Abstract
A nasal septal abscess is a rare lesion that usually results from a nasal septal hematoma after nasal trauma or surgery, although it can occur unexpectedly. Nasal septal abscesses should be prevented and treated immediately. The authors describe 2 unusual cases: 1 caused by sudden loosening of the quilting suture of the nasal septum and the other by a nasopharyngeal swab test for coronavirus disease-2019. The authors also provide an intraoperative video and a literature review.
Key Words: COVID-19, nasal septal abscess, nasopharyngeal swab, quilting suture
Since December 2019, the world has been confronted by the spread of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which causes coronavirus disease-2019 (COVID-19).1 Severe acute respiratory syndrome coronavirus-2 is usually transmitted through droplets and the clinical manifestations of COVID-19 vary from mild upper airway infection to severe pneumonia requiring intensive care unit management.2–4 Although many complications of COVID-19 disease have been reported, few reports have focused on complications related to the COVID-19 test.
Nasal septal abscess refers to pus formation inside the submucoperiosteal or submucoperichondrial space of the nasal septum.5 The most common cause of nasal septal abscesses is nasal trauma caused by accidents or nasal surgery.6 Although cases of nasal septum abscess after nasal trauma or nasal surgery have been reported, no cases have been reported of a septal abscess caused by unintentional nasal stimulation, especially in patients who underwent septoplasty several weeks before. The authors treated 2 patients with a septal abscess caused by traumatic stimulation after septoplasty. In the first patient, who had uncontrolled diabetes mellitus, a septal abscess developed after the suture thread in the septum broke suddenly. In the second patient, a septal abscess developed immediately after a nasopharyngeal swab test for COVID-19. We report these rare cases and provide an intraoperative video and literature review.
CASE REPORTS
Case 1
A 55-year-old man who had type 2 diabetes visited our hospital with yellowish rhinorrhea that had persisted for a few years. Nasal endoscopy and brain computed tomography (CT) showed the nasal septum deviated to the left and sinusitis in the left maxillary and ethmoid sinuses. At that time, the fasting blood glucose and HbA1c levels were 227 mg/dL and 8.4% respectively, indicating that his diabetes was not well controlled. Under suspicion of chronic sinusitis, left middle meatal antrostomy, left ethmoidectomy, and septoplasty was performed under general anesthesia. During septoplasty, an incision on the left side was made, and to reduce the dead space, through-and-through quilting mattress sutures were applied in the septum using polydioxanone 4-0 followed by nasal packing.
Subsequent nasal endoscopy revealed that the surgical site was healing well. However, about 7 weeks after the operation, the patient experienced nasal pain and a sudden feeling of loosening of the stitches in the surgical site, and he noticed that a fragment of thread had fallen from his nose. On physical examination, the thread was observed to have been cut in the area where the quilting mattress sutures had been applied, and the left anterior nasal septum seemed to be slightly swollen. All of the remaining stitches were removed, and aspiration of the swollen area was attempted with a syringe, but no discharge was drained.
Oral antibiotics were administered for 2 weeks, but the swelling worsened. An incision was made at the previous incision site in the nasal septum under local anesthesia. An abscess was found inside the submucoperichondrial space, and about 1 mL of pus was drained. The inside of the nasal septum was washed several times with gentamicin and normal saline, and nasal packing was performed. The swelling disappeared immediately after this procedure, and antibiotics were administered daily.
One week later, nasal endoscopy and contrast-enhanced CT of the face (Fig. 1) showed that the septal abscess reappeared at the same place. Incision and drainage were performed again under local anesthesia (Video, Supplemental Digital Content 1, http://links.lww.com/SCS/E633). An incision was made at the previous incision site and a large amount of granulation and necrotic tissue was observed inside the nasal septum and was removed through curettage. After several washes with normal saline, an additional incision was made in the left septal mucosa horizontally to facilitate drainage, and nasal packing was performed. Antibiotics were prescribed for another week. Since then, the septal abscess has not recurred, and the surgical site has healed well.
FIGURE 1.
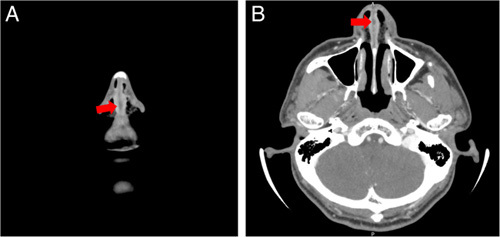
Contrast-enhanced computed tomography (CT) of the face showed a tiny low-density lesion with rim enhancement inside the nasal septum (red arrows).
