Abstract
Our recently published study of >2.4 million adults in Northern California indicated that current versus never-tobacco smoking was associated with lower risk of SARS-CoV-2 infection and less severe coronavirus disease 2019 (COVID-19). We extended this research by evaluating whether these associations were moderated by socio-demographic factors and medical comorbidities. This retrospective cohort study of 1,885,826 adults with current or never-smoking status in Kaiser Permanente Northern California from 3/5/2020 (baseline) to 12/31/2020 (pre-vaccine) included electronic health record-based socio-demographics (sex, age, race/ethnicity, neighborhood deprivation index (NDI)) and medical comorbidities (obesity, cardiovascular conditions, diabetes, renal disease, respiratory conditions). We estimated the adjusted risk of SARS-CoV-2 infection and hospitalization (≤30 days of infection) associated with smoking status using Cox proportional hazard regression models. We estimated associations within subgroups of socio-demographics and comorbidities, and tested for effect modification using interaction terms. During the study, 35,627 patients had SARS-CoV-2 infection. Current versus never-smoking status was associated with lower adjusted rates of SARS-CoV-2 infection (aHR ranging from 0.51 to 0.89) and hospitalization (aHR ranging from 0.32 to 0.70) within nearly every socio-demographic and comorbidity subgroup. Statistically significant interactions showed that the magnitude of protection for SARS-CoV-2 infection varied by sex, age, race/ethnicity, NDI, cardiovascular conditions and diabetes, and for SARS-CoV-2 hospitalization by age and renal disease. Taken together, results indicated that while some socio-demographics and comorbidities moderated the associations, the lower risk of SARS-CoV-2 infection and hospitalization associated with current versus never-smoking status persisted among patients regardless of socio-demographics or comorbidities.
Keywords: COVID-19, SARS-CoV-2, Smoking, Tobacco, Nicotine, Comorbidities, Age, Race, Hospitalization
1. Introduction
The World Health Organization (WHO) has called for well-designed population-based studies to determine whether tobacco smoking is associated with SARS-CoV-2 infection and coronavirus disease 2019 (COVID-19) severity (World Health Organization, 2023). While many prior studies have found that current versus never-smoking is associated with lower risk of SARS-CoV-2 infection (Simons et al., 2021; Lee et al., 2021; Tsigaris and Teixeira da Silva, 2020; Paleiron et al., 2021; Prinelli et al., 2021; Nono Djotsa et al., 2022), studies of COVID-19 severity are equivocal (Farsalinos et al., 2021; Gulsen et al., 2020; Patanavanich and Glantz, 2020; Umnuaypornlert et al., 2021; Razjouyan et al., 2022). Existing research has suffered from limitations, including non-representative samples (e.g., voluntary participants, people tested for active infection, hospitalized patients), smoking status misclassification (e.g., due to inconsistent recording or combining former smoking with current or never-smoking), and inadequate adjustment for important potential confounders.
Addressing many of these limitations, our recent retrospective cohort study of 2.4 million adults in Northern California within a closed healthcare system followed from testing and infection to death, examined the association between smoking status (never, former, current) and risk of SARS-CoV-2 infection and disease severity (Young-Wolff et al., 2023). Results indicated that current versus never tobacco smoking was associated with a lower risk of SARS-CoV-2 infection and lower risk of severe disease (hospitalization, intensive care unit [ICU] admissions, and death). Former versus never-smoking was associated with a slightly lower risk of SARS-CoV-2 infection and greater risk of hospitalization and death. The associations with former smoking were greatly reduced after adjusting for covariates. Given the strong associations for current vs. never-smoking status, we sought to further investigate whether these associations persisted across subgroups of patients at risk for more severe COVID-19 (e.g., racial/ethnic minorities, those with lower socioeconomic status, older age, male sex, and smoking-related comorbidities) (Razjouyan et al., 2022; Young-Wolff et al., 2023; Karmakar et al., 2021).
