Abstract
Background
maxillary cysts of dental origin are not common diagnosis. There is still debate about their perfect treatment method. There are many approaches to manage the odontogenic maxillary cysts; either intraoral, sublabial, or transnasal endoscopic approach. In this study, we present our technique of trans-antral endoscopic assisted excision of maxillary cysts of dental origin with assessing feasibility, results, and complications.
Results
Thirty-two patients were reported; 14 dentigerous cysts (43.75%) and 18 dental (radicular) cysts (56.25%). Complete cyst removal could be achieved in all cases without jeopardizing the maxillary sinus drainage through its natural ostium to the nasal cavity. Postoperative pain and facial swelling were mild in all cases and resolved within few days. No tooth loss, Sino nasal symptoms, infection or recurrence was reported throughout follow-up period ranging from 2 to 6 years.
Conclusion
Trans-antral endoscopic assisted approach for excision of odontogenic maxillary cyst is a reliable, safe, and effective procedure without recurrence, or permanent negative sequels over the long-term follow-up.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12663-022-01772-9.
Keywords: Odontogenic cyst, Dental cyst, Radicular cyst, Dentigerous cyst, Maxilla, Maxillary sinus, Teeth, Endoscopy
Introduction
Cyst is defined as a cavity layered by epithelium that contains liquid, semi-solid, or gaseous contents. Odontogenic cysts in the maxilla originate from the epithelial remain associated with odontogenesis [1]. This epithelium may derive from the following structures: a) epithelial fragments of the teeth crown, b) Epithelial debris of Malassez (cells remain by development of teeth roots from inside of periodontal ligament), c) Epithelial debris of Seres (remains of teeth lamina), d) Fragments of teeth germ cells, including enamel, dental papilla and dental sac [2].
The odontogenic cysts are either developmental, Inflammatory, or Carcinoma arising in odontogenic cysts [3]. The developmental cysts encompass dentigerous cyst, eruption cyst, odontogenic keratocyst, orthokeratinized odontogenic cyst, gingival cyst of the newborn, gingival cyst of the adult, lateral periodontal cyst, and glandular odontogenic cyst. The inflammatory cysts include periapical (radicular) cyst and residual cyst [4].
The most common type of odontogenic cysts is periapical (radicular) cysts (65%), followed by dentigerous cysts (24%) and odontogenic keratocysts (5%) [4]. Although the dentigerous cyst is the second most common cyst of the jaws [5], it is extremely rare in the maxillary sinus [6].
There are many approaches to manage the odontogenic maxillary cysts; either intraoral, sublabial, or transnasal endoscopic approach. The intraoral approach is either through enucleation, marsupialization, or tooth extraction and trans alveolar curettage [2]. The sublabial approach is through Caldwell-Luc operation [7–10]. The transnasal endoscopic approach is either through inferior meatal antrostomy [1], middle meatal antrostomy [11], or endoscopic medial maxillectomy [12]. Each of the former approaches has its supremacy and pitfalls.
The aim of this case series is to present our experience in the management of maxillary cysts of dental origin by trans-antral endoscopic assisted approach. In the study, we discuss the feasibility, results, benefits, and complications of maxillary cyst of dental origin removal through a small sublabial incision then do a small antral window and use the 0-degree telescope and endoscopic instruments to completely remove the maxillary cyst.
Methodology
A retrospective assessment of all cases that were diagnosed to have maxillary cysts of dental origin and operated in Otorhinolaryngology, Head and Neck surgery department of University Hospitals in the period from January 2012 till to June 2018. The data included patients’ demographic characteristics, indications, surgical information, and complications with follow-up period ranging from 2 to 6 years.
The study was approved by our local institutional review board, and informed written consent was signed by all patients.
Diagnosis depended on suggested clinical examination, and computed tomography axial and coronal cuts of the maxillofacial area and histopathology confirmed diagnosis cooperatively in all included cases. CT showed radiolucent lesion with a well-defined and corticated rim in the maxilla, with hydraulic expansion of the alveolar bone with remolding, thinning, and scalloping. The maxillary sinus floor is upraised, and its lumen is decreased. A thin bony plate between the cyst and the maxillary sinus cavity was demonstrated in all cases as extra-antral lesion and distinguishing the cyst from the antral lesions.
Revision cases, patients who did not complete follow up and cases of another histopathological diagnosis were excluded from the study.
