Abstract
Background
Odontogenic glandular cyst (GOC) is one of the uncommon cysts of the jaws with difficult diagnosis due to the presence of many clinical and histopathological overlaps with other odontogenic lesions, and the definitive diagnosis is only possible by histological examination. It is initially asymptomatic and affects the anterior mandible with no gender predilection. Surgical resection is the preferred treatment due to the high rate of recurrence. To date, there are less than 200 documented cases worldwide.
Case presentation
A 33-year-old female patient who consulted the Department of Oral and Maxillofacial Surgery due to numbness and swelling. She has no medical history with medications or genetic diseases. The lesion was diagnosed as an odontogenic glandular cyst, and then treated with surgical resection and plate-and-screw replacement.
Clinical discussion
Odontogenic Glandular cyst is an uncommon cyst it is difficult to diagnose depending on clinical features and radiographic imaging only, the definitive diagnosis is based on histological examination. The preferred treatment is surgical resection with safety edges.
Conclusion
More care should be given to report this rare entity to assure accurate and early diagnosis.
Keywords: Glandular odontogenic cysts, Sialo-odontogenic cyst, Botryoid, Difficulty diagnosing
Highlights
-
•
The glandular cyst is radiologically similar to many dental lesions, like some cysts and tumors.
-
•
The high recurrence rate makes surgical resection the preferred treatment for this lesion.
-
•
The confirmed diagnosis of this lesion exclusively by histological examination
-
•
Usually, the preferred site for this lesion is the anterior mandibular, unlike the case in our hands.
-
•
Unusually, there were neurological symptoms, like numbness without pain in our patient.
1. Introduction
Glandular odontogenic cyst (GOC) is a rare developmental odontogenic cyst, which was firstly described in 1987 by Padayachee and Van Wyk as a “botryoid” odontogenic cyst with glandular component called “sialo-odontogenic cyst” [1].
Later in 1988, Gardner et al. proposed the term “glandular odontogenic cyst” that was adopted by WHO in 1992 [2], and the odontogenic origin of this cyst has been confirmed by immunohistochemistry [3].
Clinically, GOCs usually presents as an asymptomatic in small sizes, slow-growing with a preferred location in the anterior region of mandible, although some cysts reach large sizes, which leads to swelling in the jaw, paresthesia and numbness in the area (14–24 %) of cases are like this in our hands [4], [5]. It occurs over a wide age range, with most cases diagnosed in the 5–7th decade and there is no preference for one gender [5], still some studies have shown a tendency for males [6].
Radiologically, GOC presents as a unilocular cystic lesion(62–76 %) and sometimes multilocular [4], with well-defined margins, which occasionally may show loss of cortical integrity and root resorption, sometimes it is associated with unerupted teeth [5], [7], [8].
Histologically, the diagnosis of GOCs can be difficult, due to the rarity of the lesion and the fact that the differential diagnosis includes both benign and malignant lesion, starting from “innocent” radicular cysts, dentigerous cysts with/without metaplastic changes, some types of ameloblastoma, to worse lesions such as low-grade mucoepidermoid carcinoma (MEC) [9], [10], [11]. GOCs appear under microscope with nonkeratinized stratified squamous lining epithelium with focal thickening (plaques) in the cystic lining, eosinophilic, cuboidal or columnar cells that are referred as hobnail cells, and sometimes, these cells may be ciliated [12], mucous cells, and interepithelial gland-like structures [1], [2], [10].
As for the treatment, several approaches has been applied in the literature include conservative methods, such as enucleation with or without curettage, peripheral ostectomy and chemical cauterization with Carnoy's solution, marsupialization to some oppressive methods, such as marginal resection/ partial jaw resection [13] due to higher rate of recurrence around 21–55 % [8], [14], [15].
To the best of our knowledge there are about 200 cases of GOC, without neoplastic transformation at the expense of lining epithelial, are reported in the literature till end of 2022. There is a strong predilection to the mandible (80 %), especially the anterior mandible [8]. Also, less than quarter of the cases were associated with symptoms [5]. Here we present another rare case of a 33-year-old female patient, was in posterior mandibular with neurological symptoms which was written according to SCARE criteria [16].
2. Case report
A 33-year-old woman consulted the department of oral and maxillofacial surgery in General Assembly of Damascus Hospital suffering from swelling in her left mandible.
The swelling was gradual, non- painful and started 3 months ago in her left mandible. The Patient denied any history of pain, fever or trismus, but in the last few days she reported that she had mild numbness in the left lower lip. She did not suffer from any psychiatric or genetic diseases, and had no history with any specific medications.
On clinical examination, she had lower facial swelling in left mandible. The mass was hard and non-tender to palpation, there were no palpable masses in the neck and no cervical lymphadenopathy.
