Abstract
Background
Social deprivation is a major risk factor of adverse pregnancy outcomes. Yet, there is few studies evaluating interventions aiming at reducing the impact of social vulnerability on pregnancy outcomes.
Objective
To compare pregnancy outcomes between patients that received personalized pregnancy follow-up (PPFU) to address social vulnerability versus standard care.
Methods
Retrospective comparative cohort in a single institution between 2020 and 2021. A total of 3958 women with social vulnerability that delivered a singleton after 14 gestational weeks were included, within which 686 patients had a PPFU. Social vulnerability was defined by the presence of at least one of the following characteristics: social isolation, poor or insecure housing conditions, no work-related household income, and absence of standard health insurance (these four variables were combined as a social deprivation index (SDI)), recent immigration (< 12 month), interpersonal violence during pregnancy, being handicaped or minor, addiction during pregnancy. Maternal characteristics and pregnancy outcomes were compared between patients that received PPFU versus standard care. The associations between poor pregnancy outcomes (premature birth before 37 gestational weeks (GW), premature birth before 34 GW, small for gestational age (SGA) and PPFU were tested using multivariate logistic regression and propensity score matching.
Results
After adjustment on SDI, maternal age, parity, body mass index, maternal origin and both high medical and obstetrical risk level before pregnancy, PPFU was an independent protective factor of premature birth before 37 gestational weeks (GW) (aOR = 0.63, 95%CI[0.46–0.86]). The result was similar for premature birth before 34 GW (aOR = 0.53, 95%CI [0.34–0.79]). There was no association between PPFU and SGA (aOR = 1.06, 95%CI [0.86 – 1.30]). Propensity score adjusted (PSa) OR for PPFU using the same variables unveiled similar results, PSaOR = 0.63, 95%CI[0.46–0.86] for premature birth before 37 GW, PSaOR = 0.52, 95%CI [0.34–0.78] for premature birth before 34 GW and PSaOR = 1.07, 95%CI [0.86 – 1.33] for SGA.
Conclusions
This work suggests that PPFU improves pregnancy outcomes and emphasizes that the detection of social vulnerability during pregnancy is a major health issue.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-023-05604-7.
Keywords: Social vulnerability, Social deprivation, Neonatal outcomes, Neonatal morbidity, SGA, Small for gestational age, Pregnancy outcomes
Background
Since the 80 s, social deprivation has been demonstrated to be a major contributor of inequalities in health [1]. It is now well established that socially deprived women experience more pregnancy complications with an increased risk small for gestational age newborn [2], stillbirth [2, 3], premature birth [4–9], extremely premature birth (both spontaneous and induced [10, 11]). Therefore, neonatal morbidity and mortality are more frequent in socially deprived women [12, 13]. Several works aiming at explaining these discrepancies in term of adverse pregnancy outcomes reported that socially deprived women do not use properly prenatal care [14, 15]. Indeed, vulnerable women seems to address their pregnancy follow-up late, with a lower number of pregnancy consultations and often don’t realize the appropriate number of screening ultrasound [16–18]. Therefore, it seems relevant to detect social deprivation in order to improve perinatal care use and reduce the impact of social vulnerability on pregnancy outcomes. Yet, studies aiming at evaluating the impact of measures to improve the perinatal care use for deprived women are rare. Three studies from the US have demonstrated that the detection of social vulnerability and an appropriate follow-up regarding this latter allowed to reduce stress factors such as interpersonal violence, addiction during pregnancy and improved perinatal care use in socially deprived women [19]. Moreover, two of these studies demonstrated that the companionship of these patients reduced the rate of SGA new-born [20] and premature birth in some sub-groups [21]. Consequently, the finding of new interventions to address social vulnerability is a major health issue. The aim of this study is to evaluate whether a personalized pregnancy follow-up (PPFU) to ease the access to both prenatal care and relevant interventions regarding the patient’s vulnerability would improve neonatal morbidity in case of maternal social vulnerability.
Material and methods
Study population
This study is a retrospective comparative cohort between patients that received PPFU versus standard care in case of maternal social vulnerability.
Maternal social vulnerability was defined as the presence of at least one of the following social vulnerabilities: social isolation, poor or insecure housing conditions, no work-related household income, absence of standard health insurance, recent immigration (< 12 month), linguistic barrier, interpersonal violence during pregnancy, being handicapped or minor, addiction during or before pregnancy.
The PPFU unit was implemented in the maternity unit at study in 2017 by the financial help of the local health administration (Agence Régionale de la Santé Île-de-France). It aims at improving maternal pregnancy follow-up in case of social vulnerability to decrease both maternal and neonatal morbidity. It consists of a multidisciplinary unit including midwifes, obstetricians, social workers, psychologists and psychiatrists. The PPFU trains all the professionals of the maternity unit in the detection of social vulnerability so that the detected patients can benefit from a PPFU. The PPFU unit takes care of the consultation booking (both medical and ultrasound appointments) and propose to the included patient a personalized follow-up regarding the relevant needs, (social worker, psychologist, addiction therapist etc.…) that are highlighted by a dedicated multidisciplinary staff. The training of all the professionals of the maternity unit allowed to have access to thorough data regarding social vulnerabilities in the patient’s medical folders.
