Abstract
Background
Peer coaching interventions are effective in helping individuals with chronic conditions understand their disease. Most peer coach training programs occur in person, which has become an obstacle during the COVID pandemic. We describe our experiences with virtual training for future peer coach interventions.
Methods
Individuals with rheumatoid arthritis (RA) between 40 and 75 years of age were recruited and interviewed by the research team. We conducted seven virtual training sessions focused on four main points: Listen, Discuss, Practice, and Certify. The peer coaches provided feedback throughout the program, which was used to refine the training and intervention. A post-training focus group assessed satisfaction with the training program and intervention development process.
Results
Four peer coaches (3 women, 1 man) were trained, including 2 Black and 2 White individuals with advanced degrees. Their ages ranged from 52 to 57, and their RA duration ranged from 5 to 15 years. An iterative process with the coaches and researchers resulted in a nine-week training program. Peer coaches reported satisfaction, confidence, and a preference for the virtual training format.
Conclusion
This virtual peer coach training program was feasible and acceptable for coaches with advanced degrees during the global COVID-19 pandemic. Our approach represents an opportunity to adapt training that has been traditionally done in person. By doing so, our approach facilitates the recruitment and training of a diverse group of coaches and promotes sustainability.
Keywords: Motivational interviewing, Peer coaching, Training, Cardiovascular risk disease, Rheumatoid arthritis
1. Background
A patient's level of health literacy can influence behavior change and engagement in care. Patients often require a high level of health literacy to be involved in their care, but a high level of health literacy is difficult for patients to achieve [1]. Role modeling has been used to achieve behavior change [2,3], and peer coaches are one way role modeling has been operationalized for successful behavior change in diseases such as diabetes, HIV, and asthma [[2], [3], [4], [5], [6], [7]]. Peer coaches are lay individuals that have a targeted condition and coach another person with the same condition to achieve a particular goal [8,9]. This includes a change in treatment adherence, conflict resolution with initiating therapies, or other disease-specific management goals [[9], [10], [11], [12]].
Patients with rheumatoid arthritis (RA), a chronic autoimmune and inflammatory condition, have a 50–60% increased risk of mortality from cardiovascular disease (CVD) compared to the general population [[13], [14], [15], [16], [17], [18]]. Despite excess CVD risk, risk assessment remains suboptimal in this population, highlighting the need for interventions to implement evidence-based preventive CVD guidelines into clinical practice [19,20]. One challenge in patients with RA is that many physicians are not aware of the excess CVD risk in this population or are conflicted on who should manage it [21,22]. A systematic review on interventions for CVD prevention reported that multilevel interventions focusing on providers, patients, and systems were the most effective compared to those that focused only on physicians [23]. This could be because physicians’ behaviors are difficult to change, which has been reported extensively in the medical literature [24].
While multilevel interventions can be complex and costly, an innovative way to change physicians' behaviors is through patients. A study observed that patients who asked for a treatment for depression were nearly eight times as likely to receive a prescription for an antidepressant medication compared to patients who made no request [25]. Therefore, an intervention focused on activating patients with RA to obtain a CVD risk assessment has the potential to change physicians’ behaviors and have the effect of a multilevel intervention while targeting only patients.
In our prior work, patients with RA expressed interest in working with peer coaches if they were knowledgeable, good communicators, and endorsed by their doctors [26,27]. Therefore, to ensure the success of interventions using peer coaches for patients with RA, we need to ensure that peer coaches are proficient in the concepts of the evidence-based intervention and in their communication skills. Peer coach interventions require coaches to obtain a minimum proficiency level in the intervention content and motivational interviewing (MoI) skills. MoI is an evidence-based counseling approach used to enact behavioral change through an interventionist-participant partnership centered around acceptance, compassion, and evocation [28]. Many peer coach training programs teach MoI skills using at least one in-person training session that allows trainers to observe learners and facilitates immediate reinforcement of skills [29]. The global COVID-19 pandemic poses challenges to in-person MoI training and adds barriers to training immunocompromised individuals with physically debilitating chronic conditions such as RA. Therefore, virtual training in MoI would be helpful for vulnerable patients who want to become peer coaches, but only if virtual training results in competency in MoI skills.
We developed the CArdiovascular Risk assEssment for patients with RA (CARE RA) program to be delivered by peer coaches. Given the circumstances of the COVID-19 pandemic, trained the CARE RA peer coaches on MoI virtually. This process modeled a training approach developed by one of the research team members [30]. The objectives of this paper were to (1) describe our approach to virtual training of peer coaches in the CARE RA intervention, and (2) describe the infrastructure for virtual MoI training that can be applied to training peer coaches in future interventions.
