Abstract
Background
An essential value in mental health care is compassion: awareness of suffering, tolerating difficult feelings in the face of suffering, and acting or being motivated to alleviate suffering. Currently, technologies for mental health care are on the rise and could offer several advantages, such as more options for self-management by clients and more accessible and economically viable care. However, digital mental health interventions (DMHIs) have not been widely implemented in daily practice. Developing and evaluating DMHIs around important mental health care values, such as compassion, could be key for a better integration of technology in the mental health care context.
Objective
This systematic scoping review explored the literature for previous instances where technology for mental health care has been linked to compassion or empathy to investigate how DMHIs can support compassion in mental health care.
Methods
Searches were conducted in the PsycINFO, PubMed, Scopus, and Web of Science databases, and screening by 2 reviewers resulted in 33 included articles. From these articles, we extracted the following data: technology types, goals, target groups, and roles of the technologies in the intervention; study designs; outcome measures; and the extent to which the technologies met a 5-step proposed definition of compassion.
Results
We found 3 main ways in which technology can contribute to compassion in mental health care: by showing compassion to people, by enhancing self-compassion in people, or by facilitating compassion between people. However, none of the included technologies met all 5 elements of compassion nor were they evaluated in terms of compassion.
Conclusions
We discuss the potential of compassionate technology, its challenges, and the need to evaluate technology for mental health care on compassion. Our findings could contribute to the development of compassionate technology, in which elements of compassion are explicitly embedded in its design, use, and evaluation.
Keywords: compassionate technology, digital mental health interventions, eHealth, e–mental health, compassion, mental health care
Introduction
Background
Currently, digital technologies for mental health care are on the rise [1,2]. Examples include not only internet-delivered cognitive behavioral therapy (CBT) but also virtual reality (VR) and artificial intelligence–enabled programs [3], mobile apps [4], socially assistive robotics [5], and serious games [6,7]. Given the increasing costs of care and growing waiting lists in this field, technology could be an important element of sustainable mental health care [3]. Technology offers a wealth of possibilities to complement health care professionals by taking over certain tasks, lightening their workload, and providing innovative ways to deliver health care [8]. In addition, technology can make mental health care more accessible to clients, give them more insight into their own mental health, and offer flexibility through personalization [9,10]. Digital mental health interventions (DMHIs) can be used as stand-alone interventions or in blended treatments: combining traditional face-to-face psychotherapy techniques with digital interventions [11]. Blended treatment has the potential to offer the best of both worlds, as it could be used to better match the intensity of the treatment to the severity of a client’s complaints and to enhance a client’s self-management [12].
Many forms of DMHIs exist and are shown to be effective in clinical trials [13], and if used well, they can often be as effective as face-to-face treatments [14-17]. However, the acceptance and use of these technologies remain low among both clients and professionals [18,19]; therefore, the actual implementation of DMHIs in daily practice has been limited. Among clients, there are low levels of adherence to DMHIs [20,21]. A potential reason for this could be that current DMHIs are often very direct translations of nondigital interventions, such as web-based CBT interventions, which closely follow their evidence-based nondigital versions [22]. Owing to the larger focus on content (eg, established therapeutic techniques) than on the user (eg, how the user prefers to engage with them), DMHIs are often perceived as impersonal [22]. This seems to be a missed opportunity, given that allowing for personalization is one of the advantages that technology could offer. Thus, the possibilities technology offers are not being optimally used. A further challenge is that professionals show hesitation and a lack of digital skills to implement DMHIs [18]. Similar to what we see from the client’s perspective, this hesitation in part stems from the doubt whether personal, empathic connections can be made or supported if DMHIs are used [18]. Moreover, professionals indicate that an explicit conceptual foundation for the use of DMHIs is currently lacking, meaning that it is not clear, and at best implicit, why and how DMHIs can be embedded in the mental health care system [19].
Compassionate Technology
Given these current barriers, a new conceptual foundation is needed to build a bridge between technology and the context of mental health care. This could be done by expanding our view of the design, use, and evaluation of DMHIs to include and center on the values that are foundational to mental health care. Values are personal or societal judgments of what is valuable and important in life [23]. Compassion is widely recognized as central and essential in mental health care or health care in general [24-26]. In short, compassion refers to the awareness of suffering and motivation to act to alleviate suffering. Although conceptions and practices surrounding compassion have existed in Buddhism for >2500 years, in Western psychology, the construct of compassion has become a topic of study only more recently [27].
After comparing and synthesizing earlier definitions and measures of compassion from science, religion, and health care, Strauss et al [28] proposed that compassion is a cognitive, affective, and behavioral process containing five elements: (1) recognizing suffering, (2) understanding the universality of suffering in the human experience, (3) feeling empathy for the person suffering and connecting with the distress (emotional resonance), (4) tolerating one’s own uncomfortable feelings that arise in the face of suffering (eg, distress, anger, and fear), to remain open and accepting of the person suffering, and (5) acting or feeling motivated to alleviate suffering [28].
Compassion can be directed not only toward ourselves (often referred to as self-compassion [29]) and loved ones but also toward strangers and ultimately toward all humankind [30].
Although empathy is part of the compassionate elements, compassion is conceptually different from empathy. Empathy has been defined as the vicarious experience of another’s emotions [31], where one understands, is affected by, and shares another’s emotions and perspectives [32]. It does not involve a motivation to act to alleviate another person’s suffering. More specifically, although empathy can also lead to behavioral outcomes, it is not part of the concept of empathy itself [33]. In contrast, the process of compassion is specifically a response to suffering and not to emotions in general. It not only entails connecting with another’s distress but also understanding the universality of suffering in the human experience and tolerating uncomfortable feelings that can be aroused in response to the suffering person, so that one can remain open and accept this person and then act to alleviate their suffering [28]. The ability to tolerate uncomfortable feelings is essential for preventing empathic distress. Empathic distress occurs when one is more upset by another’s suffering than one is concerned for the other [34]. It can lead people to close themselves off from suffering and tends to inhibit compassion [35,36]. Thus, compassion contains elements that are specifically relevant to mental health care, more so than empathy alone.
Embedding compassion in health care improves clinical outcomes, perceived quality of care, and patient satisfaction; strengthens the therapeutic alliance; and supports patient-centered care [28,37,38]. Although research is slowly beginning to include compassion as a factor in technology in general [39], research on the link between compassion and technology for mental health care is still scarce. An exception is a recent scoping review by Kemp et al [37], who investigated how digital technologies were being used by patients and professionals in the delivery of compassionate mental health care. In addition, it investigated the facilitators and barriers for the use of digital technology in the delivery of compassionate mental health care. The authors found that when used appropriately, digital technologies can facilitate and strengthen compassion and meaningful human connections in mental health care. Moreover, technology can create new means for relationships between mental health professionals and patients. Kemp et al [37] focused their review on compassionate care and examined DMHIs with a model of digital intersections with compassionate care [40]. In this review, we take a different but complementary approach, examining DMHIs with the elements of compassion in itself [28]. This way, we aimed to explore how DMHIs could support the different components of compassion as a process. We expect this process-view of compassion could be a helpful and practical guiding force to shape compassionate blended treatment.
As compassion is a pivotal value in the mental health care context, emphasizing the process of compassion as a central value in the design, evaluation, and use of mental health care technology could be key to make it more suitable to the needs of clients and professionals. In turn, this could increase the uptake and integration of technologies in current treatments, ultimately ensuring compassionate blended mental health care that realizes its potential. On the basis of the proposed definition of compassion by Strauss et al [28], technology that is designed, developed, and evaluated around the value of compassion would enable and facilitate elements of compassion, or in short, the recognition and alleviation of suffering. To the best of our knowledge, this concept of compassionate technology for mental health care has not been systematically studied. This highlights the need for a clear conceptualization of compassionate technology based on research in which DMHIs have been explicitly linked to compassion.
Research Objectives
This systematic scoping review provides an overview of how and to what degree elements of compassion have been linked to digital technologies for mental health or mental health care in previous studies. We used this information to describe the current status and scope of research on technology that is connected to compassion and to inform the future development of compassionate technology.
To reach these aims, we formulated the following research questions:
What types of technology for mental health care have been connected to compassion in previous studies, for what goals and which target groups were they developed, and what was the role of the technology in the intervention (eg, stand-alone or blended treatment)?
What study designs have previously been used to study these technologies, and what outcome measures are used?
To what extent and how do these technologies meet the 5 elements of compassion as distinguished by Strauss et al [28]?
Methods
Research Design
A systematic scoping review was conducted in accordance with existing guidelines [41]. This approach is particularly useful for bringing together the literature in disciplines with emerging evidence when a body of the literature has not yet been reviewed or exhibits a large, complex, or heterogeneous nature that is not suitable for a more precise systematic review [41]. Because of the novelty of the field and the presumed limited previous research on technologies that foster compassion, a systematic scoping review was deemed the appropriate method, as it focuses on appraising a body of literature on a specified topic in terms of extent, range, and nature [42].
Search Strategy
The search strategy was developed iteratively in consultation with an information specialist, as suggested by Horsley [43]. A systematic search was conducted between October and November 2020 using the PsycINFO, PubMed, Scopus, and Web of Science databases. The 4 databases were chosen because PsycINFO focuses on research on behavioral science and mental health, PubMed focuses on biomedicine (including psychiatry), and the other 2 databases include research from all disciplines. In this way, psychology, psychiatry, and technology research fell within the scope of our search. The query used a combination of terms related to compassion, technology, and mental health occurring in the title, abstract, or keywords of published articles (see Multimedia Appendix 1 for the search strings). The search terms used were chosen to focus specifically on the mental health field as well as on explicit mentions of either compassion or the related term empathy.