Standard care in the maternity unit at study is based on the national health authority (Haute Autorité de Santé) recommendations [22], which consists for low-risk pregnancies in 7 consultations performed by midwives and three screening ultrasounds (first trimester, second trimester and third trimester of pregnancy). In case of pregnancy complications or high medical risk level at the beginning of pregnancy, the consultations were performed by obstetricians.
Inclusion criteria in the present study were the combination of the following factors: presence of maternal social vulnerability and a singleton delivery in cephalic presentation after 14 gestational weeks.
Exclusion criteria were one of the following: the absence of maternal social vulnerability, multiple pregnancy, delivery before 14 gestational weeks or non-cephalic presentation at delivery.
Patients’ allocation to PFFU was performed as follow: when maternal social vulnerability was detected during pregnancy follow-up, the practitioner on duty should send a request to the PPFU for inclusion. The PPFU discusses the folders in a multidisciplinary staff and contacts the patients for consent. If the patient accepts, she is included in the PPFU that will provide a personalized pregnancy follow-up.
Patients with maternal social vulnerability that refused PPFU inclusion or that were not reported to the PPFU by the practitioner were included in the standard care group.
Using birth records, a total of 7643 patients who delivered a singleton in cephalic presentation after 14 weeks of gestation were identified between January 2020 and December 2021, in a single tertiary care maternity unit (CHI-Montreuil). Patients that presented maternal social vulnerability (N = 3958) were included in the study: 686 patients in the PPFU group that were compared with 3272 patients in the standard care group.
Collected data
Maternal, pregnancy, labor, delivery, and neonatal characteristics were collected from patient’s computerized pregnancy folder whose content was checked after each delivery in a multidisciplinary staff. Social vulnerabilities were defined as follow: social isolation (absence of partner), Poor or insecure housing condition (no rented nor owned housing), no work-related household income (the woman’s household income came from public assistance, relatives, friends, or a charity), No permanent health care insurance (Couverture Maladie Universelle, CMU) or illegal status (Aide Médicale d’Etat, AME)). These four variables were combined as a quantitative score called the social deprivation index. This latter was developed from the national French survey of 2010 and has been demonstrated to be relevant in classifying the degree of social deprivation in the French population [23].
Recent immigration was defined by an immigration within France < 12 months, linguistic barrier was defined by the need of an interpret during patient follow-up, interpersonal violence during pregnancy was defined as interpersonal violence during pregnancy requiring establishment of protective measures, addictions (before and during pregnancy) were defined by tobacco, alcohol, cannabis, cocaine derived drug or morphine derive drug use, unwanted pregnancy was defined as an unplanned pregnancy that was not desired by the mother.
Inadequate prenatal care use (PCU) was implemented the same way as a former French cohort study of social deprivation [15]: pregnancy follow up began after 12 weeks of gestation, or if it included less than 50% of the number of prenatal visits expected according to duration of pregnancy, or if the first-trimester ultrasound examination or both the second- and third- trimester examinations were missing.
Psychologic follow-up was performed in case of pregnancy related anxiety, depressive symptoms, or patient request for a psychologist follow-up.
Psychiatrist follow-up was performed in case of major depressive disorder, bipolar disorder, post-traumatic stress disorder or Schizophrenia.
Gestational weight gain (GWG) was calculated by subtracting the last measured weight before delivery with the maternal weight before pregnancy. GWG was considered adequate if it was ≥ 1.22 kg per month and ≤ 1.77 kg per month for women presenting a BMI < 30 kg/m2 (total pregnancy intake between 11 and 16 kg) [24]. GWG was considered adequate if it was ≥ 0.55 kg per month and ≤ 0.75 kg per month for women presenting a BMI ≥ 30 kg/m2(total pregnancy intake between 5 and 9 kg) [24].
SGA status was defined by a birthweight < to the 10th percentile according to the WHO fetal growth charts [25]. High medical risk level before pregnancy was defined as the presence of one or more of: history of cardiac disease, hypertension, diabetes, venous thrombosis, pulmonary embolism, Graves’ disease, asthma, homozygous sickle cell anemia, thrombocytopenia, coagulation disorder, a rare or systemic disease, nephropathy, HIV infection, psychiatric disease.
High obstetrical risk level before pregnancy was defined by a history of one or more of the following: pre-eclampsia, fetal growth restriction, preterm delivery, fetal death or neonatal death.
Pregnancy complication was defined as the occurrence of one or more of the following complications: gestational diabetes, pre-eclampsia, fetal growth restriction, proteinuria, thrombocytopenia, threatened preterm labor, preterm premature rupture of membranes (PPROM), deep vein thrombosis and intrahepatic cholestasis of pregnancy.
Stillbirth was defined as a fetal death occurring after 20 gestational weeks.
Statistical analysis
Maternal, pregnancy, labor, delivery, and neonatal characteristics were compared using Chi2 or Fisher exact tests for categorical variables and Student’s or Wilcoxon rank sum tests for quantitative variables, as appropriate. All tests were two-sided with p-values < 0.05 defined as statistically significant. The independent association between premature birth < 37 GW, premature birth < 34 GW and neonatal composite morbidity and PPFU was tested using multiple logistic regression. Adjustment was performed on known confusion factors and the variables that differed between the PPFU and standard care group: maternal age, parity, SDI, BMI, high medical risk level before pregnancy and high obstetrical risk level before pregnancy. No multicollinearity was detected using variance inflation factor. Visual inspection of residual plots did not reveal any obvious deviations from homoscedasticity or normality. Propensity score matching was then used (Matchit package [26]) to test the association between PPFU and adverse pregnancy outcomes. Patients in the PPFU group were matched to two patients in the standard care group based on maternal age, parity, BMI, high medical risk level before pregnancy and high obstetrical risk level before pregnancy. Each of the variables included in the propensity score matching were balanced between the two groups. R software (R Development Core Team (2008), version 4.2.0) was used for all analyses.