2. Methods
The CARE RA randomized controlled trial (RCT) protocol has been described elsewhere [31]. In summary, the CARE RA program is an ongoing RCT pilot planning to enroll 128 patients with RA. The intervention arm is allocated to receive the CARE RA program from a peer coach, and the control arm is allocated to work through the CARE RA curriculum without the guidance of a peer coach (Supplement 1). This study describes the methodology of training the peer coaches for the intervention arm of the CARE RA program.
The research team interviewed peer coach candidates between July 2020 and September 2020 from ArthritisPower. ArthritisPower is a patient-powered research network (PPRN) that connects people with RA to resources, research groups, and other people with RA [32]. Potential peer coaches were referred to the research team based off of the peer coach inclusion criteria [31]. The inclusion criteria consisted of peer coaches that have had a leadership role within ArthritisPower, were between 40 and 75 years of age, English-speaking, and had recently had a CVD risk assessment or were willing to receive a CVD risk assessment during training.
Referred individuals were interviewed by the principal investigator and the CARE RA research team. Candidates were asked questions about their background, interest in research, experience with volunteering, prior leadership roles, interest in helping others living with RA, and interest in the topic of CVD and RA. Candidates were also informed of the rationale for the CARE RA program, the anticipated time commitment (28 h), and the schedule of the training program. The research team also notified the candidates of the $500 stipend for completing the training program and additional $100 for each client that they walked through the intervention.
The research team selected candidates with prior research and volunteer experience. This was done under the assumption that individuals with these experiences would be highly committed to the study—avoiding dropouts—and creating a role model for participants of the CARE RA program. To qualify, coaches were selected based on their availability to commit the time to the program during training and recruitment. Selected individuals were notified through email emailed and a follow-up meeting was scheduled between to review the contract, training schedule, and onboarding materials. Once all the contacts were signed the first training session was scheduled. Candidates who had not received a CVD risk assessment were able to receive a CVD risk assessment during training.
Peer coach training was conducted through an online conference platform (Zoom) and recorded. All the peer coaches completed the Collaborative Institutional Training Initiative (CITI) Good Clinical Practice (GCP) training on the responsible conduct of research with human subjects.
2.1. Overview of CARE RA
CARE RA is an evidence and theory-based behavioral intervention aiming to increase CVD risk assessment among people with RA [13,33,34]. CARE RA is a 5-session curriculum (Supplement 2) using educational materials on the Patient Activated Learning System (PALS) website (www.palsforhealth.com). This novel, publicly available education platform was developed at the Weill Cornell Medicine Division of General Internal Medicine and the University of Alabama at Birmingham. It is based on Adult Learning Theory and Bandura's Social Cognitive Theory [35,36]. The PALS was designed to provide engaging, easily understood, and well-researched facts for people who want to know more about health, medicines, and diseases [37]. The content in the PALS is evidence-based and peer-reviewed and is translated into patient-facing text, aiming for a 6th-grade reading level. Content is accompanied by visuals or short videos to reinforce the concepts.
2.2. Training content
Peer coaches provided demographic information and completed a 10-question MoI and CVD knowledge questionnaire (Supplement 3) before training. They also watched two educational videos about MoI skills to prepare them for training [38,39]. MOI uses 4 main concepts – Open-Ended Questions, Affirmations, Reflective Listening, and Summarizing (O.A.R.S.). O.A.R.S. provides a set of skills that have been shown to be effective in eliciting a participant's internal motivations to change. One investigator (MMS) had experience with MoI and training peer coaches and oversaw the MoI training procedures [9,30,31,40,41].
Peer coaches received a manual and activity book for training. The manual guided the coach through the intervention delivery and included scripts for each session. The clients use the activity book to go over the content of the intervention with their peer coach. Before each training session, peer coaches reviewed the manual and activity book, and listened to a mock session recording.
2.3. Training schedule
The training consisted of nine sessions. The first session introduced peer coaches to concepts like privacy and confidentiality, the training schedule (Supplement 4), and the CARE RA program schedule (Supplement 5). Sessions two, three, four, six, and eight covered four main points: Listen, Discuss, Practice, and Certify (Supplement 6). Sessions four and seven were MoI sessions between two peer coaches. Session nine reinforced points from week 1 and reviewed the client matching and communication protocol. Training sessions lasted 1 h and began with a 15-min PowerPoint presentation outlining the objectives and agenda for the session. The rest of the sessions consisted of experiential training and the four main points.
2.3.1. Listen
Peer coaches listened to two 5-min audio recordings of a mock conversation between a peer coach and a challenging interaction with a client. Supplement 7 contains several examples of challenging scenarios. The first recording portrayed a peer coach that responded inadequately to their client's needs. The second recording highlighted an ideal response from the peer coach to the same client using elements of O.A.R.S.