Eligibility Criteria
Because of the novelty of the subject, this review aims to identify articles covering any form of digital technology for the support of mental health that fosters the presence of compassion. Digital technologies linked to empathy instead of compassion were also eligible to avoid excluding articles that used the term “empathy” instead of compassion while pertaining to a similar construct. Our review did not focus on one specific type of participant in the included studies, so that articles including different types of people in and around the mental health field were eligible (eg, therapists, clients or patients, [informal] caregivers and also the public). All types of original research studies were eligible from any year of publication, country of origin, or original language (if a copy was available in English, German, Italian, or Dutch).
Exclusion criteria were as follows:
Articles without a clear focus on compassion or empathy, for example, merely mentioning compassion or empathy without further elaboration or using these factors solely as predictors or outcomes in a study.
Articles in which the link with compassion or empathy was only found as part of web-based versions of established compassion-based approaches (eg, Compassion-Focused Therapy [44]) or in the delivery of written psychoeducation (eg, a website with information on self-compassion), and compassion or empathy did not refer to (interactions with or through) the technology itself. These articles were excluded because a lot of research has already been conducted on these therapeutic approaches [45], and the role technology plays is relatively small, so that it is not directly relevant for our current purposes.
Articles related to compassion or empathy in a different field than mental health, for example, education or health care in general without a focus on mental health.
Study Selection
Covidence (a literature review screening software recommended by Cochrane [46]) was used to filter duplicate articles and facilitate study selection in 3 steps (Figure 1). First, the titles and abstracts of all retrieved articles were screened for eligibility by 2 authors (CvL and BL). Disagreements on the inclusion or exclusion of papers were discussed until an agreement was reached. Second, the full text of all remaining articles was checked for inclusion by one author (CvL) and doubts were discussed with a second author (BL). If an agreement could not be reached between the 2 authors, a third researcher was consulted (MLN). Third, to check whether seminal works were overlooked during the initial search process, forward and backward snowballing by one author (CvL) was used, based on the reference lists and citations of the included papers.
Figure 1.
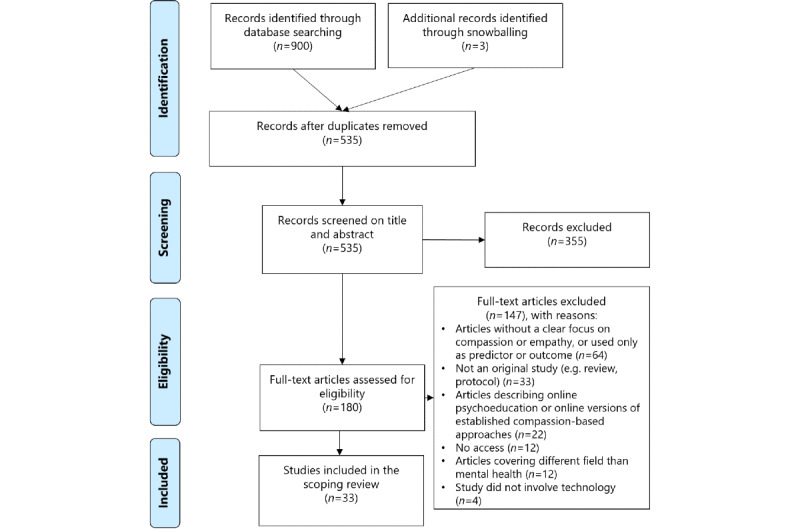
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the selection process for the systematic scoping review.
Data Extraction
Overview
Data that were extracted from each included article were author or authors, country of origin, year of publication, type of technology, target group or groups, goal or goals of the technology, the role of technology in the intervention, study design, outcome measures, elements of compassion, and compassionate role of technology. The role of technology in the intervention was coded depending on whether a technology was used by the target group on their own without guidance (“stand-alone”); only to deliver treatment sessions with a therapist or coach (“telecommunication”); with guidance from a coach or therapist, which was not face-to-face (“guided”); or was integrated into a treatment with face-to-face therapy sessions (“blended treatment”). Study designs were classified as qualitative, quantitative cross-sectional, quasi-experimental, experimental, or a combination (adapted from Centre for Evidence-Based Medicine [47]), with quasi-experimental studies referring to nonrandom allocation to groups and experimental studies referring to random allocation. For consistency, the term “outcome measures” was used for both quantitative and qualitative study designs, in the latter cases referring to the investigated variables. Elements of compassion were first described by closely following the author’s wording and then coded in the matching compassionate element (recognition, universality, empathy, tolerance, acting) by comparing them to their descriptions in Strauss et al [28]. Thus, the final results table includes the coded compassionate element and how this was described in the included study.
As we noticed that mentions of empathy or compassion in the included articles referred to different processes that technology could support, we divided articles into 3 “compassionate roles,” used to structure our results. These compassionate roles of technology have been categorized into different codes through inductive coding [48] using the method of constant comparison [49]. The roles were coded depending on whether the mentions of compassionate elements were mainly used to describe the features of the technology itself (Role A), to describe interventions for self-compassion (Role B), or to describe technology to facilitate compassionate elements between people (Role C). The characteristics of all included studies were extracted by 1 author (CvL), and data extraction of 15% of the included studies was validated by a second author (BL) with 82% agreement. This percentage of agreement was deemed sufficient to continue data extraction by one author. Data extraction occurred iteratively in consultation with several of the coauthors, where doubts were discussed until consensus was reached.
Main Perspective for Qualitative Analysis
In qualitative research, it is valuable to consider and describe the perspective held by researchers and how this could have influenced the research [50,51]. Therefore, we provide a short description of the background and perspective of the first author (CvL), focusing on elements that might have influenced the research process and vision presented in this paper.
CvL is a Dutch woman born in the Netherlands and raised in a nonreligious environment. Compassionate technology for mental health care is the topic of her PhD research project. The aim of this project was to investigate how technology in mental health care can be integrated into daily mental health care practice, where compassion is a fundamental value. This project took place in collaboration with researchers from different disciplines, a mental health care organization, and an eHealth company. CvL’s prior understanding of the topic comprises literature research on compassion, technology, and mental health care, as well as interviews with mental health care professionals, clients, and developers of DMHIs and observations of ways of working of mental health care professionals. Compassion is also an important personal value to her, in the sense of feeling responsibility for the world around you and wanting to contribute positively to society.
Results
Overview
On the basis of the inclusion and exclusion criteria, we included 33 studies (Tables 1-3), covering 31 unique DMHIs. These studies were published between 2008 and 2020, with the majority published between 2016 and 2020 (25/33, 76%) and conducted in Western countries (31/33, 94%). The technologies we found could be divided into 3 roles based on the main way the technology contributed to the presence of compassion (Figure 2). The technology could show elements of compassion to people (Role A, n=8), technology could enhance elements of self-compassion in people (Role B, n=12), and technology could facilitate elements of compassion between people (Role C, n=13).
Table 1.
Extracted data from the included studies classified as Role A: technology shows elements of compassion to people (n=8).
| Role and study | Technology (technology, target group, goal, and role in intervention) | Study (study design and outcome measures) | Compassionate elements (on the basis of the 5 elements proposed by Strauss et al [28]) | ||||
|
|
Hauser-Ulrich et al [52], 2020, Switzerland |
|
|
|
|||
|
|
Morris et al [53], 2018, United States |
|
|
|
|||
|
|
Javed and Park [54], 2019, United States |
|
|
|
|||
|
|
Pontier and Siddiqui [55], 2008, Netherlands |
|
|
|
|||
|
|
Kohori et al [56], 2018, Japan |
|
|
|
|||
|
|
Fitzpatrick et al [57], 2017, United States |
|
|
|
|||
|
|
Bickmore et al [58], 2010, United States |
|
|
|
|||
|
|
Rouaix et al [59], 2017, France |
|
|
|
|||
aRCT: randomized controlled trial.
bRecognizing suffering.
cFeeling empathy for the person suffering and connecting with the distress (emotional resonance).
dMotivation to act or acting to alleviate suffering.
eBDI: Beck Depression Inventory.
fCBT: cognitive behavioral therapy.
Table 3.
Extracted data from the included studies classified as Role C: technology supports elements of compassion between people (n=13).
| Role and study | Technology (technology, target group, goal, and role in intervention) | Study (study design and outcome measures) | Compassionate elements (on the basis of the 5 elements proposed by Strauss et al [28]) | ||||
|
|
Okita [72], 2013, United States |
|
|
|
|||
|
|
Choo et al [73], 2016, United States |
|
|
|
|||
|
|
Bar-Lev [74], 2008, Israel |
|
|
|
|||
|
|
Wijma et al [75], 2018, Netherlands |
|
|
|
|||
|
|
Han et al [76], 2011, United States |
|
|
|
|||
|
|
Högberg et al [77], 2018, Sweden |
|
|
|
|||
|
|
Steinwachs et al [78], 2011, United States |
|
|
|
|||
|
|
Kysely et al [79], 2020, Australia |
|
|
|
|||
|
|
Blair Irvine et al [80], 2012, United States |
|
|
|
|||
|
|
van Rijn et al [81], 2017, United Kingdom |
|
|
|
|||
|
|
Fordham and Ball [82], 2019, United States |
|
|
|
|||
|
|
Tippin and Maranzan [83], 2019, Canada |
|
|
|
|||
|
|
Milbury et al [84], 2020, United States |
|
|
|
|||
aRecognizing suffering.
bFeeling empathy for the person suffering and connecting with the distress (emotional resonance).
cMotivation to act or acting to alleviate suffering.
dUnderstanding the universality of suffering in the human experience.
eVR: virtual reality.
fTolerating uncomfortable feelings aroused in response to the suffering person (eg, distress, anger, fear) so remaining open to and accepting of the person suffering.
gRCT: randomized controlled trial.
Figure 2.