Surgical Technique
Under general anesthesia with oral endotracheal intubation, while the patients were supine with head elevated, 2% lidocaine with 1:100,000 epinephrine was injected into the upper sublabial area on the affected side. The upper gingivolabial fold was incised approximately 3 mm above the gingivolabial sulcus and the incision was deepened and dissected to expose the anterior bony wall of the maxillary antrum (taking care to avoid injury of the infraorbital nerve). The cutting drill is used to do a small hole in the anterior wall of the maxillary sinus in the canine fossa. The 0-degree 4-mm telescope is used in the surgical opening of the maxillary antrum to explore the cyst within the maxillary sinus (Fig. 1). The endoscopic instruments (dissectors – curettes—forceps) are used to carefully dissect the cyst with its content and its entire wall from its attachment. Sometimes there is erosion within the wall of the maxillary sinus, so careful dissection can be achieved with help of better illumination and magnification of the endoscope (Fig. 2). Throughout the procedure avoidance of injury of healthy unaffected maxillary sinus mucosa, complete removal of the entire cyst wall, and ensure hemostasis should be achieved.
Fig. 1.
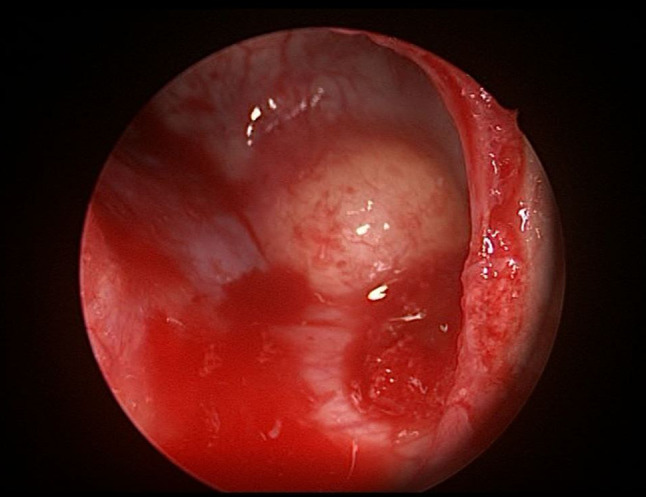
Tran-antral endoscopic view of odontogenic maxillary cyst
Fig. 2.

Tran-antral endoscopic view of maxillary sinus after removal or odontogenic maxillary cyst with exposed infratemporal fossa (*)
Trans-antral endoscopic assisted excision of the odontogenic maxillary cyst using 0° 4-mm rigid telescope through sublabial approach after doing a small window in the anterior wall of the maxillary sinus was done in all cases. This technique amalgamates between better illumination and magnification of the endoscope and direct access of sublabial approach.
It ensures complete removal of the entire cyst wall without any remnants within the cavity to avoid any chance of recurrence, avoid injury of nearby important structure if there is erosion within the maxillary wall, secure hemostasis through doing bipolar cauterization of any bleeding point to avoid postoperative hematoma, and finally evaluate the postoperative cavity to identify, and mange any oroantral fistula.
In patients with dentigerous cyst (Fig. 3), the affected tooth was removed with the cyst in all cases while in the radicular cyst patients the tooth was preserved. The covering maxillary mucoperiosteum and soft tissue were returned to their original site and the wound closed with vicryl.
Fig. 3.

CT scan of dentigerous cyst involving the maxillary sinus
Postoperative Work Up
Patients were discharged after 24 h. Swelling, cheek pain, nasal obstruction, hemorrhage, teeth loosening, and facial paresthesia were evaluated 1 to 7 days after the operation. The patients were followed up weekly for a month then at 6 months intervals. Facial swelling was measured qualitatively 3 days after the surgery. Swelling was recorded as follows: mild (almost unnoticeable swelling in the infraorbital region), moderate (noticeable swelling in the infraorbital region), and heavy (significant swelling in the infraorbital region that extends to the periorbital region) [6].
Postoperative Outcome and Results
Thirty-two patients; 18 males (56.25%) and 14 females (43.75%) were included with age range 12 to 43 years (mean = 25.6 ± 8.5). They were 14 developmental dentgerous cysts (43.75%) and 18 radicular cysts (56.25%); 20 on the left side (62.5%) and 12 on the right sides (37.5%) (Table 1). The presenting symptom was slowly growing cheek swelling in all patients, while only 6 patients (18.75%) complained also of facial pain and heaviness. All cysts involved the maxillary sinus. The size of the cysts ranged between 2 and 5 cm.
Table 1.
