Introduction and importance:
Meningiomas are intracranial extracerebral tumors derived from arachnoid cells of the neural crest. They represent ∼20% of primary intracranial tumors and are seen as more common in elderly patients and women. Recurrence of meningioma can be observed during the early years after surgical treatment, but their occurrence within 10 years is rare.
Case presentation:
In this report, the authors discuss a case of a 75-year-old patient with a recurrence of a frontal meningioma after 10 years of successful surgical resection. Our patient was a female who presented amnesia and memory lapses associated with several weeks of progressive heaviness of the lower limbs accompanied by speech heaviness, intense headaches, asthenia, consciousness disorder, and tonic–clonic convulsive seizures for 10 days. The patient had previously been treated for a benign meningioma by surgical excision. Imaging was performed, and recurrent frontal meningioma was retained as a final diagnosis. The patient underwent a successful total resection of her frontal tumor.
Clinical discussion:
Recurrent tumors after complete surgical removal of meningiomas are rare and may be associated with microscopic residues. The more radical the surgery, the lower the risk of observing a recurrence. Adjuvant radiotherapy can be proposed, but the evidence is still lacking. Careful follow-up of all patients with or without complete surgical resection is therefore recommended.
Conclusion:
This case illustrates the importance of suspecting recurrence of meningioma in adult patients after successful surgical excision, even after 10 years of free disease. Clinicians should be aware of long-term meningioma recurrence in this population, and imaging is key for a positive diagnosis.
Keywords: case report, long-term recurrence, meningioma, surgical resection
Introduction
Highlights
Meningiomas are intracranial and extracerebral benign tumors.
Long-term recurrence after complete surgical resection is rare.
Long-term and accurate follow-up of these patients with imaging is crucial to detect recurrence.
Meningiomas are intracranial and extracerebral malignancies originating from arachnoid cells1. These tumors often invade the dura mater and the skull with hyperplastic growth of bone tissue2. The annual incidence of all meningiomas is estimated at 8 per 100 000 inhabitants3. They represent ∼20% of primary intracranial tumors and are more common in elderly patients, particularly women1,4,5. Meningiomas are frequently diagnosed in the elderly population, with an increased incidence in subjects aged more than 56 years6. The recurrence of meningioma is frequent, but it becomes rare after 10 years of successful surgical removal7,8. Several symptoms can reveal recurrence, particularly cognitive and executive impairments5. In this paper, we discuss a case of a 75-year-old patient with a recurrence of a frontal meningioma after 10 years of complete surgical excision according to SCARE (Surgical CAse REport) guidelines9.
Case report
Our 75-year-old patient had amnesia and memory lapses for several months and a progressive heaviness of the lower limbs for several weeks accompanied by signs of aggravation, including heaviness of speech, intense headaches and asthenia, disorders of consciousness, and tonic–clonic convulsive seizures. Her past medical history was marked by hypertension since 1995, and she was previously treated successfully for benign frontal meningioma by complete resection. Upon admission, her Karnofsky performance index was 70%, and her Glasgow score was 12 without hemodynamic instability. The clinical examination found a patient with total Broca’s aphasia, characterized by a complete inability to speak and name relatives and objects associated with anxiety.
A brain MRI (Fig. 1) with contrast injection showed a bilateral frontal meningioma more marked on the right, measuring 7.3 cm laterally, 5.7 mm in the anteroposterior side, and extended in height over 5 cm. The tumor had meningeal implantation encompassing the anterior part of the longitudinal sinus and had a mass effect on the frontal horns of the lateral ventricles and the corpus. A computed tomography scan was also performed and showed the presence of a bifrontal extra-axial lesion surrounded by significant perilesional edema (Fig. 2).
Figure 1.
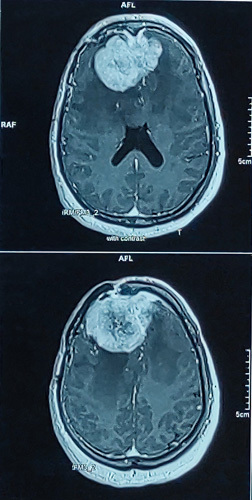
Brain MRI showing a recurrent bilateral frontal meningioma.
Figure 2.
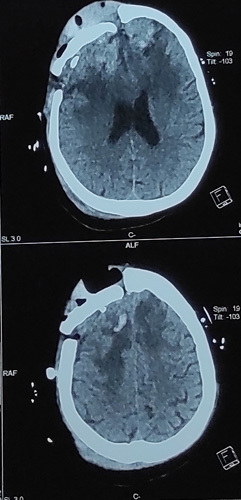
Computed tomography scan showing a recurrent lesion surrounded by significant perilesional edema.
