Abstract
Aims
Care needs represent an essential paradigm in planning residential facility (RF) interventions. However, possible disagreements between users and staff are critical issues in service delivery. The Experience Sampling Method (ESM) tracks experiences in the real world and real time. This study aimed to evaluate the care needs of patients with schizophrenia spectrum disorder (SSD) in RFs and its association with daily activities and mood monitored using the ESM.
Methods
As part of the DIAPASON project, 313 residents with SSD were recruited from 99 Italian RFs. Sociodemographic and clinical characteristics were recorded. Care needs, the severity of symptomatology and negative symptoms were assessed. Fifty-six residents were also assessed for 7 consecutive days using the mobile ESM. Descriptive, agreement, predictor and moderator analyses were conducted.
Results
The staff rated a higher number of total and met needs than service users (p < 0.001). Only a slight agreement between users and staff on unmet needs was found in self-care (k = 0.106) and information (k = 0.100) needs, while a moderate agreement was found in accommodation (k = 0.484), food (k = 0.406), childcare (k = 0.530), physical health (k = 0.470), telephone (k = 0.458) and transport (k = 0.425) needs. Older age (−0.15; p < 0.01), longer SSD diagnosis (−0.16; p < 0.01), higher collaboration (−0.16; p < 0.01) and lower symptomatology (−0.16; p < 0.01) decreased the number of unmet needs, while being a female (0.27; p < 0.05) and a shorter length of stay in an RF (0.54; p < 0.001) increased the number of unmet needs. A higher number of unmet needs was associated with a lower amount of time spent in leisure activities or reporting a positive mood: on the contrary, more unmet needs were associated with a greater amount of time spent in religious or non-productive activities. The associations between unmet needs rated by staff and users and momentary mood as assessed using the ESM were not moderated by the severity of symptomatology.
Conclusions
Although care needs are fundamental in planning residential activities aimed at recovery-oriented rehabilitation, RF interventions did not fully meet users' needs, and some disagreements on unmet needs between users and staff were reported. Further efforts are necessary to overcome Italian RF limits in delivering rehabilitative interventions defined by real users' needs to facilitate users' productivity and progress towards personal recovery.
Keywords: Community mental health, epidemiology, psychiatric services, schizophrenia
Introduction
The concept of mental health need has been suggested as a vital paradigm in planning mental health service interventions (Lasalvia et al., 2000) because it has direct treatment implications. Different definitions of mental health need have been suggested (Ruggeri et al., 2004), such as the public mental health need, assessed to provide services, programmes and staff to address this need, or the need for treatment of patients in specific mental health settings (e.g. a patient discharged from a psychiatric hospitalisation or receiving community psychiatric treatment). Furthermore, different assessment tools have been developed (Lasalvia et al., 2007; Campion et al., 2017; Mazzaia, 2018; Norman et al., 2018; Reisinger et al., 2021). In this study, we focus on the ‘need for care’, which indicates a perceived problem in a health or social domain of life (Ruggeri et al., 2004), as assessed by staff and patients with schizophrenia spectrum disorder (SSD) using the Camberwell Assessment of Need (CAN) to investigate a comprehensive range of health and social needs (Wennström and Wiesel, 2006).
A growing body of evidence has shown that mental health professionals and users may have different perceptions of needs for care (Slade et al., 1998; Brunt and Hansson, 2002; Ochoa et al., 2003). Patients and staff may disagree on both the presence of a need for care and on whether a need has or has not been met (Lasalvia et al., 2000; Cleary et al., 2006; Grinshpoon et al., 2008; Wiersma et al., 2009; Eklund and Ostman, 2010; de Girolamo et al., 2020). The disagreement between patients and professionals is a critical issue for service delivery, and any effort should be made to improve strategies aimed at increasing consensus between staff and patients, as a better staff–patient agreement may help improve treatment outcomes (Lasalvia et al., 2008).
Several studies have found an association between higher needs for care and specific sociodemographic variables, such as having a disability with severe symptomatology and low social functioning (Ruggeri et al., 2004). Moreover, needs for care are a better predictor of quality of life than clinical or sociodemographic variables, and are associated with patient-reported satisfaction with care (Ådnanes et al., 2019).
The Experience Sampling Method (ESM) tracks experiences in the real world and real-time (Granholm et al., 2008; Wee et al., 2019; Myin-Germeys and Kuppens, 2022) using self-reports to capture momentary experiences and their context. To date, several studies have used ESM in patients with SSD to evaluate daily mood or symptomatology (Myin-Germeys et al., 2001; Cho et al., 2017; Granholm et al., 2020); however, very few have used this methodology for assessing daily life activities of people with SSD (van Os et al., 2014; Kluge et al., 2018; Granholm et al., 2020; Culbreth et al., 2021). To the best of our knowledge, only van Os et al. (2014) have explicitly examined the association between needs for care evaluated via CAN and ecological indices monitored using the ESM in individuals with psychosis (Janney et al., 2013; van Os et al., 2014). They found an association between psychotic experiences and unmet needs moderated by negative affect (higher levels increased the number of unmet needs), positive affect (higher levels decreased the number of unmet needs) and environmental stress associated with events and activities (higher levels increased the number of unmet needs).
Community care in Italy is organised through 127 Departments of Mental Health that provide direct outpatient, hospital and residential care. In addition, many residential facilities (RFs) are managed by private (both non-profit and for-profit) organisations. All patients treated in private RFs are fully covered by the National Health Service for their stay and care. Previous studies have thoroughly assessed the residential care system (de Girolamo et al., 2002, 2005; Santone et al., 2005; Picardi et al., 2014).
RFs in Italy admit patients with SSD who have increased needs for care, severe psychopathology and low functioning (de Girolamo et al., 2002; Ministero Italiano della Salute, 2013; Martinelli et al., 2022a, 2022b), and who would have been hospitalised for a long time in a psychiatric hospital before de-institutionalisation (de Girolamo et al., 2002; Thornicroft and Tansella, 2004; McPhearson et al., 2018). RFs represent a fundamental component of long-term care and aim to support users in learning or relearning daily living skills and gaining confidence to achieve social inclusion, independent living and personal recovery (UN General Assembly, 2006; Priebe et al., 2009; Martinelli and Ruggeri, 2020a; Raugh et al., 2021), and to cover all adult roles (Ruggeri et al., 2004; Kimhy et al., 2014; McPhearson et al., 2018).
Despite the importance of RFs in Italian community mental health care after the early reform of psychiatric hospitals (Basaglia, 1968; Becker and Fangerau, 2018), they have not been surveyed for approximately 20 years (Culbreth et al., 2021). Furthermore, indeed the mission of Italian RFs to implement strategies aimed at developing rehabilitation activities oriented to the personal recovery ethos in order to increase personal daily life skills and well-being, and based on the real needs for care of residents (Junghan et al., 2007; Grinshpoon et al., 2008; Killaspy, 2016), no studies have investigated the association between needs for care and daily life activities in a sample of residents with SSD, in detail, using the ESM.
In the current study, we aimed to assess the needs for care as perceived by residents with SSDs and their key professionals, evaluate the agreement between users and staff perceptions of unmet needs, and identify sociodemographic and clinical predictors of unmet needs. Moreover, we aimed to address the gap in the literature by identifying unmet need predictors of daily activities and momentary mood as assessed using the ESM and investigating the interaction between symptomatology, momentary mood and unmet needs for care.
Materials and methods
This study is part of the national project ‘DAily time use, Physical Activity, quality of care and interpersonal relationships in patients with Schizophrenia spectrum disorders (DIAPASON)’ (de Girolamo et al., 2020).
The DIAPASON project included 20 Departments of Mental Health and 17 private RFs in different Italian regions.
