Abstract
Residents of rural areas are underrepresented in research. The aim of this narrative review was to explore studies describing the effectiveness of community engagement strategies with rural communities to promote participant recruitment and participation in clinical research. Following PRISMA guidelines, this narrative review was conducted in June 2020. Our search strategy was built around keywords that included community-engaged research, rural community, and recruitment strategies into clinical research. Content-related descriptive statistics were summarized. The selected articles were distributed into categories of levels of community engagement: inform, consult, involve, collaborate, or co-lead. The search resulted in 2,473 identified studies of which forty-eight met inclusion criteria. Of these, 47.1% were randomized controlled trials. The most common levels of engagement were consultation (n = 24 studies) and collaboration (n = 15), while very few focused on informing (n = 2) and co-leadership (n = 2). Strategies, limitations, and findings are discussed for each level of community engagement. This narrative addressed a gap in knowledge regarding participant recruitment in rural communities in relation to assistance from community members. Community engagement contributed to the success of the research, especially in recruitment, participation, and building trust and partnership.
Keywords: Rural communities, clinical research, community engagement
Introduction
Despite well-documented health disparities among rural residents, they remain underrepresented in clinical research [1]. Although approximately 14% of US residents live in rural areas, only 3% of the National Cancer Institute’s clinical research focused on rural populations between 2011 and 2016 [2,3]. Some factors contributing to this are that rural populations in America face several barriers to healthcare compared to urban and suburban populations, and clinical research studies are often offered as part of medical encounters [4]. Barriers to accessing healthcare in rural communities include geographical distances to medical facilities requiring extensive travel and lodging costs, lack of public transportation, stigma, and distrust of the healthcare system [5,6]. Representation of rural populations in clinical research is necessary to understand and deploy effective health care strategies that can benefit all rural individuals, increasing the generalizability and equity of research findings.
Recently, developing infrastructure and capabilities for clinical research to address health disparities among rural populations has been viewed as a national priority [7,8]. In response, collaborative efforts involving community-academic partnerships on community engagement, late-stage translation, and digital infrastructure have begun to address the inadequate digital infrastructure and barriers to health care access among rural communities [9,10]. A body of evidence showed that recruitment and participation of rural populations can be facilitated through community engagement in research [11,12]. Collaboration with community members has numerous merits including addressing prevalent health issues, strengthening researchers’ understanding of community priorities, and supporting culturally appropriate communication [13]. However, evidence for a comprehensive understanding of specific strategies for promoting participation in clinical research among residents of rural communities is unclear.
The goal of this narrative review is to evaluate the extant literature about the use of community engagement strategies to promote recruitment, enrollment, and participation in clinical research with rural communities. This review will highlight effective strategies in promoting participation and identify ineffective ones. This knowledge will progress the current understanding of the issue and outline specific strategies that can be applied in clinical research based in rural settings.
Methods
To achieve the proposed objective, a narrative review was used to address the knowledge gap on ways to engage and promote clinical research in rural communities. This narrative review followed the PRISMA-ScR guidelines to plan, conduct, and report the results [14].
Data Sources and Search Strategies
Online searches were conducted using a variety of different strategies with assistance from an experienced medical librarian. We searched PubMed, Embase, CINAHL, Scopus, Web of Science, and Cochrane Database of Systematic Reviews to identify English-language manuscripts about clinical research among rural communities. Searches of ClinicalTrials.gov were conducted to capture unpublished or ongoing research. A variety of keywords, some truncated, and subject headings were combined using Boolean operators to retrieve results in the databases. The searches included terms such as “community engaged research,” “CEnR,” “rural populations,” “recruitment,” “intervention,” “research subjects,” and “patient selection.” Results were restricted to human subjects and clinical research publication type.
Study Eligibility and Outcome Measures
In this review, studies were eligible for inclusion if they included community engagement approaches, recruitment, and enrollment of rural participants to clinical research in the United States. Clinical research was defined as “A component of medical and health research intended to produce knowledge valuable for understanding human disease, preventing and treating illness, and promoting health” [15]. Key components included a sponsor, study question, study population, inclusion/exclusion criteria, observation and/or intervention, and outcomes. Types of research studies included were bi-directional integrative (translational) research, community-based clinical research, therapeutic interventions, prevention and health promotion, behavioral research, and health services research. Exclusion criteria were non-English articles, studies conducted outside the United States, systematic reviews, non-original research, and did not include rural populations. In some strategies, the text words and publication types “systematic reviews” and “meta-analyses” were also excluded. No publication period restrictions were applied to the database searches (Table 1).
Table 1.
Summary of inclusion and exclusion criteria for the narrative review
| Factor | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | • Patient • Community • Rural or rural population • Rural health disparities • Veteran, military personnel • Farmer, farming |
• No mention of a rural population |
| Setting | • Studies conducted in the United States • Studies conducted in the rural community |
• International studies • No mention of rural setting |
| Community Engagement | • Recruitment strategies • Recruitment barriers • Peer outreach • Engagement • Patient engagement • Community engagement • Retention • Partnership • Collaboration • Community-academic partnerships • Primary care provider • Community-based participatory research • CEnR |
• No mention of a community engagement component |
| Language | • Studies published in the English language | • Studies not published in the English language |
| Study Type | • Original research • Research • Clinical trial • Intervention |
• Editorials, letters, chart review, conference, poster abstract, protocol papers, meta-analysis, and systematic reviews • Qualitative, interview, focus group |
Screening and Data Extraction
All records were screened among two-three reviewers by title and abstract, full text, and data extraction. Covidence was used for all study screening and data extraction activities. For data extraction and synthesis, three reviewers were assigned to each article, with decisions based on agreement among two-three of the reviewers. The following items were extracted from these studies: study design, study focus (recruitment, retention, or both), study population(s), study setting(s), number of rural research participants recruited, study description/aim, community engagement intervention for rural recruitment, level of community engagement, and major findings from the study.
The International Association for Public Participation’s Spectrum of Public Participation [16] broadly categorizes community engagement; thus, the levels of community engagement were adapted and defined as follows: (1) inform – communities are provided with information about research opportunities, (2) consult – feedback is solicited from communities for research procedures, (3) involve – communities informed and participate in research procedures, (4) collaborate – partnerships are formed with communities to work together on all procedures, and (5) co-lead – robust partnership with communities who hold decision-making power over all research procedures. If applicable, the number of urban participants was also extracted from the study. All data extraction, synthesis, and consensus were captured in Covidence for summarizing and comparisons.