2.3.2. Discuss
We moderated a discussion in which peer coaches identified differences between the recordings for 10 min. Coaches were asked to point out specific instances of the use of O.A.R.S., where these skills could be incorporated, and what aspects of the conversation between the peer coach and the client were adequate or needed improvement and in which way.
2.3.3. Practice
Peer coaches were paired and placed in small groups with at least one research team member to role-play for 20 min. One peer coach practiced being the peer coach first, while their partner acted as the client. Before beginning their practice session, peer coaches were asked to turn off their cameras. A prompt was provided to describe the background of the mock client. Each peer coach was given 10 min to practice with their partner after which they were provided with verbal feedback from the research team and their partner and then switched roles. At the end of each training session coaches were reminded to practice the session from training with their partner and review next week's content.
2.3.4. Certify
After practicing coaches scheduled a certification session with the research team. Peer coaches delivered the session to a member of the research team with cameras off to mimic the telephone interaction that peer coaches would have with their clients. Peer coaches had to score at least 80% in the corresponding checklist for each session to move on to the next session of training. These checklists served as evaluation and certification of the peer coaches’ proficiency and to ensure standardization of intervention delivery (i.e., fidelity). Supplement 8 includes the week 3 checklist. During certification, peer coaches received verbal feedback with suggestions on how to improve their MoI skills, communication skills, and their proficiency in the content of the session. They were prompted for feedback on the intervention and training materials as well. The checklist was provided to the peer coach after each certification along with a link to the recording of the certification session.
2.4. Motivational interviewing
Peer coaches completed two MoI sessions with a partner. The goal of these sessions was for peer coaches to achieve a high level of competency in the use of O.A.R.S. and rolling with resistance. During the MoI session, the research team reviewed MoI skills, and then peer coaches practiced delivering content to their partner. Peer coaches turned off their cameras during the practice section to mimic the telephone interactions they would experience with the clients. The research team interrupted the interaction when the peer coach faced a challenge or could have used O.A.R.S. The peer coach was provided alternatives on how to approach the situation and repeated that part of the session, incorporating the feedback received. Once one peer coach finished, they would receive verbal feedback and then switch roles. Peer coaches were evaluated using a checklist like those used for certification, however, these evaluations were strictly informative as these sessions were for practice. Peer coaches received an email with both the checklist and a link to the recording of the MoI session.
2.5. Training evaluation
The peer coaches completed a post-survey training evaluation after completing the 9 weeks of training and the post-training MoI and CVD knowledge questionnaire that they completed at baseline. We conducted a focus group with all 4 peer coaches two weeks after completing the training to elicit feedback and to describe their experience of becoming a CARE RA peer coach, the virtual learning, training structure, program materials, and overall training satisfaction. The focus group session was recorded, transcribed verbatim, and analyzed independently by two members of the research team (MCB and YDP). Data were analyzed thematically. The information gained from the discussion group was incorporated into the final training program for future peer coaches.
3. Results