The inclusion criteria were: age between 20 and 55 years old, a DSM-5 diagnosis of SSD (American Psychiatric Association, 2013) and speaking and writing in the Italian language to participate adequately in a research interview. The exclusion criteria were: severe cognitive deficits (i.e. a Mini-Mental State Examination corrected score of <24), inability to provide informed consent, a recent (last 6 months) DSM-5 diagnosis of substance use disorder (American Psychiatric Association, 2013), a cerebrovascular/neurological disease and a history of clinically significant head injury.
In the participating RFs, the facility chiefs prepared an alphabetical list of patients with SSD on an index day, and based on this list, residents were consecutively invited to participate in the study until the recruitment target was achieved. From October 2020 to October 2021, 340 residents with SSD were recruited from 98 (public and private) RFs across Italy (12.8 ± 5.7 residents). Six patients (1.8%) were excluded due to severe cognitive deficits, and 21 (6.2%) dropped out after providing informed consent. A total of 313 patients were included in this study. Each RF recruited a mean of 3.5 (± 2.6) residents. Therefore, based on the total number of occupied beds, we recruited approximately 27% of the patients from each participating RF. The sample size calculation is described in detail in the study protocol (de Girolamo et al., 2020).
Due to logistic and financial limitations, the ecological ESM study was possible only in a sub-sample of RFs (N = 30); in these RFs, 56 (17.9%) residents were assessed using the ESM.
Assessment of needs for care
Needs for care were assessed using the Italian version of the CAN (Phelan et al., 1995; Ruggeri et al., 1999), an interview developed for patients (CAN-P) and staff (CAN-S), comprising 22 items divided into five domains: health (physical health, psychotic symptoms, drugs, alcohol, safety to self, safety to others and psychological distress), basic (accommodation, food and daytime activities), social (sexual expression, social networks and intimate relationships), service (information, telephone, transport and benefits) and functioning (basic education, money, childcare, self-care and looking after the room). Each item was assessed on a three-point scale with 0 = no problem, 1 = no/moderate problem because of interventions (met need), and 2 = current serious problem (unmet need).
Users and their corresponding key professionals completed the two CAN versions in separate interviews.
Assessment of the severity of symptomatology
The 24-item Brief Psychiatric Rating Scale (BPRS) (Overall and Gorham, 1962; Morosini and Casacchia, 1995) was used to assess symptom severity. The BPRS items were rated on a seven-point Likert scale ranging from 1 (no symptoms) to 7 (extremely severe symptoms) and divided into five categories (depression/anxiety, excitement, positive symptoms, negative symptoms and cognitive symptoms). The Brief Negative Symptom Scale (BNSS) (Strauss et al., 2012; Mucci et al., 2015) was used to assess the severity of negative symptoms. The BNSS items were rated on a six-point Likert scale ranging from 0 (no symptoms) to 6 (severe symptoms), and they evaluated blunted affect, alogia, asociality, anhedonia and avolition. For both the BPRS and BNSS, higher total mean scores indicated more severe symptomatology.
Assessment of daily time use and emotions
Daily time use (i.e. daily activities) and emotions were assessed using a questionnaire on a smartphone-based application for ESM, developed ad hoc for the project (see the mobile application for ESM in online Supplementary materials). The mobile application comprised three sections: current activities, social contacts and mood. The first section asked, ‘What are you doing right now’? The participants could choose one or more of the following activity categories: sleeping; staying sick in bed; eating/self-care working; studying, doing housework; taking care of someone or something; voluntary working; doing leisure activities, thinking, resting, or doing nothing, performing sports or physical activity; getting around watching television or listening to the radio; and participating in religious activities (see list of daily activities in the online Supplementary Table 1).
The second section asked, ‘Who are you with right now’? and the participants could choose ‘alone’ or ‘with other people’. The third section showed seven mood conditions (happy, sad, tired, relaxed, nervous, quiet and full of energy) and asked the participants how they felt at that moment. The participants had to push on the screen and select the measure of that mood on a bar from 0 (not at all) to 100 (a lot).
Notifications appeared eight times a day, from 8:00 a.m. to 12:00 p.m., for 7 consecutive days. The notifications were semi-randomised (i.e. randomly sent within the scheduled time slots) in the following time slots: 8–10 a.m., 10 a.m.–12 p.m., 12 p.m.–2 p.m., 2–4 p.m., 4–6 p.m., 6–8 p.m., 8–10 p.m., 10 p.m.–12 a.m. A reminder notification appeared after 15 min. The participants had a maximum of 30 min to reply.
Statistical analysis
Data were analysed using SAS, SPSS and R (R Core Team, 2013; SAS Institute Inc, 2013; IBM Corp. Released, 2020). Descriptive statistics comprised frequency tables for categorical variables and mean (standard deviation [SD]) for continuous variables. We tested the hypothesis of normality of continuous variables using the Kolmogorov–Smirnov test. To assess differences between matched user-rated and staff-rated needs for care, we used Wilcoxon's signed-rank test (because the variables were not normally distributed).
In addition to the number of needs (total, met and unmet), the met/unmet ratio was computed. Focusing only on unmet needs, we investigated the agreement between CAN-P and CAN-S on the total, domains and items using Cohen's k coefficient. According to Landis and Koch, the agreement is poor with k < 0.00, slight with k = 0.00–0.20, fair with k = 0.21–0.40, moderate with k = 0.41–0.60, substantial with k = 0.61–0.80 and almost perfect with k = 0.81–1.00 (McHugh, 2012).
To understand if the number of unmet needs (total and domains) could be associated with daily activities, we used generalised linear models (GLM) adjusted for age, sex and the BPRS total score.
With an additional statistical model, we tested the interaction between mood ratings collected through the ESM (momentary negative and positive mood considered as independent variables), the level of symptomatology severity (assessed through the BPRS, considered as a moderator) and unmet needs (both user-rated and staff-rated, considered as dependent variables).
To understand which clinical and/or sociodemographic factors could be associated with the difference between the unmet needs rated by the staff and users, we used GLM. Finally, as an external validation of our sample, we compared (through confidence intervals) the recorded percentages of unmet needs with those reported in similar previous studies (see online Supplementary Tables 2 and 3).
Results
Sociodemographic characteristics of the residents
As shown in Table 1, the users had a mean age of 41.0 years (s.d. = 9.7), and most users were males (70.3%), single (86.9%) and unemployed (83.3%). The mean length of mental disorder was 18.3 years (s.d. = 9.6), and they mostly had spent more than 5 years in the RF (43.9%).
Table 1.