Ethics
This study (IRB00012437) was approved by the French “Comité d’Éthique de la recherche de l’hopital Foch) ethic committee and is part of the PRECACHIM project aiming at improving maternal and neonatal outcomes in case of maternal social vulnerability. This observational study waived the need to obtain informed consent according to the French law. Women were informed that their records could be used for the evaluation of medical practices and were allowed to opt out of these studies.
Results
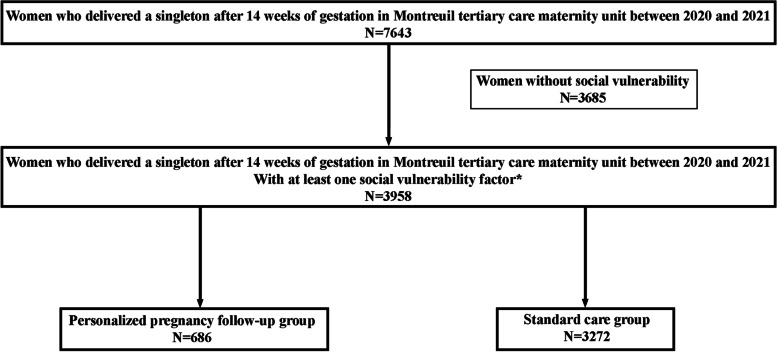
Between January 2020 and December 2021, 3958 women with social vulnerability who delivered a singleton after 14 gestational weeks were included in the study (Fig. 1): 686 in the PPFU group and 3272 in the standard care one. Patients in the PFFU group were younger and presented lower BMI (Table 1). Excessive and insufficient GWG were equally distributed between the two study groups. The PPFU group included more patients with a Sub-Saharan Africa origin. High medical risk level before pregnancy was more frequent in the PPFU group. Women included in the PPFU group presented a higher SDI with a larger number of patients presenting a SDI ≥ 3 (45% versus 19% in the standard care group, p < 0.001). Recent immigration, interpersonal violence during pregnancy and addictions both before and during pregnancy were more frequent in the PFFU group. Minor patients and patients with handicap were all included in the PPFU group. Linguistic barrier was more frequent in the standard care group. Patients with unwanted pregnancy were more prevalent in the PPFU group.
Fig. 1.
Flow Chart. *social isolation, poor or insecure housing conditions, no work-related household income, absence of standard health insurance, recent immigration (< 12 month), linguistic barrier, history of violence, being handicapped or minor, addictions
Table 1.
Maternal characteristics according to study groups
| PPFU Participation | |||
|---|---|---|---|
| Yes (N = 686) | No (N = 3272) | p | |
| Maternal characteristics | |||
| Maternal age (years, mean (SD)) | 29.01 (6.84) | 30.59 (5.72) | < 0.001 |
| Maternal age ≥ 35 years n (%) | 144 (21.0) | 778 (23.8) | 0.129 |
| Parity (mean (SD)) | 1.36 (1.52) | 1.37 (1.41) | 0.909 |
| Pre-pregnancy body mass index (kg/m2, mean (SD)) | 25.77 (5.15) | 26.37 (5.57) | 0.010 |
| Maternal obesity (BMI > 30 kg/m2) n (%) | 120 (17.5) | 681 (20.8) | 0.055 |
| Gestational weight gain n (%) | 0.106 | ||
| Insufficient | 327 (47.7) | 1427 (43.6) | |
| Adequate | 246 (35.9) | 1221 (37.3) | |
| Excessive | 113 (16.5) | 624 (19.1) | |
| Maternal origin n (%) | < 0.001 | ||
| Sub-Saharan Africa | 351 (51.2) | 1259 (38.5) | |
| Asia | 67 (9.8) | 389 (11.9) | |
| Caucasian | 268 (39.1) | 1624 (49.6) | |
| High medical risk level before pregnancya n (%) | 150 (21.9) | 383 (11.7) | < 0.001 |
| High obstetrical risk level before pregnancyb n (%) | 166 (24.2) | 909 (27.8) | 0.061 |
| Social deprivation indexc n (%) | < 0.001 | ||
| 0 | 94 (13.7) | 223 (6.8) | |
| 1 | 102 (14.9) | 1394 (42.6) | |
| 2 | 181 (26.4) | 1025 (31.3) | |
| ≥ 3 | 309 (45.0) | 630 (19.3) | |
| Type of vulnerability | |||
| Social isolation n (%) | 329 (48.0) | 950 (29.0) | < 0.001 |
| Poor or insecure housing condition n (%) | 259 (37.8) | 869 (26.6) | < 0.001 |
| Not work-related household income n (%) | 481 (70.1) | 2040 (62.3) | < 0.001 |
| No permanent health care insurance n (%) | 432 (63.0) | 1605 (49.1) | < 0.001 |
| Recent immigrationd n (%) | 191 (27.8) | 162 (5.0) | < 0.001 |
| Linguistic barrier n (%) | 69 (10.1) | 423 (12.9) | 0.045 |
| Interpersonal violence during pregnancy n (%) | 373 (54.4) | 173 (5.3) | < 0.001 |
| Handicap/minor n (%) | 213 (31.0) | 0 (0.0) | < 0.001 |
| Addiction before pregnancy n (%) | 183 (26.7) | 557 (17.0) | < 0.001 |
| Addiction during pregnancy n (%) | 156 (22.7) | 423 (12.9) | < 0.001 |
| Unwanted pregnancy n (%) | 26 (3.8) | 18 (0.6) | < 0.001 |
| Prenatal care utilization | |||
| Inadequate PCUe n (%) | 181 (26.4) | 486 (14.9) | < 0.001 |
| Term of first consultation (mean (SD)) | 23.99 (7.03) | 24.50 (6.67) | 0.073 |
| Social worker intervention n (%) | 390 (57.3) | 525 (16.3) | < 0.001 |
| Addiction therapy n (%) | 38 (5.5) | 51 (1.6) | < 0.001 |