The research team interviewed 6 peer coach candidates, recruited 4, and successfully trained them (3 women, 1 man; 2 Black, 2 White). All completed more than 80% of the evaluation checklist items during training. Peer coaches ages ranged from 52 to 57, with RA duration of 5–15 years. Two coaches needed cholesterol testing and CVD assessment to comply with eligibility criteria. Two had previously been diagnosed with hypertension. All 4 coaches had advanced degrees and backgrounds in counseling, teaching, research, and/or leadership and were located in different US regions.
3.1. Modifications as a result of peer coach feedback
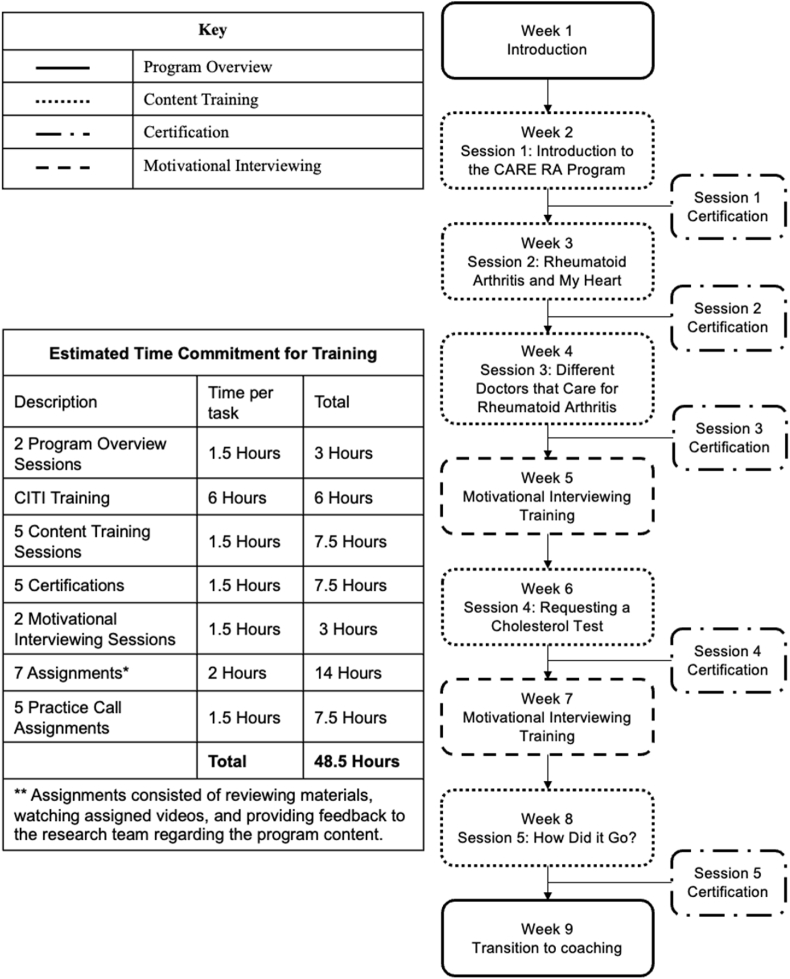
Our original training program had seven weekly sessions for seven weeks. However, peer coaches noted that the training program required more time and effort than they had initially anticipated. Most of their time was taken up by activities outside of the weekly training sessions. These activities included CITI training, program assignments, practicing calls with peer coach partners, certifying in each session with the research team, and completing MoI certification sessions. Although the peer coaches did not find these activities overwhelming, they suggested adding two additional weeks to accommodate their responsibilities. We added two “break weeks” to the training schedule to allow more time for certification, assignments, and MoI sessions (as shown in Fig. 1) and to accommodate scheduling for certification sessions.
Fig. 1.
Care RA peer coach training program schema.
The peer coaches further emphasized the need to shorten the entire intervention, so we reduced the length content in each session from 45 min to 15–20 min. Additionally, the scenarios used for training were changed based peer coach feedback. Instead of dramatizing the participants in these scenarios, peer coaches wanted there to be less difference between ideal and non-ideal ways of delivering sessions. The coaches believed that non-ideal scenarios with subtle differences in communication styles and the use of MoI would be more effective in training future coaches on the discreet applications of MoI skills.
Lastly, peer coaches wanted to take detailed notes on their clients and track their conversations, which led to the creation of a peer coach notebook. Table 1 summarizes the feedback from the peer coaches and the resulting modifications made to the training program and intervention materials.
Table 1.
Summary of major recommendations from peer coaches and resulting changes.
| Summary of Comments | Modifications | |
|---|---|---|
| Intervention Materials | There was not enough space to include client notes in the peer coach manual. | A peer coach notebook was created. One notebook would be used per client and submitted in leu of submitting the manual. |
| Study materials were still in progress during training. | Future interventions should have all study materials near completion before training can begin. | |
| Full length practice sessions outside of training took 45–60 min per peer coach. | Content in the manual was shortened to reduce length per session. | |
| Peer coaches found it difficult to have multiple PDF files opened at once. | A paper copy of the manual, activity book, and notebook were sent to each peer coach. | |
| Intervention Training | One hour training sessions felt rushed. | Training sessions were extended to an hour and a half. |
| Peer coaches learned from watching other peer coaches participate in live role playing of the scenarios during training. | Training sessions consisted of 4–5 coaches reviewing together. | |
| Audio recordings of non-ideal scenarios were perceived as more comedic than informative. | Audio recordings were made more realistic. |
3.2. Satisfaction with training
Peer coaches provided feedback through post-training surveys and discussion groups, as shown in Table 2. They stated that the research team's continuous support and encouragement kept them engaged and motivated, and they felt comfortable making mistakes without fear of judgment. They also expressed feeling included in the research team and appreciated being asked for feedback to refine the intervention. One peer coach's quote exemplified this feeling of inclusion, stating, “The first time I saw the changes that I would suggest added to the materials, I felt like I was creating it too … "
Table 2.
Themes and quotes derived from peer coach feedback.
