Abstract
Background
Falls are the leading cause of accidental injury among the elderly. Fall prevention is currently the main strategy to minimize fall-related injuries in at-risk older adults. However, the success of fall prevention programs in preventing accidental injury in elderly populations is inconsistent. An alternative novel approach to directly target fall-related injuries is teaching older adults movement patterns which reduce injury risk. The purpose of the current study will be to explore the feasibility and preliminary efficacy of teaching at-risk older adults safe-falling strategies to minimize the risk of injury.
Methods/design
The Falling Safely Training (FAST) study will be a prospective, single-blinded randomized controlled trial. A total of 28 participants will be randomly assigned to four weeks of FAST or to an active control group with a 1:1 allocation. People aged ≥65 years, at-risk of injurious falls, and with normal hip bone density will be eligible. The FAST program will consist of a standardized progressive training of safe-falling movement strategies. The control group will consist of evidence-based balance training (modified Otago exercise program). Participants will undergo a series of experimentally induced falls in a laboratory setting at baseline, after the 4-week intervention, and three months after the intervention. Data on head and hip movement during the falls will be collected through motion capture.
Discussion
The current study will provide data on the feasibility and preliminary efficacy of safe-falling training as a strategy to reduce fall impact and head motion, and potentially to reduce hip and head injuries in at-risk populations.
Registration
The FAST study is registered at http://Clinicaltrials.gov (NCT05260034).
Keywords: Falls, Accidental injury, Accident prevention, Aging, Elderly, Training
1. Introduction
Falls are the leading cause of accidental injury and injury-related death among older adults [1]. Approximately 28%–35% of community-dwelling people aged over 65 years fall at least once a year, and around 15% fall at least twice per year [2,3]. Falls are responsible for approximately 63% (2.5 million) of non-fatal injuries experienced by older adults that require emergency room treatment and hospitalization in the United States [4]. In addition, the number of annual fall-related injuries in the United States is expected to increase to 5.7 million by the year 2030 [5]. Despite the focus of scientific inquiry for decades [6], the number of fall-related deaths and injuries in older adults continues to increase [7,8]. Fall injury prevention approaches tend to focus on factors distal to the injury mechanism.
Fall-related injuries occur when an individual impacts the ground or other surface with sufficient force to cause tissue damage. For instance, fall-related traumatic brain injuries result from hitting the head on the ground or other surface with sufficient force to cause a disruption of brain function [9]. Public health programs aiming to prevent fall-related injuries have consistently employed strategies to reduce falls [10,11] and have not directly targeted the fundamental variable for injury prevention, namely, impact force [12]. Particularly, reducing the impact forces acting on the hip or head would be beneficial in decreasing the risk of severe injuries, such as hip fractures or traumatic brain injury. Nevertheless, current strategies to prevent fall-related injuries have primarily attempted to reduce impact forces indirectly, by either increasing bone strength or by using protective gear (i.e., hip protectors or helmets) [[13], [14], [15]] and/or compliant flooring [16,17]. Although these approaches have shown some promise, the evidence-base in terms of their effectiveness is very limited [18]. Indeed, a recent randomized controlled trial involving 5500 older adults at risk of falls found no group differences in fall-related injuries over three years after an intervention focusing on eight modifiable risk factors for injurious falls, compared to a standard of care control group [19]. The null result of this trial may be in part explained by the absence of a strategy to directly reduce impact forces.
An alternative approach that targets fall-related injuries by directly reducing impact forces is to teach older adults movement patterns that reduce fall-related impact forces, that is safe-falling techniques [20]. This alternative approach is bolstered by a recent analysis of over 2000 video recorded real-world falls in 658 long term care residents, which revealed that fall-related injuries were reduced when older adults rotated their body during descent [21]. A systematic review of 13 studies encompassing 219 individuals under 30 years of age identified seven safe-landing strategies and provided quantitative evidence indicating that these strategies can significantly reduce the risk of fall-related injury, as measured by kinetic or kinematic impact severity during a fall, in young and healthy individuals [22]. Importantly, previous studies, including our own, have shown the feasibility of teaching safe-falling strategies to older adults [23,24]. These investigations involved individuals over 60 years of age, who were taught movement strategies believed to reduce impact forces. Collectively, these studies revealed that older adults were able to 1) improve the mastery of such movement strategies [24], and 2) reduce the hip impact forces and head acceleration during experimentally induced falls [23]. Therefore, teaching safe-falling techniques may be an effective strategy to reduce fall-related injury in older adults. However, an implicit limitation of the existing literature is that, owing to safety reasons, only healthy older adults took part in studies involving safe-falling training. Therefore, it remains to be seen whether older adults who are at risk of falls may be able to safely learn protective movements and eventually apply these movements in real fall situations to minimize their risk of fall-related injuries.
The purpose of the current study will be to address this critical knowledge gap by exploring the feasibility and preliminary efficacy of a safe-falling training program in at-fall risk older adults. We hypothesize that, compared to controls undergoing a modified evidence-based fall-reduction intervention [25], those undergoing the FAlling Safely Training (FAST) intervention will show greater reduction in hip and head acceleration during experimentally induced falls (i.e., suggesting lower likelihood of injury) immediately post-training and at 3 months post-training. In addition, we hypothesize that, compared to controls, FAST participants will have minimally greater musculoskeletal discomfort, and no difference in training-related adverse events.