In the current population-based cohort study, we extended our prior work to test whether the associations between current versus never-smoking and polymerase chain reaction (PCR)-confirmed SARS-CoV-2 infection and COVID-19-related hospitalization were moderated by patient socio-demographics and medical comorbidities associated with increased risk for more severe COVID-19 (e.g., racial/ethnic minorities, those with lower socioeconomic status, older age, male sex, and smoking-related comorbidities) (Karmakar et al., 2021; Centers for Disease Control and Prevention, 2023; Pijls et al., 2022). Results are critical to inform better understanding of the epidemiology of SARS-CoV-2 infection and disease severity and to provide key information about whether differences in risks associated with current versus never-smoking vary among vulnerable subsets of the population.
2. Methods
2.1. Setting and population
KPNC is a multispecialty, integrated healthcare delivery system serving >4 million diverse individuals who are representative of the insured population in Northern California (Gordon, 2020). Full details of this cohort have been presented previously (Young-Wolff et al., 2023). Briefly, we conducted a retrospective cohort study of KPNC enrollees from March 5, 2020 to December 31, 2020 and included patients aged ≥18 years, with continuous KPNC health plan membership in the year prior (March 2019–March 2020), ≥1 in-person outpatient or inpatient non-emergency visit, and non-missing smoking status from March 5, 2018-March 2020. The KPNC IRB approved and waived informed consent for this study.
Of those 2,430,241 KPNC members meeting inclusion criteria, we excluded 120 (0.0%) missing sex and 2828 (0.1%) missing neighborhood deprivation index (NDI). For this follow-up study examining current versus never-smoking status, we additionally excluded 541,467 (22.2%) patients with former smoking status, for a final sample of 1,885,826 (eSupplement 1).
2.2. Measures
Measures have been described in detail elsewhere (Young-Wolff et al., 2023). Briefly, outcomes included: 1) SARS-CoV-2 infection documented by KPNC (based on a positive nasal/throat swab for SARS-CoV-2 by polymerase chain reaction [PCR]), and 2) COVID-19-related hospitalization (excluding hospitalizations associated with elective surgeries, trauma, and labor/delivery) from 5-days before to 30-days after a positive test. We did not include outcomes of ICU admission or death due to the small numbers of patients with these outcomes in stratified analyses.
Tobacco smoking status from routine primary care screening by medical assistants while taking patients' vital signs was extracted from the Electronic Health Record [EHR] and defined as the most recent charted status during the 2 years before study start.
Sociodemographics and medical comorbidities analyzed for evidence of moderation included age, sex, race/ethnicity, Medicaid insurance, NDI (Messer et al., 2006) (categorized into tertiles, with higher values representing greater deprivation), most recent documented body mass index (BMI = kg/m2; not obese<30 and obese≥30.0), and medical comorbidities associated with COVID-19 risk (diabetes, cardiovascular conditions [hypertension, atherosclerotic cardiovascular disease, cardiac dysrhythmias, heart failure], renal disease, and respiratory conditions [obstructive lung diseases, lung cancer, other lung conditions]) classified by ICD-10 codes (eSupplement 2) (Young-Wolff et al., 2023). Data on potential moderators were extracted from the EHR during the 2 years before study start.
2.3. Analysis
First, we estimated the association of current vs never-smoking and the two study outcomes (SARS-CoV-2 infection & COVID-19 related hospitalization) within each socio-demographic and comorbidity subgroup using separate multivariable Cox proportional hazards regression models. Next, we tested whether these associations varied with sociodemographic characteristics and medical comorbidities by including a term for the interaction between smoking status and each moderator in multivariable Cox proportional hazards regression models. Following the same modeling framework as our prior study (Young-Wolff et al., 2023), we adjusted for all socio-demographics and medical comorbidities except for smoking-related respiratory conditions, as they could be mediators rather than confounders. Respiratory conditions were only adjusted for in the model that examined an interaction between smoking status and respiratory conditions. We report the fully-adjusted hazard ratios (aHRs) and 95% confidence intervals (CI) from the stratified analyses, and the interaction p-values from the interaction models.