| Theme | Quotes |
|---|---|
| Training Program | I loved the zoom calls. Not having to travel to the city or other places really worked well for me. Very convenient! |
| … being on Zoom … was actually oddly easier for me to be intensely focused than if we had been in a room together. IT issues were minimal, and the team was always super helpful in resolving those sound issues when they occurred. | |
| In some of the training recordings, the coach was really mean … It would be helpful if you could do a different kind of recording where the coach is not being mean and really trying but getting off the rails doing things that shouldn't be done. | |
| I think using more realistic interactions [in the audio recordings] would be helpful so that you can know when to use the right words and when you're using words that could be challenging to other people. | |
| Maybe allocate an additional 10–15 min for the first couple of sessions because everything is new, and it would allow for more Q/A at the beginning of training. | |
| Overall Training Satisfaction | … I was afraid to bite off too much and look ahead to the content but if I were advising new peer coaches … I would actually suggest they look at the objectives and agenda and even the PALS for all sessions to get a good feel for how it progresses. I did that after session 2 and it helped me tremendously. |
| I think the way we did the testing was very effective because I liked the immediate feedback and the jumping in feedback [practice with commentary]. I heard what I was supposed to do, and it reinforced what I know. | |
| I liked the role playing and I loved when the team jumped in to say, “Wait, think about what just happened. What could you do differently?” and then trying it a different way. That was really helpful on the spot. | |
| … in the bigger rooms you received faster feedback than the small breakouts. When we came back to the big rooms, we were giggling over something and next thing you know our time is up and I still had questions that were unanswered. In the bigger breakout room, you get the immediate feedback, and you can write it down. I felt like I saw different ways of handling situations, and everybody gave their opinions, and it was really spot on. | |
| The more familiar I got with the content the less concerned I was with the words in the script and a better listener I became to what my client was saying. | |
| … stress that this is really going to be demanding. … after the second week I realized, “Oh man, this is really going to be demanding, emotionally and everything." | |
| … I felt like I could ask whatever and make a mistake. It was more like you were just really trying to support us to be the best peer coaches that we could be … |
Peer coaches preferred training using a video conference platform over in-person training because it was less disruptive to their daily lives, did not require travel, and allowed them to focus on training activities outside of the weekly calls. They provided positive feedback on the role-playing aspect of training but expressed a preference of training together in a large group instead of partnered groups. This allowed coaches to watch and learn different ways to approach the same scenario by learning from their peers.
Although training calls were scheduled to last 1 h, we extended subsequent training sessions to 1.5 h after the first three sessions went over time. Coupling the extension of training calls with the addition of two weeks to the training session, peer coaches reported feeling more relaxed and engaged in the training. On average, coaches spent 5–7 h per week on training, totaling 52 h of training – 24 h more than we initially estimated. Despite this, all four coaches completed the program with high satisfaction, engagement, and with the competencies needed to deliver the CARE RA program.
4. Discussion
We successfully virtually trained 4 individuals with RA in concepts of RA, CVD, and MoI. Through the training of these individuals as peer coaches, the research team was able to refine the CARE RA intervention and make it more patient-centered, make the training materials more in line with the priorities of patients with RA, improve the training schedule, and finalize the training program for future training cohorts. In addition, this training structure will be used for the scale-up and maintenance of CARE RA and may apply to other interventions that intend to use peer coaches in the future.
MoI was a key component in our peer coach training program. Usually, the complex components of MoI training are used by trained healthcare professionals or individuals with advanced degrees in healthcare and require many hours of in-person practice to achieve mastery [42]. Previous interventions have trained patient navigators, mentors, or laypeople in MoI to help deliver interventions and achieve behavior change [3,9,43]. One study evaluated the feasibility of an in-person peer coach training program that trained peer coaches over two 4-h training sessions [44]. While the training program was feasible, not all the coach's expressed confidence in their role as a coach and wanted shorter training sessions due to fatigue and difficulty retaining large amounts of material at one time. Another study evaluated the efficacy of virtual MoI training among physical therapists [45]. That study compared two groups; Group 1 watched eight pre-recorded MoI training videos while Group 2 watched the same videos and had one 4-h MoI practice session. Both groups showed improved knowledge and better communication skills, indicating efficacy for virtual MoI training [45]. Although this study was successful in virtual training, it was still among health professionals instead of lay individuals. Due to the global COVID-19 pandemic, the research team's work activities were transitioned to virtual. Hence, the training of the peer coaches for CARE RA could not be conducted in person. Our team proceeded to train peer coaches virtually using an approach like Schechter et al., but we included a more intense practice schedule in MoI [45]. This served to make sure that individuals without formal training in medical evaluations gained confidence in interacting one on one with clients using MoI skills.
In our study, peer coaches felt that incorporating their feedback helped increase their engagement with the program and motivated them to become peer coaches. They expressed communication with the research team made them feel that the program was committed to them. This is like the experience of Community Health Workers (CHW) reported in a study by Andreae et al., where CHWs were trained for an intervention for patients with diabetes to improve physical activity, social support, stress reduction, and healthy eating [30]. A few differences between our training approach and Andreae et al. were that we trained the peer coaches through 9 videoconferences while Andreae et al. conducted a 6-h in-person training followed by 10 telephone conferences [30]. The interventions had different objectives and patient populations as well. In the end, their study led to empowering their CHW, optimizing team functioning and communication, and high intervention fidelity during program implementation [30].