2. Methods
2.1. Study design
The study will be a prospective, single-blinded (assessor) randomized controlled trial (RCT) with two arms. A total of 28 participants (14 participants in each arm) will be recruited. Eligible participants will complete a baseline assessment (T1), a 4-week intervention, a post-training assessment testing motor skill acquisition (T2), and a follow-up assessment testing motor skill retention after three months (T3) (Fig. 1). Participants will complete experimentally induced falls during the baseline, post-training, and follow-up assessment. Each assessment session will be conducted by trained research staff blinded to group allocation and will take about 1.5 h.
Fig. 1.
Study design. Legend: FAST: Falling Safely Training.
Participants will be randomly assigned to the intervention group (FAST) or to the control group (i.e., based on the principles and practices of the Otago Exercise Program - OEP) [25]. The randomization sequence will be developed by a statistician and sealed envelopes will be used to conceal the randomization, which will take place after participants have completed the baseline assessment (T1). Participants in both groups will complete a total of eight supervised training sessions over the course of four weeks (two sessions per week). The instructor of the intervention group will be a trained researcher highly experienced in martial arts (Judo) and in conducting research in geriatric and frail populations (TZ). The instructor of the control group will be a certified physical therapist. Each training session will last 30 min.
The current study has been prospectively registered in ClinicalTrials.gov (Identifier: NCT05260034). The study protocol has received institutional review board (IRB) approval from the University of Kansas Medical Center (STUDY00147362), and therefore conforms to the ethical standards for medical research involving human subjects according to the 1964 Declaration of Helsinki and its later amendments. The IRB-approved informed consent document, summarizing the study details, is presented in Supplementary File 1.
2.2. Screening, eligibility criteria, and recruitment
Participants will be recruited from the local community and from the geriatric clinic at the Landon Center on Aging at the University of Kansas Medical Center through IRB-approved flyers. Social media posts will also be used to maximize recruitment online. People who are interested in the study will contact the research team by phone call, text, or email. A research coordinator will conduct a phone screening to preliminarily determine whether participants are eligible (Table 1). The phone screening was designed to exclude individuals who do not meet the study criteria before they are invited to attend an additional onsite screening. The onsite screening visit will be conducted at the University of Kansas Medical Center, where potential participants will undergo a Dual Energy X-ray Absorptiometry (DEXA) assessment (Table 1). In addition to the bone density assessment (DEXA), balance and cognition eligibility criteria will also be evaluated during this visit. All screening procedures will be performed in consultation with an MD geriatrician. Participants who meet the eligibility criteria will provide written informed consent during the onsite screening visit and will be scheduled for the baseline assessment.
Table 1.
Inclusion and exclusion criteria.
| Screening | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Phone screening | Age ≥65 years. | History of tumbling, gymnastics, or martial arts experience. |
| At-risk of injurious fall as indicated by: 1) positive history of fall-related injury in the last year, or 2) experience of more than two falls in the last year, or 3) concerns related to changes of balance or walking [19]. |
Currently performing ≥150 min per week of vigorous physical activity or physical therapy. | |
| Independent walking (i.e., no use of walking aids). | Unable to walk household distances unassisted. | |
| Normal or corrected vision and hearing. | At-risk of bleeding, or currently taking the anticoagulants (e.g., warfarin, apixaban, rivaroxaban, and enoxaparin). | |
| Able to speak and comprehend written and spoken English. | Previous fragility fracture of the hip, spine or wrist. | |
| Weight >350 lbs. | ||
| Onsite screening | Bone mineral density of the hip ≥ −2.3 (i.e., t score ≥ −2.3, assessed via Dual Energy X-ray Absorptiometry). | Cognitive impairment as indicated by Saint Louis University Memory Scale (SLUMS) < 25. |
| Balance impairment as indicated by performance <10 s on unipedal stance test [26]. |
2.3. Sample size
Sample size calculations were conducted using data obtained from our pilot RCT [23] to determine the required group enrollments to properly power the study. In the power calculation, power was set at .80 and the alpha level at 0.05. For acquisition, the effect size for hip impact force is a Cohen's d of 1.67 and for head acceleration d is 1.11. The required sample size to detect acquisition (i.e., a significant change) in hip impact is 4 and head acceleration is 7, in each group. For retention, the effect size Cohen's d is 1.94 for hip impact force and 1.38 for head acceleration. The required sample size to detect retention (i.e., a significant change) in hip impact is 4 and head acceleration is 5, in each group. Assuming a standard dropout rate of 20%, we propose to initially enroll 14 subjects/group (i.e., 28 in total), which should result in the required sample size, namely 11 subjects/group (i.e., 22 in total), after dropout.
2.4. Data collection methods and outcome measures
Table 2 summarizes the measures collected at different study visits. Socio-demographics and clinical characteristics will be collected as part of the onsite screening visit (T0). Measures of balance performance and confidence, and data pertaining to the execution of the experimentally induced falls will be collected through a series of standardized procedures during the assessment visits at baseline (T1), post-training (T2), and 3-month follow-up (T3). Safety and feasibility outcomes will be collected through the whole study.
Table 2.