Synthesis of Results
Following the data extraction process, the information gathered was coded for the following: strategies that worked to recruit participants, strategies that did not work to recruit participants, and recruitment findings/outcomes. Three reviewers were involved in this process, and the data were then combined for one final consensus.
Results
Search Results
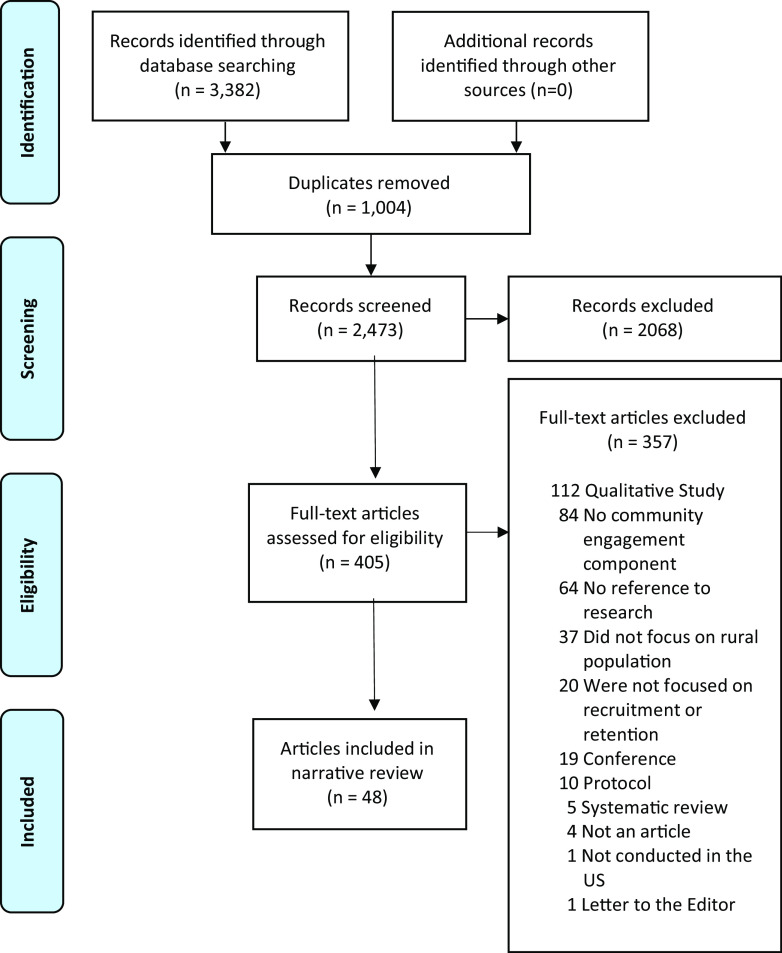
Database searches retrieved a total of 3382 papers, which yielded 2473 unique papers after de-duplication. In screening the titles and abstract, 2068 articles were excluded because of irrelevant populations, study type, setting, or missing abstract. After further screening, investigators then reviewed 405 papers of which forty-eight articles were identified to have fulfilled the inclusion criteria (see Fig. 1).
Fig. 1.
PRISMA flow diagram.
Characteristics of Included Studies
The included studies were published between 1990 and 2021. Of the forty-eight articles, almost half (41.7%) were randomized controlled trials, and a third were quasi-experimental studies (27.1%). The remaining articles included mixed methods (8.3%), cohort designs (8.3%), cross-sectionals (8.3%), non-randomized clinical research (2.1%), case studies (2.1%), and stratified random sample studies (2.1%). The majority (91.7%) focused on rural communities, and the remaining (8.3%) included both rural and urban communities. The bulk of the included articles (70.8%) either focused on or included underrepresented groups including African American, Hispanic, American Indian or Alaska Native (AIAN) or Asian people, or the transgender community. The health-related themes of forty-eight articles were diverse; however, these were clustered into five categories: nutrient-related and nutrient processing problems (39.6%), cancer (29.2%), behavioral and physical health (27.1%), cardiovascular issues (16.7%), patient engagement (6.3%), and mental health (2.1%). Although there are some articles that only emphasized one health disparity, some had multiple. Over two-thirds (68.8%) were conducted in community settings, while 18.8% were in clinical settings and 18.8% at home or by phone. Two studies were conducted in multiple settings (Table 2).
Table 2.
Characteristics of selected articles
| First Author, Year | Study setting | Study design | # Rural & urban participants |
Participant race & ethnicity | Health disparity | Level of engagement | Primary strategy(ies) | Primary outcome |
|---|---|---|---|---|---|---|---|---|
| Kupfer, 2009 | Clinical/hospital setting | Randomized clinical trial | 99 rural 416 urban |
African American non-African American |
Mental health | Inform | Community personnel | Improved recruitment |
| Gold, 1990 | Home/phone | Cohort design | 1168 rural | N/A | Cardiovascular issues | Inform | Community personnel Personnel remuneration |
Poor outcomes Community reservation Perceived charity |
| Levy, 2015 | Clinical/hospital setting | Quasi-experimental | 351 rural | N/A | Cancer | Consult | Community personnel | Increased general health awareness |
| Lilly, 2014 | Community setting | Quasi-experimental | 81 rural | Hispanic non-Hispanic Caucasian African American |
Cardiovascular issues | Consult | Community personnel Tailored materials Focus group |
Improved recruitment Tailored materials |
| Cruz, 2014 | Community setting | Randomized control trial | 2444 rural | American Indian Hispanic |
Nutrient-related and nutrient processing problems | Consult | Community personnel Feedback Personnel remuneration |
Partnership Informed adjustment |
| Nguyen, 2012 | Community setting | Cross-sectional survey | 563 rural | African American American Indian non-Hispanic Caucasian |
Nutrient-related and nutrient processing problems | Consult | Community personnel Community setting |
Improved recruitment |
| McMahon, 2015 | Community setting Home/phone |
Randomized controlled trial Repeated measures |
30 rural | Predominantly non-Hispanic Caucasian | Behavioral and physical health | Consult | Community personnel Feedback |
Feedback Input implementation |
| Warren, 2010 | Community setting | Quasi-experimental | 188 rural | Non-Hispanic Caucasian Black Hispanic |
Cancer Behavioral and physical health |
Involve | Community personnel | Improved study promotion |
| Luque, 2017 | Community setting | Quasi-experimental | 90 rural | Hispanic | Cancer | Involve | Community personnel Tailored materials Community setting |
Improved recruitment Tailored materials Patient-centered |
| Sutton, 2019 | Home/phone | Cross-sectional study-community-based research | 391 rural | Predominantly non-Hispanic Caucasian | Cancer | Involve | Community events Digital access Educational programs |
Community personnel engagement Direct exposure to information |
| Yeary, 2019 | Community setting | Cluster-randomized trial | 426 rural | African American | Nutrient-related and nutrient processing problems | Involve | Community personnel Community setting Tailored materials |
Improved recruitment Improved retention |
| Westfall, 2013 | Home/phone | Controlled trial using a quasi-experimental repeated cross-sectional ecological design | 1048 rural | Predominantly non-Hispanic Caucasian | Cancer | Involve | CBPR Tailored materials |
Improved recruitment Tailored materials |
| Hillemeier, 2008 | Clinical/hospital setting | Randomized controlled trial | 362 rural | non-Hispanic Caucasian (90%) Hispanic African American Asian |
Behavioral and physical health | Involve | CBPR Community personnel |
Tailored materials Active recruitment Passive recruitment |
| Northridge, 2008 | Clinical/hospital setting | Mixed methods | 547 rural 155 urban |
non-Hispanic Caucasian African American |
Behavioral and physical health | Involve | Community personnel | Behavior change Address hard-to-reach population |
| Kogan, 2016 | Community setting | Randomized controlled trial | 465 rural | African American | Behavioral and physical health | Involve | CBPR Community personnel Tailored materials |
Study adherence Intervention delivery |
| Dake, 2011 | Community setting | Stratified random sample | 778 rural | Predominantly non-Hispanic Caucasian | Behavioral and physical health | Involve | Community personnel Tailored materials |
Informed adjustments Co-design |
| Kogan, 2016 | Community setting | Observational/self-report | 505 rural | African American | Involve | Community personnel | N/A | |