There were several strengths of our study. Our study combined the successes of previous interventions by spending time on both didactic and interactive learning, using individuals with the same chronic condition from various geographical locations, and engaging peer coaches in content development [30,40,45]. This allowed the research team to co-create an intervention with the patients to guarantee patient-centeredness. Our training approach addresses the challenges other studies faced by using virtual training, with over 75% of the training focusing on practice through role-playing. The virtual aspect of training eliminated some of the challenges of in-person training, such as commute and limitations of geographical peer coach selection. Thus, providing us with a diverse cohort in terms of location, background, and lived experiences with RA. Additionally, the video conference platform was invaluable as the complexities of MoI training inhibit it from being taught telephonically. The emphasis on learning through role-playing allowed for engaging training sessions and provided the peer coaches the ability to learn through observation. All peer coaches supported the use of role-playing and felt that it was an invaluable piece of the training curriculum.
This study had two limitations. First, only four peer coaches were trained, which made it challenging to determine whether the changes made to training would be effective for most patients with RA. However, this small group of participants allowed for a more individualized training program that could serve as a model for training of future cohorts peer coach training either for CARE RA and other interventions. . Second, we recognize that the selected group of individuals with advance degrees and prior experience in research could present a limitation for the candidates for becoming peer coaches in future studies. . However, the feedback and modifications that the peer coaches made to the training and intervention alongside the research team simplified the peer coaching training procedures significantly. While we cannot guarantee that this training will be suitable for individuals with non-advanced degrees, our approach is simple, feasible, and can be highly desirable for investigators aiming to broaden their pool of peer coach candidates to select from and to avoid limiting their selection to a single region or community.
5. Conclusion
Virtual training of peer coaches provided a form to reach an ethnically and geographically diverse population of peer coaches to deliver an intervention across multiple states in the US. While our final virtual training can be widely disseminated, desirable qualities among peer coaches candidates should include having an advance degrees or experience equivalent to an advance degree, strong communication skills, and prior volunteer experience.
Funding
This work was supported by INM's K23AR068449 award from NIAMS.
Author disclosures
INM has received an honorarium from the advisory board of Sweden Orphan Biovitrum (SOBI).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
Authors would like to thank Shilpa Venkatachalam and Ben Nowell from Arthritis Power for their support in identifying peer coaches for the CARE RA program.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2023.101130.
Appendix A. Supplementary data
The following is the supplementary data to this article.
References
- 1.Barton J.L., Trupin L., Tonner C., et al. English language proficiency, health literacy, and trust in physician are associated with shared decision making in rheumatoid arthritis. J. Rheumatol. 2014;41(7):1290–1297. doi: 10.3899/jrheum.131350. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher E.B., Jr., Strunk R.C., Sussman L.K., et al. Acceptability and feasibility of a community approach to asthma management: the Neighborhood Asthma Coalition (NAC) J. Asthma: off. J. Assoc. Care Asthma. 1996;33(6):367–383. doi: 10.3109/02770909609068182. [DOI] [PubMed] [Google Scholar]
- 3.Shah S., Peat J.K., Mazurski E.J., et al. Effect of peer led programme for asthma education in adolescents: cluster randomised controlled trial. BMJ. 10 2001;322(7286):583–585. doi: 10.1136/bmj.322.7286.583. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horvath K.J., Oakes J.M., Rosser B.R., et al. Feasibility, acceptability and preliminary efficacy of an online peer-to-peer social support ART adherence intervention. AIDS Behav. 2013;17(6):2031–2044. doi: 10.1007/s10461-013-0469-1. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maro C.N., Roberts G.C., Sørensen M. Using sport to promote HIV/AIDS education for at-risk youths: an intervention using peer coaches in football. Scand. J. Med. Sci. Sports. 2009;19(1):129–141. doi: 10.1111/j.1600-0838.2007.00744.x. Feb. [DOI] [PubMed] [Google Scholar]
