Introduction
Head and neck cancers now account for almost 3% of all new cancer cases nationwide, with 47,813 new cases and 10,492 deaths per year.1 Malignancies of the head and neck most commonly originate from epithelial origin, namely squamous cell carcinoma (SCCa). Oropharyngeal cancer has been rising yearly by an average of 0.6% per year, with the average five-year relative survival rate at an estimated 68%.2 Human papillomavirus (HPV) is, historically, most associated with cervical cancer in women. However, HPV-related head and neck malignancies are becoming more prevalent in the United States, with a higher predilection for the male population. HPV-related oropharyngeal SCCa has now surpassed cervical cancer as the most common HPV-related cancer in the US, representing 19,775 yearly cases, compared with 12,143 yearly cases of cervical cancer.3 Current projections estimate a current upward trend for the next decade, with predictions greater than 30,000 annual cases by year 2029.3 HPV-associated malignancies are 2.7 times more frequently diagnosed in men, and has a mortality 2.8 times that of women according to the latest data.4
Risk Factors
The main risk factors for oropharyngeal SCCa have been multi-factorial, including tobacco and alcohol use. Recent data has shown an increasing trend with HPV-associated tumors, specifically, HPV-16 which has accounted for more than 90% of cases. Approximately 80% of oropharyngeal cancers in the US are associated with HPV.5 These specific tumor types have been the main reason for increasing incidences, especially in the younger population.
HPV-16 and HPV-33 have been recognized as the main etiologic factors for the increase of cancers in the cervix, vulva, vagina, penis, and anus, as well as the oropharynx, which contrasts with traditional tobacco- and alcohol-related HPV-negative cancers. The HPV-associated disease is molecularly and clinically unique compared to the traditional HPV-negative oropharyngeal cancers. The etiology is from the double stranded DNA viruses E6 and E7 oncogenes that inactivate the p53 tumor suppressor gene and the retinoblastoma protein which leads to release of transcription factors causing cell cycle progression.3
Currently, HPV is the most common and widespread sexually transmitted disease worldwide, and is the main cause of cancer in anogenital and oropharyngeal regions. Even though there has been a decrease in HPV-negative oropharyngeal cancers, there continues to be an increase in the HPV-related oropharyngeal SCCa. The main accepted hypothesis is that oral sexual behaviors have become more common and frequent in the last 50 years, particularly in younger age groups. Individuals with more than ten lifetime oral sex partners have a greater than four-fold increased risk of HPV-positive oropharyngeal SCCa.3
Diagnosis
Patients with HPV-related SCCa have a better prognosis and are usually younger and non-smokers compared to HPV-negative SCCa patients (figure 1). The HPV-related SCCa usually demonstrates a nonkeratinizing epithelium which is distinct from tobacco and alcohol related oral diseases, which are usually keratinizing SCCa.6 Due to the improved survival rate of HPV-associated oropharyngeal SCCa, the American Joint Committee on Cancer has made important changes to its staging system. In 2018, the American Society of Clinical Oncology, National Comprehensive Cancer Network, and College of American Pathologists developed guidelines that all specimens should be tested for HPV-tumor status using immunohistochemical staining against p16 with at least 70% nuclear and cytoplasmic expression as an indicator (figure 2). The other gold standard is the HPV E6/E7 mRNA and HPV DNA detection by polymerase chain reaction and in situ hybridization. In 2017, the eighth edition classified oral and oropharyngeal cancers by the p16 marker, downstaging the p16 positive oropharyngeal cancers from previous editions.6
Figure 1.
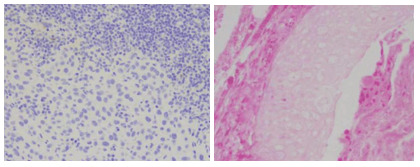
HPV-Negative Squamous Cell Carcinoma
Figure 2.
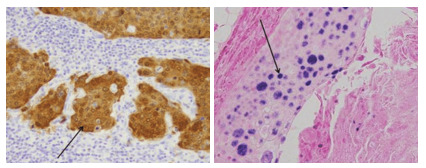
Immunohistochemistry Staining of p16 in HPV-Positive Oropharyngeal Squamous Cell Carcinoma Tumor.