The patient underwent total resection of her frontal tumor by a senior neurosurgeon with the support of young fellows. The histopathological examination found a meningioma with a hemorrhagic appearance of a grayish-white color. This was an atypical WHO grade II meningioma composed of a proliferation of meningothelial cells largely altered by fibrosis. The cells were arranged in clumps and the mitotic count was estimated at one mitosis per 10 fields. Two weeks following total surgical excision, Broca’s aphasia disappeared with a Glasgow score of 15/15 without any deficit. The Mini-Mental State Examination for global cognitive assessment was performed, and our patients had mild cognitive dementia. The patient also had postoperative anxiety without depression based on the Hospital Anxiety and Depression Scale (HADS) test. We discharged the patient, and she was followed up regularly as per international recommendations. At the time of reporting this case, our patient had a gradual decrease in anxiety and weakness in her lower limbs, and she was satisfied with our management.
Discussion
Meningiomas are frequent and represent an important number of primary brain tumors6,7. The diagnosis of meningiomas is usually made between 20 and 60 years of age, with a peak incidence in the 5th decade10. Recurrence of meningiomas after complete removal is estimated to be 10–32% of cases within 10 years7,8. The female predominance is classic and the prevalence in women is explained in part by the presence of progesterone receptors on these tumors in addition to other types of hormonal receptors such as estrogen, androgen receptors, and glucocorticoid receptors10–14. This accounts for 63–79% of female predominance12–15. Headaches represent predominant revealing symptoms10,16–18 and the motor deficit is frequent in patients treated for meningiomas and its prevalence accounts for more than 50% in some studies10,16. Epileptic seizures can also be seen in this population. Consciousness disorders are a rarely revealing sign of meningiomas. They are seen especially in patients who consult late when the tumor becomes larger. This was reported in 1.8–7.14% of patients with meningiomas19,20. For depression and anxiety in meningiomas, patients were found to show higher levels of distress than in the general population, which was also seen in our patient’s case. In fact, the proportion of patients with abnormal HADS-A scores can reach 70%, and 30% for HADS-D in operated patients21–24.
In elderly patients, intracranial meningiomas are the most commonly diagnosed benign tumors. The age of this population of patients (aged 70 years or more), in addition to other factors such as surgery duration and extent of tumor resection, is believed to drive surgical outcomes as demonstrated in several of recent studies25,26. Indeed, elderly patients have unfavorable outcomes as compared to the younger meningioma population, which was not confirmed in our surviving patient. Recurrence in patients treated with surgery is associated with incomplete resection25–27. However, recurrent tumors after complete surgical removal are rare, and they might be associated with microscopic residue, as in our patient. In a case series, recurrence was seen years and decades after surgical interventions such as in our case, but this was associated with subtotal resection28. In fact, the more radical the surgery, the smaller the risk of observing a recurrence26, which is consistent with the long-term outcomes in our patient. Some authors have proposed to proceed directly after surgery with adjuvant radiotherapy, as it reduces the risk of recurrence29. Incomplete removal of meningiomas can recur 15 years after a tumor-free period30, therefore, a careful follow-up of all patients with or without complete surgical resection is recommended.
Conclusion
This report illustrated the case of a 75-year-old patient who presented a recurrence of her meningioma after 10 years of diagnosis and complete excision. Our case report emphasizes the importance of long-term follow-up of patients with meningiomas treated with complete surgical resection.
Ethical approval
Not required for this case report.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
No funding was received for this research.
Author contribution
L.M. and E.O.A.: data collection; L.M.: writing the paper. All authors were involved in the study concept.
Conflicts of interest disclosure
The authors have no conflicts of interest to declare.
Research registration unique identifying number (UIN)
None.
Guarantor
Legmouz M.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 27 March 2023
Contributor Information
Maria Legmouz, Email: mlegmouz@hotmail.com.
Abdessamad El Ouahabi, Email: elouahabi.a@hotmail.fr.
Samira Boulbaroud, Email: samira.boulbaroud@yahoo.fr.
Fatimazahra Azzaoui, Email: azzaouifz@outlook.com.
References
- 1. Claus EB, Bondy ML, Schildkraut JM, et al. Epidemiology of intracranial meningioma. Neurosurgery 2005;57:1088–1095. [DOI] [PubMed] [Google Scholar]
- 2. Schrell UM, Rittig MG, Anders M, et al. Hydroxyurea for treatment of unresectable and recurrent meningiomas. I. Inhibition of primary human meningioma cells in culture and in meningioma transplants by induction of the apoptotic pathway. J Neurosurg 1997;86:845–852. [DOI] [PubMed] [Google Scholar]
- 3. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 2016;131:803–820. [DOI] [PubMed] [Google Scholar]
- 4. Ostrom QT, McCulloh C, Chen Y, et al. Family history of cancer in benign brain tumor subtypes versus gliomas. Front Oncol 2012;2:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tucha O, Smely C, Preier M, et al. Cognitive deficits before treatment among patients with brain tumors. Neurosurgery 2000;47:324–333. [DOI] [PubMed] [Google Scholar]
- 6. DeMonte F, Marmor E, Al-Mefty O. Meningiomas. In Kaye AH, Laws ER, editors. Brain Tumors. Churchill Livingstone; 2001:719–750.