By the radiographic examination (OPG), there was large multilocular radiolucent lesion with well-defined borders. The lesion extended from left mandibular lateral incisor to medial aspect of lower left second molar (Fig. 1). On the clinical and radiographic characteristics, differential diagnosis included: odontogenic keratocyst, central giant cell granuloma and multi-cystic ameloblastoma.
Fig. 1.
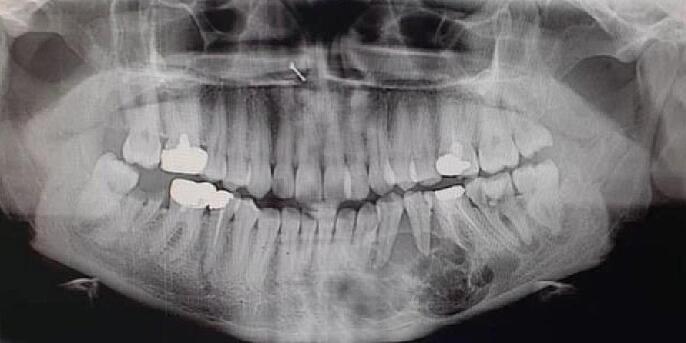
Patient's orthopantomogram (OPG) showing extension of lesion.
After the nasal and endotracheal intubation, injection was done in the working area of lidocaine with vasoconstrictor. Extra-oral sub-mandibular approach was done on left mandible and all covering tissues were elevated to isolate bone defect. Resection of bone is achieved approximately 1.5–2 cm beyond the radiological limit of the lesion. In our case we followed step design for the lower border of the mandible to get more bone bulk for reconstruction plate and screws (Fig. 2). Reconstruction plate was retained in place by screws (Fig. 3) to re-establish the normal contour of the mandible. The sample was fixed in formaldehyde solution and sent directly to oral maxillofacial pathology service for histological examination.
Fig. 2.
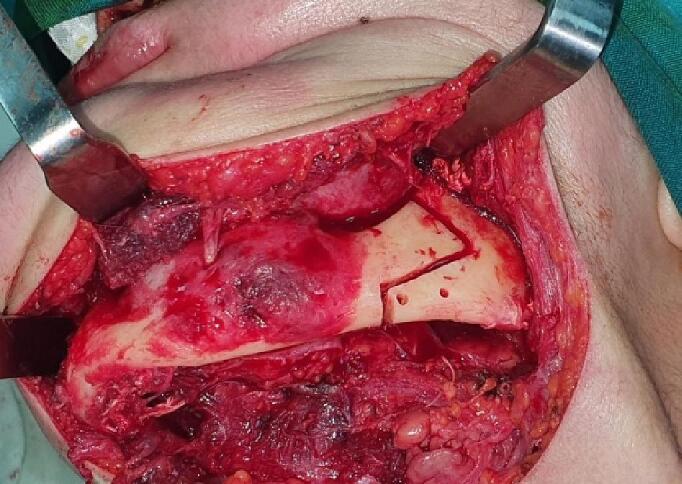
Surgical cut design.
Fig. 3.
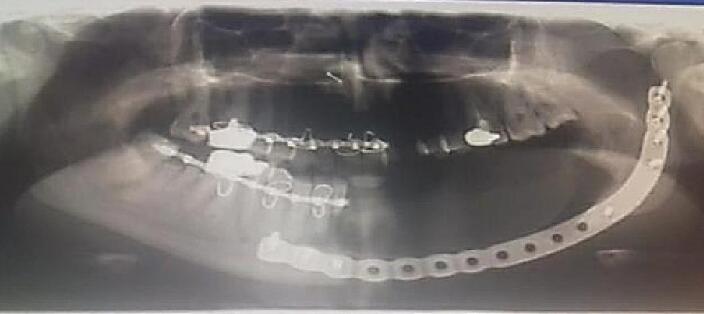
Installing the reconstruction plate in place.
The specimen was a soft tissue biopsy from a radiolucent lesion in the left mandibular body, measured 35X20X08 mm. upon cutting no abnormal structure or noodles could be detected, a clear cystic structure was still observed (Fig. 4, Fig. 5).
Fig. 4.

Clinical view of the lesion after excision.
Fig. 5.

The stage of cutting and preparing the wax block.