Socio-demographic and clinical characteristics of 313 residents of Italian RFs
| N | % | |
|---|---|---|
| Sex | ||
| Males | 220 | 70.3 |
| Females | 93 | 29.7 |
| Age (years) | ||
| Mean (s.d.) | 41.0 | (9.7) |
| Marital status | ||
| Single | 271 | 86.9 |
| Married or cohabiting | 13 | 4.2 |
| Divorced or widowed | 28 | 9.0 |
| Education level | ||
| Elementary/junior high school | 132 | 42.4 |
| Secondary school/university degree | 179 | 57.6 |
| Working statusa | ||
| Working | 38 | 12.2 |
| Studying | 14 | 4.5 |
| Not working | 260 | 83.3 |
| Length of mental disorder (years) | ||
| Mean (s.d.) | 18.3 | (9.6) |
| Length of stay in the rf (years) | ||
| <1 | 53 | 39.1 |
| 1–5 | 122 | 17.0 |
| >5 | 137 | 43.9 |
| Support system | ||
| Family/friends highly collaborative | 72 | 23.1 |
| Family/Friends interested but not supportive | 134 | 42.9 |
| Family/friends potentially available | 50 | 16.0 |
| Lack of social support | 56 | 18.0 |
| Collaboration skills | ||
| Actively seek treatment, willing to collaborate | 131 | 42.0 |
| Wants to be helped, but lacks motivation | 104 | 33.3 |
| Passively accepts the treatment/intervention | 45 | 14.4 |
| Does not show attention or comprehension of treatment efforts | 29 | 9.3 |
| Actively refuses the treatment/intervention | 3 | 1.0 |
| BPRS score (range 1–7) | Mean | s.d. |
| Depression/anxiety | 2.3 | (0.9) |
| Excitement | 1.8 | (0.9) |
| Positive symptoms | 2.4 | (1.0) |
| Negative symptoms | 2.3 | (1.1) |
| Cognitive symptoms | 1.8 | (0.9) |
| Total score | 2.1 | (0.7) |
| BNSS score (range 0–6) | ||
| Anhedonia | 2.1 | (1.6) |
| Distress | 2.2 | (1.8) |
| Asociality | 2.2 | (1.5) |
| Avolition | 2.1 | (1.6) |
| Blunted affect | 1.9 | (1.6) |
| Alogia | 1.7 | (1.6) |
| Total score | 2.0 | (1.3) |
‘Working’ includes ‘full-time or part-time job in a protected environment’ and ‘protected environment job’. ‘Studying’ includes ‘job training course’, ‘student’. ‘Not working’ includes ‘housemaker’, ‘unemployed or looking for their first job’ and ‘retired who does not carry out any remuneration activity’ (including those who benefit from the invalidity pension).
Most patients' family/friends were available but not actively supportive (42.9%). Most users actively sought treatment (42%) or wanted to be helped but lacked motivation (33.3%). A few users (9.6%) performed no activities in the RFs, while the main activities performed were housekeeping (63.5%) and cleaning up (12.3%). The severity of symptomatology was mild (BPRS, mean total score 2.1 [range: 1–7; s.d. = 0.7] and BNSS, mean total score 2.0 [range: 0–6; s.d. = 1.3]) (Table 1).
Differences in total, met and unmet needs between users and staff
The staff reported a significantly higher number of needs for care (p < 0.001) and met needs (p < 0.001) than users in all domains, except socially met needs (p = 0.138). Both the users and staff found the highest number of needs for care in health (users: 1.7; s.d. = 1.2 v. staff: 2.6; s.d. = 1.3) and the lowest in service (users: 0.9; s.d. = 0.9 v. staff: 1.0; s.d. = 1.0) (Table 2).
Table 2.
Differences in total, met and unmet needs among 313 residents with SSD
| User-rated mean (s.d.) | Staff-rated mean (s.d.) | p* | |
|---|---|---|---|
| Health | |||
| Number of needs | 1.7 (1.2) | 2.6 (1.3) | <0.001 |
| Met needs | 1.2 (1.1) | 1.9 (1.3) | <0.001 |
| Unmet needs | 0.5 (0.8) | 0.7 (0.9) | <0.001 |
| Ratio met/unmet | 2.4 | 2.7 | |
| Basic | |||
| Number of needs | 1.3 (1.0) | 1.9 (1.0) | <0.001 |
| Met needs | 1.0 (0.9) | 1.5 (1.0) | <0.001 |
| Unmet needs | 0.2 (0.5) | 0.4 (0.7) | <0.001 |
| Ratio met/unmet | 5.0 | 2.5 | |
| Social | |||
| Number of needs | 1.1 (1.0) | 1.4 (1.0) | <0.001 |
| Met needs | 0.5 (0.6) | 0.5 (0.7) | 0.138 |
| Unmet needs | 0.6 (0.9) | 0.9 (1.0) | <0.001 |
| Ratio met/unmet | 0.8 | 0.6 | |
| Service | |||
| Number of needs | 0.9 (0.9) | 1.0 (1.0) | 0.003 |
| Met needs | 0.6 (0.8) | 0.8 (0.8) | <0.001 |
| Unmet needs | 0.3 (0.6) | 0.3 (0.5) | 0.154 |
| Ratio met/unmet | 2.0 | 2.7 | |
| Functioning | |||
| Number of needs | 1.2 (1.1) | 2.1 (1.2) | <0.001 |
| Met needs | 1.0 (1.0) | 1.6 (1.1) | <0.001 |
| Unmet needs | 0.2 (0.6) | 0.5 (0.9) | <0.001 |
| Ratio met/unmet | 5.0 | 3.2 | |
| Total | |||
| Number of needs | 6.1 (3.6) | 9.0 (3.8) | <0.001 |
| Met needs | 4.2 (2.8) | 6.3 (3.1) | <0.001 |
| Unmet needs | 1.9 (1.8) | 2.7 (2.7) | <0.001 |
| Ratio met/unmet | 2.2 | 2.3 | |
Scoring of CAN items: 0 = no problem, 1 = no/moderate problem because of continuing interventions (met need) and 2 = current serious problem whether or not help is offered or given (unmet needs ratio ⩾ 1 indicates a proportion between met and unmet needs in favour of met needs). Bold values denote statistical significance at the p < 0.05 level.
The overall ratio was similar between the two groups (total: users 2.2 v. staff 2.3). The highest differences in the ratio among the users and staff were found in basic (ratio: users 5.0 v. staff 2.5) and functioning (ratio: users 5.0 v. staff 3.2) needs (Table 2).
Percentage of agreement on unmet needs between users and staff
Of the 313 user–staff pairs included in the analyses, 175 (55.9%) of the user–staff pairs reported unmet needs (Table 3). The highest number of unmet needs was reported by the staff and users in social (98; 31.3) needs, while the lowest was in functioning needs for users (55; 17.6) and service needs for the staff (68; 21.7) (Table 3).
Table 3.
Number of unmet needs (rating 2) identified by patients, staff and patient ± staff pairs and total percentage agreement for each can item
| CAN categories | User-rated unmet needs N (%) | Staff-rated unmet needs N (%) | User/staff-rated pairs of unmet needs N (%) | Total percentage agreement (k di Cohen) |
|---|---|---|---|---|
| Total | 202 (64.5) | 239 (76.4) | 175 (55.9) | 0.313 |
| Basics | 62 (19.8) | 100 (32.0) | 40 (12.8) | 0.330 |
| Accommodation | 28 (9.0) | 32 (10.2) | 16 (5.1) | 0.484 |
| Food | 22 (7.0) | 39 (12.5) | 14 (4.5) | 0.406 |
| Daytime activities | 26 (8.3) | 59 (18.9) | 16 (5.1) | 0.295 |
| Social | 125 (39.9) | 171 (54.6) | 98 (31.3) | 0.373 |
| Company | 69 (22.0) | 122 (39.0) | 48 (15.3) | 0.308 |
| Intimate relationships | 69 (22.0) | 99 (31.6) | 45 (14.4) | 0.373 |
| Sex life | 55 (17.6) | 53 (16.9) | 25 (8.0) | 0.351 |
| Functioning | 55 (17.6) | 101 (32.3) | 41 (13.1) | 0.386 |
| Basic education | 1 (0.3) | 6 (1.9) | 1 (0.3) | 0.282 |
| Money | 35 (11.2) | 59 (18.9) | 21 (6.7) | 0.357 |
| Childcare | 8 (2.6) | 14 (4.5) | 6 (1.9) | 0.530 |
| Self-care | 9 (2.9) | 32 (10.2) | 3 (1.0) | 0.106 |
| Living environment | 20 (6.4) | 46 (14.7) | 10 (3.2) | 0.235 |
| Health | 101 (32.3) | 141 (45.1) | 76 (24.3) | 0.404 |
| Physical health | 18 (5.8) | 18 (5.8) | 9 (2.9) | 0.470 |
| Psychotic symptoms | 44 (14.1) | 95 (30.4) | 32 (10.2) | 0.332 |
| Drugs | 0 | 4 (1.3) | 0 | |
| Alcohol | 1 (0.3) | 3 (1.0) | 0 | |
| Safety to self | 12 (3.8) | 5 (1.6) | 2 (0.6) | 0.218 |
| Safety to others | 2 (0.6) | 5 (1.6) | 1 (0.3) | 0.279 |
| Psychological distress | 71 (22.7) | 85 (27.2) | 42 (13.4) | 0.387 |
| Services | 77 (24.6) | 68 (21.7) | 38 (12.1) | 0.381 |
| Information | 27 (8.6) | 13 (4.2) | 3 (1.0) | 0.100 |
| Telephone | 13 (4.2) | 20 (6.4) | 8 (2.6) | 0.458 |
| Transport | 30 (9.6) | 36 (11.5) | 16 (5.1) | 0.425 |
| Benefits | 27 (8.6) | 13 (4.2) | 8 (2.6) | 0.364 |
We did not find any substantial or almost perfect agreement on unmet needs between staff and users. The highest agreement was moderate for accommodation (k = 0.484), food (k = 0.406), childcare (k = 0.530), physical health (k = 0.470), telephone (k = 0.458) and transportation (k = 0.425). A slight agreement was found in self-care (k = 0.106), where mental health professionals rated lower than patients, and information (k = 0.100), where mental health professionals rated higher than patients. A fair agreement was found for the other CAN items (Table 3).