Primary, secondary, and tertiary study outcomes.
| Information collected for all participants | T0 | T1 | In | T2 | T3 | O |
|---|---|---|---|---|---|---|
| Socio-demographics | ||||||
| Age, gender, marital status, race, height, weight, education, and occupation | ✓ | D | ||||
| Clinical characteristics | ||||||
| 12-month fall history | ✓ | D | ||||
| Bone mineral density of the hip, t score (Dual Energy X-ray Absorptiometry) | ✓ | D | ||||
| The Saint Louis University Mental Status | ✓ | D | ||||
| Balance performance and confidence | ||||||
| Berg Balance Scale | ✓ | ✓ | ✓ | T | ||
| The Activity-based Balance Confidence scale | ✓ | ✓ | ✓ | T | ||
| Performance of experimentally induced falls | ||||||
| Acceleration at hip impact and head impact | ✓ | ✓ | ✓ | P | ||
| Presence of head impacts during the experimental falls | ✓ | ✓ | ✓ | S | ||
| Safety and feasibility outcomes | ||||||
| Discomfort level – 11-point numerical rating scale and body chart | ✓ | ✓ | ✓ | ✓ | P | |
| Adverse events – defined by the NIH | ✓ | ✓ | ✓ | ✓ | P | |
| Attrition – defined as the number of patients withdrawing from the study | ✓ | ✓ | ✓ | ✓ | T | |
| Attendance to intervention – the proportion of the sessions attended | ✓ | ✓ | ✓ | ✓ | T | |
| Subjective feedback | ✓ | ✓ | ✓ | ✓ | T | |
Notes: ✓ = Examined in that session, T0 = Onsite screening visit, T1 = Baseline assessment, In = Intervention sessions, T2 = Acquisition and transfer assessment, T3 = Retention assessment.
O = Outcome measures, D = Demographics, S = Secondary, P = Primary, T = Tertiary.
During the assessment visits, participants will first complete the activity-specific balance confidence (ABC) scale and the Berg balance scale (BBS). The ABC is a short questionnaire to evaluate the balance confidence of older adults in completing different daily activities [27,28]. The score ranges from 0% (no confidence) to 100% (complete confidence) for each question (daily indoor or outdoor activity). The BBS is a widely utilized assessment to examine the static, dynamic and functional balance through 14 items relating to daily living activities [29]. Each item is scaled from 0 (failure to perform the task) to 4 (able to perform the task safely and independently). Higher scores are indicative of better balance. The BBS has established psychometric properties and has consistently shown responsiveness to balance training interventions [[29], [30], [31]].
Following the completion of balance assessments, participants will be asked to wear a unisuit before undergoing 10 min of whole-body stretching to minimize the risk of injury [23]. Whole body stretching will include the dynamic and static stretching of the neck (flexion, extension, and right/left lateral flexion), the upper trunk (shoulder rolls, arm extensions), and the lower limbs (quadriceps, hamstrings, and calves). Lower limb stretching will be performed in the sitting position if the participant's flexibility is limited. After the stretching session, participants will be equipped with protective gear including a light-weight helmet, hip protectors, and knee protectors to reduce the risk of injury during the experimentally induced falls.
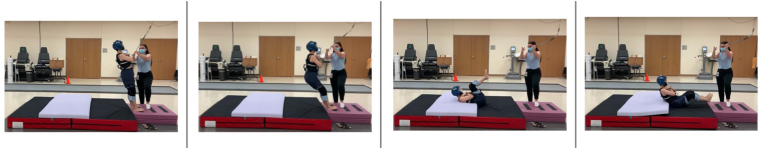
Participants will fall backwards and sideways (both left and right) onto a crash pad (Fig. 2). The setup shown in Fig. 2 consists of a body weight-supported system, an inextensible tether, a mechanical catch (a snap shackle), and a harness. The cushioning system consists of a 20-cm crash pad (Asana Drag Pad, Asana Climbing & MFG, Boise ID, USA) and an 8-cm foam pad, which will minimize the discomfort and risk of injury during the experimentally induced falls.
Fig. 2.
Experimentally induced falls (setup).
The falls will be caused by releasing the mechanical catch from the setup shown in Fig. 2. Participants will be instructed to lean backwards/sideways to more than 10° from the vertical position. It has been reported that sudden losses of balance from a 10° leaning angle cannot be recovered by taking a single step [32]. The leaning angle will be achieved by progressively adjusting the hook height of the body weight-supported system, until the participants are fully supported by the system. Once the participant has reached the required position, the mechanical catch will be released without countdown, and in a time ranging between 3 and 10 s. Prior to the fall, participants will be instructed to cross their arms in front of their chest to standardize the initial position, as well as to maximize safety (i.e., to minimize the chances that untrained individuals would fall on an outstretched hand) [23]. In addition, the following verbal instructions will be given: “land on the mat in a way that you feel comfortable with”. A total of six experimentally induced falls, including two backward falls, and four sideways falls (two left and two right), will be assessed. After each fall, participants will be allowed to rest as much as needed and will be asked to provide verbal consent before undergoing a new fall. Data collection will be stopped if participants indicate they wish to interrupt the assessment and/or if a suspected injury occurs. The order of the fall directions will be randomized. Each fall will be video recorded. Forward falls will not be assessed due to the excessive risk for head impacts and concerns for upper limb safety using our protocol (i.e., sudden release from an inclined position).
