Abstract
The authors conducted a systematic review on the effect of coronavirus disease 2019 on electrophysiology (EP) practice and procedure volume in various settings. This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. PubMed/MEDLINE, Scopus, Web of Science, CINAHL, and Embase were examined with combinations of medical subject headings terms for identification of the relevant studies. After excluding duplicates, irrelevant, and ineligible studies, 23 studies were included for full qualitative analysis. The overall study-level volume reduction of EP procedures ranged from 8 to 96.7%. All studies reported an overall reduction in EP physiology procedures being carried out except one in Poland, which reported an overall increase in the total EP procedures carried out in 2020. This study still reported a decrease in EP procedure volume during the first lockdown phase. Procedural volume reduction was seen most commonly for cardiovascular implantable electronic device placement (20/23 studies, 86.9%), electrophysiology studies (11/23 studies, 47.8%), and ablations (9/23, 39.1% studies). The most common reason stated for the observed decline in EP procedures was the cancellation and postponement of nonurgent elective cases in the hospitals (15/23 studies, 65.2%). There has been an overall reduction in EP procedure volume across different centers. The impact of the decline in EP procedures will be seen only after the services resume to prepandemic levels, but an increase in-patient volume and procedure waiting time is expected. This review will provide insights into improving healthcare service delivery in times of unprecedented public health emergencies.
Keywords: catheter ablation, COVID-19 pandemic, elective procedures, electrophysiology, emergency treatment, implantable cardioverter defibrillator, pacemaker
Introduction
Highlights
Many health and therapeutic guidelines were changed with the disease’s growing prevalence globally.
There was a reduction of nonemergency diagnostic and therapeutic procedures to make room for coronavirus disease 2019 patients and take advantage of the structural and functional capacity of the hospitals.
All medical services returned to normal slowly after 1.5 years of lockdown.
A severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused a global pandemic of Coronavirus Disease 2019 (COVID-19), starting in the province of China (Wuhan) in December 20191. An emergency was declared by the WHO in March 2020, and stay-at-home protocols were introduced throughout the world2. Many health and therapeutic guidelines were changed with the disease’s growing prevalence globally. At the start, the main initiative for these guidelines was to minimize the exposure of healthcare workers to COVID-193. Second, there was a reduction of nonemergency diagnostic and therapeutic procedures to make room for COVID-19 patients and take advantage of the structural and functional capacity of the hospitals4. However, as more research was conducted on COVID-19, the nonpulmonary complications came to light, including cardiovascular diseases5–7. Therefore, all medical services slowly returned to normal after 1.5 years of lockdown. Among these, electrophysiological studies (EPSs) and cardiac implantable electronic device (CIED) placement, which were notably decreased during the pandemic, returned to normal8. Due to the increased incidence of cardiac arrhythmias, and ischemic/nonischemic cardiomyopathies associated with COVID-19, cardiac electrophysiology (EP) procedures were started again7. We conducted a systematic review on the effect of COVID-19 on EP practice and procedure volume in various settings.
Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement9. All the data were extracted from the original investigations published on the topic. All data is presented in Table 1, and the consolidated data can be obtained from the references section.
Table 1.
Study characteristics.