Predictors of differences of unmet needs between users and staff
As shown in online Supplementary Table 3, negative associations were found between the following variables: social unmet needs and age (older age decreased the number of unmet needs) (β = −0.15; p < 0.01), length of mental health disorder (longer diagnosis of SSD decreased the number of unmet needs) (β = −0.16; p < 0.01), functioning unmet needs and collaboration skills (higher collaboration decreased the number of unmet needs) (β = −0.16; p < 0.01), BPRS (lower symptomatology decreased the number of unmet needs) (β = −0.17; p < 0.01), total unmet needs and collaboration skills (higher collaboration decreased the number of unmet needs) (β = −0.12; p < 0.05) and BPRS (shorter symptomatology decreased the number of unmet needs) (β = −0.16; p < 0.01).
Positive associations were found between unmet health needs and sex (being a female increased the number of unmet needs) (β = 0.27; p < 0.05), social unmet needs and length of stay in the RF (shorter length of stay in the RF increased the number of unmet needs), particularly when the length of stay was <1 year (β = 0.54; p < 0.001) and between 1 and 5 years (β = 0.36; p < 0.1) (online Supplementary Table 4).
User-rated and staff-rated unmet need predictors of activities and momentary mood as measured using the ESM
As shown in Table 4, among the predictors, negative associations were similarly found in users and staff between leisure activities and health (users: β = −0.22; p < 0.05 v. staff: β = −0.33; p < 0.05) and total unmet needs (users: β = −0.29; p < 0.05 v. staff: β = −0.11; p < 0.05) (higher number of unmet needs decreased leisure activities); positive mood and unmet health needs (users: β = −0.41; p < 0.001 v. staff: β = −0.32; p < 0.05). Only for users, there was a negative association between leisure activities and social (β = −0.29; p < 0.05) and service unmet needs (β = −0.28; p < 0.05) (higher number of unmet needs decreased leisure activities), and positive mood and total unmet needs (β = −0.62; p < 0.001) (higher number of unmet needs was associated with lower positive mood). Only for the staff, there was a negative association between leisure activities and basic needs (β = −0.41; p < 0.05) (a higher number of unmet needs decreased leisure activities).
Table 4.
User-rated (CAN-P) and staff-rated (CAN-S) domains unmet needs as predictors of activities and momentary mood (negative and positive affect) as measured with ESM
| Dependent variables | ||||||||
|---|---|---|---|---|---|---|---|---|
| Predictors* | Non-productive activities | Productive activities | Leisure activities | Physical activities | Self-care | Religious activities | Positive affect | Negative affect |
| User-rated (CAN-P) | ||||||||
| Basic | 0.07 (−0.16; 0.30) | −0.17 (−0.39; 0.06) | 0 (−0.22; 0.23) | −0.03 (−0.26; 0.20) | 0.01 (−0.22; 0.24) | 0.03 (−0.20; 0.26) | −0.02 (−0.26; 0.21) | −0.05 (−0.28; 0.18) |
| Social | −0.01 (−0.28; 0.27) | −0.25 (−0.52; 0.01) | −0.29* (−0.56; −0.03) | −0.25 (−0.51; 0.02) | −0.11 (−0.38; 0.17) | −0.22 (−0.49; 0.05) | −0.26 (−0.53; 0.01) | 0.08 (−0.20; 0.35) |
| Functioning | 0.27** (0.08; 0.47) | −0.09 (−0.31; 0.12) | −0.06 (−0.27; 0.15) | −0.15 (−0.35; 0.06) | 0.01 (−0.20; 0.22) | −0.13 (−0.34; 0.08) | −0.16 (−0.37; 0.05) | 0.20 (−0.01; 0.41) |
| Health | 0.14 (−0.06; 0.34) | −0.13 (−0.33; 0.07) | −0.22* (−0.41; −0.03) | −0.13 (−0.33; 0.07) | 0.05 (−0.16; 0.25) | −0.09 (−0.29; 0.11) | −0.41*** (−0.59; −0.24) | 0.38*** (0.21; 0.56) |
| Services | 0.17 (−0.10; 0.44) | 0.10 (−0.17; 0.37) | −0.28* (−0.54; −0.02) | 0.07 (−0.20; 0.34) | 0.02 (−0.26; 0.30) | 0.09 (−0.18; 0.37) | −0.15 (−0.91; 0.25) | 0.04 (−0.23; 0.31) |
| Total | 0.23 (−0.01; 0.46) | −0.21 (−0.44; 0.03) | −0.29* (−0.52; −0.07) | −0.19 (−0.43; 0.04) | 0 (−0.24; 0.25) | −0.14 (−0.38; 0.10) | −0.40*** (−0.62; −0.18) | 0.29* (0.07; 0.52) |
| Staff-rated (CAN-S) | ||||||||
| Basic | 0.07 (−0.16; 0.30) | −0.03 (−0.46; 0.40) | −0.41* (−0.82; −0.01) | 0.26 (−0.16; 0.67) | 0.10 (−0.33; 0.53) | 0.45* (0.04; 0.86) | −0.21 (−0.64; 0.22) | 0.19 (−0.23; 0.62) |
| Social | 0.13 (−0.16; 0.41) | −0.14 (−0.43; 0.15) | −0.04 (−0.33; 0.24) | −0.09 (−0.37; 0.20) | 0.07 (−0.22; 0.36) | −0.08 (−0.37; 0.21) | −0.12 (−0.41; 0.17) | 0.22 (−0.06; 0.50) |
| Functioning | 0.39* (0.04; 0.73) | 0.13 (−0.23; 0.49) | −0.16 (−0.51; 0.19) | 0.20 (−0.16; 0.55) | 0.02 (−0.34; 0.38) | 0.18 (−0.18; 0.53) | −0.25 (−0.60; 0.11) | 0.21 (−0.14; 0.57) |
| Health | 0.20 (−0.10; 0.50) | −0.17 (−0.47; 0.14) | −0.33* (−0.62; −0.04) | −0.11 (−0.42; 0.19) | 0.27 (−0.03; 0.57) | −0.06 (−0.37; 0.25) | −0.32* (−0.62; −0.02) | 0.39** (0.10; 0.68) |
| Services | −0.32 (−0.97; 0.32) | −0.18 (−0.83; 0.47) | −0.43 (−1.06; 0.21) | 0.25 (−0.39; 0.90) | 0.26 (−0.39; 0.91) | 0.34 (−0.30; 0.99) | 0.25 (−0.41; 0.90) | 0.02 (−0.62; 0.67) |
| Total | 0.08 (−0.03; 0.19) | −0.04 (−0.15; 0.07) | −0.11* (−0.22; −0.01) | 0.02 (−0.10; 0.13) | 0.06 (−0.05; 0.18) | 0.04 (−0.07; 0.15) | −0.09 (−0.20; 0.02) | 0.12* (0.01; 0.23) |
A linear regression, adjusted for age, sex and BPRS (standardised coefficients), was undergone. Bold values denote statistical significance at *p < 0.05 **p < 0.01 ***p < 0.001 level.