| Psychologic follow-upf n (%) | 393 (57.3) | 365 (11.2) | < 0.001 |
| Psychiatrist follow-upg n (%) | 98 (14.3) | 33 (1.0) | < 0.001 |
| Number of pregnancy consultation (mean (SD)) | 6.52 (5.65) | 5.30 (4.05) | < 0.001 |
| Number of hospitalization (mean (SD)) | 1.66 (1.46) | 1.52 (1.18) | 0.006 |
| Number of Emergency consultation (mean (SD)) | 1.69 (1.88) | 1.59 (1.79) | 0.200 |
adefined as the presence of one or more of: history of cardiac disease, hypertension, diabetes, venous thrombosis, pulmonary embolism, Graves’ disease, asthma, homozygous sickle cell anemia, thrombocytopenia, coagulation disorder, a rare or systemic disease, nephropathy, HIV infection, psychiatric disease
bdefined by a history of one or more of the following: pre-eclampsia, fetal growth restriction, preterm delivery, fetal or neonatal death
csimple sum of 4 deprivation dimensions: social isolation, poor or insecure housing condition, not work-related household income, and no permanent heath care insurance
epregnancy follow-up began after 12 weeks of gestation, or if it included less than 50% of the number of prenatal visits expected according to duration of pregnancy, or if the first-trimester ultrasound examination or both the second- and third- trimester examinations were missing
fPsychologic follow-up was performed in case of pregnancy related anxiety, depressive symptoms, or patient request for a psychologist follow-up
gPsychiatrist follow-up was performed in case of major depressive disorder, bipolar disorder, post-traumatic stress disorder or Schizophrenia
Inadequate PCU was more frequent in the PPFU group (Table 1). Women included in the PPFU group benefitted from more social worker intervention, addiction therapy, psychologic and psychiatric follow-up compared to the standard care group. The number of pregnancy follow-up appointments and hospitalizations was higher in the PPFU group whereas emergency consultations were equally distributed between the two groups.
Pregnancy complications were similar between the two groups (Table 2) and each complication taken separately was equally distributed (Additional Table 1).
Table 2.
Pregnancy, labor and neonatal outcomes according to study group
| PPFU Participation | |||
|---|---|---|---|
| Yes (N = 686) | No (N = 3272) | p | |
| Pregnancy characteristics | |||
| Pregnancy complicationa n (%) | 433 (63.1) | 2128 (65.0) | 0.362 |
| Labor outcomes | |||
| Induction of labor n (%) | 258 (37.6) | 1177 (36.0) | 0.443 |
| Delivery mode n (%) | |||
| Cesarean section before labor | 57 (8.3) | 193 (5.9) | 0.023 |
| Emergency Cesarean section before labor | 28 (4.1) | 129 (3.9) | 0.95 |
| Cesarean section during labor | 77 (11.2) | 314 (9.6) | 0.22 |
| Post-Partum hemorrhage n (%) | 48 (7.0) | 214 (6.5) | 0.724 |
| Neonatal outcomes | |||
| Premature birth (< 37 weeks) n (%) | 59 (8.6) | 357 (10.9) | 0.084 |
| Premature birth (< 34 weeks) n (%) | 29 (4.2) | 209 (6.4) | 0.038 |
| Neonatal intensive care unit admission n (%) | 46 (6.7) | 318 (9.7) | 0.016 |
| 5-min Apgar score < 7 | 18 (2.6) | 83 (2.5) | 1.000 |
| Cord blood pH < 7.10 | 24 (3.5) | 118 (3.6) | 0.980 |
| Small for gestational agec n (%) | 159 (23.2) | 671 (20.5) | 0.131 |
| Pregnancy outcome n (%) | 0.263 | ||
| Neonatal death | 1 (0.1) | 1 (0.0) | |
| Miscarriage/abortus | 2 (0.3) | 17 (0.5) | |
| Medical abortion | 2 (0.3) | 23 (0.7) | |
| Stillbirth | 3 (0.4) | 30 (0.9) | |
PPFU Personalized pregnancy follow-up
adefined as the occurrence of one or more of the following complications: gestational diabetes, pre-eclampsia, fetal growth restriction, proteinuria, thrombopenia, threatened preterm labor, premature rupture of membranes (PROM), deep vein thrombosis and cholestasis of pregnancy
bdefined by a cord blood pH < 7.10 and/or a 5-min Apgar score < 7 and/or neonatal intensive care unit admission
cSmall for gestational was defined by a birthweight < to the 10th percentile according to the WHO fetal growth charts
Induction of labor was similar between the two groups (Table 2). Women included in the PPFU group delivered more often by cesarean section before labor whereas the emergency cesarean section rates were similar between the two groups.