| References | Country | Type of study | Type of procedure mentioned | PreCOVID-19 procedure volume | Procedures during COVID-19 | Overall reduction (%) | PostCOVID-19 procedure volume | Summary |
|---|---|---|---|---|---|---|---|---|
| Sulaiman et al.10 | Oman | Retrospective cohort | EPS | Not reported | Not reported | 50 | Not reported | Overall 35% reduction in catheterization lab procedures and 50% reduction in EP procedures |
| Anca et al.4 | USA | Retrospective cohort | CIED placement EPS |
426 | 115 | 73 | Not reported | EP laboratories in the hot spot areas, with a significant number of COVID-19 positive patients, have had to adapt. 14 EP procedures were reduced to many fold during the pandemic |
| Boriani et al .11 | Italy | Retrospective cohort | CIED placement EPS |
Not reported | Not reported | >50% for PPM >50% for ICD >50% for EPS |
Not reported | In this period a reduction of >50% in the number of implants of cardiac electronic devices was reported, and involved pacemakers and ICDs, with an important reduction not only on ICD implants for primary prevention of sudden death, but also on ICD implants for secondary prevention. The number of ablation procedures was markedly reduced and the reduction also affected emergency procedures, especially for centers directly involved in the care of COVID-19 |
| Compagnucci et al. 12 | Italy | Retrospective cohort | CIED placement EPS |
592 | 100 | 83.1 | Not reported | The data reinforce the concept that COVID-19 can have major direct as well as indirect effects on the practice of electrophysiology |
| Elliot13 | New Zealand | Retrospective cohort | CIED | 127 | 114 | 10.2 | Not reported | The fall in total EP procedures was largely due to reduced elective volumes. The number of in-patient EP procedures has remained relatively constant throughout the lockdown |
| Fersia et al. 14 | UK | Retrospective cohort | CIED | 71 | 28 | 60.5 | Not reported | This UK single-center experience showed that the COVID-19 pandemic has led to a significant reduction in all sections of cardiology service, particularly the intracardiac devices and EP procedures |
| Li et al. 15 | Multicenter (Italy, UK, China) | Retrospective cohort | CIED EPS VT/AF ablation |
Milan (Italy): 26.3 week London (UK): 15.1 week Wenzhou (China): 25.3 |
All centers: 0.85 week | Milan (Italy): 96.7London (UK): 94.3 Wenzhou (China): 96.6 |
Wenzhou (China): 20.6 week | Interventional electrophysiology is vulnerable to closure in times of great social difficulty including the COVID-19 pandemic. Intense public health intervention can permit suppression of local disease transmission allowing resumption of some normal activity with stringent precautions |
| Mazzone et al. 16 | Italy | Retrospective cohort | CIED EPS VT/AF ablation Lead extraction LAAC |
953 | 79 | 91.7 | Not reported | Only urgent EP procedures, including ventricular tachycardia ablation and extraction of infected devices, were both maintained and optimized to meet the needs of external hospitals. In addition, most of the nonurgent EP procedures were postponed. Finally, following prompt internal reorganization, both out-patient clinics and on-call services underwent significant modification, by integrating telemedicine support whenever applicable |
| Pothineni et al. 17 | USA | Retrospective cohort | CIED EPS VT/AF ablation |
EPS: 781 CIED: 896 |
EPS: 158 CIED: 475 |
EPS: 80 CIED: 47 VT: 59 AF: 83 |
Not reported | A strong inverse relationship between regional EP procedure volume and the surge in COVID-19 cases was observed. In addition to physician practice variations, patient avoidance of medical care may have also affected EP case volume similar to the reduction seen in ST-elevation myocardial infarction interventions |
| Rao et al. 18 | USA | Retrospective cohort | EPS | 380 | 68 | 82 | Not reported | Same-day discharge after PCI, pacemakers, ICDs, and routine ablation was encouraged. These have been shown to be safe, preferred by patients, and cost saving. Adoption of 7-day a week model facilitated capability to perform all necessary procedures even on the weekend and reduce length of stay |
| Satomi et al. 19 | Japan | Retrospective cohort | CIED EPS |
EPS: 4318 CIED: 1832 |
EPS: 3671 CIED: 1550 |
EPS: 8CIED: 15.3 | EPS: 4638 CIED: 1570 |
Physicians should determine the indication for an elective EP procedure while considering three principle factors: (1) the regional burden of the COVID-19 pandemic, (2) the PPE supply level, and (3) severity of the arrhythmias |
| Shahabi et al. 20 | Iran | Cross-sectional survey | CIED EPS |
EPS: 55 CIED: 48 |
EPS: 11 CIED: 10 |
CIED and EPS: 80 | Not reported | Based on the results of the present study and other surveys, COVID-19 pandemic decreased the numbers of referred patients with cardiac problems for EPS or intracardiac device implantation to hospitals as patients/medical staff fearing to infect of COVID-19 and/or low willingness of the healthcare system to provide these services |