A positive association in both user and staff ratings was found between non-productive activities and functioning (users: β = 0.27; p < 0.01 v. staff: β = 0.39; p < 0.05) (higher number of unmet needs were associated to higher non-productive activities), negative mood and health (users: β = 0.38; p < 0.001 v. staff β = 0.39; p < 0.01) and total unmet needs (users: β = 0.29; p < 0.05 v. staff: β = 0.12; p < 0.05) (higher number of unmet needs was associated with more negative mood). Only in staff ratings was there a positive association between religious activities and basic needs (β = 0.45; p < 0.05) (a higher number of unmet needs increased religious activities) (Table 4).
Association between momentary mood (as assessed using the ESM) and user-rated and staff-rated unmet needs at different levels of the BPRS
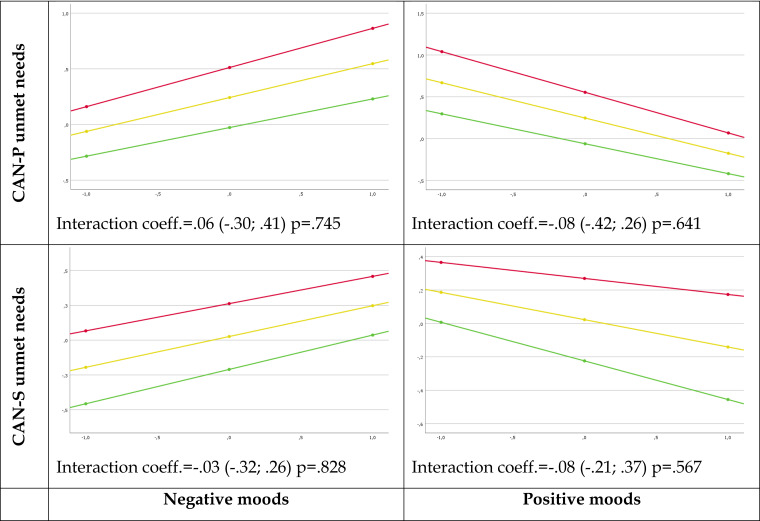
As shown in Fig. 1, a higher number of user-rated and staff-rated unmet needs negatively influenced users' positive moods and positively influenced users' negative moods. However, the associations between user-rated and staff-rated unmet needs and momentary mood (negative and positive), as assessed using the ESM, were not moderated by the level of severity of symptomatology, as assessed using the BPRS (negative mood and number of unmet needs in CAN-P [interaction coefficient = 0.06 (−0.30; 0.41), p = 0.745], and CAN-S [interaction coefficient = −0.03 (−0.32; 0.26), p = 0.828]; positive mood and the number of unmet needs in both CAN-P [interaction coefficient = −0.08 (−0.42; 0.26), p = 0.641] and CAN-S [interaction coefficient = −0.08 (−0.21; 0.37), p = 0.567]).
Figure 1.
Plot of the simple slope analysis for the moderator variable BPRS: association between mood ratings (positive affect and negative affect as assessed with ESM) and user-rated (CAN-P) and staff-rated (CAN-S) unmet needs at different severity levels of BPRS (the lowest symptomatology severity: green line, intermediate symptomatology severity: yellow line, the highest symptomatology severity: red line).
Discussion
This was the first study to investigate the association between needs for care and ecological indices, as assessed using the ESM, in residents with SSD. We confirmed the sociodemographic and clinical characteristics of similar samples from previous surveys (de Girolamo et al., 2002; Martinelli et al., 2022b). Our findings reveal that users who were younger, females, with the most severe symptomatology, the shortest length of stay in an RF or without collaborative behaviour were the most likely to report unmet needs in social, functioning and health areas. This feature might be related not only to the natural course of SSD with reduced symptoms and increased psychosocial functioning when patients are more collaborative, but also to the process of ‘institutionalisation’ (Wennström and Wiesel, 2006; SAS Institute Inc, 2013; Martinelli et al., 2019) which implies limitations in their social reintegration in society. The longer their stay in an RF, the higher the risk of being socially isolated (Federici et al., 2009; Gold, 2014; Martinelli et al., 2022a).
Our findings reveal that the agreement between users and professionals concerning needs for care (Phelan et al., 1995) is currently a challenge for Italian RFs. Moderate agreement was reported in areas where it was easier to allocate resources, such as housing and daytime activities (Werner, 2012), which represent the most frequent activities carried out by the residents of our sample. The slight agreement on self-care, which usually represents one of the main objectives in RFs, might be due to an overestimation of self-care by users with SSD, who frequently have negative symptoms which may impair their body perception and lead to neglecting personal hygiene (Goldstone, 2020). Furthermore, although the staff reported that patients were adequately informed about their disorder and ongoing treatments, users evaluated this information as not comprehensive. This might be due to staff overestimation of their communication skills or to the effect of self-stigma in patients' reticence about asking for more information (Lanfredi et al., 2015; Winkler et al., 2017; Atwoli and Muhia, 2021). The finding of a relatively close agreement on unmet needs concerning social life (sex life in particular) was somewhat surprising, considering that this area may otherwise be challenging to investigate (Ruggeri et al., 2004). However, the highest unmet needs in social areas domain confirmed (Eklund and Ostman, 2010; Gold, 2014) that few services are able to fulfil personal and subjective needs. A moderate disagreement was reported between staff and users on functioning, probably because most residents collaborated in the rehabilitative programme, which positively balanced the number of unmet needs in this area.
Most users performed some kinds of activity in the RF. However, the increase in unmet needs influenced the level of performed activity. In particular, the lack of productive activities strongly correlated with high unmet needs in functioning, while leisure activities seemed to be the first activities not performed when there was an overall increase in unmet needs, particularly in physical and psychological health, social life, media and transport.
Higher levels of met needs in physical and psychological health were associated with an increase in positive mood. Furthermore, a higher number of unmet needs were negatively associated with the fulfilment of everyday productive activities. These features may hinder the achievement of users' recovery because the lesser the user is active, motivated to pursue a productive activity, and proactive, the lesser they will have to cover all adult roles, live independently and be socially integrated (Argentzell et al., 2020).
Interestingly, our findings reveal that the association between mood and unmet needs is not moderated by the severity of symptomatology, leading us to conclude that needs for care, and particularly unmet needs, represent an important feature to be considered when planning residential interventions, independent of the severity of symptoms (Grinshpoon and Ponizovsky, 2008; Oorschot et al., 2012; Salisbury et al., 2016).
Strengths and limitations
A major strength of this study is the use of the ESM, which allows the collection of longitudinal, prospective data in real-time, reducing reporting biases and acquiring information that cannot be easily observed or monitored in daily life.
The possible assessment bias due to staff socio-demographics was reduced thanks to a comprehensive staff training on the use of the CAN and other assessment tools.