The arrows indicate a cluster of tumor cells staining positive for p16.7
Vaccination
The best diagnostic strategy for HPV-related oropharyngeal SCCa continues to be early diagnosis as well as vaccination against HPV-infection. The FDA currently has four preventive cancer vaccines, with three of the vaccines, Cervarix, Gardasil, and Gardasil-9, approved to prevent the infection of HPV and one preventive Hepatitis B (HBV) vaccine (HEPLISAV-B) that protects against the Hepatitis B virus which prevents development of HBV-related liver cancer. Since 2016, Gardasil-9 has been the only HPV vaccine available in the US and protects against the subtypes of HPV-6, 11, 16, 18, 31, 33, 45, 52, 58. HPV vaccines were initially developed to prevent anogenital tract cancers, but since the 2-dose scheduled vaccine protects against the other high-risk variants of HPV that can cause oropharyngeal cancers, the vaccine can be used to prevent oropharyngeal diseases.8 The CDC and American Academy of Pediatrics highly recommend administering the first dose of the HPV vaccine to children as early as 9-years old, but definitely by ages 11-12 years. Doses are given 6 to 12 months apart. Children who start the HPV vaccine series on or after their 15th birthday need three doses, given over 6 months. Everyone through age 26 years should get the HPV vaccine, and if over the age of 26 should consult with their doctor.9
In 2018, the American Dental Association and the American Academy of Pediatric Dentistry developed guidelines for dentists to participate in the prevention of oral and oropharyngeal cancer through education and endorsing the HPV vaccination. In 2019, Oregon passed legislation to allow dental healthcare providers to prescribe and administer any vaccine as part of Public Health Modernization Implementation.5 In 2018, Oregon’s HPV initiation dose was 67% and HPV completion doses were 46%, which has increased by 6% and 7%, respectively, in 2022. In 2019, 71.5% of adolescents aged 13-17 years had received one dose of HPV, and 54.2% had completed the HPV vaccination.10 Each year, 88.9% of eligible adolescents obtain the first dose, however only 53.7% follow up for the second dose indicating that continued efforts are needed to improve for follow up.11
Treatment
Patients diagnosed with oral and oropharyngeal SCCa require a multidisciplinary work up and treatment. The new staging algorithm for HPV-positive oropharyngeal SCCa is different from staging for HPV-negative oropharyngeal SCCa, which is based off the biomarker p16 (figure 3). Staging for p16-positive does not include T4b diseases and defines clinical nodal stages by size and laterality and defines pathological nodal stage by number of lymph nodes. Pathologic and clinical nodal staging for p16-positive diseases also omits consideration of extra nodal extension.12 Based on the most recent TNM staging, most patients with early-stage disease of the soft palate/oropharynx/tonsils/base of tongue are treated with definitive surgical resection even with evidence of isolated nodal disease.13
Figure 3.
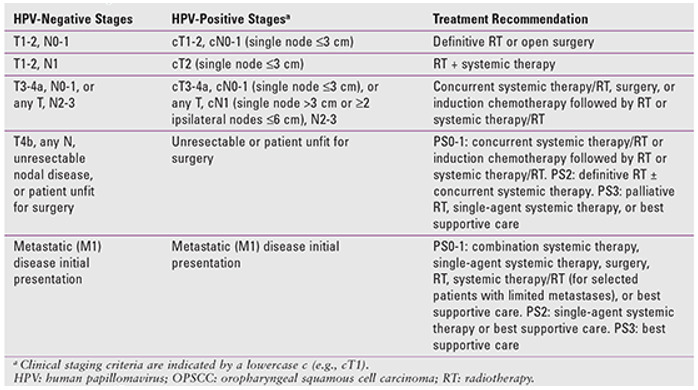
NCCN Recommendations for Managing the Different Clinical Stages of HPV-Positive and HPV-Negative Tumors
Patients with HPV-related oropharyngeal SCCa presented with higher two-year survival rates than those patients with HPV-unrelated oropharyngeal SCCa. Due to better response to surgical resection and chemoradiotherapy, there has been a de-intensification of HPV-related oropharyngeal SCCa therapies. Different nonsurgical approaches have included reducing radiotherapy or chemotherapy doses. The radiotherapy usually includes 44-72 Gy depending on tumor infiltration.13 The customary approach was previously radiation doses above 50 Grays, which caused patients to experience significant side effects (e.g.: dry mouth, limited mouth opening, loss of taste). Lowering the radiation doses as low as 44 Grays has been shown to be both safe and effective, and has resulted in patients experiencing fewer side effects.13 Optimal treatment options continue to be unclear, however the advancements of de-intensification treatments along with the better prognosis and higher five-year survival rates are improving the long-term quality of life for the patient with HPV-positive oropharyngeal cancer.14
It is important to note that in HPV-positive OPSCC, pathological staging criteria differ from clinical staging criteria. Early-stage disease is generally managed with single-modality treatment, whereas advanced-stage disease requires chemoradiotherapy with or without neck dissection or surgical resection with reconstruction and postoperative chemoradiotherapy.13
Conclusion
HPV-related SCCa continues to cause an increased incidence of oropharyngeal cancer in the US. HPV-related oropharyngeal cancer has distinct risk factors with unique epidemiology, staging, and prognosis. Within the head and neck cancer community and dental community, early diagnosis and treatment are the most important primary factors. HPV-positive oropharyngeal SCCa has great prognosis and multiple trials continue to take place to de-intensify treatment with the goal to decrease treatment related morbidities.15 Continual promotion and education of the HPV vaccination has the potential to bring more of a positive impact on public, with vaccination likely preventing oral HPV infection and the potential of living longer and better quality lives.
