;6:e914–23. doi: 10.1016/S2214-109X(18)30242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhamija RK, Mittal S, Bansal BC. Trends in clinico-epidemiological correlates of stroke in the community. J Indian Acad Clin Med. 2000;5:28–31. [Google Scholar]
- 49.Gourie-Devi M. Neuroepidemiological study in semiurban and rural areas in South India: Pattern of neurological disorders including motor neuron disease. Motor Neuron Disease: Global clinical patterns and international research. 1987:11–21. [Google Scholar]
- 50.Das SK, Biswas A, Roy T, Banerjee TK, Mukherjee CS, Raut DK, et al. A random sample survey for prevalence of major neurological disorders in Kolkata. Indian J Med Res. 2006;124:163–72. [PubMed] [Google Scholar]
- 51.Roy MP. Factors associated with stroke mortality in India. Curr Med Issues. 2020;18:179. [Google Scholar]
- 52.Government of India. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke– Operational Guidelines (Revised- 2013-2017). New Delhi; 2013 [Google Scholar]
- 53.Nethan S, Sinha D, Mehrotra R. Non communicable disease risk factors and their trends in India. Asian Pac J Cancer Prev. 2017;18:2005–10. doi: 10.22034/APJCP.2017.18.7.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharma K. Burden of non communicable diseases in India: Setting priority for action. Int J Med Sci Public Health. 2013;2:7–11. [Google Scholar]