As done previously (Young-Wolff et al., 2023), patients were followed from study start (March 5, 2020) until outcome occurrence, with censoring on death, health plan disenrollment, or study end (November 30, 2020 for infection, December 31, 2020 for hospitalization). Patients with SARS-CoV-2 infection who were not hospitalized within 30 days of their positive PCR test were censored on the 30th day following that test. Analyses were conducted using SAS software, v9.4. Statistical significance was assessed at two-sided p < .05.
3. Results
The sample consisted of 1,739,938 (92.2%) patients with never-smoking status and 145,888 (7.8%) patients with current smoking status. The sample had a median (interquartile range) of 118 (42–229) days since the most recently recorded smoking status at study start. Smoking status was assessed within 1 year of study start for 94.2% of patients who self-reported current smoking and 93.0% who self-reported never-smoking. Patients with current smoking status were similar to those with never-smoking status on most socio-demographics and comorbidities, but were more likely to be male (59.3% vs. 39.0%) (eSupplement 3).
COVID PCR-testing prevalence was comparable among patients with current (24.7%) and never-smoking status (24.6%).
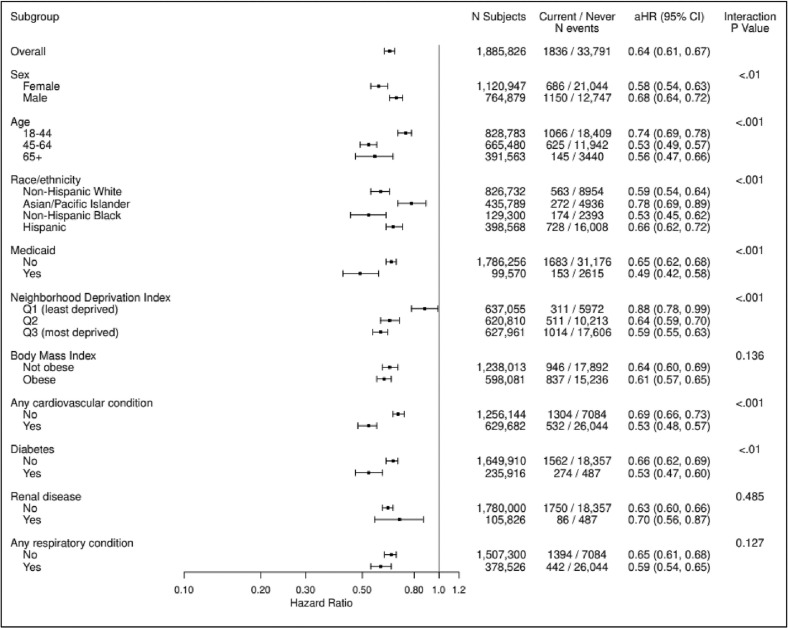
3.1. SARS-CoV-2 infection
Overall, 1836 (1.3%) of patients with current smoking status and 33,791 (1.9%) of patients with never-smoking status had a positive PCR test for SARS-CoV-2 over the study period. Current versus never-smoking was associated with a lower risk of SARS-CoV-2 infection (aHR 0.64, 95% CI:0.61–0.67). Nearly all within strata/subgroup associations for the risk of SARS-CoV-2 infection comparing current versus never-smoking status were statistically significant and < 1 (aHR ranging from 0.49 to 0.89), indicating a lower risk of SARS-CoV-2 infection for current versus never-smoking status (Fig. 1 ), with the exception of the first tertile of NDI (least deprived) (aHR 0.89, 95% CI:0.77–1.03). Those aged 45–64 years old (aHR 0.53, 95%CI:0.49–0.57), non-Hispanic Black patients (aHR 0.53, 95% CI:0.45–0.62), those with cardiovascular conditions (aHR 0.53, 95% CI:0.48–0.57), and those with diabetes (aHR 0.53, 95% CI:0.47–0.60) had the lowest risk of SARS-CoV-2 infection associated with current vs. never-smoking.