Regarding neonatal outcomes, the premature birth < 37 GW rate were similar between the two groups (10.9% in the standard care group versus 8.6% in the PPFU group, p = 0.084) whereas the PPFU group unveiled a lower rate of premature birth < 34 GW (6.4% for the standard care group and 4.2% in the PPFU one, p = 0.038). SGA status was equally distributed between the group groups. Women in the PPFU group had a lower rate of NICU admission (6.7% for the PPFU group versus 9.7% for the standard care group).
After adjustment on the social deprivation index, maternal age, parity, BMI, maternal origin, high medical and high obstetrical risk level before pregnancy (Table 3), PPFU was associated with a reduced risk of premature birth < 37 GW (aOR = 0.66, 95%CI[0.49–0.89]), a reduced risk of premature birth < 34 GW, (aOR = 0.53, 95%[0.34–0.79]). There was no association between PPFU and SGA (aOR = 1.06, 95%CI [0.86 – 1.30]). Propensity score matching adjusted (psa) OR performed on the same variables unveiled similar results for premature birth < 37 GW (psaOR = 0.63, 95%CI[0.46–0.86]), for premature birth < 34 GW (psaOR = 0.52, 95%CI[0.34–0.78] and for SGA status (psaOR = 1.07, 95%CI [0.86 – 1.33]).
Table 3.
Association between PPFU inclusion and poor neonatal outcomes
| Premature birth (< 37 weeks) | |||
| N = 3958 | OR | aOR | PSaOR |
| PPFU | 0.77 [0.57—1.02] | 0.66[0.49–0.89]** | 0.63[0.46–0.86]** |
| Social deprivation indexa | 1.08 [1.01 – 1.16]* | 1.16[1.04–1.30]* | |
| Maternal age | 1.03 [1.01 – 1.04]*** | 1.03[1.01–1.05]** | |
| Parity | 1.00 [0.93—1.07] | 0.91[0.83–0.98]* | |
| Pre-pregnancy body mass index (kg/m2) | 1.01 [0.99—1.03] | 0.99[0.98–1.01] | |
| Maternal origin | |||
| Caucasian | ref | ref | |
| Asian | 1.17 [0.84—1.61] | 1.18[0.84–1.63] | |
| Sub-Saharan Africa | 1.13 [0.91—1.40] | 1.15[0.92–1.44] | |
| High medical risk level before pregnancyb | 2.46 [1.92—3.12]*** | 2.44[1.89–3.12]*** | |
| High obstetrical risk level before pregnancyc | 1.67 [1.35—2.07]*** | 1.58[1.26–1.98]*** | |
| Premature birth (< 34 weeks) | |||
| N = 3958 | OR | aOR | PSaOR |
| PPFU | 0.65 [0.43—0.95]* | 0.53[0.34–0.79]** | 0.52[0.34–0.78]** |
| Social deprivation indexa | 1.18 [1.02—1.36]* | 1.28[1.11–1.49]** | |
| Maternal age | 1.04 [1.01—1.06]** | 1.05[1.02–1.07]*** | |
| Parity | 1.03 [1.01—1.05]* | 0.77[0.68–0.86]*** | |
| Pre-pregnancy body mass index (kg/m2) | 1.04 [1.02 – 1.06] | 1.02[0.99–1.04] | |
| Maternal origin | |||
| Caucasian | ref | ref | |
| Asian | 1.30 [0.84—1.96] | 1.31[0.84–1.98] | |
| Sub-Saharan Africa | 1.37 [1.04—1.82]* | 1.47[1.10–1.97]** | |
| High medical risk level before pregnancyb | 2.26 [1.77 – 2.86]*** | 2.45[1.77–3.34]*** | |
| High obstetrical risk level before pregnancyc | 1.83 [1.50 – 2.23]*** | 1.70[1.27–2.26]*** | |
| Small for gestational aged | |||
| N = 3958 | OR | aOR | PSaOR |
| PPFU | 1.17 [0.96 – 1.42] | 1.06 [0.86 – 1.30] | 1.07 [0.86 – 1.33] |
| Social deprivation indexa | 1.09 [1.00 – 1.18]* | 1.07 [0.98 – 1.16] | |
| Maternal age | 0.99 [0.98 – 1.00] | 1.01 [0.99 – 1.02] | |
| Parity | 0.87 |0.82 – 0.92]*** | 0.87 [0.81 – 0.93]*** | |
| Pre-pregnancy body mass index (kg/m2) | 0.96 [0.95 – 0.97]*** | 0.96 [0.95 – 0.98]*** | |
| Maternal origin | |||
| Caucasian | ref | ref | |
| Asian | 1.27 [0.99 – 1.63] | 1.27 [0.98 – 1.62] | |
| Sub-Saharan Africa | 1.36 [1.16 – 1.60]*** | 1.45 [1.22 – 1.71]*** | |
| High medical risk level before pregnancyb | 1.14 [0.91 – 1.41] | 1.20 [0.96 – 1.50] | |
| High obstetrical risk level before pregnancyc | 0.83 [0.70 – 1.00] | 0.93 [0.78 – 1.12] | |
PPFU Personalized pregnancy follow-up
OR Odd ratio
aOR Adjusted OR, adjustment on maternal age, parity, SDI, BMI, high medical risk level before pregnancy and high obstetrical risk level before pregnancy
PSaOR Propensity score adjusted OR, patients in the PPFU group were matched to two patients in the standard care group based on maternal age, parity, BMI, high medical risk level before pregnancy and high obstetrical risk level before pregnancy
*p < 0.05
**p < 0.01
***p < 0.001
asimple sum of 4 deprivation dimensions: social isolation, poor or insecure housing condition, not work-related household income, and no permanent heath care insurance
bdefined as the presence of one or more of: history of cardiac disease, hypertension, diabetes, venous thrombosis, pulmonary embolism, Graves’ disease, asthma, homozygous sickle cell anemia, thrombocytopenia, coagulation disorder, a rare or systemic disease, nephropathy, HIV infection, psychiatric disease
