Summary
On December 7, 2022, China's National Health Commission issued the Ten New Covid Rules lifting the dynamic zero-COVID policy. In the interim, vaccination campaigns continue to be promoted. We assessed the potential impacts on the status, perceptions, and attitudes toward COVID-19 vaccines via an online self-administered questionnaire. Among 1,170 participants, 1,142 (97.6%) participants were vaccinated against COVID-19, and 51.8% (591/1,142) have already received the booster. More than half of the participants who were vaccinated were ages 31 to 50 (51.8%). Participants believed the following strategies could improve the vaccination rate: timely feedback of the vaccination data (such as safety, efficacy, and other issues of public concern) from authoritative media (95.6%), increasing the number of vaccination sites and availability of vaccines and using more convenient methods of making appointment (95.2%), recommendations from friends and relatives (94.8%), and presenting the qualifications of the staff performing vaccination (89.1%). More measures, including targeted measures for different age groups and timely feedback on the vaccination data including safety and efficacy from authoritative media, are likely to help improve vaccination rates.
Keywords: COVID-19, vaccination, dynamic zero-COVID policy, China
Introduction
Since severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused an outbreak of COVID-19 in Wuhan in late 2019, this highly transmissible infection causing pneumonia has not only posed serious threats to human health and public safety but also resulted in a profound decline in social-economic development in China (1,2). Over the past three years, China had been implementing a dynamic zero-COVID policy to block national outbreaks and to keep the mortality rate low (3). Currently, the Omicron variant has reignited the pandemic in different countries and regions with enhanced transmissibility but relatively low pathogenicity (4). To better balance COVID-19 control and socioeconomic issues, more countries have gradually relaxed their policies (5,6).
On December 7, 2022, China lifted its prior severe control policy (7). Regular testing requirements and travel restrictions were suspended and people infected with COVID-19 are allowed to self-quarantine at home instead of management in centralized isolation (7). According to the National Health Commission, from December 8, 2022 to January 12, 2023, a total of 59,938 deaths related to COVID-19 occurred in hospitals, including 5,503 deaths from COVID-19-related respiratory failure and 54,435 from underlying diseases combined with COVID-19 infection (8). The average age of those who died was 80.3; 90.1% were age 65 or older, and 56.5% were age 80 or older (8).
The importance of vaccination acceptance
After lifting the zero-COVID policy, some measures such as wearing masks, washing hands, and being vaccinated have been still implemented to reduce transmission to the lowest levels (7). Although protection against the omicron variant has waned over time, current studies substantiate the effectiveness and efficacy of a booster against different COVID-19 variants of concern (9-12). Studies have also provided evidence that the COVID-19 vaccine has effective protection against SARS-CoV- 2-related diseases and is also effective in preventing severe cases and death (12-14). According to the US Centers for Disease Control and Prevention (CDC), vaccination is one of the most cost-effective strategies to effectively control COVID-19 and stop repeated outbreaks through mass immunization (15). As for the established herd/population immunity theory, vaccination of the population up to the herd immunity threshold (HIT) may help control the spread of SARS-Cov-2 and provide indirect protection to those who are susceptible and immunocompromised (16-18). Vaccine coverage of about 90% is needed to achieve herd immunity, and vaccine coverage may need to be higher for the omicron variant (19).
The success of population-level vaccination programs to obtain herd immunity to return to normal life depends mainly on vaccination acceptance. As of January 12, 2023, 1.31 billion people in China had received at least one dose of a COVID-19 vaccine, while the current vaccination rate (the proportion of those receiving a booster) in the country is only 57.92% (20).
The current study evaluated the potential impacts of the status, perceptions, and attitudes toward COVID-19 vaccines via an online self-administered questionnaire conducted from February to March 2022. The aim of this study was to provide useful information for more aggressive and targeted measures to improve vaccination rates. This study evaluated the vaccination acceptance of the participants and also collected information on opinions and suggestions for designing possible vaccination strategies to improve the vaccine coverage rate, and especially that for vulnerable populations.