References
- 1.U.S. Cancer Statistics Working Group. (2022). U.S. cancer statistics data visualizations tool. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. https://www.cdc.gov/cancer/dataviz
- 2.National Cancer Institute. (n.d.). Cancer stat facts: oral cavity and pharynx cancer. https://seer.cancer.gov/statfacts/html/oralcav.html
- 3.Rettig, E. M., & Sethi, R. K. V. (2021, October). Cancer of the oropharynx and the association with human papillomavirus. Hematology/Oncology Clinics of North America, 35(5), 913–931. 10.1016/j.hoc.2021.05.004 [DOI] [PubMed] [Google Scholar]
- 4.Siegel, R. L., Miller, K. D., & Jemal, A. (2017, January). Cancer Statistics, 2017. CA: a Cancer Journal for Clinicians, 67(1), 7–30. 10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- 5.Louredo, B. V. R., Prado-Ribeiro, A. C., Brandão, T. B., Epstein, J. B., Migliorati, C. A., Piña, A. R., et al. Santos-Silva, A. R. (2022, August). State-of-the-science concepts of HPV-related oropharyngeal squamous cell carcinoma: A comprehensive review. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 134(2), 190–205. 10.1016/j.oooo.2022.03.016 [DOI] [PubMed] [Google Scholar]
- 6.Sabu, A., Mouli, N. V. R., Tejaswini, N., Rohit, V., Nishitha, G., & Uppala, D. (2019, Oct-Dec). Human papillomavirus detection in oropharyngeal squamous cell carcinoma using p16 immunohistochemistry. International Journal of Applied & Basic Medical Research, 9(4), 212–216. 10.4103/ijabmr.IJABMR_221_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Compton, A. M., Moore-Medlin, T., Herman-Ferdinandez, L., Clark, C., Caldito, G. C., Wang, X. I., et al. Nathan, C. O. (2011, July). Human papillomavirus in metastatic lymph nodes from unknown primary head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg, 145(1), 51–57. 10.1177/0194599811400385 [DOI] [PubMed] [Google Scholar]
- 8.Dunn, G. P. (2023). Cancer Vaccines: Preventive, therapeutic, personalized. Cancer Research Institute. https://www.cancerresearch.org/treatment-types/cancer-vaccines
- 9.Centers for Disease Control and Prevention. (n.d.). National center for HIV/AIDS, viral hepatitis, STD, and TB prevention. https://www.cdc.gov/nchhstp/default.htm
- 10.Oregon Immunization Program. (n.d.). ALERT Immunization Information System. https://www.oregon.gov/oha/PH/PREVENTIONWELLNESS/VACCINESIMMUNIZATION/ALERT/Pages/index.aspx
- 11.Elam-Evans, L. D., Yankey, D., Singleton, J. A., Sterrett, N., Markowitz, L. E., Williams, C. L., et al. Stokley, S. (2020, August 21). National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years— United States, 2019. MMWR. Morbidity and Mortality Weekly Report, 69(33), 1109–1116. 10.15585/mmwr.mm6933a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flavill, E., Fang, Y. V., Miles, B., Truelson, J., & Perkins, S. (2014, May). Induction chemotherapy followed by concurrent chemoradiotherapy for advanced stage oropharyngeal squamous cell carcinoma with HPV and P16 testing. The Annals of Otology, Rhinology, and Laryngology, 123(5), 365–373. 10.1177/0003489414526685 [DOI] [PubMed] [Google Scholar]
- 13.National Comprehensive Cancer Network. (2023, Jan). Cancer of the oropharynx. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1437
- 14.Silver, J. A., Turkdogan, S., Roy, C. F., Subramaniam, T., Henry, M., & Sadeghi, N. (2022, May 18). De-escalation strategies for human papillomavirus-associated oropharyngeal squamous cell carcinoma-Where are we now? Current Oncology (Toronto, Ont.), 29(5), 3668–3697. 10.3390/curroncol29050295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vermorken, J. B., Psyrri, A., Mesía, R., Peyrade, F., Beier, F., de Blas, B., et al. Licitra, L. (2013, May). OP041: Impact of human papillomavirus (HPV) and p16 status on survival and response with cisplatin plus 5-FU and cetuximab in recurrent and/or metastatic squamous cell carcinoma of the head and neck (R/M SCCHN): Analysis of the phase III extreme trial. Oral Oncology, 49(suppl 1), S19–S20. 10.1016/j.oraloncology.2013.03.049 [DOI] [Google Scholar]