| Ali21 | Pakistan | Retrospective cohort | CIED | 250 | 168 | 32.8 | Not reported | A marked reduction in the number of patients who presented for emergency intra cardiac devices and PPM procedures was seen during COVID-19 lockdown. The patients who presented from outside the city of the hospital and women in rural setting were significantly more effected |
| Arbelo et al. 22 | Spain | Retrospective cohort | CIED | 250 month | 131 month | 56.5 | Not reported | During the first wave of the COVID-19 pandemic, a substantial decrease in CIED implantations was observed in Catalonia |
| Bechlioulis23 | Greece | Retrospective cohort | CIED | Before first lockdown: 70 Before second lockdown: 146 |
After first lockdown: 56 After second lockdown: 50 |
First lockdown: 20Second lockdown: 65.7 | Not reported | It is evident that during the first wave of COVID-19 pandemic (February 2020–April 2020) a marked decrease of hospital visits and admissions for EP procedures were noted, although emergency pacemaker implantations were not significantly affected in many centers |
| Budrejko et al. 24 | Poland | Retrospective cohort | CIED EPS |
932 | 971 | 4increase | Not reported | Effort made to restore and further sustain the numbers of electrotherapy procedures throughout the first pandemic year, brought a result that only a few would have predicted in early 2020, that is the maintenance of high volume in most electrotherapy procedures, as supported by the above analysis |
| Konig25 | Germany | Retrospective cohort | CIED EPS |
CIED: 5826 EPS: 4481 |
CIED: 5391 EPS: 4039 |
CIED: 7EPS: 10 | Not reported | A significant performance deficit for all studied cardiovascular interventions was found in this study |
| Pescariu et al. 26 | Romania | Retrospective cohort | CIED | Not reported | Not reported | DM: 81.8Non-DM: 79.3 | Not reported | COVID-19 pandemic determined a dramatic decrease of intracardiac devices related procedures, which were mostly limited to emergency pacemaker implantations. Diabetic patients which are predisposed to develop dilated cardiomyopathy and/or cardiac arrhythmias, requiring more frequently and at a younger age therapy based on intracardiac devices, were particularly affected by the reduction of elective cardiovascular procedures during the COVID-19 pandemic, and that, because of the fear of infection with SARS-CoV-2 virus, they avoided medical services and/or ignored their symptoms |
| Sezenoz27 | Turkey | Retrospective cohort | CIED EPS |
CIED: 762 EPS: not reported |
CIED: 677 EPS: Not reported |
CIED: 11.1EPS: 22.2 | Not reported | The study showed that the EP procedures were significantly affected by the outbreak. The pandemic created an unprecedented clinical scenario |
| Wranicz et al. 28 | Poland | Retrospective cohort | CIED EPS |
841 | 742 | 11.7 | Not reported | The total number of selected electrotherapy procedures in the first quarter of 2020 was similar to the quarterly mean value for 2019 (742 vs. 841. Conversely, the number of procedures performed in the second quarter of 2020 was lower than the quarterly mean value for 2019 |
| Ferrari et al. 29 | Italy | Retrospective cohort | CIED | 42 | 9 | 80 | Not reported | The impact of COVID-19 on the number of procedures performed has been dramatic: there was a reduction of about 80% during the first semester of 2020 if compared to 2019 |
| Barbhaiya et al. 30 | USA | Retrospective cohort | AF ablation | 200 | 111 | 44.5 | Not reported | There was marked reduction of AF ablations in COVID-19 era and the findings demonstrate the feasibility of safe resumption of complex electrophysiology procedures during the COVID-19 pandemic, reducing healthcare utilization and maintaining quality of care |
| Ding et al. 31 | UK | Retrospective cohort | EPS | Not reported | Not reported | 52.2 | Not reported | The COVID-19 pandemic has had a significant impact on EP services at specialist centers in the UK. The number of procedures performed was greatly reduced in the initial period with latter improvements as better coping strategies were developed. However, the waiting lists for both EP and device procedures have continued to rise steadily |
CIED, cardiac implantable electronic device; COVID-19, coronavirus disease 2019; EP, Electrophysiology; EPS, electrophysiology studies; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2.
Search strategy/Selection criteria
Various databases, including PubMed/MEDLINE, Scopus, Web of Science, CINAHL, and Embase were examined with combinations of medical subject headings (MeSH) terms for identification of the relevant studies. There were no time or language restrictions on the inclusion criteria, and to find the relevant articles, references of the included studies and reviews were performed to extract unidentified articles skipped in the primary search. The medical subject headings consisted of the following sets: ‘electrophysiology’ OR ‘EP’ OR ‘cardiac electrophysiology’ OR ‘electrocardiology’ AND ‘COVID-19’ OR ‘SARS-CoV-2’ OR ‘pandemic’ AND “procedures’ OR‘procedure volume’ OR ‘radiofrequency ablation’ OR ‘pacemaker’ OR ‘permanent pacemaker’ OR ‘cardiac implantable electronic device’. All the sets were systematically combined using the Boolean operators, and the results from all the combinations were extracted into the Covidence library.