Fig. 1.
Cox Proportional Hazard Regression Results for Risk of SARS-CoV-2 Infection Associated with Current vs. Never-Smoking Status in KPNC, Overall and by Socio-Demographic Characteristics and Chronic Health Conditions, March 5, 2020 to December 31, 2020 (N = 1,885,826).
Statistically significant interactions showed that the magnitude of protection for SARS-CoV-2 infection varied by sex, age, race/ethnicity, NDI, cardiovascular conditions and diabetes. However, the same general pattern of lower risk of SARS-CoV-2 infection for current versus never-smoking was observed across subgroups. For example, the interaction between smoking status and sex was statistically significant (p < .01), although associations were fairly similar in magnitude, with a slightly stronger association among females (aHR 0.58, 95% CI:0.54–0.63) than males (aHR 0.68, 95% CI:0.64–0.72). These small differences may not be clinically meaningful, and the consistency of the overall pattern of lower risk of SARS-CoV-2 infection within each subgroup was quite robust.
3.2. Hospitalization
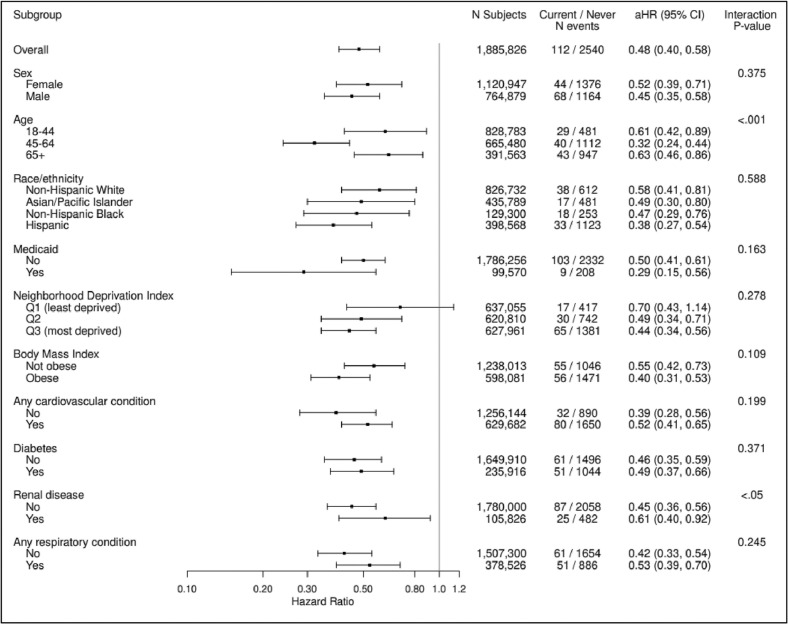
Overall, 112 (0.1%) of patients with current smoking status and 2540 (0.1%) of patients with never-smoking status were hospitalized for COVID-19 over the study period and current vs never-smoking status was associated with a lower risk of COVID-19 related hospitalization (aHR 0.48, 95% CI:0.40–0.58). Almost all within strata/subgroup associations for the risk of COVID-19 related hospitalization comparing current versus never-smoking status were statistically significant and < 1 (aHR ranging from 0.32 to 0.70; Fig. 2 ), with the exception of Other/Unknown race/ethnicity (not shown) and those living in the least deprived neighborhoods. Across subgroups, the lowest risk of hospitalization associated with current vs. never-smoking was found for those with Medicaid insurance (aHR 0.29, 95% CI: 0.15, 0.56).
Fig. 2.
Cox Proportional Hazard Regression Results for Risk of COVID-19 Related Hospitalization Associated with Current vs. Never-smoking Status in KPNC, Overall and by Socio-Demographic Characteristics and Chronic Health Conditions, March 5, 2020 to December 31, 2020 (N = 1,885,826).