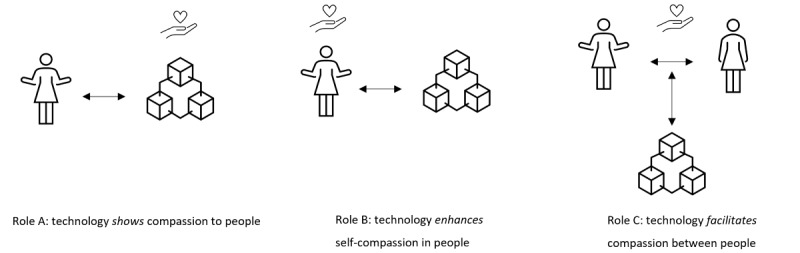
Schematic display of the 3 identified roles in which technology can contribute to compassion.
Table 2.
Extracted data from the included studies classified as Role B: technology enhances elements of self-compassion in people (n=12).
| Role and study | Technology (technology, target group, goal, and role in intervention) | Study (study design and outcome measures) | Compassionate elements (on the basis of the 5 elements proposed by Strauss et al [28]) | ||||
|
|
Ascone et al [60], 2020, Germany |
|
|
|
|||
|
|
Brown et al [61], 2020, United Kingdom |
|
|
|
|||
|
|
Pennesi and Wade [62], 2018, Australia |
|
|
|
|||
|
|
Falconer et al [63], 2016, United Kingdom |
|
|
|
|||
|
|
Falconer et al [64], 2014, United Kingdom |
|
|
|
|||
|
|
Donovan et al [65], 2016, United States |
|
|
|
|||
|
|
Rodgers et al [66], 2018, United States |
|
|
|
|||
|
|
Fonseca et al [67], 2019, Portugal |
|
|
|
|||
|
|
Schnepper et al [68], 2020, Austria |
|
|
|
|||
|
|
Raymond [69], 2019, United States |
|
|
|
|||
|
|
Lee et al [70], 2019, Netherlands |
|
|
|
|||
|
|
Köhle et al [71], 2017, Netherlands |
|
|
|
|||
aVR: virtual reality.
bUnderstanding the universality of suffering in the human experience.
cMotivation to act or acting to alleviate suffering.
dRCT: randomized controlled trial.
eFeeling empathy for the person suffering and connecting with the distress (emotional resonance).
fRecognizing suffering.
gTolerating uncomfortable feelings aroused in response to the suffering person (eg, distress, anger, fear) so remaining open to and accepting of the person suffering.
Technologies’ Types, Goals, Target Groups, and Roles in the Intervention
To answer the first research question, we will describe the different types, goals, target groups, and roles in technological interventions for each compassionate role. Table 4 shows a numeric summary of the results, including the frequencies and references of the variables that had a limited number of clear subtypes (technology types, roles in intervention, and compassionate elements). In Role A, we found 8 technologies showing elements of compassion for a person. An example is a chatbot that replies empathically to the person’s input and motivates them to complete certain activities, such as modules based on CBT [52]. For this role, the types of technology were mainly chatbots or conversational agents [52,53,57,58] and social robots [54,56,59]. The most identified goal was for technology to express empathic support and to foster the therapeutic alliance between the person and technology [52,53,55,58]. The target groups included different groups of people, such as people with dementia [59], schizophrenia [58], and ongoing or cyclic pain [52]. Some target groups were more general, such as “people who have difficulty living with pets” [56], or “people filling in the Beck’s Depression Inventory” [55]. For Role A, we found almost exclusively stand-alone interventions [52-58], meaning that they were used by the target group without any guidance from a coach or therapist. One exception was a social robot used in blended treatment [59], where the robot functioned as an assistant to the therapist in psychomotor therapy.
Table 4.
Numerical summary of the extracted variables that had a limited number of clear subtypes, including their frequencies and references, per compassionate role.
| Compassionate role, variable, and subtypes | Frequency, n (%) | References | ||||
| Role A (n=8) | ||||||
|
|
Technologies | |||||
|
|
|
Chatbot or conversational agent | 4 (50) | [52,53,57,58] | ||
|
|
|
Social robot | 3 (38) | [54,56,59] | ||
|
|
|
Web-based agent | 1 (12) | [55] | ||
|
|
Roles in interventions | |||||
|
|
|
Stand-alone | 7 (88) | [52-58] | ||
|
|
|
Blended treatment | 1 (12) | [59] | ||
|
|
Compassionate elements | |||||
|
|
|
Recognition | 4 (50) | [52,54,57,59] | ||
|
|
|
Universality | N/Aa | N/A | ||
|
|
|
Empathy | 8 (100) | [52-59] | ||
|
|
|
Tolerance | N/A | N/A | ||
|
|
|
Acting | 5 (63) | [52,54,57-59] | ||
| Role B (n=12) | ||||||
|
|
Technologies | |||||
|
|
|
Virtual reality | 4 (33) | [60,61,63,64] | ||
|
|
|
Mobile phone app or SMS text messaging | 4 (33) | [65,66,68,69] | ||
|
|
|
Web-based intervention | 3 (25) | [62,67,71] | ||
|
|
|
Chatbot | 1 (8) | [70] | ||
|
|
Roles in interventions | |||||
|
|
|
Stand-alone | 10 (83) | [60-64,66-68,70] | ||
|
|
|
Guided | 1 (8) | [71] | ||
|
|
|
Blended treatment | 1 (8) | [69] | ||
|
|
Compassionate elements | |||||
|
|
|
Recognition | 4 (33) | [65-67,71] | ||
|
|
|
Universality | 7 (58) | [60,65-68,70,71] | ||
|
|
|
Empathy | 2 (17) | [61,62] | ||
|
|
|
Tolerance | 3 (25) | [67,68,71] | ||
|
|
|
Acting | 9 (75) | [60,61,63-69] | ||
| Role C (n=13) | ||||||
|
|
Technologies | |||||
|
|
|
Web-based intervention | 5 (38) | [73,77,78,80,83] | ||
|
|
|
Online support group | 2 (15) | [74,76] | ||
|
|
|
Videoconferencing | 2 (15) | [79,84] | ||
|
|
|
Virtual reality | 2 (15) | [75,81] | ||
|
|
|
Social robot | 1 (8) | [72] | ||
|
|
|
Digital game | 1 (8) | [82] | ||
|
|
Roles in interventions | |||||
|
|
|
Stand-alone | 7 (54) | [72,74-76,78,82,83] | ||
|
|
|
Telecommunication | 4 (31) | [77,79,80,84] | ||
|
|
|
Guided | 1 (8) | [73] | ||
|
|
|
Blended treatment | 1 (8) | [81] | ||
|
|
Compassionate elements | |||||
|
|
|
Recognition | 5 (38) | [72,77,78,81,84] | ||
|
|
|
Universality | 3 (23) | [73,74,76] | ||
|
|
|
Empathy | 11 (85) | [72,73,75-77,79-84] | ||
|
|
|
Tolerance | 5 (38) | [75,77,80,83,84] | ||
|
|
|
Acting | 5 (38) | [76-78,80] | ||
aN/A: not applicable.
In Role B, we found 12 technologies that were used to enhance the elements of self-compassion in the person using them. An example is a VR intervention set in space to support the development of self-compassion [60]. The most frequently used technology types are VR [60,61,63,64], mobile phone apps, and SMS text messaging [65,66,68,69]. The goals mentioned most often for technologies with this role were to enhance self-compassion [60,62-64,66,68,70] and to decrease psychological symptoms [61,62,67,68]. Target groups were sometimes specific, for example, people with paranoia symptoms [60,61], and sometimes broader, for example, adolescents [65,66]. For Role B, most technologies served as a stand-alone intervention [60-68,70]. We found 1 study in which the intervention was guided in the form of written feedback from a personal web-based counselor [71]. Finally, in 1 study, the technology was part of a blended treatment [69]. Here, SMS text messaging was used to enhance a physical psychological intervention on self-compassion [69].
In Role C, we found 13 technologies that were used to facilitate elements of compassion between people, for instance, a therapeutic robot that acts as a social agent between pediatric patients and their parents in robot-assisted therapy [72]. The types of technologies were mainly web-based interventions [73,74,76-78], online support groups [74,76], videoconferencing [79,84], and VR [75,81]. Various goals were found, these included decreasing psychological symptoms [72,73,81,84] and enhancing empathy [75,80,82]. Target groups were often people with physical illnesses [72,74,76,77,84] but also included informal caregivers [75,84] and licensed care staff [80]. For Role C, again, most technologies formed a stand-alone intervention [72,74-76,78,82,83]. We also found several technologies that were used for telecommunication [77,79,80,84]. We found 1 study where the technological intervention was guided (albeit minimally), pertaining to the use of a “booster phone call” to review the process and challenges [73]. Finally, we also found 1 study in which technology was part of blended treatment: a VR intervention that was used in physical sessions with a counselor [81].
Study Designs and Outcome Measures
A range of different study designs and outcome measures was found in the included studies. Regarding outcome measures, none of the studies evaluated whether the technology as such was (perceived to be) compassionate. For the 8 articles categorized as Role A (technology showing compassion), we found the following study designs: experimental [52,57,59], quasi-experimental [55,58], qualitative [54], a combination of qualitative and experimental [53], and a combination of quantitative cross-sectional and qualitative [56]. Outcome measures included the acceptability of the intervention [52,56,57], evaluations of the technology [53,55,59], and symptoms and well-being [52,57,59]. One study investigated empathy in human-robot interaction by observing people with dementia interacting with a therapy robot during psychomotor therapy [59].
For the 12 articles categorized as Role B (enhancing self-compassion), the study designs were almost exclusively experimental [60-62,64,66-70], followed by qualitative [71] and quasi-experimental [63]. All but 1 study used specific outcome measures, most often symptoms and well-being [60-64,66-69] and self-compassion [60-63,66-68,70].