Factors associated with COVID-19 vaccination status
The concern about vaccine efficacy has had the largest impact on vaccine hesitancy, followed by adverse reactions (21). Several clinical trials on vaccines have reported efficacy and continuous protective effects for the majority of the participants (9,22,23). A total of 1,170 participants were included in the final analysis of the current study. As shown here, almost all of the participants were vaccinated against COVID-19 (1,142, 97.6%) (Table 1), which can be attributed to their belief in vaccination efficacy (1,005, 88.0%) (Figure 1A). More than half have already received the booster (591/1,142, 51.8%), which is similar to the national level (57.92%) (20). Perceptions and intentions have been identified as important factors influencing vaccination acceptance during the previous 2009 H1N1 pandemic (24). Most of the participants thought people engaged in high-risk occupations (1,083, 92.6%) should receive prioritized vaccination, followed by medical workers (913, 78%), people who travel frequently (887, 75.8%), and students or teachers (739, 63.2%) (Figure 1B). In terms of the manufacturer of the vaccine, about three-quarters (845, 74.0%) of the participants have received the Sinovac COVID-19 vaccine (Supplementary Figure S1, https:// www.globalhealthmedicine.com/site/supplementaldata. html?ID=64).
Table 1. Characteristics of study participants (n = 1,170).
| Variables | Total (n = 1,170) | Vaccine (n = 1,142) | No vaccine (n = 28) | p |
|---|---|---|---|---|
| Age (years) | < 0.001 | |||
| 18-30 | 405 (34.6) | 401 (35.1) | 4 (14.3) | |
| 31-50 | 600 (51.3) | 591 (51.8) | 9 (32.1) | |
| 51-65 | 136 (11.6) | 130 (11.4) | 6 (21.4) | |
| > 65 | 29 (2.5) | 20 (1.8) | 9 (32.1) | |
| Sex | 0.008 | |||
| Males | 750 (64.1) | 739 (64.7) | 11 (39.3) | |
| Females | 420 (35.9) | 403 (35.3) | 17 (60.7) | |
| Ethnicity | 0.757 | |||
| Han | 1,113 (95.1) | 1,086 (95.1) | 27 (96.4) | |
| Man | 34 (2.9) | 33 (2.9) | 1 (3.6) | |
| Mongolian | 6 (0.5) | 6 (0.5) | 0 (0) | |
| Zhuang | 3 (0.26) | 3 (0.26) | 0 (0) | |
| Chinese Korean | 3 (0.26) | 3 (0.26) | 0 (0) | |
| Bai | 2 (0.17) | 2 (0.18) | 0 (0) | |
| Yi | 2 (0.17) | 2 (0.18) | 0 (0) | |
| Tujia | 2 (0.17) | 2 (0.18) | 0 (0) | |
| Miao | 1 (0.09) | 1 (0.09) | 0 (0) | |
| Kazakh | 1 (0.09) | 1 (0.09) | 0 (0) | |
| Other | 3 (0.26) | 3 (0.26) | 0 (0) | |
| Level of education | 0.071 | |||
| Middle school or lower | 180 (15.4) | 172 (15.1) | 8 (28.6) | |
| High school, vocational school, junior college | 506 (43.2) | 498 (43.6) | 8 (28.6) | |
| University, college | 348 (29.7) | 337 (29.5) | 11 (39.3) | |
| Graduate school | 136 (11.6) | 135 (11.8) | 1 (3.6) | |
| Marital status | 0.068 | |||