- 7. Adegbite AB, Khan MI, Paine KW, et al. The recurrence of intracranial meningiomas after surgical treatment. J Neurosurg 1983;58:51–56. [DOI] [PubMed] [Google Scholar]
- 8. Mirimanoff RO, Dosoretz DE, Linggood RM, et al. Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 1985;62:18–24. [DOI] [PubMed] [Google Scholar]
- 9. Agha RA, Franchi T, Sohrabi C, et al. for the SCARE Group. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Internat J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 10. Kakou M, Mwanyombet L, Jan M. Méningiomes intracrâniens. Rev Méd Tours Centre Ouest 1993;33:278–286. [Google Scholar]
- 11. Alaywan M, Sindou M. Facteurs pronostiques dans la chirurgie des méningiomes intracrâniens. Neurochirurgie 1993;39:337–347. [PubMed] [Google Scholar]
- 12. Colli BO, Carlotti CG, Jr, Assirati JA, Jr, et al. Parasagittal meningiomas: follow-up review. Surg Neurol 2006;66(Suppl 3):S20–S27. [DOI] [PubMed] [Google Scholar]
- 13. Akagami R, Napolitano M, Sekhar LN. Patient-evaluated outcome after surgery for basal meningiomas. Neurosurgery 2002;50:941–948. [DOI] [PubMed] [Google Scholar]
- 14. Reinert M, Babey M, Curschmann J, et al. Morbidity in 201 patients with small sized meningioma treated by microsurgery. Acta Neurochir (Wien) 2006;148:1257–1265. [DOI] [PubMed] [Google Scholar]
- 15. Nema IS, Jasim M, Hamandi YMH. Intracranial meningiomas: diagnosis and treatment. N Iraqi J Med 2010;6:47–52. [Google Scholar]
- 16. Palma L, Celli P, Franco C, et al. Long-term prognosis for atypical and malignant meningiomas: a study of 71 surgical cases. J Neurosurg 1997;86:793–800. [DOI] [PubMed] [Google Scholar]
- 17. Balhaoui A. Intracranial meningiomas, about 67 cases [Les méningiomes intra-crâniens, à propos de 67 cas]. Thèse MédCasa 1990:10–45. [Google Scholar]
- 18. Amjahdi A. Management of intracranial meningiomas about 28 case [Prise en charge des méningiomes intracrâniens à propos de 28 cas]. Thèse MédCasa 2003;157:5–44. [Google Scholar]
- 19. Ephrem Mbou Ekambou. Intracranial meningiomas about 115 case [Méningiomes intracrâniens à propos de 115 cas]. Thèse n° 119: faculté de médecine de Rabat, 2008.
- 20. Hal El Fadl S. Intracranial meningiomas apropos of 387 cases [Méningiomes intracrâniens à propos de 387 cas]. Thèse n° 349, faculté de médecine de Rabat, 2002.
- 21. Bunevicius A, Deltuva VP, Tamasauskas A. Association of pre-operative depressive and anxiety symptoms with five-year survival of glioma and meningioma patients: a prospective cohort study. Oncotarget 2017;8:57543–57551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wagner A, Shiban Y, Lange N, et al. The relevant psychological burden of having a benign brain tumor: a prospective study of patients undergoing surgical treatment of cranial meningiomas. J Neurosurg 2019;131:1840–1847. [DOI] [PubMed] [Google Scholar]
- 23. Goebel S, Mehdorn HM. Development of anxiety and depression in patients with benign intracranial meningiomas: a prospective long-term study. Support Care Cancer 2013;21:1365–1372. [DOI] [PubMed] [Google Scholar]
- 24. van der Vossen S, Schepers VP, Berkelbach van der Sprenkel JW, et al. Cognitive and emotional problems in patients after cerebral meningioma surgery. J Rehabil Med 2014;46:430–437. [DOI] [PubMed] [Google Scholar]
- 25. Schul D, Wolf S, Krammer M, et al. Meningioma surgery in the elderly: outcome and validation of 2 proposed grading score systems. Neurosurgery 2012;70:555–565. [DOI] [PubMed] [Google Scholar]
- 26. Bir S, Konar S, Maiti T, et al. Surgical outcomes and predictors of recurrence in elderly patients with meningiomas. World Neurosurg 2016;90:251–261. [DOI] [PubMed] [Google Scholar]
- 27. Poon MT, Fung LH, Pu JK, et al. Outcome of elderly patients undergoing intracranial meningioma resection – a systematic review and meta-analysis. Br J Neurosurg 2014;28:303–309. [DOI] [PubMed] [Google Scholar]
- 28. Ambekar S, Sharma M, Kukreja S, et al. Complications and outcomes of surgery for spinal meningioma: a nationwide inpatient sample analysis from 2003 to 2010. Clin Neurol Neurosurg 2014;118:65–68. [DOI] [PubMed] [Google Scholar]
- 29. Klinger D, Flores B, Lewis J, et al. Atypical meningiomas: recurrence, reoperation, and radiotherapy. World Neurosurg 2015;84:839–845. [DOI] [PubMed] [Google Scholar]
- 30. Hasseleid B, Meling TR, Rønning P, et al. Surgery for convexity meningioma: simpson grade I resection as the goal. J Neurosurg 2012;117:999–1006. [DOI] [PubMed] [Google Scholar]