Finally, for the 13 articles categorized as Role C (facilitating compassion), the study designs were mostly qualitative [74,76,77,79,82] or experimental [72,78,80,83,84], followed by quasi-experimental [75], a combination of qualitative and quantitative cross-sectional [73], and a combination of qualitative and quasi-experimental [81]. Found outcome measures were mostly empathy between humans [72,75,76,78-80,83] and symptoms and well-being [72,76,81,84]. One study had compassion as an outcome measure, referring to nurses’ abilities to be compassionate through web-based communication [77].
Elements of Compassion
Overview
In general, empathy was used slightly more often as the main term to describe certain elements of technologies in the included studies (18/33, 55%) than compassion (15/33, 45%). Compassion was most often found in the form of increasing self-compassion (Role B). We did not find any technologies that embedded all the 5 elements of compassion. In the following sections, we will further specify how the 5 elements were embedded in the included DMHIs.
Recognition
The first element of compassion proposed by Strauss et al [28] is the recognition of suffering. This was observed in 13 of the included studies. In Role A (technology showing compassion), recognition referred to users being able to indicate their thoughts and feelings toward the technology. For example, people could indicate their mood to a fully automated conversational agent and receive a weekly mood description [57]. Similarly, in Role B (enhancing self-compassion), technology could allow users to track their feelings daily in a mood cloud, prompting personalized feedback or supportive emotional regulation statements to enhance self-compassion [66]. In Role C (facilitating compassion), technology could be used to help caregivers recognize suffering. An example is a robot seal that helped parents to acknowledge their children’s pain more accurately in robot-assisted therapy [72]. In another study, people with schizophrenia could use a web-based application to answer questions about their status and treatment, so the app could then act by giving recommendations on what they could discuss with their therapist and how [78]. Thus, unsuitable medications or other issues that could arise could be recognized faster.
Universality
This element refers to the understanding of the universality of suffering in human experiences [28]. It was only found in 10 of the included studies, of which none belonged to Role A, 7 studies were categorized as Role B, and 3 as Role C. In Role B, the technology could give shape to universality by giving user messages or exercises that emphasize common humanity, and that negative emotions are part of being human. For instance, in 1 study, women at risk for postpartum depressive symptoms received exercises in a web application to help them accept that they are susceptible and human, similar to all mothers [67]. Another study involved the chatbot Vincent, who “talked” about his mistakes, supporting common humanity [70]. In Role C, technology supported universality by providing a link to social support [73] so that people could exchange experiences and prevent isolation.
Empathy
This element refers to feeling empathy for those who are suffering and connecting with distress (emotional resonance [28]). Overall, the element “empathy” was the most frequently found (n=29). For Role A, empathy was found in all the studies (n=8). Most studies simply mentioned that the technology used an empathic tone in the messages it sent [52]; in some cases, it was tailored to the user’s input (current mood or text). In Role B, the element of empathy was found only twice. It refers to technology fostering the user’s empathy with the goal of targeting symptoms and well-being outcomes by letting them imagine an unpleasant experience they had from the perspective of an observer [62]. The other time it was found in a study where participants created a personal compassionate coach in VR that provided kindness and warmth, to help them be more self-compassionate [61]. In Role C, technology supports empathy among people in diverse ways and was found 11 times. Usually, technology facilitates empathy between a client and an informal or formal caregiver, for example, through a VR intervention that allows informal caregivers to experience dementia [75]. Technology can also facilitate empathy between a client and other people with similar experiences, for example, through an online support group [76]. Finally, technology could foster empathy in the general public for those with mental illnesses [83].
Tolerance
The element that was found least in the included studies was “tolerance” (n=8), referring to tolerating uncomfortable feelings aroused in response to the suffering person (such as distress, anger, or fear) and remaining open to and accepting of the person suffering [28]. Tolerance was not found in Role A. For Role B, tolerance was found 3 times. In all cases, it referred to supporting tolerance in humans and was described as helping people to be nonjudgmental and accepting toward themselves [68]. Finally, for Role C, tolerance was found the most frequently (n=5). In one instance, it was expressed in a VR intervention, giving informal caregivers of people with dementia more confidence in their care tasks and a more positive attitude toward them by increasing their resilience and proactive competence [75]. Similarly, a web-based training program for licensed care staff conveyed the philosophy that a resident’s potentially problematic behavior is an expression of an unmet need, instead of just behavior that needs to be managed [80]. In another study, tolerance was mentioned more indirectly, stating that a web-based communication service allowed a nurse to respond by expressing acceptance and validation [77].
Acting
Finally, the element “acting” refers to the motivation to act or actually acting to alleviate suffering [28]. This element was identified in 20 of the included studies. In Role A, acting was found 6 times. It was often found in very practical ways, stimulating the user to complete activities [52]. In some cases, the prompted content or activities were offered by the technology based on the user’s input, such as their mood state [57] or medication-taking behavior [58]. In one case, a social robot was used to provide positive feedback and motivate a person with dementia to engage in psychomotor therapy with their therapist [59]. For Role B, acting was found 9 times, where the technology acted to enhance the user’s self-compassion. For instance, VR was used to allow people to interact with a space nebula representing compassion, guiding them to open up compassionate feelings to increase self-compassion and decrease paranoia [60]. In another case with VR, people delivered compassionate sentences to a virtual child and then experienced these again from the perspective of the child [64]. To facilitate compassion in Role C, acting was found 5 times and could take different shapes. Technology could act as a social agent to stimulate empathic social interactions with other people [72]. Other times, the element of acting referred to human action facilitated by technology, such as the possibility of requesting support from a nurse [77].
Discussion
Principal Findings
This systematic scoping review investigated how and to what extent technology for mental health care has been connected to compassion in previous research. We could identify 3 roles that technology can play to support compassion in mental health care: showing compassion to the client, enhancing self-compassion in people, and facilitating compassion between people, such as between a client and a caretaker or therapist. The main types of technologies and their goals, as well as the main study designs and outcome measures, differed by role, whereas the main target groups varied widely across all roles. We found a large majority of technologies that were described as stand-alone interventions, to be used by the target group without guidance from a coach or therapist. Only a few included studies described technologies as part of blended treatment: integrated in face-to-face sessions with a coach or therapist. This is in line with earlier research showing a lack of clarity on how to embed technologies in blended treatment [19]. Furthermore, none of the technologies included all elements of a proposed definition of compassion [28], nor was any technology evaluated on whether it was experienced as compassionate. However, we recognized certain elements of compassion in the technologies, showing that all elements could potentially be embedded in technology.
Of the 5 proposed elements of compassion, we found descriptions matching the elements “empathy” and “acting” most often in the included studies, followed by “recognition.” In the scoping review care by Kemp et al [37], DMHIs were examined using a model of digital intersections with compassionate care. The authors found DMHIs that could support 4 of the 6 categories in this model. However, for 2 categories, no DMHIs were found in their review. These were “awareness of suffering” (the use of a DMHI to become more aware of one’s suffering) and “mediated response” (the use of a DMHI to mediate the response to suffering) [37]. “Awareness of suffering” seems to be related to “recognition of suffering” in our current review, whereas “mediated response” could have overlap with “acting to alleviate suffering.” We found several examples of how DMHIs could support both compassion components.
The elements of “universality” and “tolerance” were rarely found “Universality” was mostly found in the studies in Role B, describing DMHIs with the aim to enhance self-compassion. These studies often followed the definition of self-compassion by Neff [29], which overlaps with the definition of compassion proposed by Strauss et al [28]. Furthermore, as mentioned before, none of the included studies described technologies that fostered all elements of compassion. As Sinclair et al [38] discussed in their review on compassion in health care, the separate elements of compassion are not inherently compassionate; rather, their combination constitutes compassion. Following this logic, combined with the lack of evaluation of technology on (perceived) compassion, we cannot be sure if truly compassionate technology exists within our scope.
The Added Value of Compassion
Empathy was the element of compassion that we identified most frequently and that was used more often as a main term to describe technologies than compassion itself. As discussed in the Introduction section, there are some important differences between the constructs [28,33]. In short, compassion is specifically a response to suffering, whereas empathy can be felt for any emotion. Further, compassion includes the motivation to act to alleviate suffering, whereas empathy can also be followed by behavior in general but does not necessarily include this. These differences, as well as the additional elements of understanding the universality of human suffering and distress tolerance, make compassion especially valuable in the field of mental health or mental health care [37]. Therefore, we believe that explicitly embedding elements of compassion in the design and use of technology for mental health care, not just empathy, is a promising approach that is currently lacking.
In the current review, the lesser-known elements of compassion that are just as important in mental health care, such as understanding the universality of suffering in human experience and tolerating uncomfortable feelings, were rarely found. This indicates that a too narrow (or no) definition of compassion is used, at least when referring to features of technology. The overarching construct of compassion in “traditional” mental health care is a fundamental value and has multiple beneficial effects [28,37]. Moreover, considering the intentions, motivations, and values of stakeholders in mental health care or health care is argued to be essential in successfully blending technology into this field [12,37,85]. Thus, considering the elements of compassion in the design and use of future digital interventions could be a promising approach to improving the acceptance of DMHIs in the mental health context.
The Potential of Compassionate Technology
Our findings show that compassion offers a versatile and potentially transdiagnostic lens with which to examine technology for mental health care. First, as discussed in the Introduction, mental health professionals expressed the need for a clear conceptual basis for embedding technologies into mental health care [19]. Compassion could be a suitable basis and guiding force for the integration of technologies in mental health care: blending in technology in such a way that the therapeutic process as a whole is optimally in line with all elements of compassion. Thus, recognizing and alleviating suffering (ie, compassion) would be the central goal of both the design and evaluation of DMHIs as well as protocols for working with technology. Conventional values such as efficiency or effectiveness would be considered as means to achieve this goal. The design methodology of “Values that Matter” would lend itself very well to the design of DMHIs around compassion, as it aims to embed ethical values in technology [86].