The documents were then reviewed by two independent investigators (J.M. and S.M.J.Z.) for titles and abstracts in the initial search. Articles that reported EP procedure volumes before and during COVID-19 were included in the review. All randomized controlled trials, observational studies, and research letters were included. All preprints, conference papers, and studies with no previous procedural data were excluded from the analysis. The first author validated all the data; in the case of missing information, the authors of the original article were contacted. The last search ended on 7 July 2022, and the search strategy is shown in Figure 1.
Figure 1.
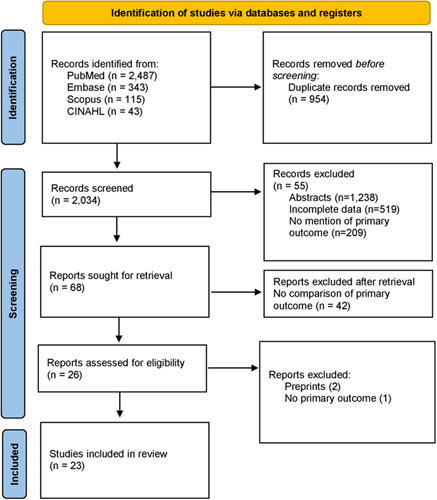
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Data extraction/Analysis
The data about CIED placement, EPS, or any other EP-related procedures were extracted independently by the two authors (J.M. and T.A). Detailed study-level baseline characteristics, including the type of study, sample size, country, and the number of procedures pre-COVID-19 were abstracted. Finally, any predictors or conclusions were extracted for each article.
The statistical analysis was executed through the Statistical Package for Social Sciences version 26 (IBM Corp.). The data were presented as mean and SD for continuous variables and frequency (n) and percentages (%) for categorical variables.
Quality assessment
The overall methodological quality was not an exclusion criterion for this review, and the Newcastle–Ottawa scale was used for assessing the nonrandomized studies32. These are presented in Figure 2.
Figure 2.
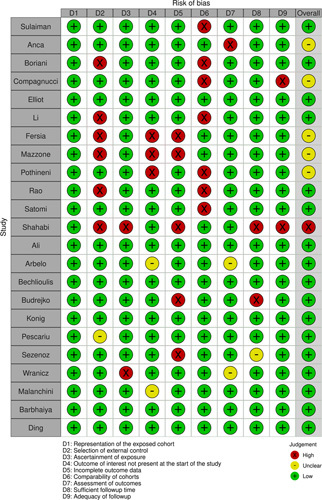
Quality assessment (Newcastle–Ottawa scale).
Results
The initial search revealed 2988 articles. After removing duplicates (954) and irrelevant studies (1966), 68 were screened for full-text review. Of these, 45 studies were excluded based on the inclusion criteria. A total of 23 studies qualified for the final qualitative analysis4,10–31. A total of 4 studies were from the United States of America, 14 from Europe, and 1 from Pakistan, Oman, Iran, Japan, and New Zealand. Most of the studies were from high-income countries with just two studies from middle-low-income countries20,21. All of the included studies were retrospective cohorts except for two cross-sectional surveys11,20. All studies were published between 2020 and 2022.
The overall study-level volume reduction of EP procedures ranged from 8 to 96.7%. All studies reported an overall reduction in EP physiology procedures being carried out except one24 in Poland, which reported an overall increase in the total EP procedures carried out in 2020. This study still reported a decrease in EP procedure volume during the first lockdown phase.
There was heterogeneity in procedure volume reduction and detailed procedure types carried out at different centers of the world with the most common ones being CIED placement (20/23 studies, 86.9%), EPS (11/23 studies, 47.8%), and ablations (9/23, 39.1% studies). The most common reason stated for the observed decline in EP procedures was the cancellation and postponement of nonurgent elective cases in the hospitals (15/23 studies, 65.2%). Seven (30.4%) studies reported their hospitals/centers being converted into COVID-19 referral centers4,10,14–16,18,19. Six (26.1%) studies reported an inverse relationship between rising COVID-19 cases and the declining rates of EP procedures11,17–20,27. Organizational restructuring in response to the pandemic and the issuance of new guidelines for EP procedures were reported in nine (39.1%) studies4,10,14–17,19,29,30.