Although residents with SSD represent most of those living in RFs (Starace et al., 2017), these findings cannot be generalised to residents with other diagnostic profiles or those with SSD also showing marked cognitive impairment.
A limitation of the study was that because of logistic and financial limitations, the use of ESM was possible only in 17.9% of enrolled residents living in a subgroup of RFs, therefore reducing the generalisation of our findings.
Another limitation was the lack of a detailed statistical analysis plan for this specific CAN investigation in the study protocol (de Girolamo et al., 2020).
We were also not able to perform a detailed statistical analysis, such as to cluster the sample, particularly the ESM subsample, based on the RFs where they live because of the limitation in the overall sample size.
Finally, data were collected during the coronavirus disease 2020 pandemic, which influenced daily clinical practice and routine activities.
Conclusions
This is the first study to investigate the needs for care of residents with SSD and its association with daily activities and mood, as monitored using the ESM.
Our findings reveal that although needs for care are important for planning rehabilitative activities (Lasalvia et al., 2008; National Institute for Health and Care Excellence, 2020; Martinelli and Ruggeri, 2020a), Italian RFs deliver interventions which do not fully meet them. Furthermore, despite national and international guidelines (Grinshpoon and Ponizovsky, 2008; IBM Corp. Released, 2020; Martinelli and Ruggeri, 2020b) recommending the implementation of shared decision-making to promote users' recovery, we found a substantial disagreement concerning unmet care needs between users and staff. Hence, Italian RFs need to deliver rehabilitative interventions that match real users' needs for care to facilitate their productive activities and progress towards recovery.
Further studies are needed to evaluate whether the use of the ESM might facilitate the design of tailored rehabilitative interventions based on the consensus of users and staff regarding needs for care.
Acknowledgements
We thank all members of the DiAPAson Consortium who actively worked to make this project possible: Niccolò Rossetto (Du Parc project, Torino), Rodolfo Pessina and Anna Auxilia (DSMD, ASST di Monza, Monza), Samantha Panigada and Stefania Ravera (Fondazione Giuseppe Costantino CRCRC Onlus, Pavia), Livia Elena Fussi and Valter Masseroni (DSMD, ASST di Melegnano e Martesana, Melegnano), Maria Concetta Miranda and Rosa Verrona (DSM, ASL Napoli 2 Nord, Napoli), Daniela di Cosimo (Fatebenefratelli, Centro Sacro Cuore di Gesù, San Colombano al Lambro), Alessandro Norbedo and Paolo Peressutti (DSM, ASUITS, Trieste), Gaetano Nappi and Domenico Semisa (DSM, ASL Bari, Bari), Fabio de Dominicis and Elisa Castagno (SRP 1 San Benedetto Menni, S. Maurizio Canavese), Lucio Ghio and Michele Tosato (DSMD, ASL 3 Genovese, Genova), Sarah Tosato and Michela Nosè (DSM, AULSS 9 Scaligera, Verona), Lorenzo Tatini and Giulio D'Anna (DSM, USL Toscana centro, Prato), Annalisa Maurizi and Filippo Maria Jacoponi (Comunità Passaggi, Aquila), Vittorio di Michele (DSM, ASL di Pescara, Penne), Vera Abbiati and Roberto Colombo (DSMD, ASST di Pavia, Pavia), Luca Rancati (CPA La Perla CREST, Grumello del Monte), Valentina Regina and Cassandra Ariu (DSMD, ASST di Brescia, Brescia), Carmela Schiavo and Carlotta lanzi (Centro Ippocrate, Cagliari), Emanuela Leuci e Lorenzo Pelizza (DSM-DP, AUSL di Parma, Parma). Graham Thornicroft is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King's College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT is also supported by the Guy's and St Thomas' Charity for the On Trac project (EFT151101), and by the UK Medical Research Council (UKRI) in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards.
Supplementary material
For supplementary material accompanying this paper visit http://doi.org/10.1017/S2045796023000124.
click here to view supplementary material
Data
Dataset referring to this manuscript is published with restricted access on Zenodo platform and accessible at this link: https://doi.org/10.5281/zenodo.686604.
Financial support
The DiAPAson project is funded by the Italian Ministry of Health (Bando per la ricerca Finalizzata 2018: RF-2018-12365514). The Ministry of Health has no role in the analyses and interpretation of study findings.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. The study has been approved by the ethical committees (ECs) of the three main participating centres: EC of IRCCS Istituto Centro San Giovanni di Dio Fatebenefratelli (31/07/2019; no. 211/2019), EC of Area Vasta Emilia Nord (25/ 09/2019; no. 0025975/19) and EC of Pavia (02/09/2019, no. 20190075685) and by the ECs of all participating sites. All participants provided informed consent to the participation.
References
- Ådnanes M, Kalseth J, Ose SO, Ruud T, Rugkåsa J and Puntis S (2019) Quality of life and service satisfaction in outpatients with severe or non-severe mental illness diagnoses. Quality of Life Research 28, 713–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Washington, DC: American Psychiatric Association. [Google Scholar]
- Argentzell E, Bäckström M, Lund K and Eklund M (2020) Exploring mediators of the recovery process over time among mental health service users, using a mixed model regression analysis based on cluster RCT data. BMC Psychiatry 20, 520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atwoli L and Muhia J (2021) Delivering truly evidence-based mental health care in low- and middle-income countries: the dangers of experimentation. In Okpaku SO (ed.), Innovations in Global Mental Health, pp. 1–14. Cham: Springer. [Google Scholar]
- Basaglia F (1968) L'istituzione negata. Milano: Baldini Castoldi Dalai. [Google Scholar]
- Becker T and Fangerau H (2018) 40th Birthday of the Italian mental health law 180 – perception and reputation abroad, and a personal suggestion. Epidemiology and Psychiatric Sciences 27, 314–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunt D and Hansson L (2002) Comparison of user assessed needs for care between psychiatric inpatients and supported community residents. Scandinavian Journal of Caring Sciences 16, 406–413. [DOI] [PubMed] [Google Scholar]
- Campion J, Coombes C and Bhaduri N (2017) Mental health coverage in needs assessments and associated opportunities. Journal of Public Health 39, 813–820. [DOI] [PubMed] [Google Scholar]
- Cho H, Gonzalez R, Lavaysse LM, Pence S, Fulford D and Gard DE (2017) Do people with schizophrenia experience more negative emotion and less positive emotion in their daily lives? A meta-analysis of experience sampling studies. Schizophrenia Research 183, 49–55. [DOI] [PubMed] [Google Scholar]
- Cleary M, Hunt GE, Walter G and Freeman A (2006) The patient's view of need and caregiving consequences: a cross-sectional study of inpatients with severe mental illness. Journal of Psychiatric and Mental Health Nursing 13, 506–551. [DOI] [PubMed] [Google Scholar]
- Culbreth AJ, Barch DM and Moran EK (2021) An ecological examination of loneliness and social functioning in people with schizophrenia. Journal of Abnormal Psychology 130, 899–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Girolamo G, Picardi A, Micciolo R, Falloon I, Fioritti A and Morosini P for the Italian PROGRES Study Group (2002) Residential care in Italy: a national survey of non-hospital facilities. British Journal of Psychiatry 181, 220–225. [DOI] [PubMed] [Google Scholar]
- de Girolamo G, Picardi A, Santone G, Falloon I, Morosini P, Fioritti A and Micciolo R for the PROGRES Group (2005) The severely mentally ill in residential facilities: a national survey in Italy. Psychological Medicine 34, 1–11. [DOI] [PubMed] [Google Scholar]