| Married | 754 (64.4) | 732 (64.1) | 22 (78.6) | |
| Single | 369 (31.5) | 365 (32.0) | 4 (14.3) | |
| Divorced | 37 (3.2) | 36 (3.2) | 1 (3.6) | |
| Widowed | 10 (0.9) | 9 (0.8) | 1 (3.6) | |
| Residence | 0.005 | |||
| Urban | 953 (81.5) | 925 (81.0) | 28 (100) | |
| Rural | 217 (18.5) | 217 (19.0) | 0 (0) | |
| Living alone | 0.829 | |||
| Yes | 311 (26.6) | 303 (26.5) | 8 (28.6) | |
| No | 859 (73.4) | 839 (73.5) | 20 (71.4) | |
| Annual household income [RMB] | 0.039 | |||
| < 30,000 | 178 (15.2) | 171 (15.0) | 7 (25.0) | |
| 30,000-80,000 | 527 (45.0) | 520 (45.5) | 7 (25.0) | |
| 80,000-150,000 | 233 (19.9) | 229 (20.1) | 4 (14,3) | |
| 150,000-300,000 | 139 (11.9) | 134 (11.7) | 5 (17.9) | |
| > 300,000 | 93 (7.9) | 88 (7.7) | 5 (17.9) | |
| Occupation | < 0.001 | |||
| Company employee | 510 (43.6) | 505 (44.2) | 5 (17.9) | |
| Medical worker | 118 (10.1) | 116 (10.2) | 2 (7.1) | |
| Student, teacher | 114 (9.7) | 114 (10.0) | 0 (0) | |
| Civil servant, government employee | 53 (4.5) | 51 (4.5) | 2 (7.1) | |
| Freelancer | 29 (2.5) | 25 (2.2) | 4 (14.3) | |
| Driver | 23 (2.0) | 22 (2.0) | 1 (3.6) | |
| Service worker (catering, express delivery, sales clerk, barber, security guard, etc.) | 15 (1.3) | 14 (1.2) | 1 (3.6) | |
| Self-employed | 12 (1.0) | 10 (0.9) | 2 (7.1) | |
| Logistics, cold chain staff | 5 (0.4) | 5 (0.4) | 0 (0) | |
| Flight attendant, airport staff | 1 (0.09) | 1 (0.09) | 0 (0) | |
| Customs personnel | 1 (0.09) | 1 (0.09) | 0 (0) | |
| Seafood market staff | 1 (0.09) | 1 (0.09) | 0 (0) | |
| Other | 288 (24.6) | 277 (24.3) | 11 (39.3) | |
| Self-rated health status | < 0.001 | |||
| Very healthy | 797 (68.1) | 784 (68.7) | 13 (46.4) | |
| Relatively healthy | 360 (30.8) | 349 (30.6) | 11 (39.3) | |
| In poor health | 13 (1.1) | 9 (0.8) | 4 (14.3) |
Figure 1.
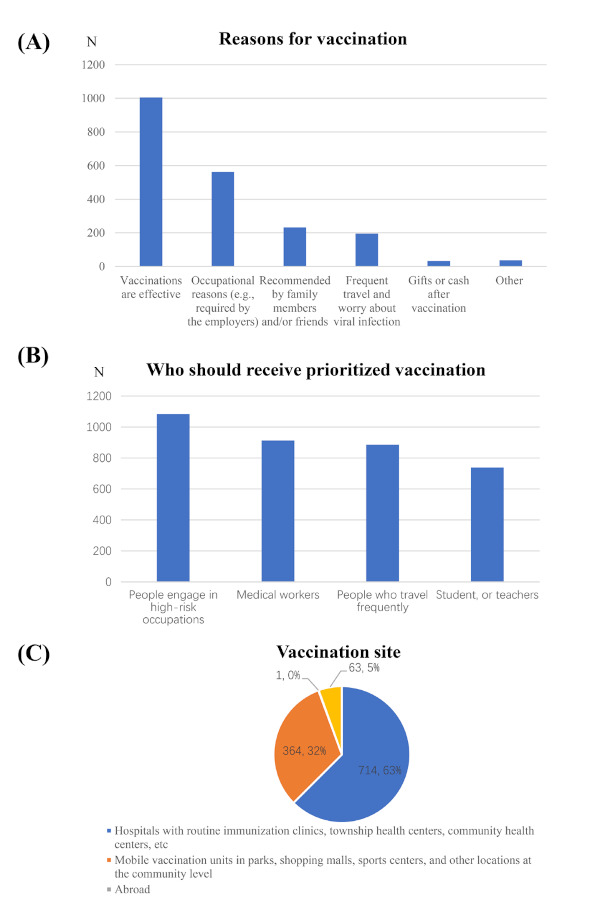
Actions and factors associated with COVID-19 vaccination. (A) Reasons for vaccination; (B) Who should receive prioritized vaccination; (C) Vaccination site.
In addition, social and demographic factors may also influence vaccination acceptance (25). More than half of the participants who were vaccinated were ages 31 to 50 (591, 51.8%) (Table 1). Compared to the unvaccinated, younger participants (ages 31-50), males (739, 64.7%), participants living in an urban area (925, 81.0%), and participants with a higher level of education were more likely to be vaccinated. Occupation and income were associated with vaccination status as well. Nearly half of the participants (520, 45.5%) who were vaccinated had an annual household income between 30,000-80,000 RMB. In addition, participants who self-rated their health as very healthy (784, 68.7%) or relatively healthy (349, 30.6%) were more likely to be vaccinated.