Second, not only can compassion offer the basis for the design of DMHIs and protocols for the integration of compassionate technology in treatment, but the other way around technology can also bring new and additional ways to foster compassion that are not possible in traditional treatment (see Figure 3 for a conceptual overview). Examples include being present anywhere and anytime without getting tired or frustrated or being easier and more accessible to share suffering. On a microlevel, every interaction with a DMHI could convey all elements of compassion, and the elements of compassion could also be conveyed in the treatment as a whole by the therapist and technology together or at different times during the therapeutic process. Here, we illustrate what the latter could look like with an extended treatment scenario based on the 5 proposed elements of compassion [28] and the elements of compassion found in the different technologies included in our review. We also referred to relevant related initiatives that did not fully meet our inclusion criteria and were therefore excluded but still provided interesting additional possibilities.
Figure 3.
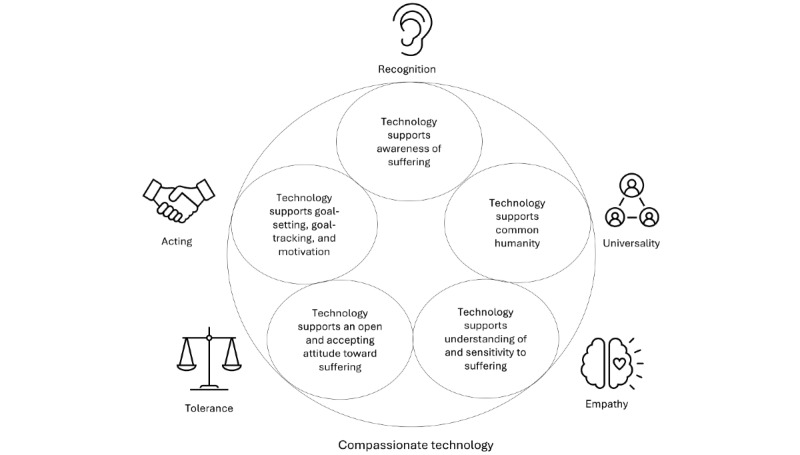
Conceptual overview of compassionate technology, which supports all elements of compassion.
First, the DMHI could help the client and therapist to (1) recognize moments of suffering anytime and anywhere. This could be based on input from the client (eg, indicating their mood and feelings [57]) but could also be combined with physiological measurements from a wearable (an example can be found in Fletcher et al [87]). The DMHI could convey the (2) universality of suffering in the human experience, for example, by connecting the client to similar experiences of others [73]. Furthermore, the DMHI could support the presence of (3) empathy for clients’ suffering by sending empathic messages based on the user’s input [52] or by helping the therapist to offer emotional support specifically during moments of potential distress [77].
Furthermore, the tone in communication with the DMHI and the therapist would remain open, accepting, and (4) tolerant of distress by acknowledging and validating difficult feelings (eg, [67,88]), where the DMHI has the advantage that it is not susceptible to empathic distress and can always be there for the client when it is needed. DMHIs could also be used to help increase the resilience and distress tolerance of mental health professionals [80]. Finally, together with the therapist, the client could look back on the recorded and experienced difficult moments and successes and set therapeutic goals. The DMHI could help to keep track of and work on these goals [57], until the next appointment with the therapist, for instance, by activating tailored exercises at the right moment and giving reminders or rewards to support (5) acting to alleviate suffering. Of course, this example raises new questions that need to be explored, such as how the tasks of the therapist and technology can be optimally blended to offer all the elements of recognizing and relieving suffering in an iterative manner.
Critical Notes on Digital Environments in Relation to Compassion and Empathy
This review has shown the possibilities for DMHIs to contribute to compassion in the field of mental health in several ways. However, it is important to acknowledge that concerns also exist regarding the use of technology in (mental) health care. First, there is concern about technology detracting from empathy and compassion. This could happen because of a lack of emotional signals and cues, and the possibility of hiding behind anonymity, and easily escaping the reactions of others [37,89]. In our review, we saw this in an article describing ambiguous experiences with videoconferencing, which could be considered impersonal [79]. These concerns point to the importance of placing more emphasis on empathy and compassion if DMHIs are used, such as by preparing (mental) health professionals to use DMHIs in a compassionate way for both themselves and their clients [89]. One possible way to enhance empathy among health professionals could be VR interventions [90,91]. In addition, there is debate about whether DMHIs actually contribute to equal access to care or whether they enlarge the existing inequities in society. For example, groups that have limited access to digital health care and limited digital literacy skills could be left behind [92]. These concerns should be considered in the development, evaluation, and use of DMHIs in mental health care. For instance, future evaluation of DMHIs should critically assess for the presence and quality of different compassion elements.
Limitations
This review is a systematic scoping review into an unexplored and diverse field. As we searched for mentions of compassion or empathy to delimit our research area, there could be technologies for mental health care that we did not include here but do show elements of compassion. There are several related initiatives in technology development, such as calm technology and affective computing, which focus on unobtrusive and emotion-sensitive technologies, respectively [93,94]. However, because this scoping review aims to provide an overview of technology explicitly related to compassion or empathy, these related initiatives did not fall within our scope.
Furthermore, it is important to keep in mind that our conceptualization of compassion, and especially the acceptability and value of suffering within Western psychological theories and therapies, may have cross-cultural limitations [95,96]. As the majority of studies included in the current review were conducted in Western countries, our findings may represent a mostly Western view of compassion and suffering. For instance, non-Western cultures generally do not see suffering as a purely negative life experience but instead believe that by appreciating it for what it offers, it can actually contribute to living a good life [95].
In addition, because the term “compassionate technology” was not found in previous studies, we used the definition of compassion proposed by Strauss et al [28] to assess the extent to which the technology in the included studies matched elements of compassion. In doing so, we closely followed the phrasing of the study authors. However, authors often did not explain (in detail) what they understood as “empathic” or “compassionate.” Therefore, we may have misinterpreted the meaning of the authors. To make future studies on compassionate technology more transparent and comparable, we recommend that the authors include their definitions of compassion or its elements.
Because the present review was a scoping review, we did not assess the methodological quality of the included articles but instead focused on creating an overview of the scope of this field. Moreover, although some studies have measured compassion or self-compassion as an outcome, no studies have measured how compassionate the technology was, for example, as experienced by its users. We do not know whether the compassionate elements actually contributed to the presence of compassion, and if so, how and which elements did. Thus, we cannot be sure that the technologies we included measurably showed, enhanced, or facilitated compassion in the mental health care process.
Future Research
On the basis of the increasing frequency we saw over the publication years of the included articles linking compassion and empathy to DMHIs, the attention for such values in this field seems to be growing. This makes it a promising area for further research, but also one where much remains to be discovered. Most importantly, compassion is not yet seen as a foundation and goal for embedding technology into mental health care, and research is needed to learn more about how to design technologies and blended ways of working around compassion, focusing on the optimal recognition and alleviation of suffering. Furthermore, no scale exists to evaluate DMHIs on compassion. To advance the field of compassionate technology, it is essential to be able to determine which types of technologies with which design features actually support the presence of compassion across the 3 roles and for whom. Thus, a scale needs to be developed to measure compassion as shown, enhanced or facilitated by technology for both clients and professionals in mental health care.
Finally, as a scoping review, this review focused on the scope and degree to which we could find compassion linked to DMHIs but did not consider the effects of technology with compassionate elements on, for example, adherence [97], engagement [98], or effectiveness. Future research is needed to study which validated measures have been used in this field, so that the effects on the aforementioned constructs could be researched. Although the types of research and outcome measures we found varied widely, research on technology enhancing self-compassion in people consisted mainly of experimental studies measuring participants’ psychological symptoms or self-compassion or both. Therefore, research in this role would lend itself well to a meta-analysis of the effectiveness of these technologies. Moreover, we used search terms related to mental health but found many studies related to mental well-being, with some components of mental health. Thus, it could be interesting for future research to expand the scope to explicitly include DMHIs around mental well-being or lifestyle, because there might be additional relevant work in these fields as well.
Conclusions
Compassion is an essential value in mental health care, pertaining to recognizing suffering, being moved by it, and acting to alleviate it. Given the importance and benefits of compassion in mental health care, shifting the focus of the design, evaluation, and use of DMHIs to center on compassion seems to be a new, fascinating, and perhaps even necessary direction in research and clinical practice. This scoping review explored how and to what degree elements of compassion have been linked to technologies for mental health care in previous studies. Our review shows that compassion is a widely applicable construct across different technologies, target groups, and for different aims in mental health care and is potentially a guiding force in embedding technology in mental health care. Moreover, it provides new input for the design and development of technology around compassion and demonstrates the necessity of evaluating technology on this foundational value in mental health care. Overall, this review serves as a first step toward “compassionate technology” as a guiding principle in the use and design of technology for mental health care. This principle refers to technology that contributes to the recognition and alleviation of suffering and is appropriately suited to the mental health care context for both clients and professionals.
Acknowledgments
This publication is part of the project “designing compassionate technology with high societal readiness levels for mental health care” (project number 403.19.229) of the research program Transitions and Behavior, financed by the Dutch Research Council (NWO), Minddistrict BV, and Dimence Groep. Funding sources were not involved in the writing of this manuscript or in the decision to submit it for publication.
Abbreviations
- CBT
cognitive behavioral therapy
- DMHI
digital mental health intervention
- VR
virtual reality
Search strategies for each of the included databases.
Footnotes
Authors' Contributions: CvL, GJW, GDSL, SMK, and MLN conceptualized the study and wrote the original draft of the manuscript. CvL and BL screened the literature. CvL extracted data from the included articles and BL validated the data extraction. CvL, BL, and MLN contributed to data interpretation. All authors edited multiple drafts and reviewed the final manuscript.
Conflicts of Interest: None declared.
