Introduction and importance:
Gastrointestinal metastasis of pleomorphic lung cancer presents with nonspecific manifestations, leading to delayed diagnosis. Herein, the authors report the case of a 56-year-old patient who presented with gastrointestinal bleeding due to pleomorphic lung carcinoma.
Case presentation:
A 56-year-old patient presented to the emergency department with melena. On examination, he was hemodynamically stable. He had a sensitive and mobile mass in the periumbilical region. A thoracoabdominal computed tomography scan showed a mass of the right apical superior lobe measuring 4 cm and a lobulated jejunal mass measuring 10 cm. A percutaneous biopsy of the lung tumor revealed primary pleomorphic lung carcinoma. The authors performed a midline laparotomy and made a bowel resection with an end-to-end anastomosis. The postoperative course was marked by severe nosocomial pneumonia, leading to septic shock and death. The histopathologic examination concluded with a metastatic lesion of pleomorphic lung carcinoma.
Clinical discussion:
The authors reported a rare case of jejunal metastasis of pleomorphic lung cancer. Pleomorphic carcinoma of the lung is a rare pathology that accounts for 0.1–0.4% of nonsmall-cell lung cancer. The prognosis is poor. In the presence of gastrointestinal bleeding caused by small bowel metastases of pleomorphic lung cancer, surgery is the treatment of choice.
Conclusions:
Small bowel metastasis of pleomorphic lung cancer is rare. Surgical treatment is the treatment of choice. The authors highlight the importance of suspecting gastrointestinal metastases in patients with pleomorphic lung cancer in the presence of nonspecific digestive symptoms.
Keywords: pleomorphic lung cancer, jejunal metastasis, gastrointestinal bleeding, case report
Background
Highlights
Jejunal metastases of pleomorphic carcinoma of the lung are rare.
The clinical presentation is not specific.
Surgical treatment is the best option in the presence of gastrointestinal bleeding.
The prognosis is poor.
Pleomorphic carcinoma of the lung is defined as a poorly differentiated nonsmall-cell carcinoma1. It is rare and represents less than 1% of all lung malignancies2. Gastrointestinal metastasis of pleomorphic lung cancer presents with nonspecific manifestations, leading to delayed diagnosis. Thus, those metastases are recognized at an important size or at the stage of complications. Symptomatic gastrointestinal metastasis of lung cancer is rare and accounts for 0.17–2% of nonsmall-cell lung cancer cases3–5.
Herein, we report the case of a 56-year-old patient who presented with gastrointestinal bleeding due to pleomorphic lung carcinoma.
This work has been reported in line with the SCARE 2020 criteria6.
Case presentation
A 56-year-old patient, nonsmoker, having a chronic cough and weight loss for 8 months presented to the emergency department with melena.
On examination, the patient had a poor general status. He had restricted physical activity, spending less than 50% of the day in bed (World Health Organization performance status score=2). He was hemodynamically stable. He had a sensitive and mobile mass in the periumbilical region. On rectal examination, he had melena.
Laboratory studies revealed a hemoglobin of 7.2 g/dl, urea of 11 mmol/l, creatinine of 89 µmol/l, platelet count of 344 000/µl, prothrombin time of 98%, white blood cell count of 9800/µl, and C-reactive protein of 32 mg/l.
Initially, the patient had fluid resuscitation and required two units of packed red blood cells during the initial 3 days of hospitalization.
The esogastroduodenal fibroscopy showed no evidence of bleeding. A total colonoscopy showed melena in the colon but failed to reveal the bleeding site.
A thoracoabdominal computed tomography scan showed an irregular mass of the right apical superior lobe measuring 4 cm (Fig. 1) and a lobulated heterogeneous jejunal mass with a necrotic center measuring 10 cm (Fig. 2).
Figure 1.

Thoracic computed tomography scan showing the tumor in the right apical superior lobe (arrow).
Figure 2.
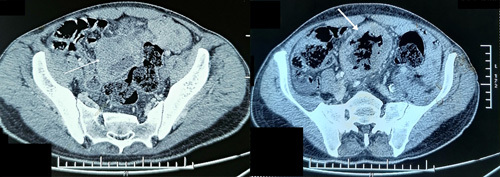
Abdominal computed tomography scan showing the jejunal mass (arrow).
We performed a percutaneous biopsy of the thoracic tumor. Histopathology concluded with a primary pleomorphic lung carcinoma.
At the multidisciplinary meeting, we decided to operate on the jejunal tumor first due to the persistence of bleeding.
We performed a midline laparotomy. We found a large jejunal mass (Fig. 3). We performed bowel resection with end-to-end anastomosis. The postoperative course was marked by severe nosocomial pneumonia, leading to septic shock and death. The histopathologic examination concluded with a metastatic lesion of the pleomorphic lung carcinoma (Fig. 4).
Figure 3.