Studies have suggested that other vaccine-related profiles can also influence people's behavior, such as convenience, price, and recommendations from doctors (21). China is a developing country with unequal economic development among regions, so the free vaccination policy has dispelled the price worries of some people and markedly increased the vaccine acceptance and vaccination rate (26). Convenient models for making appointments and ubiquitous vaccination sites have greatly increased vaccination rates. Figure 1C shows the vaccination sites. Most participants were vaccinated in hospitals with routine immunization clinics or health centers at different levels (714, 62.5%); some other participants were vaccinated at mobile vaccination units in parks, shopping malls, or sports centers (364, 31.9%).
The current study also obtained opinions and suggestions from the participants to improve the vaccination rate. Participants believed the following strategies could improve the vaccination rate: timely feedback of the vaccination data (such as safety, efficacy, and other issues of public concern) from authoritative media (1119, 95.6%), increasing the number of vaccination sites and availability of vaccines and using more convenient methods of making appointment (1,114, 95.2%), recommendations from friends and relatives (1,109, 94.8%), and presenting the qualifications of the staff performing vaccination (1,043, 89.1%).
Influence of population heterogeneity on vaccination acceptance
Despite the generally positive findings, there were still 28 participants (2.4%) who had yet not been vaccinated, their detailed characteristics are also shown in Table 1. Both adults ages 31 to 50 and older people over the age of 65 accounted for 30% of the unvaccinated. A major factor that influenced general vaccine acceptance was fear and anxiety, and especially fear of adverse reactions (27). Recent studies have noted an increased risk of myocarditis in adults younger than 40 particularly associated with the two-dose mRNA vaccine (28,29). Some regions adopted vaccination incentives to encourage the unvaccinated and these measures led to young adults' decreased confidence in and distrust of the vaccine (30). Older adults who were unsure of being vaccinated against COVID-19 or who refused vaccination would rather take nonpharmaceutical measures like wearing a mask and washing their hands frequently (31). They were concerned about the safety and efficacy of the vaccine. Rare but severe events involving thrombosis and the potential increased risk of blood clots may have had a profound effect on their vaccination acceptance (32). Individuals with cancer or other severe comorbidities were unsure about the personal benefits of vaccination and eventually refused (33). In addition, older adults with family members younger than 18 years of age refused to be vaccinated for fear of affecting younger family members (34).
Despite the low reported risk of COVID-19 vaccination affecting fertility, a small proportion of the female population, and especially pregnant women, still have doubts about infertility and concerns about exposing their babies to potential harm (35,36). Another reason may be the fear of menstrual disruption (37-39). About half of the participants (548, 46.8%) had children (under 18 years of age) in their families, and more than half (326, 59.5%) were unwilling to let their children be vaccinated. Concern about vaccine efficacy has the greatest impact on vaccine hesitancy, followed by adverse reactions (36). Incidents such as the Changchun Changsheng vaccine incident have severely undermined public trust (40). At the same time, negative reports on adverse events without valid evidence continuously alter and distort the public perceptions of vaccine safety and efficacy and eventually lead to vaccine hesitancy or even vaccine refusal (41). Parents are skeptical of the vaccine development process and also afraid of adverse reactions, which may be overlooked in the rush to develop vaccines (42). Moreover, the fact that immunosuppressants may affect the immunogenicity of the vaccine played a role in whether parents allowed their children to be vaccinated (43). The adolescents themselves believed that they had no risk of infection and that their symptoms would not be severe if they were infected (44). Adolescents with a history of immune-related diseases or other primary diseases in particular refused vaccination unless convincing evidence indicated clear benefits to them (42,44). Moreover, clinical trials on the COVID-19 vaccine for adolescents (younger than 18) are still lacking and real-time dissemination of information on vaccine efficacy among adolescents is still limited.
Conclusions and Suggestions
The current results indicated a high level of COVID-19 vaccine acceptance among the adult population in China during the pandemic. With accurate perceptions and proper understanding of the purpose of COVID-19 vaccines, coverage at the population level has improved. However, challenges still remain as a small fraction of eligible people is still not vaccinated. Moreover, there is reluctance to vaccinate children.
To achieve and maintain herd immunity, we recommend the following multifaceted efforts. First, developing more safe and effective vaccines is crucial in the face of a drastic change in policy and the uncertainty of viral mutation. Second, age group heterogeneity affects vaccination and therefore targeted measures need to be taken for different age groups. Third, timely feedback on vaccination data, including safety and efficacy, from authoritative media can dispel skepticism regarding the necessity and efficacy of vaccines and effectively improve the acceptance rate.
