Abstract
恶性颈动脉体瘤非常罕见,本研究报告1例颈动脉体瘤全切术后16年发生颈部淋巴结转移的病例。该病例为1例老年男性,68岁,发现左颈部无痛性肿物半年,既往16年前行颈动脉体瘤切除及左颈动脉人工血管重建术,查体可触及颈部左侧胸锁乳突肌后方多个肿物,质硬无压痛,界限不清。血常规及生化等血化验检查未见异常,颈部MRI强化显示左胸锁乳突肌后方多个圆形异常信号,强化明显。本病例的颈部包块经过再次手术切除,术后病理证实为颈动脉体瘤颈部淋巴结转移。故诊断为恶性颈动脉体瘤伴颈部淋巴结转移。术后PET-CT检查可见肺门、纵隔、腹主动脉旁多发淋巴结肿大,代谢异常,考虑恶性颈动脉体瘤全身多发转移。提示术前可行全身PET-CT检查用以评估肿瘤有无全身转移。
Keywords: 颈动脉体瘤, 淋巴结, 转移
Abstract
Malignant carotid body tumor is rare, reported this case who had experienced the totally resection of carotid body tumor 16 years ago and presented with cervical tumor now. The patient was a 68 year old male who presented with a low growing left-sided painless neck mass for half a year. Carotid body tumor resection and left carotid artery artificial vascular reconstruction were performed 16 years ago. Physical examination showed that multiple hard and painless masses can be touched behind the left sternocleidomastoid muscle of the neck. Blood routine and biochemical tests were normal. MRI enhancement of the neck showed multiple circular abnormal signals behind the left sternocleidomastoid muscle, with obvious enhancement. The cervical masses of this case were experienced totally resected again, and the postoperative pathology confirmed that it was carotid body tumor and cervical lymph node metastasis. The clinical diagnosis was malignant carotid body tumor with cervical lymph node metastasis. Postoperative PET-CT examination showed multiple lymphadenopathy and abnormal metabolism in hilar, mediastinum and abdominal aorta. Multiple systemic metastasis of malignant carotid body tumor was considered. It was suggested that preoperative whole-body PET-CT examination can be used to evaluate whether the tumor has systemic metastasis.
Keywords: carotid body tumor, lymph gland, metastasis
1. 病例报告
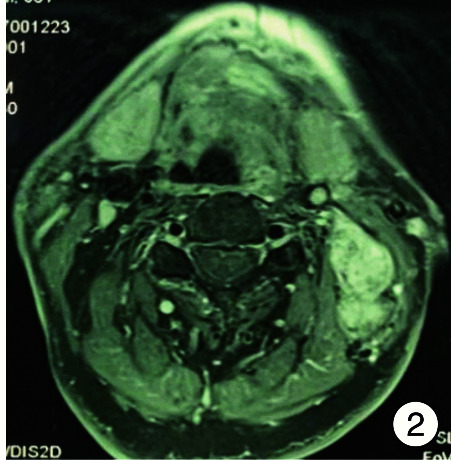
患者,男,68岁,主因“发现左颈部肿物半年”于2020年8月7日入院。患者半年前无明显诱因发现左下颌角后下方皮下肿物,无明显触痛,生长缓慢,无声嘶、涕中带血及咽异物感。16年前行左颈动脉体瘤切除术和左侧颈动脉人工血管重建术。高血压、高脂血症及脑梗死病史16年。入院后纤维鼻咽喉镜检查见鼻咽部对称、黏膜光滑,左侧声带旁中位固定,喉室结构正常,未见新生物。颈动脉超声示左侧颈总动脉近-中段闭塞(血栓形成),左侧颈总动脉中段至球部人造搭桥术后闭塞(血栓形成)。颈部MRI强化显示左侧颈部胸锁乳突肌内后方可见多个类圆形异常信号,边界清,较大直径约2.4 cm,T1稍高混杂信号,T2高信号,强化明显(图 1、2)。甲状腺、腮腺、颌下腺信号未见异常,颈部显示多个淋巴结。入院后完善术前检查,于2020年8月10日全身麻醉下行颈部肿物切除术,术中见最大肿物为肿大淋巴结,位于颈部Ⅱ区,直径3 cm,质地硬韧,与周围组织粘连,周围组织瘢痕化,并可见多发淋巴结肿大位于颈部Ⅲ区。术中探查左侧人工血管无搏动,颈内静脉与瘤体融合,术中冷冻病理结果示淋巴结转移瘤。遂按区域性颈清扫范围彻底切除病变,手术顺利,出血量为100 mL。术后PET-CT示左侧肺门占位,葡萄糖代谢增高,考虑恶性病变。左侧锁骨上、两肺门区、纵隔内及腹主动脉旁多发淋巴结肿大,代谢增高,考虑转移可能。左颈部有代谢增高影,内部伴气体影,考虑术后改变。术后病理示左颈部Ⅱ区病变融合淋巴结内肿瘤细胞呈器官样及结节状生长,肿瘤细胞核大深染,具有异型性,多个脉管内可见肿瘤细胞团,符合颈动脉体瘤淋巴结转移。颈部Ⅲ区淋巴结可见肿瘤转移。
图 1.