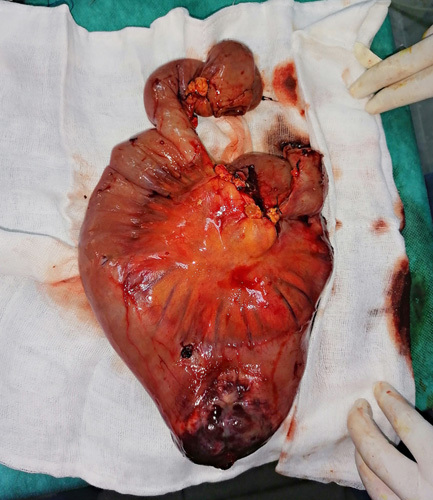
Intraoperative view.
Figure 4.
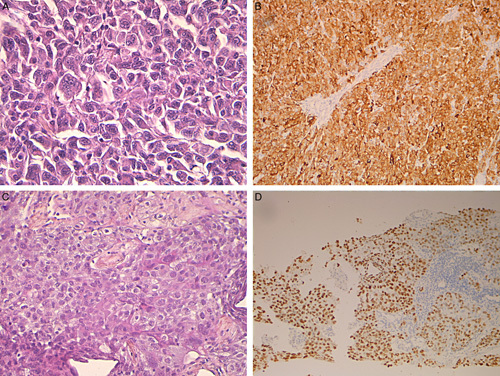
Histopathology findings. (A) Small bowel wall infiltration by poorly differentiated malignant proliferation with large fusiform or polyhedral cells and pleomorphic nuclei (hematoxylin and eosin, ×400). (B) Small bowel tumor cells intensely and diffusely express cytokeratin marker in immunohistochemistry. (C) Primary pleomorphic lung carcinoma similar in appearance to that described in the small bowel (hematoxylin and eosin, ×200). (D) Intense and diffuse expression of TTF1 in the lung tumor. TTF1, Thyroid transcription factor.
Discussion
We reported a rare case of jejunal metastasis of pleomorphic lung cancer. The main strength of our work is the rarity of this pathology and its presentation with gastrointestinal bleeding. The main weakness is the impossibility of performing a long follow-up to assess the importance of surgical treatment for bowel metastases due to the death of the patient.
Pleomorphic carcinoma of the lung is a rare pathology that accounts for 0.1–0.4% of nonsmall-cell lung cancer7. The prognosis of pleomorphic carcinoma is poor compared to that of adenocarcinoma or squamous cell carcinoma. It is characterized by the presence of malignant epithelial and homologous sarcomatoid cell components with coexpression of cytokeratin and vimentin in different proportions8,9. It is associated with smoking and occurs more frequently in men10. This tumor is more aggressive due to its rapid progression and the higher risk of distant metastases11,12. Yoshimoto et al. 13 found that pleomorphic carcinoma is significantly more associated with gastrointestinal metastases compared to the other types of nonsmall-cell lung carcinomas. Previous observational studies showed that the nonsmall-cell lung carcinoma that caused intestinal metastases presented prominent PD-L1 expression14,15. Small bowel metastases do not present with specific manifestations, leading to a late diagnosis. It can manifest with tarry stools, gastrointestinal bleeding, abdominal pain, and rarely intussusception8. In our case, the jejunal metastasis was symptomatic with gastrointestinal bleeding. Preoperatively, differential diagnoses were evoked: gastrointestinal stromal tumor, lymphoma, adenocarcinoma, and leiomyosarcoma of the small bowel16–19. Routine endoscopy cannot detect those metastases. In an autopsy analysis, it was found that 11.9% of lung cancer patients had gastrointestinal metastases13.
An enhanced computed tomography scan is essential to reveal the lesion. However, the definitive diagnosis can only be confirmed postoperatively via histopathology examination.
In the presence of gastrointestinal bleeding caused by small bowel metastases of pleomorphic lung cancer, surgery is the treatment of choice. Ikushima et al. 20 reported successful control of intestinal bleeding from ileal metastasis of pleomorphic lung cancer with pembrolizumab. This can be an efficient therapeutic option to control the tumor and its metastases. It permits to prepare the patient for surgery under better conditions.
In summary, we reported a rare case of jejunal metastasis of pleomorphic lung cancer that presented with gastrointestinal bleeding. An enterectomy was performed to treat the complication. The poor general status of the patient was the main cause of severe postoperative pneumonia and death.
Conclusions
Small bowel metastasis of pleomorphic lung cancer is rare. Gastrointestinal bleeding is one of the clinical presentations of those metastases. Surgical treatment is the treatment of choice. We highlight the importance of suspecting gastrointestinal metastases in patients with pleomorphic lung cancer in the presence of nonspecific digestive symptoms.
Ethical approval
Ethical approval for this study was obtained from the ethical committee of the hospital.
Patient consent
Written informed consent was obtained from the patient’s next of kin for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
H.B. and G.L. did the conception and design of the work, the data collection, the data analysis and interpretation, and the writing of the manuscript. M.F.C., S.Z., S.S., and S.N. participated in the writing of the manuscript. M.B. and H.T. did the critical revision of the article and the final approval of the version to be published.