Case 2
A 69-year-old woman visited our hospital with a 2-year history of nonproductive cough and nasal stuffiness. She had hypertension but no other conditions. On physical examination and paranasal sinus CT, the nasal septum deviated to the left, and sinusitis in the left maxillary sinus was seen. Therefore, septoplasty, left middle meatal antrostomy, and left anterior ethmoidectomy were performed under general anesthesia. A small incision was made in the left septal mucosa where a bony spur was located, and the spur was removed. The surgical site seemed to be healing well.
About 7 weeks after the surgery, left nasal pain occurred immediately after the patient underwent a nasopharyngeal swab test for COVID-19, and this pain lasted a few days. Nasal endoscopy showed no specific findings other than a mild reddish change in the left anterior septal mucosa. Medical treatment included antibiotics for 2 weeks. Despite the treatment, the pain worsened and was accompanied by left nasal obstruction, and bulging of the anterior nasal septum developed on the left side. Contrast-enhanced CT of the face revealed a low-density lesion measuring 19 mm×14 mm with rim enhancement inside the anterior nasal septum (Fig. 2). Incision and drainage were performed in the left anterior septal mucosa, and about 5 mL of purulent discharge were drained, and packing was performed. The patient was hospitalized to receive intravenous antibiotics. After discharge, the nasal septal mucosa remained intact without recurrence of the abscess.
FIGURE 2.
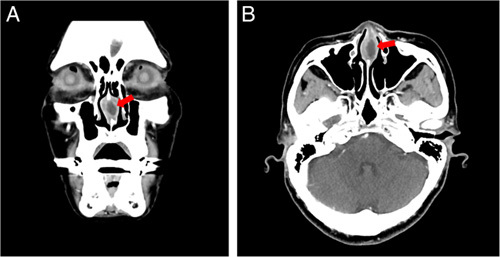
Coronal (A) and axial (B) views of the contrast-enhanced CT of the face revealed a low-density lesion measuring 19 mm×14 mm with rim enhancement inside the anterior nasal septum (red arrows).
DISCUSSION
The most common cause of a nasal septal abscess is a nasal septal hematoma resulting from nasal trauma, such as an accident or surgery. After the blood vessels of the nasal septum are damaged by trauma, blood accumulates in the medial space of the septal perichondrium. This can lead to the formation of a septal hematoma and detachment of septal cartilage from the perichondrium. Insufficient blood supply to the septal cartilage can lead to ischemic necrosis, which increases susceptibility to infection and can lead eventually to the formation of a septal abscess.7 When a septal abscess occurs, it is important to perform an incision to allow drainage and administer antibiotics without delay to prevent permanent cartilaginous deformities or fatal complications.5 A septal abscess not treated properly can lead to saddle-nose deformity, intracranial complications such as meningitis or cavernous sinus thrombosis, and sepsis.6 Therefore, it is important to prevent the occurrence of a nasal septal abscess and to manage it immediately if a septal abscess does occur.
There seem to be several possible causes for the formation of septal abscesses in our patients. In both patients, the abscess occurred only a few weeks after septoplasty, when the nasal septum would have been vulnerable to damage or infection because the surgical site was not fully healed. In the first patient, uncontrolled diabetes may have slowed wound healing and promoted infection. Luan et al8 reported that among patients who underwent septoplasty, the risk of developing a nasal septal abscess was 2.6 times higher in diabetic patients than in nondiabetic patients. Among patients with diabetes, septal abscess occurs at a higher rate in patients with more severe than in those with less severe disease.8 These findings suggest that diabetes can increase the risk of developing a septal abscess after septoplasty and that the severity of diabetes may affect the susceptibility. Strict glucose control is therefore required before and after surgery for patients with diabetes.8 Surgical site injuries should be avoided in patients who have recently undergone septoplasty because the wound may require at least several weeks to heal fully.
To prevent a nasal septal abscess, proper suturing techniques of the septum during septoplasty can be also useful. Transseptal suturing is often used during septoplasty to reduce dead space and stabilize the nasal septum.9 This procedure is as effective as nasal packing for the prevention of postoperative bleeding or hematoma and can be used instead of nasal packing, which should prevent the pain or anxiety caused by the removal of the packing material.9 Suturing that is too tight may cause septal necrosis, whereas suturing with an adequate distance between stitches can significantly reduce the risk of local infection.10 In the first patient with uncontrolled diabetes in our study, the suture loosened and this exposed the cut thread within the nasal mucosa. We postulate that this acted as a traumatic stimulus or became the source of infection in the damaged septal mucosa after septoplasty. This case suggests that it is important to maintain proper tension and distance between the stitches during transseptal suturing to avoid interfering with the blood supply or wound healing in the nasal septum.