| Tussing-Humphreys, 2013 | Community setting | Quasi-experimental | 403 rural | African American | Nutrient-related and nutrient processing problems Behavioral and physical health Cardiovascular issues |
Involve | Community personnel | Educational sessions attendance |
| Folta, 2019 | Home/phone Community setting |
Randomized controlled trial | 194 rural | Predominantly non-Hispanic Caucasian | Nutrient-related and nutrient processing problems Behavioral and physical health Cardiovascular issues |
Involve | Community personnel Community setting Feedback |
Feasible intervention delivery |
| Abbott, 2020 | Community setting | Cluster-randomized controlled trial | 146 rural | African American | Nutrient-related and nutrient processing problems Cardiovascular issues |
Involve | Community personnel Community setting |
Improved retention |
| Logan, 2015 | Home/phone | Mixed method | 806 rural | non-Hispanic Caucasian African American |
Cancer | Involve | Community personnel Tailored materials Feedback |
Feedback Tailored materials Input implementation |
| Hilgeman, 2014 | Clinical/hospital setting | Pilot Study. prospective, randomized, controlled multi-site study Pragmatic trial | 203 rural | Predominantly non-Hispanic Caucasian Black Asian Hispanic |
Patient engagement | Involve | Community personnel Tailored materials |
Decreased time to first appointment |
| Briant, 2018 | Home/phone | Pre- and Post-test cohort design. | 101 rural | Hispanic | Cancer | Involve | CBPR Community personnel Tailored materials |
Tailored materials Improved screening rate |
| Jones, 2016 | Community setting | Quasi-experimental | 41 rural | Predominantly non-Hispanic Caucasian | Behavioral and physical health | Involve | Community personnel Tailored materials Feedback |
Partnership |
| Befort, 2015 | Clinical/hospital setting | Randomized trial | 210 rural | N/A | Cancer Behavioral and physical health |
Involve | Community personnel Tailored materials Community events |
Improved recruitment Tailored materials Partnership |
| Flynn, 1997 | Community setting | Randomized controlled trial-two matched sets | 540 rural | Predominantly non-Hispanic Caucasian | Cancer | Involve | Community personnel Focus group Feedback |
Educational program Barrier-reduction strategies |
| Leach, 2011 | Community setting | Case study | 15 rural | N/A | Cancer | Involve | CBPR Community personnel Tailored materials |
Increased trust Tailored materials Improved recruitment |
| Estabrooks, 2017 | Community setting Home/phone |
Randomized controlled trial-case study | 301 rural | Predominantly non-Hispanic Caucasian | Nutrient-related and nutrient processing problems | Involve | Community personnel Community setting |
Improved recruitment Tailored materials |
| Abbott, 2018 | Community setting | Cluster-randomized controlled trial | 229 rural | African American | Cardiovascular issues | Involve | Community personnel Community setting |
Tailored materials Behavior change |
| Tiwari, 2014 | Community setting | CNOHR – Randomized controlled trial GIFVT – stratified randomized trial TSHS – stratified cluster-randomized trial |
461 rural 597 urban |
Rural American Indian Urban Hispanic, African American, and non-Hispanic Caucasian |
Behavioral and physical health | Involve | CBPR Community personnel Tailored materials |
Improved recruitment Increased trust Partnership Addressing community needs |
| Allman, 2011 | Home/phone | Prospective observational cohort | 366 rural 367 urban |
African American, non-Hispanic Caucasian | Patient engagement | Involve | CBPR Tailored materials |
Improved recruitment Increased trust |
| Hopper, 2017 | Community setting | Community-based participatory research project. Quasi-experimental design | 166 rural | Predominantly African American and American Indian Non-Hispanic Caucasian Other |
Nutrient-related and nutrient processing problems | Collaborate | CBPR Community personnel |
Evidence-informed intervention Community participation |
| Andreae, 2012 | Clinical/hospital setting | Cluster-randomized trial | 424 rural | African American Non-Hispanic Caucasian |
Nutrient-related and nutrient processing problems | Collaborate | Community personnel Feedback |
Improved recruitment Partnership |
| Zoellner, 2013 | Community setting | Randomized controlled pilot study | 91 rural | Predominantly African American | Nutrient-related and nutrient processing problems | Collaborate | CBPR Community personnel |
Increased trust Partnership |
| Powell, 2005 | Community setting | Quasi-experimental and community-based research | 192 rural | African American | Cancer | Collaborate | CBPR Community personnel Tailored materials |
Improved recruitment Improved retention Increased trust Tailored materials |
| Yeary, 2011 | Community setting | Quasi-experimental | 26 rural | African American | Nutrient-related and nutrient processing problems | Collaborate | CBPR Community personnel |
Tailored materials Study sustainability |
| Valerio, 2016 | Community setting | Mixed methods | 117 rural | Hispanic | Patient engagement | Collaborate | Community personnel CAB |
Increased trust Improved recruitment |
| Lemacks, 2018 | Community setting | Theory-driven intervention-clinical trial | 42 rural | African American | Nutrient-related and nutrient processing problems | Collaborate | Community personnel Remuneration Digital access |
Improved recruitment Co-design |
| Vines, 2016 | Community setting | Quasi-experimental | 129 rural | African American | Cancer | Collaborate | Community personnel | Increased trust Partnership |
| Harrell, 2005 | Community setting | Controlled experiment | 205 rural | Racially diverse | Nutrient-related and nutrient processing problems Cardiovascular issues Behavioral and physical health |
Collaborate | Community personnel Community setting Feedback |
Increased participation Community support |
| Love, 2019 | Community setting | Quasi-experimental | 513 rural | American Indian | Nutrient-related and nutrient processing problems Cardiovascular issues | Collaborate | CBPR Community personnel |
N/A |
| Davis, 2009 | Community setting | Randomized controlled clinical trial | 165 rural | African American Non-Hispanic Caucasian |
Nutrient-related and nutrient processing problems | Collaborate | Community personnel Tailored materials |
Community personnel involvement |
| DeMarco, 2014 | Community setting | Pilot project | 44 rural | N/A | Nutrient-related and nutrient processing problems | Collaborate | Community personnel Tailored materials |