An estimated 19 124 EP procedures were carried out during the COVID-19 pandemic in all studies compared to 24 916 EP procedures carried out before the pandemic. Nineteen studies reported pre-COVID-19 data on EP procedures being carried out in tertiary level care centers4,12–18,20,22–31. Only one study reported data on postCOVID EP procedure volumes15. Only two studies reported any EP procedures carried out on COVID-19 positive cases4,16. Only two studies reported any kind of mortality due to EP procedures carried out during the pandemic4,15. A total of seven fatalities were reported in these two studies of which three were due to COVID-19. Two studies showed an increase in ventricular tachycardia (VT) ablation rates despite a decline in other EP procedures27,28. One study from Pakistan elaborated on gender and regional disparities in emergency EP procedures documenting a five-fold reduction in-patient volume in centers outside the main city as well as a decrease in the number of women attending the facilities. Although another study from Iran reported no significant difference in EP practice based on sex20. One study19 reported worsened patient outcomes due to the postponement of EP procedures. One study showed the impact of postponement on cardiac rhythm management waiting lists during the pandemic31.
Discussion
In this systematic review, we report the effect that the COVID-19 pandemic had on EP procedure volumes throughout the world. A decrease in all kinds of EP procedures was observed in all studies (n=23) included in this systematic review, except one24 which shows a uniform decline in EP practice throughout the world. The most common reason for this decline was the cancellation or postponement of nonurgent elective EP procedures as a result of organizational restructuring to shift healthcare services towards battling the rising COVID-19 cases in the region. This restructuring of healthcare services was reported in nine (39.1%) studies included in this systematic review. In light of the COVID-19 pandemic and the burden placed on healthcare service delivery, the American College of Cardiology and Heart Rhythm Society released a statement to guide hospitals/healthcare systems in better managing heart rhythm disorders amidst the rising COVID-19 cases. The statement recommended triaging all EP procedures into three categories: urgent, semi-urgent, and nonurgent. The guidelines recommended postponing all urgent/elective cases to decrease patient exposure to infection as well as to better utilize hospital resources towards battling the pandemic33. This restructuring and cancellation of elective procedures might not be the sole reason for the decline in procedure volume and the actual cause might be multifactorial. Nine studies reported an inverse relationship between COVID-19 cases and EP procedure volumes in their hospitals, which also shows the negative impact of the pandemic on electrophysiology service delivery. Seven studies reported their facilities being turned into COVID-19 referral centers, in which cases electrophysiologists and staff involved in cardiac care were re-routed to help in providing care for COVID-19 patients. This shows how healthcare systems adapt to a global public health emergency. Only two studies reported any kind of mortality among patients who underwent EP procedures, of which three deaths were due to COVID-19 infection.
One study conducted in Pakistan that analyzed data regarding EP procedures from 10 hospitals in one province reported regional and gender disparities in emergency arrhythmia procedures among people living outside urban areas, rural cities, and women being disproportionately affected than those living in urban cities21. This indicates how socially and economically disadvantaged populations can be disproportionately affected by the measures applied to combat a global public health emergency and special attention should be placed on these groups in the wake of a pandemic. The impact COVID-19 had on socially and economically disadvantaged communities have been seen in several studies that report communities with low income living in deprived areas and of certain ethnic backgrounds have an increased risk of COVID-19-related death compared to the general population34. Two studies27,28 reported an increase in VT ablation procedures despite an overall decline in EP procedure volume. This may be because ventricular tachycardia is a life-threatening condition, and hence VT ablation procedures were undertaken as a matter of priority and classified as urgent non-deferrable cases. These studies; however, did not provide concrete evidence for this reasoning to be established.
The pandemic placed immense strain on the healthcare systems throughout the world; hospitals had to focus their resources on managing the influx of COVID-19 patients, which impacted the delivery of care to other patients. Elective/nonurgent cases were postponed to decrease the load on hospital resources, that is, personal protective equipment, etc. and to lower the risk of infection transmission as well. Telemedicine services were utilized for triaging patients, remote patient monitoring, chronic disease management, and much more thus reducing the risk of infection transmission while still providing healthcare services35. Along with this, the hospital staff was redeployed to COVID-19 ICUs and emergency rooms and some electrophysiologists even served as backup consultants during the time of this emergency4. This restructuring of healthcare services provided us with the resources as well as the manpower to handle the peaks of the pandemic. In addition, the measures enforced by governments throughout the world, including mandatory confinements, strict lockdowns, closing out-patient services, and limiting intercity and international travel all lead to a marked decline in the influx of patients to healthcare centers. It might also be possible that the fear of acquiring the contagion also prevented patients from seeking healthcare. Many other healthcare services also saw a considerable decline during the pandemic, the reasons behind which may be multifactorial and similar to the ones behind EP procedures. A decrease has been reported in ST-segment elevation laboratory activities in the USA36 as well as a reduction in hospitalization rates for acute myocardial infarction in Italy37. A similar decline has also been seen in oncology services in many centers throughout the world38,39.