- 6.Thom D.H., Ghorob A., Hessler D., De Vore D., Chen E., Bodenheimer T.A. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann. Fam. Med. 2013;11(2):137–144. doi: 10.1370/afm.1443. Mar-Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Young S.D., Zhao M., Tieu K., Kwok J., Gill H., Gill N. A social media-based HIV prevention intervention using peer leaders. J. Consum. Health Internet. 2013;17(4):353–361. doi: 10.1080/15398285.2013.833445. /10/01 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dennis C.L. Peer support within a health care context: a concept analysis. Int. J. Nurs. Stud. 2003;40(3):321–332. doi: 10.1016/s0020-7489(02)00092-5. Mar. [DOI] [PubMed] [Google Scholar]
- 9.Safford M.M., Andreae S., Cherrington A.L., et al. Peer coaches to improve diabetes outcomes in rural Alabama: a cluster randomized trial. Ann. Fam. Med. 2015;13(Suppl 1):S18–S26. doi: 10.1370/afm.1798. Aug. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castro C.M., Pruitt L.A., Buman M.P., King A.C. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychol. 2011;30:285–294. doi: 10.1037/a0021980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindner H., Menzies D., Kelly J., Taylor S., Shearer M. Coaching for behaviour change in chronic disease: a review of the literature and the implications for coaching as a self-management intervention. Aust. J. Prim. Health. 2003;9:177–185. [Google Scholar]
- 12.Parent N., Fortin F. A randomized, controlled trial of vicarious experience through peer support for male first-time cardiac surgery patients: impact on anxiety, self-efficacy expectation, and self-reported activity. Heart Lung. 2000;29(6):389–400. doi: 10.1067/mhl.2000.110626. Nov-Dec. [DOI] [PubMed] [Google Scholar]
- 13.Avina-Zubieta J.A., Choi H.K., Sadatsafavi M., Etminan M., Esdaile J.M., Lacaille D. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008;59(12):1690–1697. doi: 10.1002/art.24092. Dec 15. [DOI] [PubMed] [Google Scholar]
- 14.England B.R., Sayles H., Michaud K., et al. Cause-specific mortality in male US veterans with rheumatoid arthritis. Arthritis Care Res. 2016;68(1):36–45. doi: 10.1002/acr.22642. Jan. [DOI] [PubMed] [Google Scholar]
- 15.Goodson N.J., Wiles N.J., Lunt M., Barrett E.M., Silman A.J., Symmons D.P. Mortality in early inflammatory polyarthritis: cardiovascular mortality is increased in seropositive patients. Arthritis Rheum. 2002;46(8):2010–2019. doi: 10.1002/art.10419. Aug. [DOI] [PubMed] [Google Scholar]
- 16.John H., Kitas G., Toms T., Goodson N. Cardiovascular co-morbidity in early rheumatoid arthritis. Research Support, Non-U.S. Gov't Review. Best Pract. Res. Clin. Rheumatol. 2009;23(1):71–82. doi: 10.1016/j.berh.2008.11.007. Feb. [DOI] [PubMed] [Google Scholar]
- 17.Kvalvik A.G., Jones M.A., Symmons D.P. Mortality in a cohort of Norwegian patients with rheumatoid arthritis followed from 1977 to 1992. Scand. J. Rheumatol. 2000;29(1):29–37. doi: 10.1080/030097400750001770. [DOI] [PubMed] [Google Scholar]
- 18.Meune C., Touze E., Trinquart L., Allanore Y. Trends in cardiovascular mortality in patients with rheumatoid arthritis over 50 years: a systematic review and meta-analysis of cohort studies. Meta-Analysis Review. Rheumatology. 2009;48(10):1309–1313. doi: 10.1093/rheumatology/kep252. Oct. [DOI] [PubMed] [Google Scholar]
- 19.Grundy S.M., Stone N.J., Bailey A.L., et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018;73(24):e285–e350. doi: 10.1016/j.jacc.2018.11.003. Jun 25 2019. [DOI] [PubMed] [Google Scholar]
- 20.Navarro-Millán I., Yang S., Chen L., et al. Screening of hyperlipidemia among patients with rheumatoid arthritis in the United States. Arthritis Care Res. 2019;71(12):1593–1599. doi: 10.1002/acr.23810. 2019/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bell C., Rowe I.F. The recognition and assessment of cardiovascular risk in people with rheumatoid arthritis in primary care: a questionnaire-based study of general practitioners. Muscoskel. Care. 2011;9(2):69–74. doi: 10.1002/msc.196. Jun. [DOI] [PubMed] [Google Scholar]
- 22.Navarro-Millán I., Cornelius-Schecter A., O'Beirne R.J., et al. Views of primary care physicians and rheumatologists regarding screening and treatment of hyperlipidemia among patients with rheumatoid arthritis. BMC Rheumatol. 2020;4:14. doi: 10.1186/s41927-020-0112-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aspry K.E., Furman R., Karalis D.G., et al. Effect of health information technology interventions on lipid management in clinical practice: a systematic review of randomized controlled trials. J. clin. lipidol. 2013;7(6):546–560. doi: 10.1016/j.jacl.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Wilensky G. Changing physician behavior is harder than we thought. JAMA. 2016;316(1):21–22. doi: 10.1001/jama.2016.8019. [DOI] [PubMed] [Google Scholar]