Acknowledgements
The authors would thank Zhejiang Baoying Materials Group Co., Ltd. and all participants in this survey. The authors also wish to sincerely thank Peng Li and Suna Tian for their assistance in preparing the figures in this manuscript.
Funding:
This work was supported by grants from the Shanghai Fund for Personnel Development (Grant No. 2017090 to Y Du), a project under the Scientific and Technological Innovation Action Plan of the Shanghai Natural Science Fund (Grant No. 20ZR1409100 to L Wang), a project of the Chinese Association of Integration of Traditional and Western Medicine special foundation for Obstetrics and Gynecology-PuZheng Pharmaceutical Foundation (Grant No. FCK-PZ-08 to L Wang), a project for hospital management of the Shanghai Hospital Association (Grant No. X2021046 to L Wang), and a clinical trial project of the Special Foundation for Healthcare Research of the Shanghai Municipal Health Commission (Grant No. 202150042 to L Wang). The funding agencies played no role in the conduct of the research and preparation of the article.
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021; 19:141-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020; 78:185-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Central People's Government of China Web Portal. Why insist on "dynamic zeroing"?. http://www.gov.cn/xinwen/2022-04/29/content_5688064.htm (accessed January19, 2023). (in Chinese) .
- 4. Hong Q, Han W, Li J, et al. Molecular basis of receptor binding and antibody neutralization of Omicron. Nature. 2022; 604:546-552. [DOI] [PubMed] [Google Scholar]
- 5. Normand A, Marot M, Darnon C. Economic insecurity and compliance with the COVID-19 restrictions. Eur J Soc Psychol. 2022; 52:448-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Karako K, Song P, Chen Y, Karako T. Trends in managing COVID-19 from an emerging infectious disease to a common respiratory infectious disease: What are the subsequent impacts on and new challenges for healthcare systems? Biosci Trends. 2022; 16:381-385. [DOI] [PubMed] [Google Scholar]
- 7. National Health Commission. Notice on further optimization of the implementation of measures for the prevention and control of the COVID-19 epidemic (Issued on December 7, 2022). http://www.nhc.gov.cn/xcs/gzzcwj/202212/8278e7a7aee34e5bb378f0e0fc94e0f0.shtml (accessed January 19, 2023). (in Chinese) .
- 8. Publicity Division, National Health Commission. Transcript of a January 14, 2023 press conference by the State Council's Joint Prevention and Control Mechanism. http://www.nhc.gov.cn/xcs/s3574/202301/a68301ee500b436b989ec5be2a35cad2.shtml (accessed January 19, 2023). (in Chinese) .
- 9. Andrews N, Stowe J, Kirsebom F, et al. Covid-19 vaccine effectiveness against the Omicron (B.1.1.529) variant N Engl J Med. 2022; 386:1532-1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Accorsi EK, Britton A, Fleming-Dutra KE, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta variants. JAMA. 2022; 327:639-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chenchula S, Karunakaran P, Sharma S, Chavan M. Current evidence on efficacy of COVID-19 booster dose vaccination against the Omicron variant: A systematic review. J Med Virol. 2022; 94:2969-2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feikin DR, Higdon MM, Abu-Raddad LJ, et al. Duration of effectiveness of vaccines against SARS-CoV-2 infection and COVID-19 disease: Results of a systematic review and meta-regression. Lancet. 2022; 399:924-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Heath PT, Galiza EP, Baxter DN, et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021; 385:1172-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021; 384:403-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention. How to protect yourself and others. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed January 19, 2023).
- 16. Rappuoli R, Mandl CW, Black S, De Gregorio E. Vaccines for the twenty-first century society. Nat Rev Immunol. 2011; 11:865-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goldblatt D. SARS-CoV-2: from herd immunity to hybrid immunity. Nat Rev Immunol. 2022; 22:333-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bolotin S, Wilson S, Murti M. Achieving and sustaining herd immunity to SARS-CoV-2. CMAJ. 2021; 193:E1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chung H, He S, Nasreen S, et al. Effectiveness of BNT162b2 and mRNA-1273 covid-19 vaccines against symptomatic SARS-CoV-2 infection and severe covid-19 outcomes in Ontario, Canada: Test negative design study. BMJ. 2021; 374:n1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Our world in Data. Coronavirus (COVID-19 vaccination). https://ourworldindata.org/covid-vaccinations (accessed January 19, 2023).