Increased trust |
| Zoellner, 2007 | Community setting | Quasi-experimental | 83 rural | Predominantly African American | Nutrient-related and nutrient processing problems | Collaborate | CBPR Community personnel |
Tailored materials Effective delivery |
| Jernigan, 2018 | Community setting | Cluster-randomized controlled trial | 1646 rural | Native American | Nutrient-related and nutrient processing problems | Collaborate | Community personnel Tailored materials Feedback |
Improved recruitment Tailored materials |
| Lane, 2019 | Community setting | Mixed methods | 13 rural | N/A | Nutrient-related and nutrient processing problems | Collaborate | Community personnel CAB |
Increased participant motivation Tailored materials Behavior change |
| Angell, 2003 | Clinical/hospital setting | Randomized controlled trial | 100 rural | Predominantly non-Hispanic Caucasian | Cancer | Co-lead | CBPR Community personnel Tailored materials |
Improved recruitment Improved retention Tailored materials |
| Schroepfer, 2009 | Clinical/hospital setting | Community-based participatory research method-survey | 37 rural | American Indian | Cancer | Co-lead | CBPR Community personnel Tailored materials |
Improved recruitment Improved retention Tailored materials |
Recruitment Strategies
All the studies were examined in four categories: recruitment strategies, recruitment strengths, recruitment limitations, and findings (Table 3). Of the forty-eight articles included, thirty-one had a study focus on recruitment. Most of these relied on community engagement for successful recruitment of research participants. Involvement of community personnel (n = 46) [17–62], feedback (n = 22) [18,20,23,25,26,31,32,34,38,42–45,49,51–53,55–57,61,62], and customization of recruitment materials and processes in accordance with the characteristics of the community (n = 17) [19,22,25–27,32,34,45,47–50,52,56,58,61,63] were mentioned most frequently. Some other recruitment strategies included providing remuneration (either for participants or for community personnel) (n = 14) [19,23,31,33,35,37,42,44,48,49,51,54,58,61] and utilizing local spaces and events (n = 15) [19,21,22,28–30,38,39,42,46,56,58–60,63]. Although the majority of articles did not discuss limitations of the recruitment strategies, a few mentioned some challenges, including issues regarding community personnel recruitment [55,61], community personnel turnover [20,61], study interval [54], absence of educational programs [54], and ineffective recruitment via faith-based organizations [55]. Numerous outcomes of the recruitment strategies were discussed, most of which were positive. Among all the findings, production of tailored materials and procedures (n = 17) [19,25–28,31,34,45,48,51,52,56,58–60,62,64], improved participant recruitment (n = 19) [19,20,22,25–27,34,35,37,41,43,46,52,56,58,59,61–63], building partnership (n = 9) [20,23,27,40,42,49,55,56,61], and increased trust (n = 8) [23,27,35,40,50,58,61,63] were the most commonly observed outcomes. Additionally, there were other noteworthy outcomes: seven studies discussed improved participant retention [22,25,27,39,58,62,63], five studies successfully addressed community needs [52,57,61,62,64], and five studies effectively encompassed hard-to-reach populations [28,29,41,56,58].
Table 3.
Levels of community engagement for recruitment
| Level of community engagement |
Definition | Recruitment approaches | Recruitment findings |
|---|---|---|---|
| Inform (n = 2) | Communities are provided with information about research opportunities. | Study team provided the communities with information via visual mediums on media platforms. | The information was successful in recruiting participants but involvement of community members in the production of these mediums would have made them more effective. |
| Consult (n = 5) | Feedback is solicited from communities for research procedures. | Community members provided consultation in recruitment and retention. Community members also helped validate the study to other residents. |
Consultation from community personnel helped build trust and partnership between the research team and the community. Consultation also provided great insights into various aspects of research including recruitment and retention. |
| Involve (n = 24) | Communities are informed and participate in research procedures. | Research teams built partnerships with community organizations and local liaisons. Community members were involved directly in the process of producing materials and directly in recruitment. |
Direct involvement of community members in recruitment resulted in effective recruiting, engaging hard-to-reach populations. Topics of research and information delivery methods can impact overall efficacy of recruitment. |
| Collaborate (n = 15) | Partnerships are formed with communities to work together on all procedures. | Community members were included in different stages and procedures, including recruitment, problem assessment, data collection, and evaluation. | Collaboration with community members at numerous stages built trust, improved recruitment, developed partnership, and produced tailored materials for research. Collaboration, if done at an early stage, can also generate well-informed intervention that is easily introduced to the community. |
| Co-lead (n = 2) | Robust partnership with communities who hold decision-making power over all research procedures. | Community personnel and researchers had numerous interpersonal contacts to help direct the study. | The skills and knowledge of community personnel were integrated into research. Co-leading allowed for reduction of barriers to participation and ensured that the data collected were unique and beneficial to the community. |
Levels of Rural Community Engagement
Inform
Among the 48 articles, only 2 involved the community at the “inform” level [41,54]. Both studies utilized visual mediums as methods of recruitment, specifically TV ads in Kupfer’s article and community presentations in Gold’s article. Although Kupfer’s study was successful in engaging African American population [41], Gold identified three shortcomings in that study including initial failure to involve community members to produce tailored educational materials, an absence of ongoing educational programs, and the short interval of the study [41].