Patients' data
| Sex | Males | 18 (56.25%) |
| Females | 14 (43.75%) | |
| Age | 12 to 43 years | |
| Side | Right | 12 (37.5%) |
| Left | 20 (62.5%) | |
| Types | Dental (radicular) cysts | 18 (56.25%) |
| Dentigerous cyst | 14 (43.75%) | |
Complete cyst removal with its entire wall could be achieved in all cases without jeopardizing the maxillary sinus drainage through its natural ostium to the nasal cavity.
Recovery was event-less in all cases. Postoperative pain and facial swelling were mild in all cases and resolved within 7 days. Facial paraesthesia, nasal obstruction, and hemorrhage were not detected. No tooth loss, infection or recurrence was reported throughout the follow-up period that ranged between 2 and 6 years (mean = 4.7 ± 1.2). Postoperatively and throughout follow up, the vitality of the teeth was regularly checked and was found sound. All over the follow-up period, there were no nasal and/or paranasal sinuses persistence symptoms with normally apparent nasal endoscopy examinations on the follow-up visits every 6 months.
In one patient (3%) with infected dentigerous cyst an oroantral fistula was reported 1 week postoperatively. It did not close spontaneously as we assumed so after control of infection and a dental opinion was asked, the fistula was primary closed after curettage of the bone.
Because in all the included cases in the current study, the teeth involved in the cystic process had no severe loss of alveolar bone support and were presenting with enough bone support, and good survival prognosis. So the teeth were preserved. Orthodontic evaluation and treatment was started after healing from surgery mostly 10 days after removal of the cyst by the orthodontist.
Discussion
Odontogenic cysts are lesions originating from the teeth bearing bones of the maxilla and/or mandible. They emerge from the epithelial remnants associated with odontogenesis. They may be developmental, inflammatory, or neoplastic [3].
The most frequent types are periapical (radicular) cyst, dentigerous cyst and primordial or keratocyst [4]. Research on the Odontogenic cysts in the maxillary sinus are seldom discussed on account of the disease's low morbidity [6].
Surgical excision of these cysts is indicated to prevent oroantral fistula formation and chronic rhinosinusitis in addition to relive the cosmetic disfigurement in large cysts.
The odontogenic cysts management is either through intraoral, sublabial, and/or transnasal endoscopic approaches. Most dentists are using the intraoral approaches such as enucleation, curettage, marsupialization, and tooth extraction [1], as in most cases the dentist discover it early before expansion in the maxillary sinus and do sinus complications.
In odontogenic cysts in the maxillary sinus, tooth extraction and trans alveolar curettage are usually associated with potential morbidity such as oroantral fistula, chronic rhinosinusitis, need for extensive reconstruction, loss of surrounding dentition, the affected teeth are extracted along with the cyst walls, and high recurrence rate. So, if the teeth are involved within the cyst with severe loss of alveolar bone support it is extracted otherwise teeth are preserved by doing root canal treatment [7].
The sublabial approach by Caldwell-Luc operation offer the advantage of wide operative field with the feasibility of complete removal of the cyst, but it is presumed to be associated with co-morbidity as facial edema, cheek discomfort, dental pain, facial asymmetry, facial paresthesia, maxillary sinusitis following extensive sinus mucosa removal, and a partial loss of the bony wall of the canine fossa [8–10, 13].
The transnasal endoscopic approach through inferior meatal antrostomy is done by resection of anterior edge of the inferior turbinate and the bony wall of the inferior meatus is opened to observe the cyst wall in the maxillary sinus which is partially or completely removed [1].
In the study of Seno et al. [1] who used the above approach the cyst wall was completely removed in only 61.5% of cases and partially resected in 38.5% of cases [1]. This is not only increasing the incidence of recurrence rate but also make hazards if the cyst was neoplastic or have a neoplastic change.
The transnasal endoscopic approach through a wide maxillary antrostomy is performed with removal of the uncinate process and the unattached portion of the maxillary cyst is delivered from the lateral and anterior aspect of the sinus and debulked using a microdebrider, curettes and non-cutting instruments. To access the inferior portion of the maxillary sinus, an endoscopic maxillary mega-antrostomy is performed [11].
In the study of Jain and Goyal [11], they used the above technique which did not offer complete removal of the cyst wall and they did only marsupialization and depended on nasal hygiene measures to clear any material produced by the residual cyst [11]. This technique also due to the incomplete removal of the entire cyst wall carries the hazard of recurrence or missing tissue in neoplastic cyst.
The transnasal endoscopic approach through endoscopic medial maxillectomy has been used to ensure complete removal of the cyst with its entire wall [12] as described by Nakayama et al. however, this technique carries all the risk of endoscopic medial maxillectomy of injury of the nasolacrimal duct, orbit, or risk of empty nose syndrome.