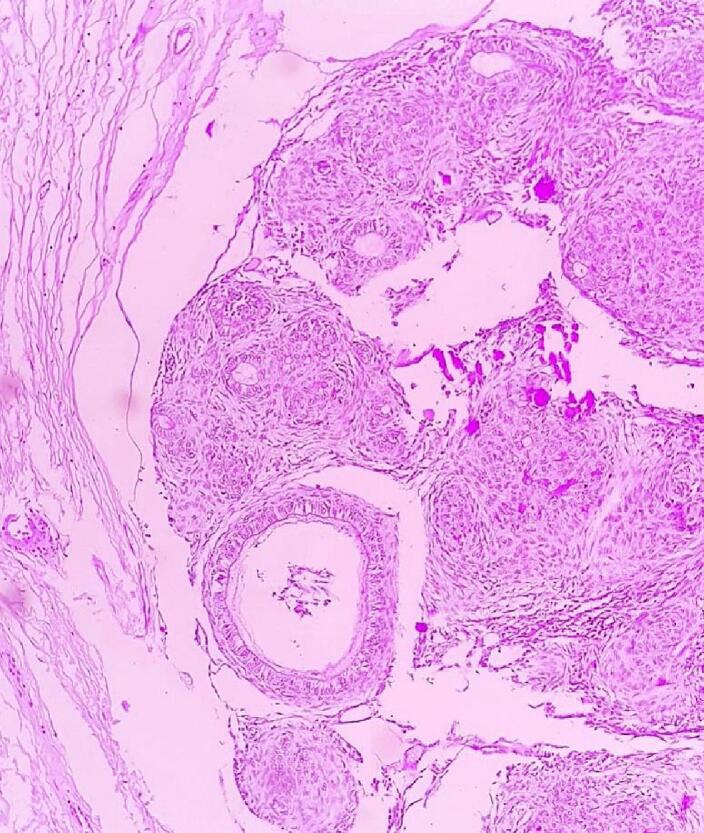
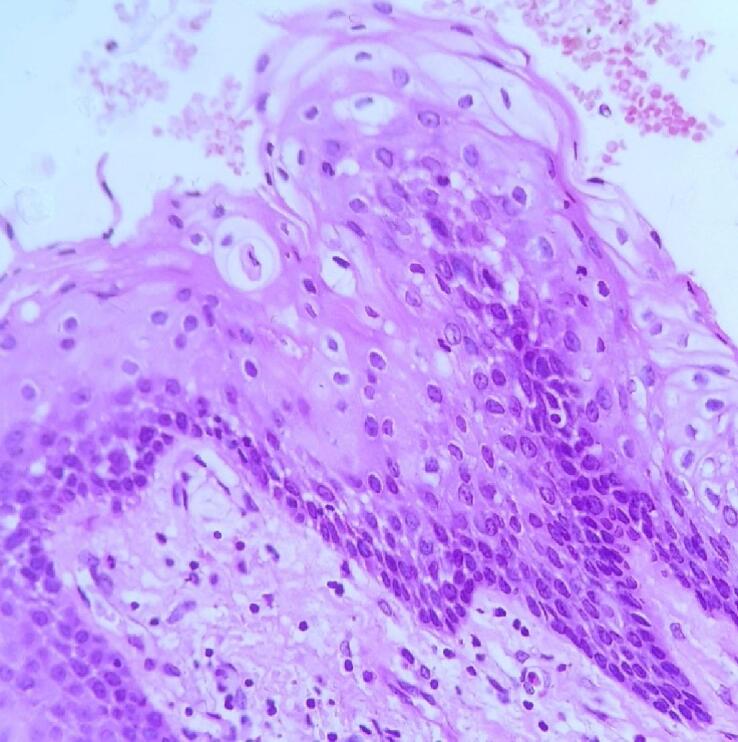
Microscopically, the surgical biopsy showed cystic cavity lined by a Non-keratinized stratified squamous odontogenic epithelium with variable thickness and clear cells (Fig. 6), within the epithelium, glandular structure was easily detected (Fig. 7), as well as intraepithelial duct-like spaces lined by a single layer of cuboidal to columnar cells, there was also some mucosal contents positive for PAS staining (Fig. 8). Few small micro cysts can also be seen within the epithelium (Fig. 9).
Fig. 6.
Cystic cavity lined by nonkeratinized stratified squamous epithelium, variable thickness and clear cells (H&E, ×100).
Fig. 7.

Photomicrography showing epithelium and glandular structure and clear cells (H&E, ×100).
Fig. 8.
Lining epithelium showing duct-like spaces and some mucosal contents (PAS, ×100).
Fig. 9.
Lining epithelium showing few clear cells, and microcystic space (H&E, ×400).