Consult
There were five studies identified as engaging the community at the “consult” level [34,42,46,53,65]. The community members provided different types of support to the research teams. Although in one study, the recruited community leaders helped validate the legitimacy of the research to elder participants of the community, another demonstrated the effectiveness of a focus group which helped inform the various aspects of the intervention including acceptability, marketing, content, and environment [34,46]. The articles reported some major advantages of engaging the community members in consultation. Cruz maintained that involvement of community members who advocated for the project served to build a foundation of trust and to ensure equity in the partnership, while McMahon noted that the community partners provided advice of great value regarding maximizing participant recruitment and retention [42,53].
Involve
Involvement was identified as the level of engagement in half of the studies (n = 24) [17,19,21,22,26,28–30,32,33,36,38,39,45,47,48,55–61,63]. In most of these studies, the research teams developed partnerships with local organizations or recruited community personnel and liaisons. These community partners provided insights into the study processes and materials, as well as managing and executing the recruitment process. By employing local members as study staff in the recruitment, populations that would be otherwise unable to reach were engaged in the study due to the increased trust among community members, as observed in Leach’s success in involving rural Appalachian women [58]. Furthermore, the community partners also helped in tailoring materials and processes to address the communities’ specific needs and characteristics, further improving the effectiveness of recruitment. However, it must be noted that there are some limitations to involving communities to participate in the research procedures. Leach outlined that the effectiveness of community partners recruiting participants was greatly reduced due to the topic of cancer, which was too frightening, especially for those who had experienced loss of loved ones due to cancer. Moreover, some recruitment mediums in the community including emails, paid newspaper advertisements, community flyers, and postcards have also been illustrated to lack efficacy in recruiting participants [59].
Collaborate
Collaboration was the level of community engagement in fifteen articles [18,20,23,27,31,35,37,40,43,44,49–52,64]. In these studies, community members were involved in numerous phases of the research, including problem assessment, recruitment, data collection, and evaluation. The results of collaboration with community members were quite positive. Some of the benefits of collaboration with community personnel include increased trust, improved participant recruitment, partnership between the research group and the locals, production of specialized materials and processes, and addressing the needs of the community. Furthermore, Hopper and colleagues [18] showed that early dedication of time and resources to engage community participation generated well-informed intervention and procedures, both of which were more easily accepted and effectively disseminated within the community.
Co-lead
Co-leading is the driving principle regarding community personnel in only two studies [25,62]. In Angell’s study, the skills and knowledge of community personnel were integrated into the model which produced numerous interpersonal contacts between recruiters and potential participants and received great advocacy from the community [25]. In Schroepfer’s research, the community leaders who had expressed interest in the study met with university partners to assess the study’s accuracy, cultural appropriateness, and other related areas including questions involving insurance [62]. The findings from these two articles maintained that the presence of community members in every step greatly reduced barriers to participation and ensured that the data collected was distinct and bore benefits to the community, adhering to the standards of equitable and ethical research.
Discussion
This review unveiled a body of literature regarding the use of community engagement strategies in research conducted in rural populations. The engagement of community members in research was shown to be of great benefit to study recruitment, participant participation, building partnership and trust with the community, and creation of materials and processes tailored to the community’s specific characteristics. Furthermore, engagement of community personnel in the research team ensured that the research was relevant to the community, addressed its specific needs, and benefited the community with its results. This idea of involving community members in the research team has recently been highlighted by existing health programs. A survey conducted in 2011 of the Clinical and Translation Science Awards programs demonstrated that 89% of the projects engaged Community Advisory Boards [66]. Thus, it can be maintained that the role of community engagement in research is crucial and is becoming increasingly better acknowledged within the scientific community.
The majority of studies utilized community partners to inform the research regarding recruitment, study materials, and dissemination of the intervention. Different levels of engagement imply different impacts by the community members on the research. Involvement of community personnel is most effective in the recruitment stage in which either the members provide advice on appropriate strategies, directly recruit participants, or serve as a connection between research members and residents of the community [45,47]. The presence of community members in this stage has been shown to greatly increase participant recruitment, as well as retention in some studies [63]. Moreover, involvement of community members in the research team can also foster increased trust between the researchers and the community participants [58], which is critical to facilitating effective intervention and access to hard-to-reach populations [67].
Although it was not included in the original inclusion criteria, partnership with local organizations, which is essential in establishing relationships in rural communities, was mentioned in 29 studies [17,18,22,24,26–29,32,35–43,47,48,50–52,55,56,59–61,64]. The majority of partnerships were formed with faith-based organizations (70%) and/or local health-related facilities (55%). Additionally, some other organizations involved as partners in the research were local businesses, schools or educational institutions, and general local community organizations. The importance of engaging with rural community-based organizations as a method of promoting research participation has been noted in various literature [68–70], as well as the CDC’s Principles of Community Engagement [71]. Culturally appropriate designs and trust in the research are important factors in engaging with the community [72], which can be facilitated through partnering with community-based organizations and receiving feedback from them. Through building solid relationships with existing local organizations, researchers can familiarize the research to a body of residents and help spread information about the project within the community. Because the majority of the selected papers did not explore the theme of participation engagement exclusively, more research exploring the effects of partnership with community-based organizations is warranted.
Successful recruitment observed in numerous studies was mostly attributed to the engagement of community members who advocated for the study. Most of the studies employed involvement and collaboration as the strategies to engage the community. Compared to information and consultation, collaboration, and involvement transfer some of the decision-making ability to the community members, as they can directly make decisions that impact the studies, evoking a sense of ownership and responsibility toward the research. In a corporate setting, involving employees in the decision-making process can induce a sense of ownership, produce an alignment of interest, and improve overall productivity and quality [73]. In the setting of clinical research, this can translate into improvement of the quality and effectiveness as observed in the selected articles. Additionally, with more power, community members can positively influence the procedures, strategies, and materials to ensure they best address and benefit the members of the community.
Of the forty-eight studies, only two employed co-leadership as the method of community engagement; however, the findings were very promising. In Angell’s article, efforts made by the community and their input were depicted as indispensable components to the research’s success. Moreover, Schroepfer’s study demonstrated that co-leadership empowered the community, enhanced the capacity of conducting research, and allowed for interpretation of data within the framework of local knowledge, available resources, specific values and beliefs [25,62]. These positive results certainly highlight the need for future research employing co-leadership as the engagement principle. Notably, both community personnel recruitment and turnover were mentioned as some of the potential challenges of this approach to consider in future research.