- 25.Kravitz R.L., Epstein R.M., Feldman M.D., et al. Influence of patients' requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA. 2005;293(16):1995–2002. doi: 10.1001/jama.293.16.1995. Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Navarro-Millan I., Zinski A., Shurbaji S., et al. Perspectives of rheumatoid arthritis patients on electronic communication and patient-reported outcome data collection: a qualitative study. Arthritis Care Res. 2019;71(1):80–87. doi: 10.1002/acr.23580. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Navarro-Millán I., Young S.R., Shurbaji S., et al. Barriers and facilitators for screening and treatment of hyperlipidemia among patients with inflammatory arthritis. BMC Rheumatol. 2020;4:26. doi: 10.1186/s41927-020-00123-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Treasure J. Motivational interviewing. Adv. Psychiatr. Treat. 2004;10(5):331–337. doi: 10.1192/apt.10.5.331. [DOI] [Google Scholar]
- 29.Hettema J., Steele J., Miller W.R. Motivational interviewing. Annu. Rev. Clin. Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 30.Andreae S.J., Andreae L.J., Cherrington A.L., et al. Development of a community health worker-delivered cognitive behavioral training intervention for individuals with diabetes and chronic pain. Fam. Community Health. 2018;41(3):178–184. doi: 10.1097/fch.0000000000000197. Jul-Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiner J., Lui G., Brown M., et al. Protocol for the pilot randomized trial of the CArdiovascular Risk assEssment for Rheumatoid Arthritis (CARE RA) intervention: a peer coach behavioral intervention. Pilot Feasibility Stud. 2022;8(1):84. doi: 10.1186/s40814-022-01041-z. /04/15 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nowell W.B., Curtis D., Thai M., et al. Digital interventions to build a patient registry for rheumatology research. Rheum. Dis. Clin. N. Am. 2019;45(2):173–186. doi: 10.1016/j.rdc.2019.01.009. May. [DOI] [PubMed] [Google Scholar]
- 33.Navarro-Millan I., Yang S., Chen L., et al. Screening of hyperlipidemia among patients with rheumatoid arthritis in the United States. Arthritis Care Res. 2019;71(12):1593–1599. doi: 10.1002/acr.23810. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Navarro-Millan I., Yang S., DuVall S.L., et al. Association of hyperlipidaemia, inflammation and serological status and coronary heart disease among patients with rheumatoid arthritis: data from the National Veterans Health Administration. Ann. Rheum. Dis. 2016;75(2):341–347. doi: 10.1136/annrheumdis-2013-204987. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 36.Knowles M. Gulf Publishing; Houston, TX USA: 1984. The Adult Learner: A Neglected Species. [Google Scholar]
- 37.Carmel A.S., Cornelius-Schecter A., Frankel B., et al. Evaluation of the Patient Activated Learning System (PALS) to improve knowledge acquisition, retention, and medication decision making among hypertensive adults: results of a pilot randomized controlled trial. Patient Educ. Counsel. 2019 doi: 10.1016/j.pec.2019.03.001. Mar 4. [DOI] [PubMed] [Google Scholar]
- 38.Motivational B.H.W.P. Interviewing for tobacco cessation. https://www.youtube.com/watch?v=1jfH055byg4 Video File.
- 39.Matulich B. Introduction to motivational interviewing. https://www.youtube.com/watch?v=s3MCJZ7OGRk Vidoe File.
- 40.Andreae S.J., Andreae L.J., Cherrington A., Richman J., Safford M. Peer coach delivered storytelling program for diabetes medication adherence: intervention development and process outcomes. Contemp Clin. Trials Commun. 2020;20 doi: 10.1016/j.conctc.2020.100653. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andreae S.J., Andreae L.J., Richman J.S., Cherrington A.L., Safford M.M. Peer-delivered cognitive behavioral training to improve functioning in patients with diabetes: a cluster-randomized trial. Ann. Fam. Med. 2020;18(1):15–23. doi: 10.1370/afm.2469. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Madson M.B., Loignon A.C., Lane C. Training in motivational interviewing: a systematic review. J. Subst. Abuse Treat. 2009;36(1):101–109. doi: 10.1016/j.jsat.2008.05.005. Jan. [DOI] [PubMed] [Google Scholar]
- 43.Khodneva Y., Richman J., Andreae S., Cherrington A., Safford M.M. Peer support intervention improves pain-related outcomes among rural adults with diabetes and chronic pain at 12-month follow-up. J. Rural Health. 2021;37(2):394–405. doi: 10.1111/jrh.12422. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Colón-Semenza C., Latham N.K., Quintiliani L.M., Ellis T.D. Peer coaching through mHealth targeting physical activity in people with Parkinson disease: feasibility study. JMIR Mhealth Uhealth. 2018;6(2):e42. doi: 10.2196/mhealth.8074. Feb 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schechter N., Butt L., Jacocks C., Staguhn E., Castillo R., Wegener S.T. Evaluation of an online motivational interviewing training program for rehabilitation professionals: a pilot study. Clin. Rehabil. 2021;35(9):1266–1276. doi: 10.1177/02692155211002958. Sep. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.