The occurrence of head impacts will be determined by reviewing the video of each fall. Two trained research staff will use the following standardized criteria to determine whether a head impact occurs: 1) the head makes contact with the mat, 2) the mat deforms as a result of the head impact, and 3) the head rebounds on the mat. Disagreements regarding the occurrence of a head impact will be resolved through group discussion by involving a third researcher [33]. In addition, the level of pain/discomfort and adverse events will be recorded following each fall. Discomfort will be assessed through an 11-point (0-10) numerical rating scale, which has shown strong validity and reliability in adult samples [34]. The locations of bodily discomfort (e.g., hip, shoulder, head, etc.) will be recorded on a standardized body chart. Adverse events, as defined by the National Institutes of Health (NIH), will also be recorded.
In addition to the video evaluations of falls, the kinematic data of the falls will also be collected by means of an eight-camera motion capture system (Cortex, MotionAnalysis Corp., Santa Rosa, USA) with a 100Hz sampling rate [23]. Five reflective markers will be attached on the helmet: one placed on top of the sagittal suture, two placed anteriorly over the frontal bone, and two placed posteriorly over the occipital bone. Six markers will be attached on the upper body: two placed on the spinous processes of the second (C2) and seventh cervical (C7) vertebrae, one on the chin, one on the jugular notch, and two on the left and right acromioclavicular joints. Twenty markers will be bilaterally attached on the lower body, including the anterior and posterior iliac spines, the greater trochanter, the medial and lateral femoral epicondyles, the lateral half shank, the medial and lateral malleolus, the head of the first hallux, and the calcaneus. One marker will also be attached on the shackle to capture the release of the mechanical catch. Supplemental Fig. 1 (Fig. S1) displays the marker set in a study participant, at the beginning of a backward fall, shown in sagittal view. The post-processing and analysis of kinematic data are further described in the section below.
2.5. Data post-processing and cleaning
Prior to post-processing, a trained researcher will manually label collected marker data in Cortex. To maximize accuracy, the markers occluded during falls will also be labeled based on the standardized interpolation methods within Cortex. Motion capture data will be converted to CSV format and analyzed via customized MatLab code. The impact of the head and hip will be calculated based on the second derivation of the marker location data using the formula below:
Where represent the location of each axis of the markers. The mid-point of the six markers on the head will be used to calculate head acceleration and the mid-point of the pelvis markers will be used to calculate hip acceleration. The peak value of the square root acceleration data will be determined. In addition, to ensure the motion capture yields accurate acceleration data, we will also record head and hip acceleration by means of a body-worn 9° of freedom inertial measurement unit (IMU) system (APDM. Inc., USA). Specifically, participants will wear three IMUs attached on the forehead, sternum, and lumbar area during the falls. The sampling rate of the IMUs will be set at 100Hz to match the motion capture system and the data will be synced by a trigger module to the motion capture system.
2.6. Interventions
2.6.1. FAST group
All training sessions will begin with a 10-min stretching session consisting of the following exercises from a sitting position on a chair: side rotation of the head, side head tilt, forward and backward head tilt, shoulder rolls, chest stretch, and hamstrings stretch. During each exercise, participants will be instructed to perform body movements slowly until reaching the desired stretching position and to hold a light stretch for a few seconds before returning to the initial position. Participants will perform three sets for each exercise. Following this standardized stretching protocol, participants will undergo 20 min of FAST training. The FAST program is a progressive safe-falling training performed on a cushioned mat (width: 3 m, length: 2.4 m, height: 5 cm) and based on adaptations of martial-arts tuck and roll strategies [22,23]. This program aims to teach how to effectively reduce impact forces during a fall by, 1) changing the trunk/knee angles during descent to decrease body acceleration, and 2) using a rolling movement to allow for an optimal distribution of impact forces applied to any site along the contact path. The FAST program consists of practicing self-initiated (i.e., voluntary) movements only and does not involve external perturbations and/or responding to sudden losses of balance. Participants will perform exercises involving rolling on the back in supine position (week 1), rolling on the back from sitting position (week 2), and rolling on the back from the kneeling position and/or from the standing position (week 3–4). Participants will receive visual demonstration by the trained researcher prior to practicing any of the required movements. The progression and description of the FAST program are fully detailed in Table 3. During the last training session, the trainer will use standardized criteria to evaluate to what extent participants have mastered the safe-falling techniques practiced during the program (Table 4). We also note that participants will progress to the last stage of training (weeks 3–4) only if they demonstrate adequate mastery of the intermediate motor skills, namely rolling on the back from the supine and sitting positions. An adequate level of mastery will be defined as scores ≥1 for the criteria Q5 and Q6 (Table 4). No pilot data to estimate how many individuals will be able to complete all stages of training is currently available. Therefore, we will record the proportion of participants who can effectively learn key intermediate motor skills for execution of the tuck and roll strategy during the FAST program. The potential occurrence of adverse events, as defined by the NIH, as well as the level of discomfort measured through a numerical rating scale [34] will be recorded during each training session.
Table 3.