Only seven of the studies focused on implementing community engagement strategies among American Indian and Alaska Natives (AIAN) persons [18,42,44,46,52,61,62]. This is important to consider as AIAN communities remain disproportionately rural compared to other groups, with 29% identified as living in rural areas in 2010 compared to 15% of the total US population [74]. Comprising a large part of rural communities, AIAN people must be included in clinical research in order to learn effective community engagement strategies within this population. Moreover, community engagement techniques may be particularly beneficial when working with AIAN people due to research historically often not addressing community priorities and with little regard for cultural practices [75]. Furthermore, research has often been done without seeking consent from Indigenous communities or not communicating clearly when obtaining consent [76]. Recent initiatives have called for the need for more culturally sensitive and collaborative approaches in research with indigenous populations [77,78]. Community engagement strategies could provide a necessary framework for such efforts; however, more research is needed to better understand best practices within this population.
There are several limitations to the present review. While each level of engagement demonstrated unique benefits to the research, none of the included studies directly compared the different levels of engagement. In future research, it will be beneficial to understand the context in which each level would yield the highest contribution to the successes of the study. Furthermore, knowledge of different engagement principles will also determine balancing community involvement in decision-making and maintaining scientific vigor. Our narrative review is limited to research conducted in the United States and studies published in the English language, limiting generalizability to other countries and languages. Future narrative reviews that include international studies are needed to learn from the work of our neighbors and international partners such as Australia and Canada, who are working on similar issues. Moreover, this review highlights that compared to the whole, CEnR with rural populations occupy only a small portion of the existing body of research. Hence, more CEnR is needed in rural settings that are often underrepresented in the scientific world [4]. Additionally, specific definitions and characteristics of rurality were not captured in the present review (e.g., town size). Rurality is a multidimensional concept, and there is great variation across rural communities that need to be considered when implementing community engagement strategies.
Conclusion
This review highlighted the sizeable contributions community members and community leaders can have to the success of research. Most of the studies used collaboration and involvement as the principle driving community engagement. It can be easily observed that including community members on the research staff can enhance the quality of the research, appropriateness of the materials, and effectiveness of intervention delivery. Although it contains many benefits, community engagement is not the omnipotent answer to tackle every barrier, such as transportation, geological isolation, or insufficient services and infrastructure, all of which contribute to the exclusion of rural populations in clinical research. However, it is a necessary component to include in any solution to resolve these issues. Community engagement strategies produce more equity in clinical research, as the participants are part of the team and can ensure that the research is appropriate and beneficial to community. Additional research on community-engaged strategies to enhance clinical research participation among rural populations is warranted [4].
Acknowledgements
This publication was supported by Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Disclosures
The authors have no conflict of interest to disclose.
References
- 1. Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer: Interdisciplinary International Journal of the American Cancer Society 2008; 112(2): 228–242. [DOI] [PubMed] [Google Scholar]
- 2. Rural America at a Glance. U.S. Department of Agriculture, 2021. [Google Scholar]
- 3. Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiology, Biomarkers & Prevention 2017; 26(7): 992–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen X, Orom H, Hay JL, et al. Differences in rural and urban health information access and use. Journal of Rural Health 2019; 35(3): 405–417. DOI: 10.1111/jrh.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Golembiewski E, Gravholt D, Torres Roldan V, et al. Rural patient experiences of accessing care for chronic conditions: a systematic review and thematic synthesis of qualitative studies. Annals of Family Medicine 2022; 3(3): 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davis TC, Arnold CL, Mills G, Miele L. A qualitative study exploring barriers and facilitators of enrolling underrepresented populations in clinical trials and biobanking. Frontiers in Cell and Developmental Biology 2019; 7: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Temple K. NIH National Center for Advancing Translational Sciences: Involving Rural America in Research. Rural Monitor 2019. (https://www.ruralhealthinfo.org/rural-monitor/ncats-rural-research/)
- 8. Health CoSDo. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health. World Health Organization, 2008. [DOI] [PubMed] [Google Scholar]
- 9. Leppin AL, Mahoney JE, Stevens KR, et al. Situating dissemination and implementation sciences within and across the translational research spectrum. Journal of Clinical and Translational Science 2020; 4(3): 152–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Department of Health and Human Services (HSS). Rural Action Plan, 2020. (hhs.gov)
- 11. Julian McFarlane S, Occa A, Peng W, Awonuga O, Morgan SE. Community-based participatory research (CBPR) to enhance participation of racial/ethnic minorities in clinical trials: a 10-year systematic review. Health Communication 2022; 37(9): 1075–1092. [DOI] [PubMed] [Google Scholar]
- 12. Baquet CR, Bromwell JL, Hall MB, Frego JF. Rural community-academic partnership model for community engagement and partnered research. Progress in Community Health Partnerships: Research, Education, and Action 2013; 7(3): 281–290. DOI: 10.1353/cpr.2013.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wieland ML, Njeru JW, Alahdab F, Doubeni CA, Sia IG. Community-Engaged approaches for minority recruitment into clinical research: a scoping review of the literature. Mayo Clinic Proceedings 2021; 96(3): 733–743. [DOI] [PubMed] [Google Scholar]
- 14. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 2018; 169(7): 467–473. [DOI] [PubMed] [Google Scholar]
- 15. Institute of Medicine (US) Clinical Research Roundtable. The role of purchasers and payers in the clinical research enterprise: workshop summary. In Tunis S, Korn A, Ommaya A, eds. Washington, DC: National Academies Press (US); 2002. DOI: 10.17226/10400. (https://www.ncbi.nlm.nih.gov/books/NBK220723/) [DOI] [PubMed] [Google Scholar]
- 16.Participation IAfP. IAP2 Public Participation Spectrum. (https://iap2.org.au/resources/iap2-published-resources/)
- 17. Warren BS, Maley M, Sugarwala LJ, Wells MT, Devine CM. Small steps are easier together: a goal-based ecological intervention to increase walking by women in rural worksites. Preventive Medicine 2010; 50(5-6): 230–234. [DOI] [PubMed] [Google Scholar]