cdefined by a history of one or more of the following: pre-eclampsia, fetal growth restriction, preterm delivery, fetal or neonatal death
dSmall for gestational was defined by a birthweight < to the 10th percentile according to the WHO fetal growth charts
Discussion
To our knowledge, this retrospective study is the first to evaluate a personalized patient-based intervention to address all types of social vulnerabilities with the aim of reducing poor neonatal outcomes. This work highly suggests that PPFU reduces the impact of social stress factors on prematurity and neonatal morbidity by improving medical care access and coordination for socially deprived women.
Indeed, patients included in the PPFU group had a significantly better access to any of the different care providers such as social care workers, psychologists, and addiction therapist. Even if inadequate PCU was more frequent at patient inclusion in the PPFU group, PPFU patients had more pregnancy follow-up appointments and were more often hospitalized (Table 1). This point suggests that PPFU patients had a more appropriate pregnancy follow-up given that the rate of pregnancy complications was similar between the two groups and might explain the differences observed in terms of prematurity. Moreover, maternal psychiatric disorders [27], pregnancy related anxiety in socially deprived women [28] and maternal stress [29] are established risk factors of premature birth. Therefore, the benefit regarding prematurity in the PPFU group can be explained by the difference in terms of psychologic follow-up, psychiatric follow-up, and addiction therapy.
The novelty of our personalized clinical approach comes from the facts that PPFU addresses all types of maternal social vulnerability and proposes customized pregnancy follow-up. Former studies aiming at reducing the impact of social vulnerabilities on neonatal outcomes in the US demonstrated that reducing psychosocial stress factor along with dietary counselling [20] or improving prenatal care access [21] reduces the rate of low birth weight and prematurity in the sub-group of Hispanic women [21]. Yet, within these studies, included patients were proposed similar pregnancy follow-up and only particular types of social vulnerabilities were addressed.
This work suggests that PPFU reduces prematurity regardless of maternal ethnicity. Yet, PPFU had no impact on SGA rates compared to the two studies carried out in the US [20, 21]. This point can be explained by the absence of dietary counselling within the PPFU. Indeed, inadequate GWG was similar between the PPFU and standard care group.
It is of importance to highlight that this study was carried out in high risk patients with high figures of social vulnerability, which was also the case for the two aforementioned studies [20, 21]. Indeed, a recent randomized control trial in the Netherlands testing an intervention aiming at detecting and addressing social deprivation in a low risk population that didn’t reach the expected figures of social deprivation [30], didn’t show any benefit regarding low birth weight and premature birth.
It is of note that the results are consistent with previous studies addressing social vulnerability and poor pregnancy outcomes (Table 3). Indeed, the increase of the social deprivation index was independently associated with premature birth (< 37 GW) (aOR = 1.16[1.04–1.30] for one point increase of the SDI), premature birth (< 34GW) (aOR = 1.28[1.11–1.49]) [2, 4, 5, 7, 16, 23]. In addition, these data are consistent with the impact of PCU on pregnancy outcomes unveiled in former studies [15, 16]. Indeed, the main differences between the two study groups resides in the access to both medical and non-medical prenatal care (Table 1). This suggests that the differences observed in terms of poor neonatal outcomes comes from the improvement of prenatal care use.
The main strength of this study is the combined accurate and thorough access to both precise data on the social vulnerabilities and medical factors thanks to the computerized patient folder. This was the result of the training of all the professionals of the maternity unit performed by the PPFU unit midwifes since 2017, in the detection of social vulnerabilities. Moreover, the sample size of socially deprived women is substantial compared to former studies conducted in France [10, 15, 31]. The access to medical and obstetrical history of the patients allowed to properly adjust on medical and non-medical factors in the multiple logistic regression and propensity score matching (Table 3).