The FAST program.
| Progression | Description | Exercises | Instructions |
|---|---|---|---|
| Week 1 | Exercises in the supine position. | Bring chin to chest. | Bend your legs, keep your arms out on the mat, and slowly bring your chin to the chest. |
| Slap arms on the mat. | Keep your chin tucked and use your arms, forearms and hands (palms down) to impact the mat 10 times. | ||
| Roll on your back. | bring your chin close to the chest, grab both your knees with your hands and roll back and forth. | ||
| Roll from side to side (right and left side). | Put one hand on your abdomen, roll sideways and use your arm and leg to stop the roll. Always keep your chin to the chest while you do this. | ||
| Week 2 | Exercises from a sitting position. | Roll on your back from a sitting position. | Bring your chin close to the chest, roll on your back, and use your arms to stop the fall. |
| Roll on your side from a sitting position (right and left side). | Put your left hand on your abdomen, bring your chin close to the chest, roll on the side, and use the right arm and leg to stop the fall. | ||
| Weeks 3–4 | Exercises from a kneeling/standing position. | Rolling backwards on the back from standing position. | Bring your chin to the chest, bend your knees, sit back and roll on your back. Use both arms to arrest the roll and keep your head up. |
| Rolling sideways on the back from kneeling position (right and left side). | Bring your chin to the chest, sit back and your (right or left) side, roll on your side and use your (right or left) arm and leg to arrest the roll. | ||
| * Rolling sideways on the back from standing position (right and left side). | Bring your chin to the chest, sit back and your (right or left) side, roll on your side and use your (right or left) arm and leg to arrest the roll. |
Notes: * Participants will practice rolling sideways from a standing position if they have any known knee joint conditions (e.g., osteoarthritis) or if they report any knee discomfort in the kneeling position. Two crash pads stacked on top of each other will be utilized for all exercises performed from the standing position.
Table 4.
Criteria for qualitative assessment (mastery) of the safe-falling techniques.
| Criteria | Scoring |
||
|---|---|---|---|
| 0 | 1 | 2 | |
| Q1. The body is relaxed during descent. | |||
| Q2. Body twists slightly during descent – participant lands on buttocks (for sideways falls only) | |||
| Q3. Squat during descent (knee and hip flexion) | |||
| Q4. Buttock lands softly with smooth rolling motion | |||
| Q5. Back is flexed during descent to maximize impact areas | |||
| Q6. Chin is kept tucked during descent | |||
Notes: Score = 0: criterion is not performed; Score = 1: criterion is partially performed; Score = 2: criterion is excellently performed.
2.6.2. Control group (OEP)
The control group will receive balance exercises adapted from the evidenced-based OEP [25]. A modified version of OEP, rather than no control intervention, was chosen to increase the level of evidence required to demonstrate efficacy, and because, similarly to the FAST training, it was designed to be performed individually or in small groups. Briefly, all eight OEP sessions will involve 30 min of balance and strength exercises using ankle weights. The difficulty of the exercises will progressively increase as performance improves by increasing resistance and/or the difficulty of the balance exercises (e.g., reducing the base of support). Analogously to FAST, the potential occurrence of adverse events, as defined by the NIH, as well as the level of discomfort measured through a numerical rating scale [34] will be recorded during each training session.
2.7. Statistical methods
To test the hypothesis that the FAST participants will show greater reduction in hip impact acceleration and head acceleration than the OEP participants immediately following the 4-week training, one-way analysis of variance (ANOVA) with the group (FAST vs. OEP) as the main factor will be used to compare the changes in these fall injury parameters. Changes in hip impact and head acceleration will be calculated as the difference from T2 to T1 for each respective measure. Separate analyses will be conducted on hip impact acceleration and head acceleration. To test the hypothesis that FAST participants will show greater reduction in hip impact force and head acceleration than OEP participants at 3 months post training, a similar ANOVA analysis will be conducted. Changes in ABC and BBS scores from T2 to T1, and from T3 to T1, will also be calculated and differences between groups will be explored through one-way ANOVAs. To test the hypothesis that there will be greater musculoskeletal discomfort in the FAST group compared to the OEP group, a two-sample independent t-test will be performed to compare the discomfort scale score at each assessment and training session. Additionally, a cross-tabulation of adverse events as a function of the group (FAST vs. OEP) will be analyzed to examine group differences in the frequency of training-related adverse events.
2.8. Data and safety monitoring
The current research project will comply with all NIH requirements and guidelines for data and safety monitoring boards (DSMBs). The appointed members of the DSMB will receive regular data reports at a schedule agreed upon by the members. In addition to reviewing the overall study protocol, the DSMB will also review the progress of trial (e.g., recruitment by ethnicity and sex, protocol deviations, adverse events, data quality, attrition, research outcomes) and make appropriate recommendations. Members of the study team will attend the DSMB meetings, which will take place with a frequency of at least once a year for the whole study duration.
2.9. Confidentiality
Participants’ confidentiality will be kept by performing informed consent, paperwork, and screening within the University of Kansas Medical Center. Participants will be assigned a unique study identification number, and all study forms will be de-identified. After the completion of the study, other researchers will have access to the de-identified study data. This will enable others to address additional questions and further investigate the results of the interventions.