In our technique of trans-antral endoscopic assisted excision, we combined the advantages of endoscopy (better illumination, magnification, and small approach) and sublabial approach (wide operative field) while avoiding the disadvantage of each; endoscopy (indirect approach which need removal important structures which may affect the drainage and ciliary function of the sinus), and the sublabial approach by Caldwell-Luc operation (associated co-morbidity).
In this technique, we got the advantage of wide exposure with better illumination and magnification that ensure complete removal of all the cyst wall without any remnants within the cavity to avoid any chance of recurrence and to ensure complete removal of any suspected neoplastic tissue if present, avoid injury of any nearby structures if there is erosion within the sinus wall, secure hemostasis, identify and early management of any oroantral fistula.
Because of the malignant transformation within the dentigerous cysts has been reported [12, 14, 15], discrimination between keratocystic odontogenic tumors and radicular cysts before surgery is sometimes difficult [16] and the recurrence rate, the decision of complete removal of the odontogenic cyst is crucial and the marsupialization is not satisfactory.
The transnasal endoscopic approach through inferior meatal antrostomy or wide maxillary antrostomy cannot offer the complete removal of the cyst with its entire wall in all cases as the anterior and lateral wall of the maxillary sinus are not feasible accessible endoscopically even with 700 telescope in all cases. Also they are associated with co-morbidity due to removed structures in order to access the cyst.
The transnasal endoscopic approach through endoscopic medial maxillectomy can offer complete removal of the entire cyst wall; however, it is associated with much co-morbidity with incidence of injury the nearby structures.
The sublabial approach by Caldwell-Luc operation although it offers direct access operative filed however it need more bony removal of the anterior maxillary wall to achieve wide operative field that beside the lack of magnification and better illumination. Also, it is associated with much co-morbidity of facial edema, cheek discomfort, dental pain, facial asymmetry, facial paraesthesia, maxillary sinusitis following extensive sinus mucosa removal, and a partial loss of the bony wall of the canine fossa.
The trans-antral endoscopic assisted approach co-morbidity seems to be the least (small opening of the anterior maxillary wall) comparing to the benefit of complete excision of the cyst within its entire wall in all the cases with minimal injury of the unaffected maxillary sinus mucosa as well as avoidance of injury of any nearby structure if there is a defect in the sinus wall, confirm hemostasis and evaluate the postoperative cavity to identify oroantral fistula.
So, our technique offers the advantage of complete resection of the odontogenic maxillary cyst without the extensive maneuver of endoscopic medial maxillectomy with the least acceptable co-morbidity and recurrence rate reach 0%. It also offers less destructive effect than Caldwell-Luc operation with better endoscopic illumination and magnification.
This study aimed to report our experience in the management of maxillary cysts of dental origin with long term follow up (2 – 6 years).
The trans-antral endoscopic assisted approach was used safely without facial scar or interferes with the mucociliary function of the maxillary sinus or its natural drainage pathway. No need for hypotensive anesthesia which often required during endoscopic approach. The nasal patency was preserved as the nasal cavity was away from the work theater thus the patients recover without nasal packing. The endoscopic assistance adds the benefits of better illumination and magnification as well as the trans-antral approach add the benefit of direct access of the lesion.
So, it offers complete removal of the entire cyst wall without any remnants within the cavity to avoid any chance of recurrence, avoid injury of nearby important structures if there is erosion within the maxillary wall, secure hemostasis through doing bipolar cauterization of any bleeding point to avoid postoperative hematoma, and finally evaluate the postoperative cavity to identify, and mange of any oroantral fistula.
The commonest odontogenic cyst detected in the current study was the dental cyst as previously recorded by Xu et al. [6].
Although the trans-antral endoscopic assisted approach was associated with some morbidity as temporary cheek edema, however, this edema was mild and resolved within one week. No permanent paraesthesia, sinusitis or teeth loss was reported in our cases. However, randomized comparative studies between all approaches are needed.
Conclusion
The trans-antral endoscopic assisted excision of odontogenic maxillary cyst approach has the advantage of direct lesion access of the sublabial approach as well as the advantages of better illumination, magnification, and small access of endoscopic approach. It offers complete removal of the entire cyst wall without any remnants, avoid injury of nearby important structures, secure hemostasis and evaluate the postoperative cavity for any oroantral fistula. Thus, we recommend it as a priority choice for such lesions.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
The authors declare no financial support or interest to this study.
Declarations
Conflict of interest
the authors declare no conflict of interest.