Only time will tell about the actual impact of this decline in health-service delivery, but it is still safe to assume that these services will be resumed to prepandemic levels after this public health emergency subsides. Only one study included in this systematic review reported data on postCOVID procedure volumes15 in which electrophysiology centers in Wenzhou were able to resume routine activity close to their previous work rates, albeit with strict precautionary measures for COVID-19 due to stringent public health interventions that controlled the spread of disease. It might also be speculated that the postponement of nonurgent elective procedures might cause a resurgence of EP procedures postpandemic as it was only a short-term strategy and only deferred the burden of disease, which might present at a later time. These patients might even present with adverse health outcomes or emergency life-threatening conditions. One study19 in our review reported that 8.5% of centers to experience adverse patient outcomes as a result of postponing elective procedures. A case–control study that evaluated the effect of deferral of nonemergency cardiac procedures during the pandemic revealed increased emergency early cardiovascular hospitalizations in patients whose elective procedures were deferred during the pandemic compared to the control group40. Subgroup analysis revealed that valvular heart disease patients were particularly susceptible to adverse outcomes. Another effect of deferring elective cases could be an increase in the waiting list for these EP procedures. Another study conducted in the UK31 in our review reported a 67.8% increase in the waiting list for cardiac rhythm management services as compared to prepandemic levels, which would require almost 3 years to clear this backlog alone. This effect might also be seen in other elective healthcare services that were postponed during the pandemic41,42. This increase might prolong the waiting times for EP services postpandemic, which will require strategies to manage the patient load efficiently once services are resumed.
A valuable lesson from the COVID-19 pandemic is that healthcare systems across the world need to adopt strategies and develop preparedness for future pandemics. Several studies have demonstrated exemplary adaptation to the challenges in EP practice in this public health crisis. While some modified procedures and recovery areas to accommodate SARS-CoV-2 positive patients, taking strict precautions regarding cleanliness and disinfection, abiding by triage guidelines, and utilizing telemedicine2, others even devised their case prioritization schemes19. The decline in emergency, lifesaving procedures can and must be addressed by ensuring the availability of personal protective equipment and the service of SARS-CoV-2 testing to limit the spread of infection. Strict adherence to COVID-19 protocols can prevent postprocedural COVID-19 infections in both patients and staff amidst marked local COVID-19 prevalence. The practice of postprocedural same-day discharge wherever possible and virtual follow-up decreases the duration of hospital stays and provides adequate care to patients30.
Limitations
Our review has certain limitations. First, the studies included were retrospective in nature, and data were recorded for administrative rather than research purposes. There is always a chance of bias in the form of incorrect coding and entry of procedures and diagnoses. Most comparisons were made only between pre-COVID 2019 and the pandemic peak in 2020, which means outcomes could have been caused by year-dependent fluctuations in admission numbers. Furthermore, the survey methodology used in two of the included studies is subject to recall and selection bias.
Conclusion
There has been an overall reduction in EP procedure volume across different centers. Postponement of nonurgent electrophysiology procedures was the main reason behind the decline in procedure volumes. An inverse relationship was reported between COVID-19 cases and EP procedure volumes. Very little data was reported on mortality during EP procedures carried out during the pandemic. The impact of the decline in EP procedures will be seen only after the services resume to prepandemic levels, but an increase in-patient volume and procedure waiting times is expected. This review will provide insights into improving healthcare service delivery in times of unprecedented public health emergencies.
Ethical approval
NA.
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
The authors received no specific funding for this manuscript.
Author contribution
T.A., A.K.A., H.A., R.A., H.I.: first draft, methodology, final draft; S.M.J.Z.: first draft, methodology, final draft; S.M.J.Z., J.M., T.A.: supervision; M.A., M.E., A.A.K., M.N., S.H.: literature review; M.N.R., M.A., J.Z.: first draft, concept, methodology.
Conflicts of interest disclosure
The authors declare that they have no competing interests.
Research registration unique identifying number (UIN)
Name of the registry: NA.
Unique Identifying number or registration ID: NA.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NA.
Guarantor
Talal Almas, RCSI University of Medicine and Health Sciences, 123 St. Stephen’s Green, Dublin 2, Ireland. E-mail address: talalalmas.almas@gmail.com
Provenance and peer-review
Not commissioned, externally peer-reviewed.
Footnotes
Talal Almas and Maryam Ehtesham contributed equally to the manuscript and are joint first authors.