- 21. Kaplan RM, Milstein A. Influence of a COVID-19 vaccine's effectiveness and safety profile on vaccination acceptance. Proc Natl Acad Sci U S A. 2021; 118:e2021726118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vergnes J-N. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2021; 384:1577. [DOI] [PubMed] [Google Scholar]
- 23. Thomas SJ, Moreira ED Jr, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine through 6 months. N Engl J Med. 2021; 385:1761-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Renner B, Reuter T. Predicting vaccination using numerical and affective risk perceptions: The case of A/ H1N1 influenza. Vaccine. 2012; 30:7019-7026. [DOI] [PubMed] [Google Scholar]
- 25. Lau JT, Yeung NC, Choi KC, Cheng MY, Tsui HY, Griffiths S. Factors in association with acceptability of A/ H1N1 vaccination during the influenza A/H1N1 pandemic phase in the Hong Kong general population. Vaccine. 2010; 28:4632-4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lai X, Zhu H, Wang J, et al. Public perceptions and acceptance of COVID-19 booster vaccination in China: A cross-sectional study. Vaccines (Basel). 2021; 9:1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. 2021; 97:107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Patone M, Mei XW, Handunnetthi L, et al. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation. 2022; 146:743-754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Patone M, Mei XW, Handunnetthi L, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022; 28:410-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hogan CM, Waselewski ME, Szachta P, Wolff C, Amaro X, Chang T. Perceptions of COVID-19 vaccine incentives among adolescents and young adults. JAMA Netw Open. 2022; 5:e2216628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fadda M, Suggs LS, Albanese E. Willingness to vaccinate against Covid-19: A qualitative study involving older adults from Southern Switzerland. Vaccine X. 2021; 8:100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Prickett KC, Habibi H, Carr PA. COVID-19 vaccine hesitancy and acceptance in a cohort of diverse New Zealanders. Lancet Reg Health West Pac. 2021; 14:100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Freeman D, Loe BS, Yu LM, et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. Lancet Public Health. 2021; 6:e416-e427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Soares P, Rocha JV, Moniz M, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel). 2021; 9:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chen F, Zhu S, Dai Z, et al. Effects of COVID-19 and mRNA vaccines on human fertility. Hum Reprod. 2021; 37:5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gutierrez S, Logan R, Marshall C, Kerns J, Diamond- Smith N. Predictors of COVID-19 vaccination likelihood among reproductive-aged women in the United States. Public Health Rep. 2022; 137:588-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Edelman A, Boniface ER, Benhar E, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: A U.S. cohort. Obstet Gynecol. 2022; 139:481-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Taşkaldıran I, Vuraloğlu E, Bozkuş Y, Turhan İyidir Ö, Nar A, Başçıl Tütüncü N. Menstrual changes after COVID-19 infection and COVID-19 vaccination. Int J Clin Pract. 2022; 2022:3199758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Matar SG, Nourelden AZ, Assar A, et al. Effect of COVID-19 vaccine on menstrual experience among females in six Arab countries: A cross sectional study. Influenza Other Respir Viruses. 2023; 17:e13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Du F, Chantler T, Francis MR, et al. The determinants of vaccine hesitancy in China: A cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. 2020; 38:7464-7471. [DOI] [PubMed] [Google Scholar]
- 41. Sage WM, Yang YT. Reducing "COVID-19 misinformation" while preserving free speech. JAMA. 2022; 327:1443-1444. [DOI] [PubMed] [Google Scholar]
- 42. Wang CS, Doma R, Westbrook AL, et al. Vaccine attitudes and COVID-19 vaccine intention among parents of children with kidney disease or primary hypertension. Am J Kidney Dis. 2023; 81:25-35. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Alexander JL, Kennedy NA, Ibraheim H, et al. COVID-19 vaccine-induced antibody responses in immunosuppressed patients with inflammatory bowel disease (VIP): A multicentre, prospective, case-control study. Lancet Gastroenterol Hepatol. 2022; 7:342-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang P, Li Y, Wang H, et al. COVID-19 vaccine hesitancy among older adolescents and young adults: A national cross-sectional study in China. Front Public Health. 2022; 10:877668. [DOI] [PMC free article] [PubMed] [Google Scholar]