- 18. Hopper LN, Blackman KF, Page RA, et al. Seeds of HOPE: incorporating community-based strategies to implement a weight-loss and empowerment intervention in Eastern North Carolina. North Carolina Medical Journal 2017; 78(4): 230–236. [DOI] [PubMed] [Google Scholar]
- 19. Luque JS, Tarasenko YN, Reyes-Garcia C, et al. Salud es Vida: a cervical cancer screening intervention for rural Latina immigrant women. Journal of Cancer Education 2017; 32(4): 690–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Andreae SJ, Halanych JH, Cherrington A, Safford MM. Recruitment of a rural, southern, predominantly African-American population into a diabetes self-management trial. Contemporary Clinical Trials 2012; 33(3): 499–506. [DOI] [PubMed] [Google Scholar]
- 21. Sutton AL, Preston MA, Thomson M, et al. Reaching rural residents to identify colorectal cancer education and intervention targets. Journal of Cancer Education 2021; 36(2): 338–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yeary KHK, Moore PC, Gauss CH, et al. Reach and adoption of a randomized weight loss maintenance trial in rural African Americans of Faith: the WORD (Wholeness, Oneness, Righteousness, Deliverance). American Journal of Health Promotion 2019; 33(4): 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zoellner J, Hill JL, Grier K, et al. Peer reviewed: randomized controlled trial targeting obesity-related behaviors: better together healthy caswell county. Preventing Chronic Disease 2013; 10: E96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Levy BT, Wolff CK, Niles P, Morehead H, Xu Y, Daly JM. Radon testing: community engagement by a rural family medicine office. The Journal of the American Board of Family Medicine 2015; 28(5): 617–623. [DOI] [PubMed] [Google Scholar]
- 25. Angell KL, Kreshka MA, McCoy R, et al. Psychosocial intervention for rural women with breast cancer. Journal of General Internal Medicine 2003; 18(7): 499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Westfall JM, Zittleman L, Sutter C, et al. Testing to prevent colon cancer: results from a rural community intervention. The Annals of Family Medicine 2013; 11(6): 500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Powell ME, Carter V, Bonsi E, et al. Increasing mammography screening among African American women in rural areas. Journal of Health Care for the Poor and Underserved 2005; 16(4): 11–21. [DOI] [PubMed] [Google Scholar]
- 28. Hillemeier MM, Downs DS, Feinberg ME, et al. Improving women’s preconceptional health: Findings from a randomized trial of the Strong Healthy Women intervention in the Central Pennsylvania women’s health study. Women’s Health Issues 2008; 18(6): S87–S96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Northridge ME, Vallone D, Xiao H, et al. The importance of location for tobacco cessation: rural-urban disparities in quit success in underserved West Virginia counties. The Journal of Rural Health 2008; 24(2): 106–115. [DOI] [PubMed] [Google Scholar]
- 30. Kogan SM, Lei M-K, Brody GH, Futris TG, Sperr M, Anderson T. Implementing family-centered prevention in rural African American communities: a randomized effectiveness trial of the strong African American families program. Prevention Science 2016; 17(2): 248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. KH-cK Yeary, Cornell CE, Moore P, et al. Peer reviewed: feasibility of an evidence-based weight loss intervention for a faith-based, rural, African American population. Preventing Chronic Disease 2011; 8(6): A146. [PMC free article] [PubMed] [Google Scholar]
- 32. Dake JA, Price JH, McKinney M, Ward B. Midwestern rural adolescents’ anal intercourse experience. The Journal of Rural Health 2011; 27(2): 196–204. [DOI] [PubMed] [Google Scholar]
- 33. Kogan SM, Cho J, Oshri A. The influence of childhood adversity on rural black men’s sexual risk behavior. Annals of Behavioral Medicine 2016; 50(6): 813–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lilly CL, Bryant LL, Vu MB, et al. Evaluation of the effectiveness of a problem-solving intervention addressing barriers to cardiovascular disease prevention behaviors in 3 underserved populations: Colorado, North Carolina, West Virginia, 2009. Preventing Chronic Disease 2014; 11: E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Valerio MA, Rodriguez N, Winkler P, et al. Comparing two sampling methods to engage hard-to-reach communities in research priority setting. BMC Medical Research Methodology 2016; 16(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tussing-Humphreys L, Thomson JL, Mayo T, Edmond E. A church-based diet and physical activity intervention for rural, lower Mississippi Delta African American adults: Delta Body and Soul effectiveness study, 2010-2011. Preventing Chronic Disease 2013; 10: E92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lemacks JL, James RE, Abbott L, et al. The church bridge project: an academic-community perspective of a church-based weight management pilot intervention among young adult African Americans. Progress in Community Health Partnerships: Research, Education, and Action 2018; 12(1 Suppl): 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Folta SC, Paul L, Nelson ME, et al. Changes in diet and physical activity resulting from the Strong Hearts, Healthy Communities randomized cardiovascular disease risk reduction multilevel intervention trial. International Journal of Behavioral Nutrition and Physical Activity 2019; 16(1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Abbott LS, Slate EH, Graven LJ. Cardiovascular disease risk among rural residents living with diabetes and prediabetes: a cluster randomized trial. Public Health Nursing 2020; 37(1): 16–24. [DOI] [PubMed] [Google Scholar]
- 40. Vines AI, Hunter JC, White BS, Richmond AN. Building capacity in a rural North Carolina community to address prostate health using a lay health advisor model. Health Promotion Practice 2016; 17(3): 364–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kupfer DJ, Axelson DA, Birmaher B, et al. Bipolar disorder center for Pennsylvanians: implementing an effectiveness trial to improve treatment for at-risk patients. Psychiatric Services 2009; 60(7): 888–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cruz TH, Davis SM, FitzGerald CA, Canaca GF, Keane PC. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in rural American Indian and Hispanic children. The Journal of Primary Prevention 2014; 35(3): 135–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Harrell TK, Davy BM, Stewart JL, King DS. Effectiveness of a school-based intervention to increase health knowledge of cardiovascular disease risk factors among rural Mississippi middle school children. Southern Medical Journal 2005; 98(12): 1173–1181. [DOI] [PubMed] [Google Scholar]
- 44. Love CV, Taniguchi TE, Williams MB, et al. Diabetes and obesity associated with poor food environments in American Indian communities: the Tribal Health and Resilience in Vulnerable Environments (THRIVE) Study. Current Developments in Nutrition 2019; 3(Supplement_2): 63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Logan HL, Guo Y, Emanuel AS, et al. Determinants of first-time cancer examinations in a rural community: a mechanism for behavior change. American Journal of Public Health 2015; 105(7): 1424–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Nguyen HT, Arcury TA, Grzywacz JG, et al. The association of mental conditions with blood glucose levels in older adults with diabetes. Aging & Mental Health 2012; 16(8): 950–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hilgeman MM, Mahaney-Price AF, Stanton MP, et al. Alabama Veterans Rural Health Initiative: a pilot study of enhanced community outreach in rural areas. The Journal of Rural Health 2014; 30(2): 153–163. [DOI] [PubMed] [Google Scholar]