Published online 27 March 2023
Contributor Information
Talal Almas, Email: talalalmas.almas@gmail.com.
Maryam Ehtesham, Email: maryamehtesham@rcsi.com.
Alishba A. Khan, Email: alishba.ashraf.98@gmail.com.
Rahul K. Ramtohul, Email: rahulramtohul@rcsi.com.
Maheen Nazir, Email: maheennazir32@gmail.com.
Syed M. J. Zaidi, Email: mjawad927@gmail.com.
Abdulla K. Alsubai, Email: alsubaiabdulla@gmail.com.
Haya Al-Ansari, Email: haa2060@qatar-med.cornell.edu.
Muhammad Awais, Email: awais2007aimc@gmail.com.
Reema Alsufyani, Email: reemaalsufyani@rcsi.ie.
Majid Alsufyani, Email: MajidAlsufyani@rcsi.ie.
Abdulla Almesri, Email: abdullahalmesri@rcsi.com.
Hebatalla Ismail, Email: hebaismail@rcsi.com.
Sebastian Hadeed, Email: sebastianhadeed@rcsi.com.
Jahanzeb Malik, Email: heartdoc86@gmail.com.
References
- 1. Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern. Lancet 2020;395:470–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Palacios Cruz M, Santos E, Velázquez Cervantes MA, et al. COVID-19, a worldwide public health emergency. Rev Clin Esp (Barc) 2021;221:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lakkireddy DR, Chung MK, Gopinathannair R, et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 task force; electrophysiology section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm 2020;17:e233–e241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anca D, Reyes O, Mitra RL, et al. Electrophysiology practice during COVID-19 pandemic: a New York Tertiary Hospital experience. J Cardiothorac Vasc Anesth 2021;35:1281–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jaiswal V, Almas T, Peng Ang S, et al. Symptomatology, prognosis and clinical findings of STEMI as a ramification of COVID-19: a systematic review and proportion meta- analysis. Ann Med Surg (Lond) 2022;76:103429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Almas T, Malik J, Alsubai AK, et al. Post-acute COVID-19 syndrome and its prolonged effects: an updated systematic review. Ann Med Surg (Lond) 2022;4:103995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Almas T, Rehman S, Mansour E, et al. Epidemiology, clinical ramifications, and cellular pathogenesis of COVID-19 mRNA-vaccination-induced adverse cardiovascular outcomes: a state-of-the-heart review. Biomed Pharmacother 2022;149:112843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pothineni NVK, Santangeli P. Electrophysiology, and interventional cardiology procedure volumes during the coronavirus disease 2019 pandemic. Card Electrophysiol Clin 2022;14:105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 10. Sulaiman K, Al Riyami M, Al Riyami A, et al. Short-term impact of the covid-19 pandemic on cardiology service in Oman. Heart Views 2020;21:149–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boriani G, Palmisano P, Guerra F, et al. AIAC Ricerca Network Investigators. Impact of COVID-19 pandemic on the clinical activities related to arrhythmias and electrophysiology in Italy: results of a survey promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Intern Emerg Med 2020;15:1445–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Compagnucci P, Volpato G, Pascucci R, et al. Impact of the COVID-19 pandemic on a tertiary-level electrophysiology laboratory in Italy. Circ Arrhythm Electrophysiol 2020;13:e008774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elliott JM, Crozier IG. Decreases in cardiac catheter laboratory workload during the COVID-19 level 4 lockdown in New Zealand. Intern Med J 2020;50:1000–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fersia O, Bryant S, Nicholson R, et al. The impact of the COVID-19 pandemic on cardiology services. Open Heart 2020;7:e001359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li J, Mazzone P, Leung LWM, et al. Electrophysiology in the time of coronavirus: coping with the great wave. Europace 2020;22:1841–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mazzone P, Peretto G, Radinovic A, et al. The COVID-19 challenge to cardiac electrophysiologists: optimizing resources at a referral center. J Interv Card Electrophysiol 2020;59:321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pothineni NVK, Santangeli P, Deo R, et al. COVID-19 and electrophysiology procedures-review, reset, reboot!!! J Interv Card Electrophysiol 2020;59:303–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rao G, Singh A, Gandhotra P, et al. Paradigm shifts in cardiac care: lessons learned from COVID-19 at a large New York health system. Curr Probl Cardiol 2021;46:100675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Satomi K, Watanabe E, Takatsuki S, et al. Statement for electrophysiological procedures under the COVID-19 pandemic from the Japanese heart rhythm society task force. J Arrhythm 2020;36:1117–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shahabi J, Askari M, Azhari A, et al. The survey of electrophysiology lab activity during the COVID-19 pandemic. J Arrhythm 2021;37:899–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ali PS, Mansoor S, Shafquat A. gender and regional disparities in emergency arrhythmia procedures during COVID-19 lockdown. Pak Heart J 2021;54:344–347. [Google Scholar]