- de Girolamo G, Rocchetti M, Benzi IMA, Agosta S, Casiraghi L, Ferrari C, De Franceschi N, Macis A, Pogliaghi S and Starace F (2020) DAily time use, physical activity, quality of care and interpersonal relationships in patients with schizophrenia spectrum disorders (DiAPASon): an Italian multicentre study. BMC Psychiatry 20, 287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eklund M and Ostman M (2010) Belonging and doing: important factors for satisfaction with sexual relations as perceived by people with persistent mental illness. The International Journal of Social Psychiatry 56, 336–347. [DOI] [PubMed] [Google Scholar]
- Federici S, Meloni F, Mancini A, Lauriola M and Olivetti Belardinelli M (2009) World health organisation disability assessment schedule II: contribution to the Italian validation. Disability and Rehabilitation 31, 553–564. [DOI] [PubMed] [Google Scholar]
- Gold LH (2014) DSM-5 and the assessment of functioning: the world health organization disability assessment schedule 2.0 (WHODAS 2.0). The Journal of the American Academy of Psychiatry and the Law 42, 173–181. [PubMed] [Google Scholar]
- Goldstone LW (2020) Unmet medical needs and other challenges in the treatment of patients with schizophrenia. The American Journal of Managed Care 26, S48–S54. [DOI] [PubMed] [Google Scholar]
- Granholm E, Loh C and Swendsen J (2008) Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophrenia Bulletin 34, 507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, Holden JL, Mikhael T, Link PC, Swendsen J, Depp C, Moore RC and Harvey PD (2020) What do people with schizophrenia do all day? Ecological momentary assessment of real-world functioning in schizophrenia. Schizophrenia Bulletin 46, 242–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinshpoon A and Ponizovsky AM (2008) The relationships between need profiles, clinical symptoms, functioning and the well-being of inpatients with severe mental disorders. Journal of Evaluation in Clinical Practice 14, 218–225. [DOI] [PubMed] [Google Scholar]
- Grinshpoon A, Friger M, Orev E, Shvarts S, Kaplan Z, Abramowitz MZ and Ponizovsky AM (2008) Relative perceptions of the needs of inpatients with schizophrenia and schizoaffective disorders. The Israel Journal of Psychiatry and Related Sciences 45, 201–209. [PubMed] [Google Scholar]
- IBM Corp. (2020) IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp. [Google Scholar]
- Janney CA, Ganguli R, Richardson CR, Holleman RG, Tang G, Cauley JA and Kriska AM (2013) Sedentary behavior and psychiatric symptoms in overweight and obese adults with schizophrenia and schizoaffective disorders (WAIST study). Schizophrenia Research 145, 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junghan UM, Leese M, Priebe S and Slade M (2007) Staff and patient perspectives on unmet need and therapeutic alliance in community mental health services. The British Journal of Psychiatry: The Journal of Mental Science 191, 543–547. [DOI] [PubMed] [Google Scholar]
- Killaspy H (2016) Supported accommodation for people with mental health problems. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 15, 74–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhy D, Vakhrusheva J, Liu Y and Wang Y (2014) Use of mobile assessment technologies in inpatient psychiatric settings. Asian Journal of Psychiatry 10, 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluge A, Kirschner M, Hager OM, Bischofm M, Habermeyer B, Seifritz E, Walther S and Kaiser S (2018) Combining actigraphy, ecological momentary assessment and neuroimaging to study apathy in patients with schizophrenia. Schizophrenia Research 195, 176–182. [DOI] [PubMed] [Google Scholar]
- Lanfredi M, Zoppei S, Ferrari C, Bonetto C, van Bortel T, Thornicroft G, Knifton L, Quinn N, Rossi G and Lasalvia A (2015) Self-stigma as a mediator between social capital and empowerment among people with major depressive disorder in Europe: the ASPEN study. European Psychiatry 30, 58–64. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Ruggeri M, Mazzi MA and Dall'Agnola RB (2000) The perception of needs for care in staff and patients in community-based mental health services. The south-Verona outcome project 3. Acta Psychiatrica Scandinavica 102, 366–375. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Bonetto C, Salvi G, Bissoli S, Tansella M and Ruggeri M (2007) Predictors of changes in needs for care in patients receiving community psychiatric treatment: a 4-year follow-up study. Acta Psychiatrica Scandinavica 437, 31–41. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Bonetto C, Tansella M, Stefani B and Ruggeri M (2008) Does staff-patient agreement on needs for care predict a better mental health outcome? A 4-year follow-up in a community service. Psychological Medicine 38, 123–133. [DOI] [PubMed] [Google Scholar]
- Martinelli A and Ruggeri M (2020a) The impact on psychiatric rehabilitation of personal recovery-oriented approach. Journal of Psychopathology 26, 189–195. [Google Scholar]
- Martinelli A and Ruggeri M (2020b) An overview of mental health recovery-oriented practices: potentiality, challenges, prejudices, and misunderstandings. Journal of Psychopathology 26, 1–8. [Google Scholar]
- Martinelli A, Iozzino L, Ruggeri M, Marston L and Killaspy H (2019) Mental health supported accommodation services in England and in Italy: a comparison. Social Psychiatry and Psychiatric Epidemiology 54, 1419–1427. [DOI] [PubMed] [Google Scholar]
- Martinelli A, Iozzino L, Pozzan T, Cristofalo D, Bonetto C and Ruggeri M (2022a) Performance and effectiveness of step progressive care pathways within mental health supported accommodation services in Italy. Social Psychiatry and Psychiatric Epidemiology 57, 939–952. [DOI] [PubMed] [Google Scholar]
- Martinelli A, Killaspy H, Zarbo C, Agosta S, Casiraghi L, Zamparini M, Starace F, Rocchetti M, de Girolamo G, Ruggeri M and DiAPAson Consortium (Barlati S, Boero ME, Cerveri G, Clerici M, D'Anna G, De Novellis A, Di Michele V, Di Prisco P, Durbano F, Facchini F, Ghio L, Giosuè P, Greco C, Latorre V, Leuci E, Maone A, Marina M, Maurizi A, Monzani E, Placenti R, Rancati L, Rippa A, Rovera C, Silva A, Tura G, Zanolini S) (2022b) Quality of residential facilities in Italy: satisfaction and quality of life of residents with schizophrenia spectrum disorders. BMC Psychiatry 22, 717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzaia MC (2018) Needs in mental health and research. Revista Brasileira de Enfermagem 71, 2077–2078. [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012) Interrater reliability: the kappa statistic. Biochemia Medica 22, 276–282. [PMC free article] [PubMed] [Google Scholar]
- McPhearson P, Krotofil J and Killaspy H (2018) Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry 18, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministero Italiano della Salute (2013) Accordo Conferenza Unificata 17 ottobre 2013. Le Strutture Residenziali Psichiatriche. Rome: Ministero della Salute. [Google Scholar]
- Morosini P and Casacchia M (1995) Traduzione italiana della brief psychiatric rating scale, versione 4.0 ampliata (BPRS 4.0). Rivista Di Riabilitazione Psichiatrica e Psicosociale 3, 199–228. [Google Scholar]
- Mucci A, Galderisi S, Merlotti E, Rossi A, Rocca P, Bucci P, Piegari G, Chieffi M, Vignapiano A and Maj M (2015) The brief negative symptom scale (BNSS): independent validation in a large sample of Italian patients with schizophrenia. European Psychiatry: The Journal of the Association of European Psychiatrists 30, 641–647. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I and Kuppens P (2022) The Open Handbook of Experience Sampling Methodology. A Step-by-Step Guide to Designing, Conducting and Analyzing ESM Studies. Leuven: The centre for Research on Experience sampling and Ambulatory methods Leuven (REAL). [Google Scholar]