Ethical Approval
The institutional review board (IRB) approved the research. The study was performed according to the Declaration of Helsinki on Biomedical Research Involving Human Subjects.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Seno S, Ogawa T, Shibayama M, Ogawa F, Fukui J, Owaki S, Suzuki M, Shimizu T. Endoscopic sinus surgery for the odontogenic maxillary cysts. Rhinology. 2009;47(3):305. doi: 10.4193/Rhin08.162. [DOI] [PubMed] [Google Scholar]
- 2.Cedin AC, Junior FA, Landim ER, da Silva FLP, de Oliveira LF, Sotter AC. Endoscopic treatment of odontogenic cyst with intrasinusalextension. Rev Bras Otorrinolaringol. 2005;71(3):392–395. doi: 10.1590/S0034-72992005000300023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neville BW, Damm DD, Allen CM, Chi AC. Oral and maxillofacial pathology. Netherlands: Elsevier; 2015. [Google Scholar]
- 4.Daley TD, Wisoccki GP, Pringle GA. Relative incidence of odontogenic tumors and oral jaw cysts in Canadian population. Oral surg. 1994;77:276–280. doi: 10.1016/0030-4220(94)90299-2. [DOI] [PubMed] [Google Scholar]
- 5.Motamedi MH, Talesh KT. Management of extensive dentigerous cysts. Br Dent J. 2005;198:203–206. doi: 10.1038/sj.bdj.4812082. [DOI] [PubMed] [Google Scholar]
- 6.Xu C, Yang C, Fan X, Ying-Kai Hu MM. Chuang-Qi Yu Functional surgery for the treatment of dentigerous cyst in the maxillary sinus. J Craniofac Surg. 2015;26(2):84–86. doi: 10.1097/SCS.0000000000001287. [DOI] [PubMed] [Google Scholar]
- 7.Safadi A, Kleinman S, Gigi D, Wengier A, Oz I, Abergel A, Koren I, Ungar OJ. Surgical management of odontogenic cysts involving the maxillary sinus-a retrospective study. J Cranio Maxillofac Surg. 2020;48(8):800–807. doi: 10.1016/j.jcms.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Matheny KE, Duncavage JA. Contemporary indications for the Caldwell-Luc procedure. Curr Opin Otolaryngol Head Neck Surg. 2003;11:23–26. doi: 10.1097/00020840-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Saito H, Takanami N, Saito T, et al. Studies on the Caldwell-Luc operation with or without counter opening at the inferior meatus. J Otorhinolaryngol Relat Spec. 1990;52:249–253. doi: 10.1159/000276143. [DOI] [PubMed] [Google Scholar]
- 10.Kasat VO, Karjodkar FR, Laddha RS. Dentigerous cyst associated with an ectopic third molar in the maxillary sinus: a case report and review of literature. Contemp Clin Dent. 2012;3:373–376. doi: 10.4103/0976-237X.103642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain K, Goyal P. Endoscopic surgical treatment of maxillary odontogenic cysts. Int Forum Allergy Rhinol. 2015;5(7):602–604. doi: 10.1002/alr.21525. [DOI] [PubMed] [Google Scholar]
- 12.Nakayama T, Otori N, Asaka D, Okushi T, Haruna SI. Endoscopic modified medial maxillectomy for odontogenic cysts and tumours. Rhinology. 2014;52(4):376–380. doi: 10.4193/Rhino13.134. [DOI] [PubMed] [Google Scholar]
- 13.Akyol UK, Salman IA. A case of an extensive dentigerous cyst in the maxillary sinus leading to epiphora and nasalobstruction. J Emerg Med. 2012;43:1004–1007. doi: 10.1016/j.jemermed.2010.11.045. [DOI] [PubMed] [Google Scholar]
- 14.Yasuoka T, Yonemoto K, Kato Y, Tatematsu N. Squamous cell carcinoma arising in a dentigerous cyst. J Oral Maxillofac Surg. 2000;58:900–905. doi: 10.1053/joms.2000.8219. [DOI] [PubMed] [Google Scholar]
- 15.Gulbranson SH, Wolfrey JD, Raines JM, McNally BP. Squamous cell carcinoma arising in a dentigerous cyst in a 16-month-old girl. Otolaryngol Head Neck Surg. 2002;127:463–464. doi: 10.1067/mhn.2002.129039. [DOI] [PubMed] [Google Scholar]
- 16.Hyo Y, Akisada T, Harada T. A case of keratocyst in the maxillary sinus. Jap J Rhinol. 2007;46:97–101. doi: 10.7248/jjrhi1982.46.2_97. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