- 48. Briant KJ, Sanchez JI, Ibarra G, et al. Using a culturally tailored intervention to increase colorectal cancer knowledge and screening among Hispanics in a rural community. AACR 2018; 27(11): 1283–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemporary Clinical Trials 2009; 30(1): 63–70. [DOI] [PubMed] [Google Scholar]
- 50. De Marco M, Kearney W, Smith T, Jones C, Kearney-Powell A, Ammerman A. Growing partners: building a community-academic partnership to address health disparities in rural North Carolina. Progress in Community Health Partnerships: Research, Education, and Action 2014; 8(2): 181–186. [DOI] [PubMed] [Google Scholar]
- 51. Zoellner J, Connell CL, Santell R, et al. Fit for Life Steps: results of a community walking intervention in the rural Mississippi Delta. Progress in Community Health Partnerships: Research, Education, and Action 2007; 1(1): 49–60. [DOI] [PubMed] [Google Scholar]
- 52. Jernigan VBB, Williams M, Wetherill M, et al. Using community-based participatory research to develop healthy retail strategies in Native American-owned convenience stores: the THRIVE study. Preventive Medicine Reports 2018; 11: 148–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McMahon SK, Wyman JF, Belyea MJ, Shearer N, Hekler EB, Fleury J. Combining motivational and physical intervention components to promote fall-reducing physical activity among community-dwelling older adults: a feasibility study. American Journal of Health Promotion 2016; 30(8): 638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gold MR, Franks P. A community-oriented primary care project in a rural population: reducing cardiovascular risk. The Journal of Family Practice 1990; 30(6): 639–644. [PubMed] [Google Scholar]
- 55. Jones DL, Starcher RW, Eicher JL, Wilcox S. Adoption of a Tai Chi intervention, Tai Ji Quan: moving for better balance, for fall prevention by rural faith-based organizations, 2013-2014. Preventing Chronic Disease 2016; 13: E92. DOI: 10.5888/pcd13.160083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Befort CA, Bennett L, Christafano D, Klemp JR, Krebill H. Effective recruitment of rural breast cancer survivors into a lifestyle intervention. Psycho-Oncology 2015; 24(4): 487–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Flynn BS, Gavin P, Worden JK, Ashikaga T, Gautam S, Carpenter J. Community education programs to promote mammography participation in rural New York State. Preventive Medicine 1997; 26(1): 102–108. [DOI] [PubMed] [Google Scholar]
- 58. Leach CR, Schoenberg NE, Hatcher J. Factors associated with participation in cancer prevention and control studies among rural Appalachian women. Family & Community Health 2011; 34(2): 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Estabrooks P, You W, Hedrick V, Reinholt M, Dohm E, Zoellner J. A pragmatic examination of active and passive recruitment methods to improve the reach of community lifestyle programs: the Talking Health Trial. International Journal of Behavioral Nutrition and Physical Activity 2017; 14(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Abbott L, Williams C, Slate E, Gropper S. Promoting heart health among rural African Americans. Journal of Cardiovascular Nursing 2018; 33(1): E8–E14. [DOI] [PubMed] [Google Scholar]
- 61. Tiwari T. Recruitment for health disparities preventive intervention trials: the early childhood caries collaborating centers. Preventing Chronic Disease 2014; 11: E133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Schroepfer TA, Matloub J, Creswell P, Strickland R, Anderson DM. A community-specific approach to cancer research in Indian country. Progress in Community Health Partnerships: Research, Education, and Action 2009; 3(4): 317–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Allman RM, Sawyer P, Crowther M, Strothers III HS, Turner T, Fouad MN. Predictors of 4-year retention among African American and white community-dwelling participants in the UAB study of aging. The Gerontologist 2011; 51(suppl_1): S46–S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lane HG, Porter KJ, Hecht E, Harris P, Zoellner JM. A participatory process to engage Appalachian youth in reducing sugar-sweetened beverage consumption. Health Promotion Practice 2019; 20(2): 258–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Levy I, Cohen-Louck K, Bonny-Noach H. Gender, employment, and continuous pandemic as predictors of alcohol and drug consumption during the COVID-19. Drug and Alcohol Dependence 2021; 228: 109029. DOI: 10.1016/j.drugalcdep.2021.109029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wilkins C, Spofford M, Williams N, et al. CTSA Consortium’s Community Engagement Key Function Committee Community Partners Integration Workgroup. Community representatives’ involvement in clinical and translational science awardee activities. Clinical and Translational Science 2013; 6: 292–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Emmel N, Hughes K, Greenhalgh J, Sales A. Accessing socially excluded people—Trust and the gatekeeper in the researcher-participant relationship. Sociological Research Online 2007; 12(2): 43–55. [Google Scholar]
- 68. Alvarez RA, Vasquez E, Mayorga CC, Feaster DJ, Mitrani VB. Increasing minority research participation through community organization outreach. Western Journal of Nursing Research 2006; 28(5): 541–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Holzer JK, Ellis L, Merritt MW. Why we need community engagement in medical research. Journal of Investigative Medicine 2014; 62(6): 851–855. DOI: 10.1097/jim.0000000000000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Clauser SB, Johnson MR, OʼBrien DM, Beveridge JM, Fennell ML, Kaluzny AD. Improving clinical research and cancer care delivery in community settings: evaluating the NCI community cancer centers program. Implementation Science 2009; 4(1): 63. DOI: 10.1186/1748-5908-4-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. CDC A. Principles of Community Engagement. NIH publication, 2011. [Google Scholar]
- 72. Spears CR, Nolan BV, O’Neill JL, Arcury TA, Grzywacz JG, Feldman SR. Recruiting underserved populations to dermatologic research: a systematic review. International Journal of Dermatology 2011; 50(4): 385–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Javed T, Idris S. Impact of employee ownership on an organizational productivity: a mediating role of psychological ownership. Academy of Accounting and Financial Studies Journal 2018; 22(2): 1–12. [Google Scholar]
- 74. U.S. Department of Agriculture (USDA), Economic Research Service. American Indians remain disproportionally rural. 2014. (https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=77893)
- 75. Saunkeah B, Beans JA, Peercy MT, Hiratsuka VY, Spicer P. Extending research protections to tribal communities. The American Journal of Bioethics 2021; 21(10): 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Fitzpatrick EF, Martiniuk AL, D’Antoine H, Oscar J, Carter M, Elliott EJ. Seeking consent for research with indigenous communities: a systematic review. BMC Medical Ethics 2016; 17(1): 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Datta R. Decolonizing both researcher and research and its effectiveness in Indigenous research. Research Ethics 2018; 14(2): 1–24. [Google Scholar]
- 78. Walters KL, Simoni JM. Decolonizing strategies for mentoring American Indians and Alaska Natives in HIV and mental health research. American Journal of Public Health 2009; 99(S1): S71–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]