- Myin-Germeys I, van Os J, Schwartz JE, Stone AA and Delespaul PA (2001) Emotional reactivity to daily life stress in psychosis. Archives of General Psychiatry 58, 1137–1144. [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2020) Rehabilitation for adults with complex psychosis: summary of NICE guidance. British Medical Journal 372, 7–10. [PubMed] [Google Scholar]
- Norman CC, McDonald K, Schneider AE, Malinovsky I, Goldmann E, Blauschild MK and Driver C (2018) The New York City Mental Health Needs Assessment Study (MHNAS): objectives, design, and methods. Internal Journal of Methods in Psychiatric Research 27, e1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochoa S, Haro JM, Autonell J, Pendàs A, Teba F, Màrquez M and Nedes Group (2003) Met and unmet needs of schizophrenia patients in a Spanish sample. Schizophrenia Bulletin 29, 201–210. [DOI] [PubMed] [Google Scholar]
- Oorschot M, Lataster T, Thewissen V, Lardinois M, van Os J, Delespaul PA and Myin-Germeys I (2012) Symptomatic remission in psychosis and real-life functioning. The British Journal of Psychiatry: The Journal of Mental Science 201, 215–220. [DOI] [PubMed] [Google Scholar]
- Overall JE and Gorham DR (1962) The brief psychiatric rating scale. Journal of Psychological Reports 10, 799–812. [Google Scholar]
- Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T, Strathdee G, Loftus L, McCrone P and Hayward P (1995) The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. The British Journal of Psychiatry 167, 589–595. [DOI] [PubMed] [Google Scholar]
- Picardi A, Lega I, Candini V, Dagani J, Iozzino L and de Girolamo G (2014) Monitoring and evaluating the Italian mental health system: the ‘Progetto Residenze’ study and beyond. Journal of Nervous Mental Disease 202, 451–459. [DOI] [PubMed] [Google Scholar]
- Priebe S, Saidi M, Want A, Mangalore R and Knapp M (2009) Housing services for people with mental disorders in England: patient characteristics, care provision and costs. Social Psychiatry and Psychiatric Epidemiology 44, 805–814. [DOI] [PubMed] [Google Scholar]
- Raugh IM, James SH, Gonzalez CM, Chapman HC, Cohen AS, Kirkpatrick B and Strauss GP (2021) Digital phenotyping adherence, feasibility, and tolerability in outpatients with schizophrenia. Journal of Psychiatric Research 138, 436–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2013) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. Available at http://www.R-project.org/ (Accessed 24 January 2023). [Google Scholar]
- Reisinger EW, Moore E, Tapscott S, Alperin M, Cumming JR and Druss BJ (2021) Developing regional mental health priorities: mixed-methods needs assessment of eight states in the southeastern United States. Psychiatric Service 72, 358–361. [DOI] [PubMed] [Google Scholar]
- Ruggeri M, Lasalvia A, Nicolaou S and Tansella M (1999) The Italian version of the Camberwell Assessment of Need (CAN), an interview for the identification of needs of care. [La versione italiana della Camberwell Assessment of Need (CAN), un'intervista per l'identificazione dei bisogni di cura]. Epidemiologia e Psichiatria Sociale 8, 135–167. [DOI] [PubMed] [Google Scholar]
- Ruggeri M, Leese M, Slade M, Bonizzato P, Fontecedro L and Tansella M (2004) Demographic, clinical, social and service variables associated with higher needs for care in community psychiatric service patients. The south Verona outcome project 8. Social Psychiatry and Psychiatric Epidemiology 39, 60–68. [DOI] [PubMed] [Google Scholar]
- Salisbury T, Killaspy H and King M (2016) An international comparison of the deinstitutionalisation of mental health care: development and findings of the mental health services deinstitutionalisation measure (MENDit). BMC Psychiatry 16, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santone G, de Girolamo G, Falloon I, Fioritti A, Micciolo A, Picardi A and Zanalda E for the PROGRES Group (2005) The process of care in residential facilities. A national survey in Italy. Social Psychiatry and Psychiatric Epidemiology 40, 540–550. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc (2013) SAS® 9.4 Statements: Reference. Cary, NC: SAS Institute Inc. [Google Scholar]
- Slade M, Phelan M and Thornicroft G (1998) A comparison of needs assessed by staff and by an epidemiologically representative sample of patients with psychosis. Psychological Medicine 28, 543–550. [DOI] [PubMed] [Google Scholar]
- Starace F, Baccari F and Mungai F (2017) La salute mentale in italia. analisi delle strutture e delle attività dei dipartimenti di salute mentale SIEP. Dipartimenti di salute mentale Quaderni di epidemiologia psichiatrica 1, 15. [Google Scholar]
- Strauss GP, Keller WR, Buchanan RW, Gold JM, Fischer BA, McMahon RP, Catalano LT, Culbreth AJ, Carpenter WT and Kirkpatrick B (2012) Next-generation negative symptom assessment for clinical trials: validation of the brief negative symptom scale. Schizophrenia Research 142, 88–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft G and Tansella M (2004) Components of a modern mental health service: a pragmatic balance of community and hospital care: overview of systematic evidence. The British Journal of Psychiatry: The Journal of Mental Science 185, 283–290. [DOI] [PubMed] [Google Scholar]
- United Nations (2006) Convention on the Rights of Persons with Disabilities Dec 2006. United Nations General Assembly A/61/611. Available at http://www.un.org/disabilities/default.aspid=61 (Accessed 24 January 2023).
- van Os J, Lataster T, Delespaul P, Wichers M and Myin-Germeys I (2014) Evidence that a psychopathology interactome has diagnostic value, predicting clinical needs: an experience sampling study. PLoS ONE 9, e86652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wee ZY, Yong SWL, Chew QH, Guan C, Lee TS and Sim K (2019) Actigraphy studies and clinical and biobehavioural correlates in schizophrenia: a systematic review. Journal of Neural Transmission 126, 531–558. [DOI] [PubMed] [Google Scholar]
- Wennström E and Wiesel FA (2006) The Camberwell assessment of need as an outcome measure in routine mental health care. Social Psychiatry and Psychiatric Epidemiology 41, 728–733. [DOI] [PubMed] [Google Scholar]
- Werner S (2012) Needs assessment of individuals with serious mental illness. Can it help in promoting recovery? Community Mental Health 48, 56–573. [DOI] [PubMed] [Google Scholar]
- Wiersma D, van den Brink R, Wolters K, McCabe R, Bullenkamp J, Hansson L, Lauber C, Martinez-Leal R, Rössler W, Salize H, Björkman T, Torres-Gonzales F, Wright DJ and Priebe S (2009) Individual unmet needs for care: are they sensitive as outcome criterion for the effectiveness of mental health services interventions? Social Psychiatry and Psychiatric Epidemiology 44, 317–324. [DOI] [PubMed] [Google Scholar]
- Winkler P, Krupchanka D, Roberts T, Kondratova L, Machů V, Höschl C, Sartorius N, Van Voren R, Aizberg O, Bitter I, Cerga-Pashoja A, Deljkovic A, Fanaj N, Germanavicius A, Hinkov H, Hovsepyan A, Ismayilov FN, Ivezic SS, Jarema M, Jordanova V, Kukić S, Makhashvili N, Šarotar BN, Plevachuk O, Smirnova D, Voinescu BI, Vrublevska J and Thornicroft G (2017) A blind spot on the global mental health map: a scoping review of 25 years’ development of mental health care for people with severe mental illnesses in central and eastern Europe. The Lancet. Psychiatry 4, 634–642. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://doi.org/10.1017/S2045796023000124.
click here to view supplementary material
Data Availability Statement
Dataset referring to this manuscript is published with restricted access on Zenodo platform and accessible at this link: https://doi.org/10.5281/zenodo.686604.