References
- 1.Tal A, Torous J. The digital mental health revolution: opportunities and risks. Psychiatr Rehabil J. 2017 Sep;40(3):263–5. doi: 10.1037/prj0000285.2017-39812-001 [DOI] [PubMed] [Google Scholar]
- 2.Fairburn CG, Patel V. The impact of digital technology on psychological treatments and their dissemination. Behav Res Ther. 2017 Jan;88:19–25. doi: 10.1016/j.brat.2016.08.012. https://linkinghub.elsevier.com/retrieve/pii/S0005-7967(16)30137-1 .S0005-7967(16)30137-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aboujaoude E, Gega L, Parish MB, Hilty DM. Editorial: digital interventions in mental health: current status and future directions. Front Psychiatry. 2020 Feb 27;11:111. doi: 10.3389/fpsyt.2020.00111. https://europepmc.org/abstract/MED/32174858 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marzano L, Bardill A, Fields B, Herd K, Veale D, Grey N, Moran P. The application of mHealth to mental health: opportunities and challenges. Lancet Psychiatry. 2015 Oct;2(10):942–8. doi: 10.1016/S2215-0366(15)00268-0.S2215-0366(15)00268-0 [DOI] [PubMed] [Google Scholar]
- 5.Rabbitt SM, Kazdin AE, Hong JH. Acceptability of robot-assisted therapy for disruptive behavior problems in children. Arch Sci Psychol. 2015 Aug 03;3(1):101–10. doi: 10.1037/arc0000017. https://psycnet.apa.org/fulltext/2015-34826-001.html . [DOI] [Google Scholar]
- 6.Fleming TM, Bavin L, Stasiak K, Hermansson-Webb E, Merry SN, Cheek C, Lucassen M, Lau HM, Pollmuller B, Hetrick S. Serious games and gamification for mental health: current status and promising directions. Front Psychiatry. 2017 Jan 10;7:215. doi: 10.3389/fpsyt.2016.00215. doi: 10.3389/fpsyt.2016.00215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mandryk RL, Birk MV. Toward game-based digital mental health interventions: player habits and preferences. J Med Internet Res. 2017 Apr 20;19(4):e128. doi: 10.2196/jmir.6906. https://www.jmir.org/2017/4/e128/ v19i4e128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bergmo TS. How to measure costs and benefits of eHealth interventions: an overview of methods and frameworks. J Med Internet Res. 2015 Nov 09;17(11):e254. doi: 10.2196/jmir.4521. https://www.jmir.org/2015/11/e254/ v17i11e254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doherty G, Coyle D, Matthews M. Design and evaluation guidelines for mental health technologies. Interact Comput. 2010 Jul;22(4):243–52. doi: 10.1016/j.intcom.2010.02.006. [DOI] [Google Scholar]
- 10.Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatr Serv. 2014 Jan 01;65(1):24–32. doi: 10.1176/appi.ps.201300009.1745988 [DOI] [PubMed] [Google Scholar]
- 11.Wentzel J, van der Vaart R, Bohlmeijer ET, van Gemert-Pijnen JE. Mixing online and face-to-face therapy: how to benefit from blended care in mental health care. JMIR Ment Health. 2016 Feb 09;3(1):e9. doi: 10.2196/mental.4534. https://mental.jmir.org/2016/1/e9/ v3i1e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Vaart R, Witting M, Riper H, Kooistra L, Bohlmeijer ET, van Gemert-Pijnen LJ. Blending online therapy into regular face-to-face therapy for depression: content, ratio and preconditions according to patients and therapists using a Delphi study. BMC Psychiatry. 2014 Dec 14;14:355. doi: 10.1186/s12888-014-0355-z. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0355-z .s12888-014-0355-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andersson G. Internet-delivered psychological treatments. Annu Rev Clin Psychol. 2016;12:157–79. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- 14.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jun;32(4):329–42. doi: 10.1016/j.cpr.2012.02.004.S0272-7358(12)00027-X [DOI] [PubMed] [Google Scholar]
- 15.Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn Behav Ther. 2018 Jan;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- 16.Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014 Oct;13(3):288–95. doi: 10.1002/wps.20151. https://europepmc.org/abstract/MED/25273302 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andersson G, Topooco N, Havik O, Nordgreen T. Internet-supported versus face-to-face cognitive behavior therapy for depression. Expert Rev Neurother. 2016;16(1):55–60. doi: 10.1586/14737175.2015.1125783. [DOI] [PubMed] [Google Scholar]
- 18.Feijt MA, de Kort YA, Bongers IM, IJsselsteijn WA. Perceived drivers and barriers to the adoption of eMental health by psychologists: the construction of the levels of adoption of eMental health model. J Med Internet Res. 2018 Apr 24;20(4):e153. doi: 10.2196/jmir.9485. https://www.jmir.org/2018/4/e153/ v20i4e153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Titzler I, Saruhanjan K, Berking M, Riper H, Ebert DD. Barriers and facilitators for the implementation of blended psychotherapy for depression: a qualitative pilot study of therapists' perspective. Internet Interv. 2018 Jun;12:150–64. doi: 10.1016/j.invent.2018.01.002. https://linkinghub.elsevier.com/retrieve/pii/S2214-7829(17)30090-8 .S2214-7829(17)30090-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011 Aug 05;13(3):e52. doi: 10.2196/jmir.1772. https://www.jmir.org/2011/3/e52/ v13i3e52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sharry J, Davidson R, McLoughlin O, Doherty G. A service-based evaluation of a therapist-supported online cognitive behavioral therapy program for depression. J Med Internet Res. 2013 Jun 27;15(6):e121. doi: 10.2196/jmir.2248. https://www.jmir.org/2013/6/e121/ v15i6e121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scholten H, Granic I. Use of the principles of design thinking to address limitations of digital mental health interventions for youth: viewpoint. J Med Internet Res. 2019 Jan 14;21(1):e11528. doi: 10.2196/11528. https://www.jmir.org/2019/1/e11528/ v21i1e11528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simpson JA, Weiner ES. Oxford English Dictionary. 2nd edition. Oxford, UK: Clarendon Press; 1989. [Google Scholar]
- 24.Shea S, Lionis C. The call for compassion in health care. In: Seppälä EM, Simon-Thomas E, Brown SL, Worline MC, Cameron CD, Doty JD, editors. The Oxford Handbook of Compassion Science. Oxford, UK: Oxford University Press; 2017. Sep 28, pp. 457–74. [Google Scholar]
- 25.Gilbert P. Compassion and cruelty: a biopsychosocial approach. In: Gilbert P, editor. Compassion: Conceptualisations, Research and Use in Psychotherapy. London, UK: Routledge; 2005. pp. 9–74. [Google Scholar]
- 26.Gilbert P. Introducing compassion-focused therapy. Adv Psychiatr Treat. 2009;15(3):199–208. doi: 10.1192/apt.bp.107.005264. https://www.cambridge.org/core/journals/advances-in-psychiatric-treatment/article/introducing-compassionfocused-therapy/ECBC8B7B87E90ABB58C4530CDEE04088 . [DOI] [Google Scholar]
- 27.Feldman C, Kuyken W. Compassion in the landscape of suffering. Contemp Buddhism. 2011 Jun 14;12(1):143–55. doi: 10.1080/14639947.2011.564831. https://www.tandfonline.com/doi/abs/10.1080/14639947.2011.564831 . [DOI] [Google Scholar]
- 28.Strauss C, Lever Taylor B, Gu J, Kuyken W, Baer R, Jones F, Cavanagh K. What is compassion and how can we measure it? A review of definitions and measures. Clin Psychol Rev. 2016 Jul;47:15–27. doi: 10.1016/j.cpr.2016.05.004. https://linkinghub.elsevier.com/retrieve/pii/S0272-7358(16)30021-6 .S0272-7358(16)30021-6 [DOI] [PubMed] [Google Scholar]
- 29.Neff KD. The science of self-compassion. In: Germer C, Siegel R, editors. Compassion and Wisdom in Psychotherapy. New York, NY, USA: Guilford Press; 2012. pp. 79–92. [Google Scholar]
- 30.Elices M, Carmona C, Pascual JC, Feliu-Soler A, Martin-Blanco A, Soler J. Compassion and self-compassion: construct and measurement. Mindfulness Compassion. 2017 Jan;2(1):34–40. doi: 10.1016/j.mincom.2016.11.003. https://self-compassion.org/wp-content/uploads/2018/05/Elices2017.pdf . [DOI] [Google Scholar]
- 31.Lazarus RS. Emotion and Adaptation. Oxford, UK: Oxford University Press; 1991. [Google Scholar]
- 32.Davis MH. Measuring individual differences in empathy: evidence for a multidimensional approach. J Pers Soc Psychol. 1983;44(1):113–26. doi: 10.1037/0022-3514.44.1.113. https://psycnet.apa.org/record/1983-22418-001 . [DOI] [Google Scholar]
- 33.Cuff BM, Brown SJ, Taylor L, Howat DJ. Empathy: a review of the concept. Emot Rev. 2016 Apr;8(2):144–53. doi: 10.1177/1754073914558466. https://journals.sagepub.com/doi/10.1177/1754073914558466 . [DOI] [Google Scholar]
- 34.Batson CD. Altruism in Humans. New York, NY, USA: Oxford University Press; 2011. Jul, [Google Scholar]
- 35.Eisenberg N, Eggum ND. Empathic responding: sympathy and personal distress. In: Decety J, Ickes W, editors. The Social Neuroscience of Empathy. Cambridge, MA, USA: MIT Press; 2009. Mar, pp. 71–83. [Google Scholar]
- 36.Goetz JL, Simon-Thomas E. The landscape of compassion: definitions and scientific approaches. In: Seppälä EM, Brown SL, Worline MC, Cameron CD, Doty JR, editors. The Oxford Handbook of Compassion Science. Oxford, UK: Oxford University Press; 2017. pp. 3–15. [Google Scholar]
- 37.Kemp J, Zhang T, Inglis F, Wiljer D, Sockalingam S, Crawford A, Lo B, Charow R, Munnery M, Singh Takhar S, Strudwick G. Delivery of compassionate mental health care in a digital technology-driven age: scoping review. J Med Internet Res. 2020 Mar 06;22(3):e16263. doi: 10.2196/16263. https://www.jmir.org/2020/3/e16263/ v22i3e16263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinclair S, Norris JM, McConnell SJ, Chochinov HM, Hack TF, Hagen NA, McClement S, Bouchal SR. Compassion: a scoping review of the healthcare literature. BMC Palliat Care. 2016 Jan 19;15:6. doi: 10.1186/s12904-016-0080-0. https://bmcpalliatcare.biomedcentral.com/articles/10.1186/s12904-016-0080-0 .10.1186/s12904-016-0080-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Day J, Finkelstein JC, Field BA, Matthews B, Kirby JN, Doty JR. Compassion-focused technologies: reflections and future directions. Front Psychol. 2021 May 13;12:603618. doi: 10.3389/fpsyg.2021.603618. https://europepmc.org/abstract/MED/34054636 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wiljer D, Strudwick G, Crawford A. Caring in a digital age: exploring the interface of humans and machines in the provision of compassionate healthcare. In: Hodges BD, Paech G, Bennett J, editors. Without Compassion, There Is No Healthcare: Leading with Care in a Technological Age. Montreal, Quebec: McGill-Queen's University Press; 2020. Nov, pp. 33–41. [Google Scholar]
- 41.Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015 Sep;13(3):141–6. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 42.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005 Feb;8(1):19–32. doi: 10.1080/1364557032000119616. https://www.tandfonline.com/doi/abs/10.1080/1364557032000119616 . [DOI] [Google Scholar]
- 43.Horsley T. Tips for improving the writing and reporting quality of systematic, scoping, and narrative reviews. J Contin Educ Health Prof. 2019;39(1):54–7. doi: 10.1097/CEH.0000000000000241. [DOI] [PubMed] [Google Scholar]
- 44.Gilbert P. Compassion Focused Therapy: Distinctive Features. Oxfordshire, UK: Routledge; 2010. [Google Scholar]
- 45.Leaviss J, Uttley L. Psychotherapeutic benefits of compassion-focused therapy: an early systematic review. Psychol Med. 2015 Apr;45(5):927–45. doi: 10.1017/S0033291714002141. https://europepmc.org/abstract/MED/25215860 .S0033291714002141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Covidence systematic review software. Covidence. 2020. [2020-09-15]. https://get.covidence.org/literature-review? campaignid=18238395256&adgroupid=138114520982&gclid=EAIaIQobChMI6_7lgZ30_QIVe5lmAh0qpg22EAAYAiAAEgKUcvD_BwE .