2.10. Dissemination plan
The research team will publish the results of this research project in a peer reviewed journal. Researchers who have made intellectual contributions to the publication(s) will be listed in the authorship. The manuscripts will be subjected to rigorous review before they are submitted for publication. The research findings may also be presented at national and international conferences.
3. Discussion
Despite evidence that falls can be prevented in older adults, the number of fall-related injuries in this segment of the U.S. population have been increasing steadily over time [35]. Therefore, there is a critical need for innovative approaches that specifically aim to minimize fall-related injuries when falls cannot be avoided. Teaching older adults how to fall safely is a potentially cost-effective strategy to mitigate severe injuries such as traumatic brain injury and hip fractures. In this respect, previous studies have already highlighted the potential benefits of teaching older adults how to execute protective movements [23,24]. For instance, our pilot study involving healthy individuals aged between 55 and 75 years showed that participants who were taught a safe-falling technique were able to decrease hip acceleration by 33% and head acceleration by 54% after training [23]. However, there is a critical need for further research to examine the feasibility and preliminary efficacy of safe-falling training in older adults who are at high risk of fall-related injury.
The current project will address this critical knowledge gap and inform future, larger RCTs of the importance of safe-falling training as a strategy to reduce fall impact and head motion, and potentially to reduce hip and head injuries in at-risk populations. Importantly the current project will utilize a motor learning approach to evaluate the key stages of FAST mastery. In particular, the FAST program was designed with a partial backward chaining approach [36], namely a progressive step by step practice of protective movements taught backwards (i.e., from the final to the initial sequences of the motor task). This strategy has been successfully employed to teach older adults how to safely get up from the floor [36] and, in the current project, it will provide insights as to which aspects of FAST can and/or cannot be learned by at-risk older adults.
Potential problems of the current project will mainly consist of participant recruitment issues. Indeed, it is possible that older adults at risk of fall-related injury will be unwilling to participate in a safe-fall training program. In addition, injury or disinterest may prevent continued participation in the study. In this respect, we are going to incorporate stringent criteria for participants’ use of safety equipment to minimize the risk of injury. Further, should participants experience an injury, we will discontinue training, and will account for potential attrition through increased recruitment. Some methodological limitations of the proposed project should also be acknowledged. First, while we are setting out to investigate the preliminary efficacy of teaching safe-falling techniques as a strategy to minimize fall-related injury in older adults, all the study procedures will be performed in a controlled laboratory setting. Consequently, the study design will not allow us to fully understand whether learning to fall in the lab may translate into a better ability to fall safely in the real world. Analogously, the transferability of the learned safe-falling strategies to different falling scenarios will not be examined. For instance, due to the identical pre- and post-intervention testing paradigms, we will not be able to determine whether the FAST techniques can be used during unexpected balance perturbations. Second, our inclusion criteria aim to identify individuals at-risk of injurious fall, as indicated by: 1) positive history of fall-related injury in last year, or 2) experience of more than two falls in the last year, or 3) concerns related to changes of balance or walking (Table 1). While these inclusion criteria are based on a previous RCT aiming to decrease injury risk in older adults at-risk of injurious falls [19], we should at least acknowledge the possibility that participants meeting criterion 3 only may have a lower risk of falls compared to participants meeting criteria 1 and/or 2. Third, this study will predominately focus on examining the operational feasibility and safety of the FAST intervention rather than on the economic feasibility of FAST. Therefore, further research will be required to evaluate the cost-effectiveness of the proposed safe-falling program. In addition, it is possible that the proposed FAST training duration (four weeks, twice a week) may not be sufficient to observe an adequate mastery of the safe-falling techniques in the study participants. In this respect, the qualitative assessment (Table 4) will be critical to better understand whether the proposed intervention may benefit from additional training time and/or from additional training elements. Lastly, we should acknowledge that the sample size will be relatively small for this investigation. Although our sample size calculation suggests that the study will be adequately powered to detect changes in the main preliminary efficacy measures (i.e., hip and head acceleration), the relatively small sample may inflate the probability of committing a type two error when comparing differences in adverse events between the two groups.
Ultimately, the long-term vision of this research project is that the FAST program and/or adaptations of this safe-falling training could be implemented as part of current community-based fall-risk reduction programs, such as balance and resistance training, to not only reduce falls, but reduce fall-related injury when the falls cannot be absolutely prevented.
Funding
This work is supported by a research grant from the National Institutes of Health (1R21AG073892-01) awarded to JJS. The funders have no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CRediT authorship contribution statement
Tobia Zanotto: Conceptualization, Methodology, Investigation, Funding acquisition, Writing – Original Draft. Lingjun Chen: Methodology, Investigation, Visualization, Writing – Original Draft. James Fang: Methodology, Investigation, Visualization, Writing – Review & Editing. Shelley B. Bhattacharya: Methodology, Investigation, Project administration, Writing – Review & Editing. Neil B. Alexander: Conceptualization, Methodology, Project administration, Funding acquisition, Writing – Review & Editing. Jacob J. Sosnoff: Conceptualization, Methodology, Project administration, Funding acquisition, Writing – Original Draft.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2023.101133.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
Fig. S1.
Motion capture system: marker set in sagittal view (backward fall).