Statistically significant interactions showed that the magnitude of protection for COVID-19 related hospitalization varied by age and renal disease. However, the same general pattern of lower risk of COVID-19 related hospitalization for current vs never-smoking status was observed across subgroups. For example, while the interaction between smoking status and renal disease was statistically significant (p < .05), the magnitudes of association were fairly similar, although slightly stronger among those without renal disease (aHR 0.45, 95% CI:0.36–0.54) versus with renal disease (aHR 0.53, 95% CI: 0.39–0.70).
4. Discussion
Using data from >1.8 million patients in a large, integrated healthcare delivery system in Northern California, we found that the lower risk of SARS-CoV-2 infection and COVID-19 related hospitalization associated with current versus never-smoking status generally persisted across patients regardless of socio-demographic factors or medical comorbidities. While there was evidence of moderation, such that there was significantly lower risk of SARS-CoV-2 infection and hospitalization associated with current versus never-smoking within certain strata of socio-demographics and comorbidities, the general pattern of results was consistent across strata. Results suggest that findings from our recently published cohort study are robust across patients with different socio-demographic and medical comorbidities.
Notably, in most cases where the risk of SARS-CoV-2 infection associated with smoking status was moderated by socio-demographics or comorbidities, the lower risk of infection tended to be among those in the more at-risk subgroups (e.g., those living in the most deprived neighborhoods, those with cardiovascular conditions, those with diabetes). This could reflect potential differences in heaviness of smoking across subgroups. This pattern did not hold for the outcome of hospitalization, where there were fewer significant interactions, potentially due to lower power/smaller sample sizes. Hypothesized biologically plausible mechanisms for reduced risk SARS-CoV-2 infection and severe COVID-19 associated with current versus never-smoking have been described in detail elsewhere (Young-Wolff et al., 2023; Boutou et al., 2020a; Lutchman, 2020; Tindle et al., 2020; Usman et al., 2021). Tobacco smoke and nicotine may downregulate the expression of angiotensin-converting enzyme 2 (ACE2), the principal receptor for SARS-CoV-2, which could prevent viral particles from entering cells thus reduce infection rates (Young-Wolff et al., 2023; Boutou et al., 2020a; Lutchman, 2020; Tindle et al., 2020; Usman et al., 2021). Nicotine also has anti-inflammatory properties that could prevent or suppress cytokine storms and modulate COVID-19 severity (Young-Wolff et al., 2023; Boutou et al., 2020a; Lutchman, 2020; Tindle et al., 2020; Usman et al., 2021).
4.1. Limitations
Our cohort was limited to KPNC patients with a past-year in-person healthcare visit and results may not generalize to uninsured adults or those who did not interact with the healthcare system. However, because all patients were insured, results are unlikely to be due to variations in access to care. Tobacco smoking was based on the most recent smoking status in the EHR during the 2 years prior to the start of the study, and some patients may have been misclassified. While most patients had their smoking status updated within the year before COVID-19, status changes during the pandemic are not reflected. Our study took place during the first 9 months of the pandemic before home tests were available, and findings may not generalize to later in the pandemic. PCR-test results were limited to those recorded by KPNC and reasons for getting tested were not documented. Data on key aspects of tobacco use, including frequency, heaviness, and duration, were not available and should be included in future studies. Finally, while we adjusted for many covariates, some potentially important confounders (e.g., social distancing, essential worker designation, KPNC employee status) were not available. Notably, <2% of KPNC patients are KPNC employees (including non-patient facing employees).