- 47.Centre for Evidence-Based Medicine. Oxford, UK: University of Oxford; [2021-09-15]. Study designs. https://www.cebm.ox.ac.uk/resources/ebm-tools/study-designs . [Google Scholar]
- 48.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006 Jun 01;27(2):237–46. doi: 10.1177/1098214005283748. https://journals.sagepub.com/doi/10.1177/1098214005283748 . [DOI] [Google Scholar]
- 49.Coghlan A, Filo K. Using constant comparison method and qualitative data to understand participants’ experiences at the nexus of tourism, sport and charity events. Tour Manag. 2013 Apr;35:122–31. doi: 10.1016/j.tourman.2012.06.007. https://www.cabdirect.org/cabdirect/abstract/20133017817 . [DOI] [Google Scholar]
- 50.Levitt HM, Bamberg M, Creswell JW, Frost DM, Josselson R, Suárez-Orozco C. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: the APA publications and communications board task force report. Am Psychol. 2018 Jan;73(1):26–46. doi: 10.1037/amp0000151. https://core.ac.uk/reader/151186911?utm_source=linkout .2018-00750-003 [DOI] [PubMed] [Google Scholar]
- 51.Morrow SL. Quality and trustworthiness in qualitative research in counseling psychology. J Couns Psychol. 2005;52(2):250–60. doi: 10.1037/0022-0167.52.2.250. https://psycnet.apa.org/record/2005-03263-015 . [DOI] [Google Scholar]
- 52.Hauser-Ulrich S, Künzli H, Meier-Peterhans D, Kowatsch T. A smartphone-based health care chatbot to promote self-management of chronic pain (SELMA): pilot randomized controlled trial. JMIR Mhealth Uhealth. 2020 Apr 03;8(4):e15806. doi: 10.2196/15806. https://mhealth.jmir.org/2020/4/e15806/ v8i4e15806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Morris RR, Kouddous K, Kshirsagar R, Schueller SM. Towards an artificially empathic conversational agent for mental health applications: system design and user perceptions. J Med Internet Res. 2018 Jun 26;20(6):e10148. doi: 10.2196/10148. https://www.jmir.org/2018/6/e10148/ v20i6e10148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Javed H, Park CH. Interactions with an empathetic agent: regulating emotions and improving engagement in autism. IEEE Robot Autom Mag. 2019 Jun;26(2):40–8. doi: 10.1109/mra.2019.2904638. https://europepmc.org/abstract/MED/34887653 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pontier M, Siddiqui GF. A virtual therapist that responds empathically to your answers. Proceedings of the 8th International Conference on Intelligent Virtual Agents; IVA '08; September 1-3, 2008; Tokyo, Japan. 2008. Sep, pp. 417–25. [DOI] [Google Scholar]
- 56.Kohori T, Hirayama S, Hara T, Muramatsu M, Naganuma H, Yamano M, Ichikawa K, Matsumoto H, Uchiyama H. Development and evaluation of an interactive therapy robot. Proceedings of the 14th International Conference on Advances in Computer Entertainment Technology; ACE' 17; December 14-16, 2017; London, UK. 2017. pp. 66–83. [DOI] [Google Scholar]
- 57.Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health. 2017 Jun 06;4(2):e19. doi: 10.2196/mental.7785. https://mental.jmir.org/2017/2/e19/ v4i2e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bickmore TW, Puskar K, Schlenk EA, Pfeifer LM, Sereika SM. Maintaining reality: relational agents for antipsychotic medication adherence. Interact Comput. 2010 Jul;22(4):276–88. doi: 10.1016/j.intcom.2010.02.001. https://academic.oup.com/iwc/article-abstract/22/4/276/932479?redirectedFrom=fulltext&login=false . [DOI] [Google Scholar]
- 59.Rouaix N, Retru-Chavastel L, Rigaud AS, Monnet C, Lenoir H, Pino M. Affective and engagement issues in the conception and assessment of a robot-assisted psychomotor therapy for persons with dementia. Front Psychol. 2017 Jun 30;8:950. doi: 10.3389/fpsyg.2017.00950. https://europepmc.org/abstract/MED/28713296 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ascone L, Ney K, Mostajeran F, Steinicke F, Moritz S, Gallinat J, Kühn S. Virtual reality for individuals with occasional paranoid thoughts. Proceedings of the Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems; CHI EA '20; April 25-30, 2020; Honolulu, HI, USA. 2020. Apr, pp. 1–8. [DOI] [Google Scholar]
- 61.Brown P, Waite F, Rovira A, Nickless A, Freeman D. Virtual reality clinical-experimental tests of compassion treatment techniques to reduce paranoia. Sci Rep. 2020 May 22;10(1):8547. doi: 10.1038/s41598-020-64957-7. doi: 10.1038/s41598-020-64957-7.10.1038/s41598-020-64957-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pennesi JL, Wade TD. Imagery rescripting and cognitive dissonance: a randomized controlled trial of two brief online interventions for women at risk of developing an eating disorder. Int J Eat Disord. 2018 May;51(5):439–48. doi: 10.1002/eat.22849. [DOI] [PubMed] [Google Scholar]
- 63.Falconer CJ, Rovira A, King JA, Gilbert P, Antley A, Fearon P, Ralph N, Slater M, Brewin CR. Embodying self-compassion within virtual reality and its effects on patients with depression. BJPsych Open. 2016 Jan;2(1):74–80. doi: 10.1192/bjpo.bp.115.002147. https://europepmc.org/abstract/MED/27703757 .S2056472400001186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Falconer CJ, Slater M, Rovira A, King JA, Gilbert P, Antley A, Brewin CR. Embodying compassion: a virtual reality paradigm for overcoming excessive self-criticism. PLoS One. 2014 Nov 12;9(11):e111933. doi: 10.1371/journal.pone.0111933. https://dx.plos.org/10.1371/journal.pone.0111933 .PONE-D-14-31083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Donovan E, Rodgers RF, Cousineau TM, McGowan KM, Luk S, Yates K, Franko DL. Brief report: feasibility of a mindfulness and self-compassion based mobile intervention for adolescents. J Adolesc. 2016 Dec;53:217–21. doi: 10.1016/j.adolescence.2016.09.009.S0140-1971(16)30132-4 [DOI] [PubMed] [Google Scholar]
- 66.Rodgers RF, Donovan E, Cousineau T, Yates K, McGowan K, Cook E, Lowy AS, Franko DL. BodiMojo: efficacy of a mobile-based intervention in improving body image and self-compassion among adolescents. J Youth Adolesc. 2018 Jul;47(7):1363–72. doi: 10.1007/s10964-017-0804-3.10.1007/s10964-017-0804-3 [DOI] [PubMed] [Google Scholar]
- 67.Fonseca A, Monteiro F, Alves S, Gorayeb R, Canavarro MC. Be a mom, a web-based intervention to prevent postpartum depression: the enhancement of self-regulatory skills and its association with postpartum depressive symptoms. Front Psychol. 2019 Feb 18;10:265. doi: 10.3389/fpsyg.2019.00265. https://europepmc.org/abstract/MED/30873060 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schnepper R, Reichenberger J, Blechert J. Being my own companion in times of social isolation - a 14-day mobile self-compassion intervention improves stress levels and eating behavior. Front Psychol. 2020 Oct 09;11:595806. doi: 10.3389/fpsyg.2020.595806. https://europepmc.org/abstract/MED/33162922 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Raymond RR. Experience sampling assessment of a brief text-message enhanced self-compassion intervention. The Catholic University of America. 2019. [2020-11-30]. https://cuislandora.wrlc.org/islandora/object/cuislandora%3A213710 .