References
- 1.Grossman D.C., Curry S.J., Owens D.K., Barry M.J., Caughey A.B., Davidson K.W., Doubeni C.A., Jr Epling J.W., Kemper A.R., Krist A.H., Kubik M., Landefeld S., Mangione C.M., Pignone M., Silverstein M., Simon M.A., Tseng C.W. Interventions to prevent falls in community-dwelling older adults: US preventive services task force recommendation statement. JAMA. 2018;319:1696–1704. doi: 10.1001/jama.2018.3097. [DOI] [PubMed] [Google Scholar]
- 2.Stel V.S., Smit J.H., Pluijm S.M., Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. 2004;33:58–65. doi: 10.1093/ageing/afh028. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Ageing W.H.O., Unit L.C. 2008. Global Report on Falls Prevention in Older Age. [Google Scholar]
- 4.Centers for Disease Control and Prevention C Ten leading causes of non-fatal injury (charts) 2013. http://www.cdc.gov/injury/wisqars/LeadingCauses.html
- 5.Orces C.H., Alamgir H. Trends in fall-related injuries among older adults treated in emergency departments in the USA. Inj. Prev. 2014;20:421–423. doi: 10.1136/injuryprev-2014-041268. [DOI] [PubMed] [Google Scholar]
- 6.Gillespie L.D., Gillespie W.J., Robertson M.C., Lamb S.E., Cumming R.G., Rowe B.H. Interventions for preventing falls in elderly people. Cochrane Database Syst. Rev. 2003;4:CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- 7.Hartholt K.A., Lee R., Burns E.R., van Beeck E.F. Mortality from falls among US adults aged 75 Years or older, 2000-2016. JAMA. 2019;321:2131–2133. doi: 10.1001/jama.2019.4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burns E., Kakara R. Deaths from falls among persons aged ≥65 Years - United States, 2007-2016. MMWR Morb. Mortal. Wkly. Rep. 2018;67:509–514. doi: 10.15585/mmwr.mm6718a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor C.A., Bell J.M., Breiding M.J., Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017;66:1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montero-Odasso M.M., Kamkar N., Pieruccini-Faria F., Osman A., Sarquis-Adamson Y., Close J., Hogan D.B., Hunter S.W., Kenny R.A., Lipsitz L.A., Lord S.R., Madden K.M., Petrovic M., Ryg J., Speechley M., Sultana M., Tan M.P., van der Velde N., Verghese J., Masud T. Task force on global guidelines for falls in older adults, evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.38911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drahota A., Felix L.M., Raftery J., Keenan B.E., Lachance C.C., Mackey D.C., Markham C., Laing Ac A.C. The SAFEST review: a mixed methods systematic review of shock-absorbing flooring for fall-related injury prevention. BMC Geriatr. 2022;22:32. doi: 10.1186/s12877-021-02670-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groen B.E., Weerdesteyn V., Duysens J. The relation between hip impact velocity and hip impact force differs between sideways fall techniques. J. Electromyogr. Kinesiol. 2008;18:228–234. doi: 10.1016/j.jelekin.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Gillespie W.J., Gillespie L.D., Parker M.J. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst. Rev. 2010;10:CD001255. doi: 10.1002/14651858.CD001255.pub4. [DOI] [PubMed] [Google Scholar]
- 14.Leytin V., Beaudoin F.L. Reducing hip fractures in the elderly. Clin. Interv. Aging. 2011;6:61–65. doi: 10.2147/CIA.S10163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korall A.M.B., Feldman F., Yang Y., Cameron I.D., Leung P.M., Sims-Gould J., Robinovitch S.N. Effectiveness of hip protectors to reduce risk for hip fracture from falls in long-term care. J. Am. Med. Dir. Assoc. 2019;20:1397–1403.e1. doi: 10.1016/j.jamda.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Lachance C.C., Jurkowski M.P., Dymarz A.C., Robinovitch S.N., Feldman F., Laing A.C., Mackey D.C. Compliant flooring to prevent fall-related injuries in older adults: a scoping review of biomechanical efficacy, clinical effectiveness, cost-effectiveness, and workplace safety. PLoS One. 2017;12 doi: 10.1371/journal.pone.0171652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mackey D.C., Lachance C.C., Wang P.T., Feldman F., Laing A.C., Leung P.M., Hu X.J., Robinovitch S.N. The Flooring for Injury Prevention (FLIP) Study of compliant flooring for the prevention of fall-related injuries in long-term care: a randomized trial. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiel D.P., Magaziner J., Zimmerman S., Ball L., Barton B.A., Brown K.M., Stone J.P., Dewkett D., Birge S.J. vol. 298. 2007. pp. 413–422. (Efficacy of a Hip Protector to Prevent Hip Fracture in Nursing Home Residents: the HIP PRO Randomized Controlled Trial). [DOI] [PubMed] [Google Scholar]