Yet, this study is not without limitations. The retrospective and unicentric design might limit the generalization of the results. Indeed, the population studied in this work presented a high level of social deprivation with 54.2% of the included patients presenting a SDI ≥ 2 and 23.7% with a SDI ≥ 3. Moreover, the neighborhood of the maternity unit at study present a high level of social deprivation with a high rate of neonatal mortality [32]. Finally, the vulnerable women population included in this study presented a high medical risk level and a high rate of pregnancy complications (Table 1, and Table 2). Therefore, the application of the same protocol in a less socially deprived population with a lower medical risk might alter the impact of PPFU. Lastly, the retrospective design of this study lessens the strength of the results. Yet, testing this intervention in a prospective randomized manner would be ethically questionable given the impact of social vulnerabilities on pregnancy outcomes.
Conclusions
This work suggests that PPFU to address social vulnerabilities reduces prematurity and neonatal morbidity. These results could be explained by an improvement of relevant prenatal care access.
Further research should focus on characterizing the relevant non-medical needs according to social vulnerability profiles to improve both mother’s and neonates’ wellbeing.
Supplementary Information
Acknowledgements
The PRECACHIM project investigators deeply thank all the midwives and obstetrician that participated in the collection of accurate data on social vulnerabilities in each patient folder.
Abbreviations
- PPFU
Personalized pregnancy follow-up
- SDI
Social deprivation index
- SGA
Small for gestational age
- PCU
Prenatal care use
- BMI
Body mass index
- OR
Odd ratio
- aOR
Adjusted Odd ratio
- PSaOR
Propensity score adjusted odd ratio
Authors’ contributions
SC participated in the experimental design, data collection, statistical analysis and writing of the manuscript, GB participated in data collection and reviewing of the manuscript, MP and SB participated in data collection and reviewing of the manuscript, ADL participated in writing of the manuscript, NS participated in writing of the manuscript and ethical approval, BR participated in the experimental design and writing of the manuscript. The author(s) read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study (IRB00012437) was approved by the French “Comité d’Éthique de la recherche de l’hopital Foch) ethic committee and is part of the PRECACHIM project aiming at improving maternal and neonatal outcomes in case of maternal social vulnerability. This observational study waived the need to obtain informed consent according to the French law (article L1121-1–1 du Code de la Santé Publique). Women were informed that their records could be used for the evaluation of medical practices and were allowed to opt out of these studies. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gray AM. Inequalities in health. the black report: a summary and comment. Int J Health Serv. 1982;12(3):349–380. doi: 10.2190/XXMM-JMQU-2A7Y-HX1E. [DOI] [PubMed] [Google Scholar]
- 2.Vos AA, Posthumus AG, Bonsel GJ, Steegers EAP, Denktaş S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2014;93(8):727–740. doi: 10.1111/aogs.12430. [DOI] [PubMed] [Google Scholar]
- 3.Reeske A, Kutschmann M, Razum O, Spallek J. Stillbirth differences according to regions of origin: an analysis of the German perinatal database, 2004–2007. BMC Pregnancy Childbirth. 2011;11(1):63. doi: 10.1186/1471-2393-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calling S, Li X, Sundquist J, Sundquist K. Socioeconomic inequalities and infant mortality of 46 470 preterm infants born in Sweden between 1992 and 2006: Infant mortality inequalities in Swedish preterms. Paediatr Perinat Epidemiol. 2011;25(4):357–365. doi: 10.1111/j.1365-3016.2011.01200.x. [DOI] [PubMed] [Google Scholar]
- 5.Auger N, Park AL, Gamache P, Pampalon R, Daniel M. Weighing the contributions of material and social area deprivation to preterm birth. Soc Sci Med. 2012;75(6):1032–1037. doi: 10.1016/j.socscimed.2012.04.033. [DOI] [PubMed] [Google Scholar]
- 6.Reime B, Ratner PA, Tomaselli-Reime SN, Kelly A, Schuecking BA, Wenzlaff P. The role of mediating factors in the association between social deprivation and low birth weight in Germany. Soc Sci Med. 2006;62(7):1731–1744. doi: 10.1016/j.socscimed.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Taylor-Robinson D, Agarwal U, Diggle PJ, Platt MJ, Yoxall B, Alfirevic Z. Quantifying the impact of deprivation on preterm births: a retrospective cohort study. Middleton P, ed. PLoS ONE. 2011;6(8):e23163. doi: 10.1371/journal.pone.0023163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janevic T, Stein CR, Savitz DA, Kaufman JS, Mason SM, Herring AH. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Ann Epidemiol. 2010;20(6):445–451. doi: 10.1016/j.annepidem.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huynh M, Parker JD, Harper S, Pamuk E, Schoendorf KC. Contextual effect of income inequality on birth outcomes. Int J Epidemiol. 2005;34(4):888–895. doi: 10.1093/ije/dyi092. [DOI] [PubMed] [Google Scholar]
- 10.Bonet M, Smith LK, Pilkington H, Draper ES, Zeitlin J. Neighbourhood deprivation and very preterm birth in an English and French cohort. BMC Pregnancy Childbirth. 2013;13(1):97. doi: 10.1186/1471-2393-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith LK, Draper ES, Manktelow BN, Field DJ. Deprivation and infection among spontaneous very preterm births. Obstet Gynecol. 2007;110(2):325–329. doi: 10.1097/01.AOG.0000270158.57566.2f. [DOI] [PubMed] [Google Scholar]