5. Conclusions
During the first 9 months of the COVID-19 pandemic, before vaccines and treatments became widely available, lower risk of SARS-CoV-2 infection and COVID-19-related hospitalization associated with current versus never-smoking status generally persisted among patients regardless of socio-demographic factors or medical comorbidities. Results do not support prioritizing vaccination outreach or future treatments for individuals who currently smoke. Continued research is needed to replicate these findings and to better understand whether these risks have changed over time as the pandemic continues to unfold. Further, studies are needed to test whether nicotine replacement therapy (NRT) and other nicotinic agents might provide some protection against SARS-CoV-2 infection and COVID-19 severity (Simons et al., 2021; Lutchman, 2020; Tindle et al., 2020; Boutou et al., 2020b); however, initial data on nicotine application in patients hospitalized with COVID-19 show no benefit (Nono Djotsa et al., 2022). Importantly, population-based findings from our study cannot be used to predict individual-level risk for SARS-CoV-2 infection or hospitalization for any patient based on smoking status and other characteristics. Given the substantial increased risk of preventable morbidity and mortality associated with tobacco smoking, clinicians should continue to screen for smoking status, strongly encourage patients who smoke to quit, offer cessation treatment, and provide referrals to evidence-based smoking cessation tools.
Funding
This study was supported by grants from the Tobacco-Related Disease Research Program (grant numbers R00RG2609 and R01RG3724) and a NIH NIDA K01 Award (DA043604). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Author contributions
Concept and design: Kelly C. Young-Wolff, Natalie Slama, Stacey E. Alexeeff. Acquisition, analysis, or interpretation of data: Kelly C. Young-Wolff, Natalie Slama, Lori C. Sakoda, Judith J. Prochaska, Renee Fogelberg, Stacey E. Alexeeff. Drafting of Manuscript: Kelly C. Young-Wolff, Natalie Slama. Critical revision of manuscript for important intellectual content: Kelly C. Young-Wolff, Natalie Slama, Lori C. Sakoda, Judith J. Prochaska, Renee Fogelberg, Stacey E. Alexeeff. Statistical Analysis: Natalie Slama, Stacey Alexeeff. Obtained funding: Kelly C. Young-Wolff. Administrative, technical or material support: Renee Fogelberg. All authors read and approved this manuscript.
Data sharing
The data underlying this article cannot be shared publicly as we do not have permission from patients to share their data outside of the Kaiser Permanente Northern California healthcare system.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Judith J. Prochaska, PhD, MPH, has provided consultation to pharmaceutical and technology companies that make medications and other treatments for quitting smoking and has served as an expert witness in lawsuits against the tobacco companies. All other authors declare no conflict of interest.
Acknowledgments
We acknowledge Agatha Hinman, BA, for her editorial assistance.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2023.107523.
Appendix A. Supplementary data
Supplementary material
Data availability
The authors do not have permission to share data.
References
- Boutou A.K., Pitsiou G., Kontakiotis T., Kioumis I. Nicotine treatment and smoking cessation in the era of COVID-19 pandemic: an interesting alliance. ERJ Open Res. 2020;6(3):00306–02020. doi: 10.1183/23120541.00306-2020. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutou A.K., Pitsiou G., Kontakiotis T., Kioumis I. Nicotine treatment and smoking cessation in the era of COVID-19 pandemic: an interesting alliance. ERJ Open Res. 2020;6(3) doi: 10.1183/23120541.00306-2020. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control & Prevention People with Certain Medical Conditions. 2023. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- Farsalinos K., Bagos P.G., Giannouchos T., Niaura R., Barbouni A., Poulas K. Smoking prevalence among hospitalized COVID-19 patients and its association with disease severity and mortality: an expanded re-analysis of a recent publication. Harm Reduct. J. 2021;18(1):9. doi: 10.1186/s12954-020-00437-5. Jan 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon N.P. Similarity of Adult Kaiser Permanente Members to the Adult Population in Kaiser Permanente's Northern California Service Area: Comparisons Based on the 2017/2018 Cycle of the California Health Interview Survey. 2020. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/compare_kp_ncal_chis2017-18.pdf Accessed Jan 4, 2023.