3. Discussion
Glandular odontogenic cysts are a rare entity accounting for about 0.012 % to 1.3 % of all jaw cysts [14], difficult-to-diagnose that needs integrating histopathological criteria to confirm its diagnosis, because of the large number of differential diagnoses that include many benign and malignant lesions, and the few numbers of them archived globally (to be exact 169 cases until 2017) [4], about 200 cases until 2022. These lesions were most common in males compared to females with predilection for anterior mandible [4]. It occur usually between the fifth and seventh decades of life, but in our case the patient was in the early fourth decade, on the other hand, the lesion in our study affected a female and included most of the body of left mandible. Usually, asymptomatic swelling is the most common clinical presentation, followed by pain, and sometimes numbness [5], experienced by the patient in our case. Its recurrence rate is about 35.9 %, especially when choosing a conservative surgical treatment [10]. Some authors have also reported that larger lesions have a higher recurrence rate [3]. Therefore, the decision was made to use surgical resection as a treatment to avoid recurrence, given the large size of the lesion. Since this lesion involves most of the body of the mandible, the case has been followed up for 6 months so far and there is no indication of recurrence. However, the patient should be kept under follow-up for at least 3 years [17].
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Patient perspective
Patient was quite happy with the surgical procedure and overall treatment.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Ethical approval has been exempted because this is a case report and no new studies or new techniques were carried out.
Funding
We have no sponsors.
Guarantor
Prof. Dr. Nabil Kochaji.
Research registration number
This paper is case report. The authors don't need to register this work.
CRediT authorship contribution statement
Prof. Dr. Nabil Kochaji: pathological study and paper writing
Dr. Sulieman Alhessani: literature review and paper editing
Dr. Sami Ibrahim and Dr. Ali Al-Awad: surgical procedure and patient follow up.
Declaration of competing interest
Authors have no conflicts of interest.
Acknowledgements
None.
References
- 1.Padayachee A., Van Wyk C. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J. Oral Pathol. Med. 1987;16(10):499–504. doi: 10.1111/j.1600-0714.1987.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 2.Kramer I.R., Pindborg J.J., Shear M. The WHO histological typing of odontogenic tumours. A commentary on the second edition. Cancer. 1992;70(12):2988–2994. doi: 10.1002/1097-0142(19921215)70:12<2988::aid-cncr2820701242>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 3.Poudel P., et al. Glandular odontogenic cyst—report of a rare case. Clin. Case Rep. 2020;8(2):351–354. doi: 10.1002/ccr3.2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chrcanovic B.R., Gomez R.S. Glandular odontogenic cyst: an updated analysis of 169 cases reported in the literature. Oral Dis. 2018;24(5):717–724. doi: 10.1111/odi.12719. [DOI] [PubMed] [Google Scholar]
- 5.Ferreira J.C.B., et al. Glandular odontogenic cyst in dentigerous relationship: an uncommon case report. Case Rep. Dent. 2019;2019:8647158. doi: 10.1155/2019/8647158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah A.A., et al. Glandular odontogenic cyst: a diagnostic dilemma. Indian J. Dent. 2016;7(1):38–43. doi: 10.4103/0975-962X.179371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tambawala S.S., et al. Glandular odontogenic cyst: a case report. Imaging Sci. Dent. 2014;44(1):75–79. doi: 10.5624/isd.2014.44.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Regezi J.A., Sciubba J.J., Jordan R.C. Elsevier Health Sciences; 2016. Oral Pathology: Clinical Pathologic Correlations. [Google Scholar]
- 9.Mascitti M., et al. Glandular odontogenic cyst: review of literature and report of a new case with cytokeratin-19 expression. Open Dent. J. 2014;8:1–12. doi: 10.2174/1874210601408010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan I., Anavi Y., Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis. 2008;14(7):575–581. doi: 10.1111/j.1601-0825.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 11.Fowler C.B., et al. Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011;5(4):364–375. doi: 10.1007/s12105-011-0298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shear M., Speight P.M. John Wiley & Sons; 2008. Cysts of the Oral and Maxillofacial Regions. [Google Scholar]
- 13.Faisal M., Ahmad S.A., Ansari U. Glandular odontogenic cyst - literature review and report of a paediatric case. J. Oral Biol. Craniofac. Res. 2015;5(3):219–225. doi: 10.1016/j.jobcr.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krishnamurthy A., et al. Glandular odontogenic cyst: report of two cases and review of literature. Head Neck Pathol. 2009;3(2):153–158. doi: 10.1007/s12105-009-0117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyrio M.C., et al. Treatment of mandibular glandular odontogenic cyst with immediate reconstruction: case report and 5-year follow-up. Br. J. Oral Maxillofac. Surg. 2010;48(8):651–653. doi: 10.1016/j.bjoms.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Agha R.A., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 17.Chandolia B., Bajpai M., Arora M. Glandular odontogenic cyst. J. Coll. Physicians Surg. Pak. 2017;27(3):S23–S25. [PubMed] [Google Scholar]



