To the Editor: Ankylosing spondylitis (AS) is a chronic inflammatory disease that causes bony fusion of spine and sacroiliac joints, resulting in restricted spinal movement and deformity. In China, the prevalence of AS is about 0.29% with a male to female ratio of approximately 3:1, and most cases occur in the adolescent period.[1] The misdiagnosis rate of AS patients in China is >50%, and the average delay time of diagnosis is >7 years. Without standardized treatment, the 3-year disability rate of AS patients can reach 45.5%, and the 5-year disability rate can reach 70%. At present, there are approximately 100,000 AS people among the low-income population registered in China, including about 20,000 people with moderate to severe AS. Lacking timely and correct treatment, nearly half of patients suffer from different degrees of disability every year, and most of them give up treatment for financial conditions, resulting in lifelong paralysis. 10.5% of male AS patients, as the “breadwinners” of family, lose their jobs due to the decline in working ability, absence of treatment, and unaffordable treatment cost, causing a serious impact on the patient, family, and society.[2] Thus, it is an important social health problem to tackle poverty and return of poverty among people with moderate to severe AS in developing areas.
On October 8, 2019, the State Council Leading Group Office of Poverty Alleviation and Development of China and the National Health Commission of the People's Republic of China distributed a document that AS health poverty alleviation project would be officially implemented in 832 impoverished counties of 22 central and western provinces. Therefore, our study was carried out in the mentioned 832 impoverished counties and investigated the current state of the medical environment for patients with moderate to severe AS in developing areas of China, which was expected to enrich the project and provide a reference for the public health authorities.
The study was conducted between March 2019 and December 2020 in 20 provinces (municipalities and autonomous regions) across China, including Yunnan, Henan, Guangxi, Shanxi, Anhui, Hubei, Jiangxi, Guizhou, Gansu, Shaanxi, Hunan, Chongqing, Inner Mongolia, Hebei, Ningxia, Hainan, Heilongjiang, Jilin, and Qinghai. The criterion for poverty is defined as an annual income of <¥2300 for a person per year referenced to the 2010 Rural Poverty Standard in China.[3] In our study, the disease activity of AS patients was assessed using the Ankylosing Spondylitis Disease Activity Score (ASDAS). The criterion of moderate to severe AS was defined as the ASDAS of 1.3 or above.[4] All the primary hospitals admitting patients with poverty and moderate to severe AS were screened out in the mentioned 832 impoverished counties, and their doctors occupied in AS-related treatment were also investigated through online questionnaires. Informed consent either orally or in writing was obtained from these primary hospitals and doctors. The statistical analysis was conducted on the establishment of rheumatology departments, rheumatology screening capacity, traffic conditions to primary hospitals, and the learning needs of doctors. All data were analyzed using the Statistical Package for the Social Sciences (SPSS) 26.0 (IBM Corp., NY, USA).
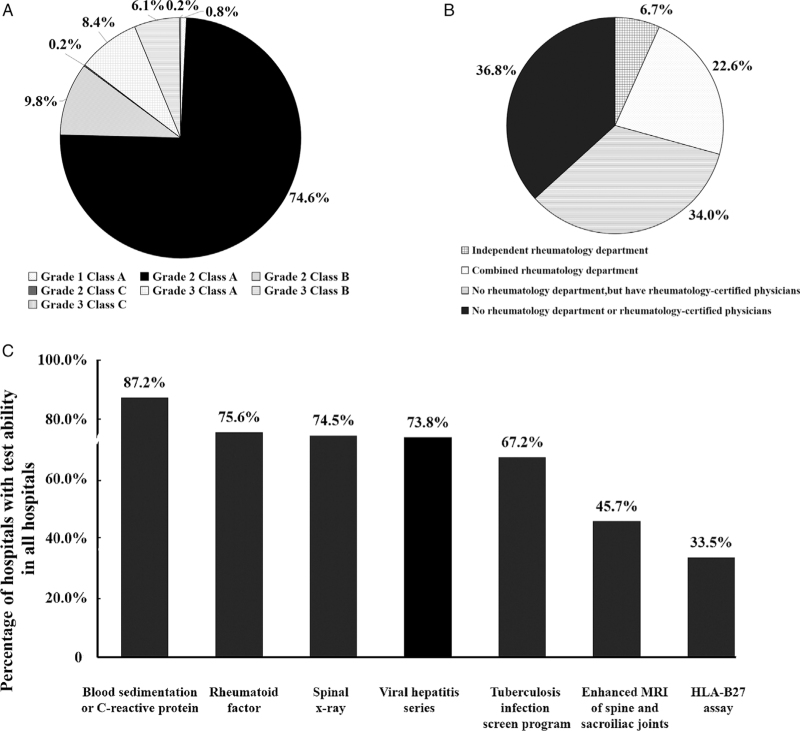
During the study, a total of 756 primary hospitals and 4305 doctors were included. Among these primary hospitals, 85.3% were Grade 2 and below [Figure 1A]; 93.3% did not establish an independent rheumatology department, 70.8% did not have rheumatology-related departments, and 36.8% did not have rheumatology-certified physicians [Figure 1B]. In addition, 66.5% of primary hospitals still did not have HLA-B27 testing capability, and 54.3% of primary hospitals were not able to perform enhanced magnetic resonance imaging (MRI) of the spine and sacroiliac joints [Figure 1C].