- 12.Smith LK, Manktelow BN, Draper ES, Springett A, Field DJ. Nature of socioeconomic inequalities in neonatal mortality: population based study. BMJ. 2010;341:c6654–c6654. doi: 10.1136/bmj.c6654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poeran J, Maas AFG, Birnie E, Denktas S, Steegers EAP, Bonsel GJ. Social deprivation and adverse perinatal outcomes among Western and non-Western pregnant women in a Dutch urban population. Soc Sci Med. 2013;83:42–49. doi: 10.1016/j.socscimed.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Herbst MA, Mercer BM, Beazley D, Meyer N, Carr T. Relationship of prenatal care and perinatal morbidity in low-birth-weight infants. Am J Obstet Gynecol. 2003;189(4):930–933. doi: 10.1067/S0002-9378(03)01055-X. [DOI] [PubMed] [Google Scholar]
- 15.Gonthier C, Estellat C, Deneux-Tharaux C, et al. Association between maternal social deprivation and prenatal care utilization: the PreCARE cohort study. BMC Pregnancy Childbirth. 2017;17(1):126. doi: 10.1186/s12884-017-1310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linard M, Blondel B, Estellat C, et al. Association between inadequate antenatal care utilisation and severe perinatal and maternal morbidity : an analysis in the PreCARE cohort. BJOG. Int J Obstet Gy. 2018;125(5):587–595. doi: 10.1111/1471-0528.14794. [DOI] [PubMed] [Google Scholar]
- 17.Partridge S, Balayla J, Holcroft C, Abenhaim H. Inadequate prenatal care utilization and risks of infant mortality and poor birth outcome: a Retrospective Analysis of 28,729,765 U.S. deliveries over 8 years. Amer J Perinatol. 2012;29(10):787–794. doi: 10.1055/s-0032-1316439. [DOI] [PubMed] [Google Scholar]
- 18.Kapaya H, Mercer E, Boffey F, Jones G, Mitchell C, Anumba D. Deprivation and poor psychosocial support are key determinants of late antenatal presentation and poor fetal outcomes-a combined retrospective and prospective study. BMC Pregnancy Childbirth. 2015;15(1):309. doi: 10.1186/s12884-015-0753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joseph JG, El-Mohandes AAE, Kiely M, et al. Reducing psychosocial and behavioral pregnancy risk factors: results of a randomized clinical trial among high-risk pregnant African American women. Am J Public Health. 2009;99(6):1053–1061. doi: 10.2105/AJPH.2007.131425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ricketts SA, Murray EK, Schwalberg R. Reducing low birthweight by resolving risks: results from colorado’s prenatal plus program. Am J Public Health. 2005;95(11):1952–1957. doi: 10.2105/AJPH.2004.047068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arima Y, Guthrie BL, Rhew IC, De Roos AJ. The impact of the first steps prenatal care program on birth outcomes among women receiving Medicaid in Washington State. Health Policy. 2009;92(1):49–54. doi: 10.1016/j.healthpol.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Suivi et orientation des femmes enceintes en fonction des situations à risque identifiées. La Revue Sage-Femme. 2007;6(4):216–218. doi:10.1016/S1637-4088(07)79647-5
- 23.Opatowski M, Blondel B, Khoshnood B, Saurel-Cubizolles MJ. New index of social deprivation during pregnancy: results from a national study in France. BMJ Open. 2016;6(4):e009511. doi: 10.1136/bmjopen-2015-009511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sebire N, Jolly M, Harris J, et al. Maternal obesity and pregnancy outcome: a study of 287 213 pregnancies in London. Int J Obes. 2001;25(8):1175–1182. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 25.Kiserud T, Piaggio G, Carroli G, et al. The world health organization fetal growth charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. Myers JE, ed. PLoS Med. 2017;14(1):e1002220. doi: 10.1371/journal.pmed.1002220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho DE, Imai K, King G, Stuart EA. MatchIt : Nonparametric preprocessing for parametric causal inference. J Stat Soft. 2011;42(8). doi:10.18637/jss.v042.i08.
- 27.Männistö T, Mendola P, Kiely M, et al. Maternal psychiatric disorders and risk of preterm birth. Ann Epidemiol. 2016;26(1):14–20. doi: 10.1016/j.annepidem.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kramer MS, Lydon J, Seguin L, et al. Stress pathways to spontaneous preterm birth: the role of stressors, psychological distress, and stress hormones. Am J Epidemiol. 2009;169(11):1319–1326. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- 29.Lobel M, Dunkel-Schetter C, Scrimshaw SC. Prenatal maternal stress and prematurity: a prospective study of socioeconomically disadvantaged women. Health Psychol. 1992;11(1):32–40. doi: 10.1037/0278-6133.11.1.32. [DOI] [PubMed] [Google Scholar]
- 30.Lagendijk J, Vos AA, Bertens LCM, et al. Antenatal non-medical risk assessment and care pathways to improve pregnancy outcomes: a cluster randomised controlled trial. Eur J Epidemiol. 2018;33(6):579–589. doi: 10.1007/s10654-018-0387-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lelong A, Jiroff L, Blanquet M, et al. Is individual social deprivation associated with adverse perinatal outcomes? results of a French multicentre cross-sectional survey. :7. [PMC free article] [PubMed]
- 32.Carayol M, Bucourt M, Cuesta J, Zeitlin J, Blondel B. Mortalité néonatale en Seine-Saint-Denis : analyse des certificats de décès néonatals. J Gynecol Obstet Biol Reprod. 2013;42(3):271–274. doi: 10.1016/j.jgyn.2012.10.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.