- 19.Bhasin S., Gill T.M., Reuben D.B., Latham N.K., Ganz D.A., Greene E.J., Dziura J., Basaria S., Gurwitz J.H., Dykes P.C., McMahon S., Storer T.W., Gazarian P., Miller M.E., Travison T.G., Esserman D., Carnie M.B., Goehring L., Fagan M., Greenspan S.L., Alexander N., Wiggins J., Ko F., Siu A.L., Volpi E., Wu A.W., Rich J., Waring S.C., Wallace R.B., Casteel C., Resnick N.M., Magaziner J., Charpentier P., Lu C., Araujo K., Rajeevan H., Meng C., Allore H., Brawley B.F., Eder R., McGloin J.M., Skokos E.A., Duncan P.W., Baker D., Boult C., Correa-de-Araujo R., Peduzzi P. STRIDE trial investigators, A randomized trial of a multifactorial strategy to prevent serious fall injuries. N. Engl. J. Med. 2020;383:129–140. doi: 10.1056/NEJMoa2002183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh K.L., Sosnoff Jj J.J. A motor learning approach to reducing fall-related injuries. J. Mot. Behav. 2021;53:663–667. doi: 10.1080/00222895.2020.1814195. [DOI] [PubMed] [Google Scholar]
- 21.Robinovitch S.N., Dojnov A., Komisar V., Yang Y., Shishov N., Yu Y., Bercovitz I., Cusimano M.D., Becker C., Mackey D.C., Chong H H. Protective responses of older adults for avoiding injury during falls: evidence from video capture of real-life falls in long-term care. Age Ageing. 2022;51:afac273. doi: 10.1093/ageing/afac273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moon Y., Sosnoff J.J. Safe landing strategies during a fall: systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2017;98:783–794. doi: 10.1016/j.apmr.2016.08.460. [DOI] [PubMed] [Google Scholar]
- 23.Moon Y., Bishnoi A., Sun R., Shin J.C., Sosnoff J.J. Preliminary investigation of teaching older adults the tuck-and-roll strategy: can older adults learn to fall with reduced impact severity. J. Biomech. 2019;83:291–297. doi: 10.1016/j.jbiomech.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Arkkukangas M., Strömqvist Bååthe K., Ekholm A., Tonkonogi M. High challenge exercise and learning safe landing strategies among community-dwelling older adults: a randomized controlled trial. Int. J. Environ. Res. Publ. Health. 2022;19:7370. doi: 10.3390/ijerph19127370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell A.J., Robertson M.C., Gardner M.M., Norton R.N., Tilyard M.W., Buchner D.M. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065–1069. doi: 10.1136/bmj.315.7115.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobs J.V., Horak F.B., Tran V.K., Nutt J.G. Multiple balance tests improve the assessment of postural stability in subjects with Parkinson's disease. J. Neurol. Neurosurg. Psychiatry. 2006;77:322–326. doi: 10.1136/jnnp.2005.068742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Powell L.E., Myers A.M. The Activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50:28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 28.Schepens S., Goldberg A., Wallace M. The short version of the Activities-specific Balance Confidence (ABC) scale: its validity, reliability, and relationship to balance impairment and falls in older adults. Arch. Gerontol. Geriatr. 2010;51:9–12. doi: 10.1016/j.archger.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berg K.O., Maki B.E., Williams J.I., Holliday P.J., Wood-Dauphinee S.L. Clinical and laboratory measures of postural balance in an elderly population. Arch. Phys. Med. Rehabil. 1992;73:1073–1080. [PubMed] [Google Scholar]
- 30.Viveiro L.A.P., Gomes G.C.V., Bacha J.M.R., Carvas Junior N., Kallas M.E., Reis M., Jacob Filho W., Pompeu J.E. Reliability, validity, and ability to identity fall status of the Berg balance scale, balance evaluation systems test (BESTest), mini-BESTest, and brief-BESTest in older adults who live in nursing homes. J. Geriatr. Phys. Ther. 2019;42:E45–E54. doi: 10.1519/JPT.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 31.Lesinski M., Hortobágyi T., Muehlbauer T., Gollhofer A., Granacher U. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports Med. 2015;45:1721–1738. doi: 10.1007/s40279-015-0375-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hsiao E.T., Robinovitch S.N. Elderly subjects' ability to recover balance with a single backward step associates with body configuration at step contact. J Gerontol A Biol Sci Med Sci. 2001;56:M42–M47. doi: 10.1093/gerona/56.1.m42. [DOI] [PubMed] [Google Scholar]
- 33.Wood T.A., Moon Y., Sun R., Bishnoi A., Sosnoff J.J. Age-related differences in head impact during experimentally induced sideways falls. BioMed Res. Int. 2019;2019 doi: 10.1155/2019/6804614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K., Krebs E.E., Turk D., Von Korff M., Bair M.J., Allen K.D., Sandbrink F., Cheville A.L., DeBar L., Lorenz K.A., Kerns R.D. Core outcome measures for chronic musculoskeletal pain research: recommendations from a veterans health administration work group. Pain Med. 2019;20:1500–1508. doi: 10.1093/pm/pny279. [DOI] [PubMed] [Google Scholar]
- 35.Bergen G., Stevens M.R., Burns E.R. Falls and fall injuries among adults aged ≥65 Years - United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016;65:993–998. doi: 10.15585/mmwr.mm6537a2. [DOI] [PubMed] [Google Scholar]
- 36.Leonhardt R., Becker C., Groß M., Mikolaizak A.S. Impact of the backward chaining method on physical and psychological outcome measures in older adults at risk of falling: a systematic review. Aging Clin. Exp. Res. 2020;32:985–997. doi: 10.1007/s40520-019-01459-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.