- 22. Arbelo E, Angera I, Trucco E, et al. Reduction in new cardiac electronic device implantations in Catalonia during COVID-19. Europace 2021;23:456–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bechlioulis A, Sfairopoulos D, Korantzopoulos P. Impact of COVID-19 pandemic on cardiac electronic device implantations in Northwestern Greece. Am J Cardiovasc Dis 2021;11:489–493. [PMC free article] [PubMed] [Google Scholar]
- 24. Budrejko S, Kempa M, Królak T, et al. Procedural volume of cardiac electrotherapy procedures does not have to be reduced during COVID-19 pandemic - one year analysis from a tertiary Polish center. Kardiol Pol 2021;79:848–850. [DOI] [PubMed] [Google Scholar]
- 25. König S, Ueberham L, Pellissier V, et al. Helios hospitals, Germany. Hospitalization deficit of in- and outpatient cases with cardiovascular diseases and utilization of cardiological interventions during the COVID-19 pandemic: insights from the German-wide helios hospital network. Clin Cardiol 2021;44:392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pescariu SA, Tudoran C, Pop GN, et al. Impact of COVID- 19 pandemic on the implantation of intra-cardiac devices in diabetic and non-diabetic patients in the western of Romania. Medicina (Kaunas) 2021;57:441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sezenöz B, Ateş AH, Yorgun H, et al. The impact of COVID-19 outbreak on electrophysiological procedures: a single-center tertiary experience. Eur J Ther 2022;28:52–56. [Google Scholar]
- 28. Wranicz JK, Dróżdż J, Różycka‐ Kosmalska M, et al. Impact of the COVID-19 pandemic on the performance of selected cardiac electrotherapy and electrophysiology procedures. Kardiol Pol 2021;79:452–454. [DOI] [PubMed] [Google Scholar]
- 29. Ferrari P, Malanchini G, Malacrida M, et al. Experience of a pediatric electrophysiology clinic during the COVID-19 pandemic. J Arrhythm 2022;38:446–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Barbhaiya CR, Wadhwani L, Manmadhan A, et al. Rebooting atrial fibrillation ablation in the COVID-19 pandemic. J Interv Card Electrophysiol 2022;63:97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ding WY, Cranley J, Begley D, et al. Impact of COVID-19 pandemic on cardiac rhythm management services: views from the United Kingdom. Heart Rhythm. O2 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–605. [DOI] [PubMed] [Google Scholar]
- 33. Lakkireddy DR, Chung MK, Gopinathannair R, et al. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 task force; electrophysiology section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Circulation 2020;141:e823–e831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lauvrak V, Juvet LK. Social and economic vulnerable groups during the COVID-19 pandemic. Norwegian Institute of Public Health; 2020.
- 35. Bahl S, Singh RP, Javaid M, et al. Telemedicine technologies for confronting COVID-19 pandemic: a review. J Indust Integ Manag 2020;5:547–561. [Google Scholar]
- 36. Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. De Rosa S, Spaccarotella C, Basso C, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J 2020;41:2083–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ranganathan P, Sengar M, Chinnaswamy G, et al. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021;22:970–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Graetz D, Agulnik A, Ranadive R, et al. Global effect of the COVID-19 pandemic on paediatric cancer care: a cross-sectional study. Lancet Child Adolesc Health 2021;5:332–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Andreß S, Stephan T, Felbel D, et al. Deferral of non-emergency cardiac procedures is associated with increased early emergency cardiovascular hospitalizations. Clin Res Cardiol 2022;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Uimonen M, Kuitunen I, Paloneva J, et al. The impact of the COVID-19 pandemic on waiting times for elective surgery patients: a multicenter study. PLoS One 2021;16:e0253875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. García-Rojo E, Manfredi C, Santos-Pérez-de-la-Blanca R, et al. Impact of COVID-19 outbreak on urology surgical waiting lists and waiting lists prioritization strategies in the post-COVID-19 era. Actas Urol Esp (Engl Ed) 2021;45:207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]