Figure 1.
Grades of primary hospitals (A), a circumstance of the establishment of rheumatology departments in primary hospitals (B), and capacity of rheumatology-related test and imaging examinations in primary hospitals (C).
The results showed that rheumatology departments in primary hospitals in developing areas of China were imperfectly established, lacking rheumatologists and the capability of rheumatology-related index testing and imaging examination. There are >200 million patients with rheumatic diseases in China, but only 12,189 rheumatology and immunology specialists and 6250 registered rheumatology specialists, presenting a big gap between the number of doctors and patients. Therefore, the training of rheumatology professionals will remain an important focus in the future, meanwhile, much improvements are needed in public health education, medical level of primary hospitals, the establishment of specific rheumatology department, and data management of patient treatment. On the other hand, early and effective intervention for AS can largely influence the progress and promote the recovery of patients, so the early diagnosis of AS is particularly important. As one of the effective means for early diagnosis of AS, MRI examination has a higher sensitivity and can detect changes in the sacroiliac joint at an earlier stage than X-ray. However, our results showed that nearly half of the primary hospitals were unable to perform MRI examination, so it is also one of the future concentrated directions to improve the primary testing facilities.
Among the 756 primary hospitals in our study, 34.8% were >100 km (in the straight-line distance) away from their urban area, with an average distance of 90 km; 92.7% were >100 km away from their provincial capital, and 73.0% were >200 km with an average distance of 301 km. A survey on the current status of outpatient treatment for patients with rheumatoid arthritis and AS in Xi’an showed that AS patients were mainly farmers who participated in the new rural cooperative medical care, and only 45.3% of patients had been treated with biologics.[5] It can be speculated that low use of biologics in poor AS patients might be connected with the long distance to the designated hospital, in addition to the high cost of treatment.
As for learning, many doctors prefer online skills training. However, the learning needs of primary hospitals’ doctors in descending order were offline theoretical knowledge training (78%), advanced training at higher-level hospitals (68%), regular medical consultations by higher-level specialists (66%), regular visits by higher-level specialists (60%), online training (50%), participation in academic conferences (48%), and online consultations by specialists (43%). It is an interesting finding in our study that primary hospitals’ doctors still prefer traditional offline teaching, thus subsequent training projects may be mainly based on offline learning or a combination of online and offline learning.
There are some shortcomings in the present study, including (1) This study lacks the transportation used by patients, which only investigated the distance between primary hospitals and the city center; (2) Patients receiving non-steroidal anti-inflammatory drugs and sulfasalazine is not included in this study due to difficulties in obtaining information about their previous medication; (3) Due to inadequate training of primary hospitals’ doctors in AS history collection, physical examination, and condition assessment, information about AS characteristics is incomplete in this study; (4) The current evaluation indicators of this study are incomprehensive and less convincing to reflect the diagnosis and treatment level of primary hospitals’ doctors, the diagnostic accuracy rate, treatment efficiency, and other indicators should be included for comprehensive evaluation.
To conclude, the study has far-reaching social significance, which addresses the problems and concerns in the current medical environment of AS patients in developing areas of China. With the joint efforts of rheumatology clinicians and related institutions, the appropriate prevention and treatment system of AS, as well as the med-tech in primary hospitals can be largely promoted to contribute to the poverty population.
Conflicts of interest
None.
Footnotes
How to cite this article: Zhao Y, Wang Q, Duan L, Huang X, Wang P, Fan P, Zou Q, Lin Z, Zhao J, Wu X, Wang L, Gen Y, Zhu X, Zhang Z, Zhang W, Zhao Y. Current health resources required for the management of ankylosing spondylitis in developing areas of China. Chin Med J 2023;136:737–739. doi: 10.1097/CM9.0000000000002200
References
- 1.Wu X, Zhong JY, Wang G, Xu HJ. Factors relating to bone mineral density in young and middle-aged patients with ankylosing spondylitis. Chin Med J 2021; 134:2556–2563. doi: 10.1097/CM9.0000000000001787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tu L, Rai JC, Cao S, Lin Z, Hu Z, Gu J. Costs and work limitation of patients with ankylosing spondylitis in China. Clin Exp Rheumatol 2014; 32:661–666. [PubMed] [Google Scholar]
- 3.Fan ZZ, Zou W. From anti-poverty campaign to common prosperity: dynamic identification of relative poverty and quantitative decomposition of poverty changes in China (in Chinese). China Indust Econ 2021; 10:59–77. doi: 10.3969/j.issn.1006-480X.2021.10.004. [Google Scholar]
- 4.Machado P, Landewé R, Lie E, Kvien TK, Braun J, Baker D, et al. Ankylosing spondylitis disease activity score (ASDAS): defining cut-off values for disease activity states and improvement scores. Ann Rheum Dis 2011; 70:47–53. doi: 10.1136/ard.2010.138594. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Niu R, Zhang XM, Feng BL. Status of implementation and influential factors of the outpatient special diagnosis and treatment project on RA/AS (in Chinese). Herald Med 2018; 37:771–776. doi: 10.3870/j.issn.1004-0781.2018.06.030. [Google Scholar]