颈部MRI强化(冠状位)
示左侧下颌角下后方多个串状淋巴结肿大,强化明显

图 2.
颈部MRI强化(轴位)
示颈部左侧多个淋巴结肿大,强化明显,后方界限不清
2. 讨论
颈动脉体瘤是位于颈动脉分叉处的副神经节瘤,发病率低,约占头颈部肿瘤的0.6%[1],占头颈部副神经节瘤的60%~70%,发病原因可能与遗传因素、慢性缺氧有关,缺氧导致颈动脉体增生肥大,最终促使颈动脉体瘤发生[2-4]。其恶变率为4%~10%。一般发生淋巴结转移或远处转移被认为发生恶变。治疗方法主要是手术切除[5],根据瘤体与颈动脉的关系考虑是否行血管重建。
本例患者于16年前因“反复头晕伴意识障碍、脑梗死”,查出颈动脉体瘤,遂于血管外科行颈动脉体瘤切除术及颈动脉人工血管重建术,回顾当时术中病理结果显示颈动脉体瘤结构,瘤细胞在纤维组织内穿插生长,可见瘤巨细胞,被膜可见瘤细胞,送检淋巴结淋巴组织增生。术后1年复查发现人工血管闭塞血栓形成,之后间断复查若干次均未发现颈部肿物,直至本次发病。根据上述病史,可以认为当时手术治疗已达到了瘤体全切的目的,且颈部淋巴结当时未见转移。现患者经过16年出现了颈部淋巴结转移,并且PET-CT显示肺部及纵隔有异常高代谢,考虑转移可能。这种时隔16年再次发病并出现恶变转移的情况实属罕见。恶性颈动脉体瘤的恶性生物学行为比较少,有报道肿瘤的大小与恶性行为有一定相关性,肿瘤越大恶性程度可能越大,与血管神经关系也越密切[6]。颈动脉体瘤以散发性和家族性发病,其中家族性占10%以上[7]。散发性颈动脉体瘤中多灶性占10%~20%,而在家族性中多灶性高达80%[8]。绝大多数颈动脉体瘤都是良性且无分泌功能,家族性的常双侧发病并且有分泌功能[9]。本例患者无明显家族遗传性,至于初次起病是否存在多灶性,而后是因为其他病灶引起恶变转移,还是当时有隐匿的局部残留组织经过数年发生了恶变转移(16年前并未行全身PET-CT),目前无从评估。
本例患者术后预后良好,后继续在胸外科、肿瘤科进行治疗。因为颈动脉体瘤生长有局部侵袭性、一定的恶变率及多灶性特点,除常规的CT、MRI增强、DSA等检查外,术前行PET-CT检查将有助于对肿瘤有无转移及多灶性进行评估。
Footnotes
利益冲突 所有作者均声明不存在利益冲突
References
- 1.Hoang VT, Trinh CT, Lai T, et al. Carotid body tumor: a case report and literature review. J Radiol Case Rep. 2019;13(8):19–30. doi: 10.3941/jrcr.v13i8.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metheetrairut C, Chotikavanich C, Keskool P, et al. Carotid bdoy tumor: a 25-year experience. Eur Arch Otorhinolaryngy. 2016;273(8):2171–2179. doi: 10.1007/s00405-015-3737-z. [DOI] [PubMed] [Google Scholar]
- 3.Darouassi Y, Alaoui M, Mliha Touati M, et al. Carotid body tumors: a case series and review of the literature. Ann Vasc Surg. 2017;43:265–271. doi: 10.1016/j.avsg.2017.03.167. [DOI] [PubMed] [Google Scholar]
- 4.Usman R, Jamil M, Aman A. Surgical Excision of Carotid Body Tumor at an Early Stage Has Best Outcome: Results of 22 Cases along with Literature Review. Ann Vasc Dis. 2020;13(4):365–369. doi: 10.3400/avd.oa.20-00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.陈 婷, 沈 暘. 颈动脉体瘤的外科治疗及并发症预防与处理. 临床耳鼻咽喉头颈外科杂志. 2018;32(9):713–716. doi: 10.13201/j.issn.1001-1781.2018.09.018. [DOI] [PubMed] [Google Scholar]
- 6.顾 光超, 刘 志丽, 刘 暴, et al. 恶性颈动脉体瘤的外科治疗. 中华普通外科杂志. 2020;35(3):183–186. [Google Scholar]
- 7.Yao L, Schiavi F, Cascon A, et al. Spectrum and prevalence of FP/TMEM127 gene mutations in pheochromocytomas and paragangliomas. JAMA. 2010;304(23):2611–2619. doi: 10.1001/jama.2010.1830. [DOI] [PubMed] [Google Scholar]
- 8.Lee JH, Barich F, Karnell LH, et al. National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer. 2002;94(3):730–737. doi: 10.1002/cncr.10252. [DOI] [PubMed] [Google Scholar]
- 9.Alshamsan B, Atallah JP. Durable Response to Pazopanib in Recurrent Metastatic Carotid Body Paraganglioma. Case Rep Oncol. 2020;13(3):1227–1231. doi: 10.1159/000510003. [DOI] [PMC free article] [PubMed] [Google Scholar]