- 70.Lee M, Ackermans S, Van As N, Chang H, Lucas E, IJsselsteijn WA. Caring for vincent: a chatbot for self-compassion. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems; CHI '19; May 4-9, 2019; Glasgow, UK. 2019. May, p. 702. [DOI] [Google Scholar]
- 71.Köhle N, Drossaert CH, Jaran J, Schreurs KM, Verdonck-de Leeuw IM, Bohlmeijer ET. User-experiences with a web-based self-help intervention for partners of cancer patients based on acceptance and commitment therapy and self-compassion: a qualitative study. BMC Public Health. 2017 Feb 28;17(1):225. doi: 10.1186/s12889-017-4121-2. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4121-2 .10.1186/s12889-017-4121-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Okita SY. Self-other's perspective taking: the use of therapeutic robot companions as social agents for reducing pain and anxiety in pediatric patients. Cyberpsychol Behav Soc Netw. 2013 Jun;16(6):436–41. doi: 10.1089/cyber.2012.0513. [DOI] [PubMed] [Google Scholar]
- 73.Choo E, Guthrie KM, Mello M, Wetle TF, Ranney M, Tapé C, Zlotnick C. "I need to hear from women who have 'been there'": developing a woman-focused intervention for drug use and partner violence in the emergency department. Partner Abuse. 2016 Apr;7(2):193–220. doi: 10.1891/1946-6560.7.2.193. https://europepmc.org/abstract/MED/27695604 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bar-Lev S. "We are here to give you emotional support": performing emotions in an online HIV/AIDS support group. Qual Health Res. 2008 Apr;18(4):509–21. doi: 10.1177/1049732307311680.1049732307311680 [DOI] [PubMed] [Google Scholar]
- 75.Wijma EM, Veerbeek MA, Prins M, Pot AM, Willemse BM. A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: results of a pilot study. Aging Ment Health. 2018 Sep;22(9):1115–23. doi: 10.1080/13607863.2017.1348470. [DOI] [PubMed] [Google Scholar]
- 76.Han JY, Shah DV, Kim E, Namkoong K, Lee SY, Moon TJ, Cleland R, Bu QL, McTavish FM, Gustafson DH. Empathic exchanges in online cancer support groups: distinguishing message expression and reception effects. Health Commun. 2011 Mar;26(2):185–97. doi: 10.1080/10410236.2010.544283. https://europepmc.org/abstract/MED/21318917 .933308503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Högberg KM, Sandman L, Nyström M, Stockelberg D, Broström A. Caring through web-based communication: a qualitative evaluation of a nursing intervention to create holistic well-being among patients with hematological disease. J Holist Nurs. 2018 Sep;36(3):218–27. doi: 10.1177/0898010116667343.0898010116667343 [DOI] [PubMed] [Google Scholar]
- 78.Steinwachs DM, Roter DL, Skinner EA, Lehman AF, Fahey M, Cullen B, Everett AS, Gallucci G. A web-based program to empower patients who have schizophrenia to discuss quality of care with mental health providers. Psychiatr Serv. 2011 Nov;62(11):1296–302. doi: 10.1176/ps.62.11.pss6211_1296. https://europepmc.org/abstract/MED/22211208 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kysely A, Bishop B, Kane R, Cheng M, De Palma M, Rooney R. Expectations and experiences of couples receiving therapy through videoconferencing: a qualitative study. Front Psychol. 2019 Jan 21;10:2992. doi: 10.3389/fpsyg.2019.02992. https://europepmc.org/abstract/MED/32038380 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Blair Irvine A, Billow MB, Eberhage MG, Seeley JR, McMahon E, Bourgeois M. Mental illness training for licensed staff in long-term care. Issues Ment Health Nurs. 2012 Mar;33(3):181–94. doi: 10.3109/01612840.2011.639482. https://europepmc.org/abstract/MED/22364430 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.van Rijn B, Cooper M, Jackson A, Wild C. Avatar-based therapy within prison settings: pilot evaluation. Br J Guid Counc. 2017;45(3):268–83. doi: 10.1080/03069885.2015.1068273. https://eric.ed.gov/?id=EJ1140297 . [DOI] [Google Scholar]
- 82.Fordham J, Ball C. Framing mental health within digital games: an exploratory case study of hellblade. JMIR Ment Health. 2019 Apr 18;6(4):e12432. doi: 10.2196/12432. https://mental.jmir.org/2019/4/e12432/ v6i4e12432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tippin GK, Maranzan KA. Efficacy of a photovoice‐based video as an online mental illness anti‐stigma intervention and the role of empathy in audience response: a randomized controlled trial. J Appl Soc Psychol. 2019 Jun;49(6):381–94. doi: 10.1111/jasp.12590. https://psycnet.apa.org/record/2019-17669-001 . [DOI] [Google Scholar]
- 84.Milbury K, Weathers SP, Durrani S, Li Y, Whisenant M, Li J, Lim B, Weinberg JS, Kesler SR, Cohen L, Bruera E. Online couple-based meditation intervention for patients with primary or metastatic brain tumors and their partners: results of a pilot randomized controlled trial. J Pain Symptom Manage. 2020 Jun;59(6):1260–7. doi: 10.1016/j.jpainsymman.2020.02.004.S0885-3924(20)30088-9 [DOI] [PubMed] [Google Scholar]
- 85.van Velsen L, Ludden G, Grünloh C. The limitations of user-and human-centered design in an eHealth context and how to move beyond them. J Med Internet Res. 2022 Oct 05;24(10):e37341. doi: 10.2196/37341. https://www.jmir.org/2022/10/e37341/ v24i10e37341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Smits M, Ludden G, Peters R, Bredie SJ, van Goor H, Verbeek PP. Values that matter: a new method to design and assess moral mediation of technology. Des Issues. 2022;38(1):39–54. doi: 10.1162/desi_a_00669. https://direct.mit.edu/desi/article-abstract/38/1/39/108742/Values-that-Matter-A-New-Method-to-Design-and?redirectedFrom=fulltext . [DOI] [Google Scholar]
- 87.Fletcher RR, Tam S, Omojola O, Redemske R, Kwan J. Wearable sensor platform and mobile application for use in cognitive behavioral therapy for drug addiction and PTSD. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:1802–5. doi: 10.1109/IEMBS.2011.6090513. [DOI] [PubMed] [Google Scholar]
- 88.Wray T, Kahler CW, Simpanen EM, Operario D. Game plan: development of a web app designed to help men who have sex with men reduce their HIV risk and alcohol use. JMIR Form Res. 2018 Aug 23;2(2):e10125. doi: 10.2196/10125. https://formative.jmir.org/2018/2/e10125/ v2i2e10125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Terry C, Cain J. The emerging issue of digital empathy. Am J Pharm Educ. 2016 May 25;80(4):58. doi: 10.5688/ajpe80458. https://europepmc.org/abstract/MED/27293225 .ajpe58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Louie AK, Coverdale JH, Balon R, Beresin EV, Brenner AM, Guerrero AP, Roberts LW. Enhancing empathy: a role for virtual reality? Acad Psychiatry. 2018 Dec;42(6):747–52. doi: 10.1007/s40596-018-0995-2.10.1007/s40596-018-0995-2 [DOI] [PubMed] [Google Scholar]
- 91.Elzie CA, Shaia J. Virtually walking in a patient's shoes-the path to empathy? Med Sci Educ. 2020 Dec;30(4):1737–9. doi: 10.1007/s40670-020-01101-0. https://europepmc.org/abstract/MED/34457839 .1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020 Jun 02;22(6):e19361. doi: 10.2196/19361. https://www.jmir.org/2020/6/e19361/ v22i6e19361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Case A. Calm Technology: Principles and Patterns for Non-Intrusive Design. New York, NY, USA: O′Reilly; 2015. Dec, [Google Scholar]
- 94.Picard RW. Affective Computing. Cambridge, MA, USA: MIT Press; 1997. [Google Scholar]
- 95.Joshanloo M. Eastern conceptualizations of happiness: fundamental differences with western views. J Happiness Stud. 2014;15(2):475–93. doi: 10.1007/s10902-013-9431-1. https://link.springer.com/article/10.1007/s10902-013-9431-1 . [DOI] [Google Scholar]
- 96.Ji LJ, Khei M, Yap S, Wang X, Zhang Z, Hou Y. Cultural differences in the construal of suffering and the COVID-19 pandemic. Soc Psychol Personal Sci. 2021 Aug;12(6):1039–47. doi: 10.1177/1948550620958807. https://journals.sagepub.com/doi/10.1177/1948550620958807 . [DOI] [Google Scholar]
- 97.Sieverink F, Kelders SM, van Gemert-Pijnen JE. Clarifying the concept of adherence to eHealth technology: systematic review on when usage becomes adherence. J Med Internet Res. 2017 Dec 06;19(12):e402. doi: 10.2196/jmir.8578. https://www.jmir.org/2017/12/e402/ v19i12e402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kelders SM, van Zyl LE, Ludden GD. The concept and components of engagement in different domains applied to eHealth: a systematic scoping review. Front Psychol. 2020 May 27;11:926. doi: 10.3389/fpsyg.2020.00926. https://europepmc.org/abstract/MED/32536888 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies for each of the included databases.