In the second patient, the nasal symptoms started immediately after the nasopharyngeal swab was performed for COVID-19 testing. To date, there has been only 1 reported case in the literature of a septal abscess after a nasopharyngeal swab test.11 The patient in that study had diabetes mellitus and neutropenia, and developed a septal abscess after a COVID-19 nasopharyngeal swab test that required incision and drainage.11 In both the patient in our study and the previous study, the nasal septum may have been accidentally injured during the insertion of the cotton swab into the nasopharynx. In our second patient, the painful swab test caused injury to the fragile septal mucosa after septoplasty, and this traumatic injury to the delicate septal mucosa seemed to have caused the septal abscess.
Nasopharyngeal swabs have been used on a huge number of people since December 2019, when the COVID-19 pandemic began to spread around the world. Various complications, such as epistaxis, have been reported to occur after the COVID-19 nasopharyngeal swab test.11 For patients who have recently undergone nasal surgery such as septoplasty, rhinoplasty, or sinus surgery, unnecessary nasopharyngeal swabs should be avoided to protect the surgical sites. If the swab test is unavoidable during the postoperative period, care must be taken not to irritate the surgical site. Even in patients without a history of nasal surgery, attention should be paid to the possibility of anatomical variations such as nasal polyps or nasal septal deviation. Observing the nasal structure through a nasal speculum or nasal endoscopy before the swab and adequate training in sampling procedures to avoid injuring the nasal structure may help to reduce the risk of complications caused by the COVID-19 nasopharyngeal swab test.11 In addition, less invasive and safer testing methods are needed to reduce the risk of complications related to COVID-19 testing, along with further research on effective responses to the COVID-19 pandemic.1–4,11
CONCLUSION
A nasal septal abscess is a rare condition, but it can occur unexpectedly. Patients with a history of recent nose surgery should be careful to avoid exposing the surgical site to trauma or infection. Risk factors such as diabetes should be controlled as much as possible before and after surgery. Proper use of transseptal suturing techniques during nasal septal surgery can help prevent septal abscesses. It is also important to be careful not to injure the intranasal structures during the nasopharyngeal swab test for COVID-19. When a nasal septal abscess occurs, prompt treatment is required to prevent further complications.
Supplementary Material
Footnotes
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.jcraniofacialsurgery.com.
Contributor Information
Yeon Hee Im, Email: younheeim@naver.com.
Dong-Hyun Kim, Email: monolithkim@catholic.ac.kr.
Il Hwan Lee, Email: ilhwanloves@hanmail.net.
REFERENCES
- 1. Hosseini ES, Kashani NR, Nikzad H, et al. The novel coronavirus disease-2019 (COVID-19): mechanism of action, detection and recent therapeutic strategies. Virology 2020;551:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salzberger B, Buder F, Lampl B, et al. Epidemiology of SARS-CoV-2. Infection 2021;49:233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cavallo L, Marcianò A, Cicciù M, et al. 3D printing beyond dentistry during COVID 19 epidemic: a technical note for producing connectors to breathing devices. Prosthesis 2020;2:46–52 [Google Scholar]
- 4. Cervino G, Fiorillo L, Surace G, et al. SARS-CoV-2 persistence: data summary up to Q2 2020. Data 2020;5:81 [Google Scholar]
- 5. Cheng LH, Wu PC, Shih CP, et al. Nasal septal abscess: a 10-year retrospective study. Eur Arch Otorhinolaryngol 2019;276:417–420 [DOI] [PubMed] [Google Scholar]
- 6. Hyo Y, Fukushima H, Harada T, et al. Nasal septal abscess caused by anaerobic bacteria of oral flora. Auris Nasus Larynx 2019;46:147–150 [DOI] [PubMed] [Google Scholar]
- 7. Ambrus PS, Eavey RD, Baker AS, et al. Management of nasal septal abscess. Laryngoscope 1981;91:575–582 [DOI] [PubMed] [Google Scholar]
- 8. Luan CW, Tsai MS, Liu CY, et al. Increased risk of nasal septal abscess after septoplasty in patients with type 2 diabetes mellitus. Laryngoscope 2021;131:E2420–E2425 [DOI] [PubMed] [Google Scholar]
- 9. Wang WW, Dong BC. Comparison on effectiveness of trans-septal suturing versus nasal packing after septoplasty: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 2017;274:3915–3925 [DOI] [PubMed] [Google Scholar]
- 10. Rettinger G, Kirsche H. Complications in septoplasty. Facial plast surg 2006;22:289–297 [DOI] [PubMed] [Google Scholar]
- 11. Fabbris C, Cestaro W, Menegaldo A, et al. Is oro/nasopharyngeal swab for SARS-CoV-2 detection a safe procedure? Complications observed among a case series of 4876 consecutive swabs. Am J Otolaryngol 2021;42:102758 [DOI] [PMC free article] [PubMed] [Google Scholar]