Conflicts of interest disclosure
No conflicts of interest.
Research registration unique identifying number (UIN)
None.
Guarantor
Dr Hazem Beji.
Provenance and peer review
Not commissioned, externally peer reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online ■ ■
Contributor Information
Hazem Beji, Email: Hazembj@gmail.com.
Ghazi Laamiri, Email: lamirighazi@gmail.com.
Mohamed F. Chtourou, Email: medchtourou@yahoo.fr.
Slim Zribi, Email: slim_z@msn.com.
Siwar Sbaihi, Email: Siwar_sb@hotmail.com.
Salwa Nechi, Email: salwanechi@hotmail.com.
Mahdi Bouassida, Email: bouassidamahdi@yahoo.fr.
Hassen Touinsi, Email: hassen.touinsi@gmx.fr.
References
- 1. Travis WD, Brambilla E, Nicholson AG, et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 2015;10:1243–1260. [DOI] [PubMed] [Google Scholar]
- 2. Ito K, Oizumi S, Fukumoto S, et al. Clinical characteristics of pleomorphic carcinoma of the lung. Lung Cancer 2010;68:204–210. [DOI] [PubMed] [Google Scholar]
- 3. Nishizawa Y, Kobayashi A, Saito N, et al. Surgical management of small bowel metastases from primary carcinoma of the lung. Surg Today 2012;42:233–237. [DOI] [PubMed] [Google Scholar]
- 4. Lee PC, Lo C, Lin MT, et al. Role of surgical intervention in managing gastrointestinal metastases from lung cancer. World J Gastroenterol 2011;17:4314–4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang CJ, Hwang JJ, Kang WY, et al. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer 2006;54:319–323. [DOI] [PubMed] [Google Scholar]
- 6. Agha RA, Franchi T, Sohrabi C, et al. SCARE Group. The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 7. Kaira K, Horie Y, Ayabe E, et al. Pulmonary pleomorphic carcinoma: a clinicopathological study including EGFR mutation analysis. J Thorac Oncol 2010;5:460–465. [DOI] [PubMed] [Google Scholar]
- 8. Lin MW, Wu CT, Chang YL. Intussusception caused by intestinal metastasis from lung pleomorphic carcinoma. Ann Thorac Cardiovasc Surg 2014;20(Suppl):635–638. [DOI] [PubMed] [Google Scholar]
- 9. Shi B, Gaebelein G, Hildebrandt B, et al. Adult jejunojejunal intussusception caused by metastasized pleomorphic carcinoma of the lung: report of a case. Surg Today 2009;39:984–989. [DOI] [PubMed] [Google Scholar]
- 10. Raveglia F, Mezzetti M, Panigalli T, et al. Personal experience in surgical management of pulmonary pleomorphic carcinoma. Ann Thorac Surg 2004;78:1742–1747. [DOI] [PubMed] [Google Scholar]
- 11. Chen M, Yang Q, Xu Z, et al. Survival analysis and prediction model for pulmonary sarcomatoid carcinoma based on SEER Database. Front Oncol 2021;11:630885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xiao C, Yang X, Hao J, et al. Clinicopathological features and prognostic analysis of metastatic pulmonary sarcomatoid carcinoma: a SEER analysis. J Thorac Dis 2021;13:893–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yoshimoto A, Kasahara K, Kawashima A. Gastrointestinal metastases from primary lung cancer. Eur J Cancer 2006;42:3157–3160. [DOI] [PubMed] [Google Scholar]
- 14. Suzuki T, Noda M, Yamamura A, et al. Persistent fecal occult blood due to the small intestinal metastasis of pleomorphic lung carcinoma. J Surg Case Rep 2022;2022:rjac043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ishikawa E, Nakaguro M, Nakamura M, et al. Gastrointestinal tract metastasis of lung cancer: the PD-L1 expression and correlated clinicopathological variables. Pathol Int 2021;71:33–41. [DOI] [PubMed] [Google Scholar]
- 16. Beji H, Zribi S, Bouassida M, et al. Snapshots quiz. Br J Surg 2022;109:390. [DOI] [PubMed] [Google Scholar]
- 17. Beji H, Bouassida M, Zribi S, et al. Ileal gastrointestinal stromal tumor causing mesenteric gangrene. Clin Case Rep 2022;10:e05772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bouassida M, Beji H, Chtourou MF, et al. Leiomyosarcoma of the small bowel: a case report and literature review. Int J Surg Case Rep 2022;97:107456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ma JLG, Strauss PN. The elusive small bowel adenocarcinoma in the terminal ileum – a case report. Int J Surg Case Rep 2018;47:97–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ikushima H, Asaga R, Sakatani T, et al. Successful control of intestinal bleeding from metastasis of pulmonary pleomorphic carcinoma with pembrolizumab: a case report. Medicine (Baltimore) 2022;101:e31220. [DOI] [PMC free article] [PubMed] [Google Scholar]