- Gulsen A., Yigitbas B.A., Uslu B., Dromann D., Kilinc O. The effect of smoking on COVID-19 symptom severity: systematic review and meta-analysis. Pulm. Med. 2020;2020:7590207. doi: 10.1155/2020/7590207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karmakar M., Lantz P.M., Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw. Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.36462. Jan 4. e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.C., Son K.J., Kim D.W., et al. Smoking and the risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Nicotine Tob. Res. 2021;23(10):1787–1792. doi: 10.1093/ntr/ntab079. Aug 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutchman D. Could the smoking gun in the fight against COVID-19 be the (rh)ACE-2? Eur. Respir. J. 2020;56(1) doi: 10.1183/13993003.01560-2020. Jul. 2001560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer L.C., Laraia B.A., Kaufman J.S., et al. The development of a standardized neighborhood deprivation index. J. Urban Health. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nono Djotsa A.B.S., Helmer D.A., Park C., et al. Assessing smoking status and risk of SARS-CoV-2 infection: a machine learning approach among veterans. Healthcare (Basel) 2022;10(7) doi: 10.3390/healthcare10071244. Jul 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paleiron N., Mayet A., Marbac V., et al. Impact of tobacco smoking on the risk of COVID-19: a large scale retrospective cohort study. Nicotine Tob. Res. 2021;23(8):1398–1404. doi: 10.1093/ntr/ntab004. Aug 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patanavanich R., Glantz S.A. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob. Res. 2020;22(9):1653–1656. doi: 10.1093/ntr/ntaa082. Aug 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pijls B.G., Jolani S., Atherley A., et al. Temporal trends of sex differences for COVID-19 infection, hospitalisation, severe disease, intensive care unit (ICU) admission and death: a meta-analysis of 229 studies covering over 10M patients. F1000Res. 2022;11:5. doi: 10.12688/f1000research.74645.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinelli F., Bianchi F., Drago G., et al. Association between smoking and SARS-CoV-2 infection: cross-sectional study of the EPICOVID19 internet-based survey. JMIR Public Health Surveill. 2021;7(4) doi: 10.2196/27091. Apr 28. e27091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razjouyan J., Helmer D.A., Lynch K.E., et al. Smoking status and factors associated with COVID-19 in-hospital mortality among US veterans. Nicotine Tob. Res. 2022;24(5):785–793. doi: 10.1093/ntr/ntab223. Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons D., Shahab L., Brown J., Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalization and mortality from COVID-19: a living rapid evidence review with Bayesian meta-analyses (version 7) Addiction. 2021;116(6):1319–1368. doi: 10.1111/add.15276. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle H.A., Newhouse P.A., Freiberg M.S. Beyond smoking cessation: investigating medicinal nicotine to prevent and treat COVID-19. Nicotine Tob. Res. 2020;22(9):1669–1670. doi: 10.1093/ntr/ntaa077. Aug 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsigaris P., Teixeira da Silva J.A. Smoking prevalence and COVID-19 in Europe. Nicotine Tob. Res. 2020;22(9):1646–1649. doi: 10.1093/ntr/ntaa121. Aug 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umnuaypornlert A., Kanchanasurakit S., Lucero-Prisno D.E.I., Saokaew S. Smoking and risk of negative outcomes among COVID-19 patients: a systematic review and meta-analysis. Tob. Induc. Dis. 2021;19:09. doi: 10.18332/tid/132411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usman M.S., Siddiqi T.J., Khan M.S., et al. Is there a smoker’s paradox in COVID-19? BMJ Evid. Based Med. 2021;26(6):279–284. doi: 10.1136/bmjebm-2020-111492. Dec. [DOI] [PubMed] [Google Scholar]
- World Health Organization Smoking and COVID-19: Scientific Brief. 2023. https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19
- Young-Wolff K.C., Slama N., Alexeeff S.E., et al. Tobacco smoking and risk of SARS-CoV-2 infection and disease severity among adults in an integrated healthcare system in California. Nicotine Tob. Res. 2023;25(2):211–220. doi: 10.1093/ntr/ntac090. Jan 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The authors do not have permission to share data.