Abstract
Objectives:
We aimed to examine the impact of COVID-19 pandemic related stay-at-home orders on weekly reports of mood and activity before and during COVID-19 in a sample of older Veterans and their cohabitants.
Methods:
Urban and rural Veterans and their cohabitants living in the Pacific Northwest ≥62 years old were enrolled as part of the Collaborative Aging Research Using Technology initiative (n=100, age = 71.2 ± 6.5, 41% women). Participants reported frequency of social activities (e.g., travel away), physical illness, and mood (blue mood and loneliness) via weekly online health forms.
Results:
A total of 2,441 weekly online health forms (OHFs) were collected from 100 participants. During the COVID-19 pandemic, blue mood (OR=4.4, p<.0001) and loneliness (OR=7.2, p<.0001) were significantly higher than before the pandemic, and travel away from home was significantly lower (OR=0.5, p<.0001). Prevalence of blue mood and loneliness were not associated with rurality.
Conclusions:
The current study established that blue mood and loneliness were significantly more prevalent in older Veterans following COVID-19 stay-at-home orders regardless of rurality.
Clinical Implications:
The COVID-19 pandemic associated health precautions, while necessary to curb acute health risks, have created a unique situation that places vulnerable populations at increased risk of low mood.
Keywords: depression, social isolation, rural, military personnel, remote monitoring, COVID-19
Introduction
Social isolation and loneliness is a growing concern among older adults (Menec et al., 2020) and is notably high among at-risk subgroups (e.g., older United States Veterans) (Wilson et al., 2018). Social isolation is often defined as a deficit in the number and frequency of contact with relationships (Perissinotto et al., 2019). Related to social isolation, loneliness reflects the discrepancy between one’s desired and actual level of social connectedness. A recent report highlights that approximately one-third of adults 45 years of age or older reported feeling lonely and at least 25% of those 65 years and older reported feeling social isolated (National Academies of Sciences, 2020). While social isolation does not necessarily result in loneliness, they often co-occur and are associated with multiple poor health outcomes (Cacioppo et al., 2010; Hoogendijk et al., 2020; Perissinotto et al., 2012). Social isolation is associated with a 50% increased risk of serious medical conditions, such as dementia, and a four times greater risk for hospitalization related to psychiatric care (Mistry et al., 2001; National Academies of Sciences, 2020). Loneliness, on the other hand, is associated with emotional distress, including depression (Cacioppo et al., 2010; Kotwal et al., 2021).
The COVID-19 pandemic and associated health precautions, while necessary to curb acute health risks, have by their nature increased social isolation in older adults (Wilson et al., 2018). Stress process models of mental health posit that periods of prolonged stress, such as the uncertainty associated with the pandemic, result in negative mental health outcomes, although there is evidence that social interactions may mitigate these symptoms somewhat (Katerndahl & Parchman, 2002). In prior pandemics, quarantines were associated with potentially long term negative psychological effects, presumably exacerbated by the pandemic associated social isolation (Dennis et al., 2021). There is early evidence of similar negative outcomes being associated with the COVID-19 pandemic and sheltering in place, including depression, higher risk for mortality, greater health care spending, and lower quality of life (Ammar et al., 2020; Krendl & Perry, 2021; Lebrasseur et al., 2021). Recent research suggests increased depression and worry is associated with social isolation and loneliness during the COVID-19 pandemic, with a subgroup of older adults experiencing persistent difficulty with emotional coping and loneliness despite the rollback of stay-at-home orders (Kotwal et al., 2021). For instance, Veterans are at high risk for loneliness and social isolation during the pandemic, with reported loneliness compounding depressive rates and substance abuse, with little benefit from social support (Fitzke et al., 2021). Given the negative outcomes associated with social isolation, depression, and loneliness, early detection may be key in providing services to at-risk subgroups of older adults such as Veterans to curb potential long-term difficulties.
Technology in the form of short but frequent online surveys offers the unique ability to frequently assess physical and mental health-related changes in aging and rural populations over time and investigate their associations with specific outcomes (Beattie et al., 2020; Kaye et al., 2011). This is especially important during the COVID-19 pandemic given frequent in-person assessments were not feasible or allowed. Accordingly, the current study utilized weekly online surveys in a rural and urban Veteran cohort and their cohabitants in Oregon, United States to longitudinally monitor for changes in reported blue mood and loneliness, social activities (overnight visitors, travel away), and physical illness (physical health limitations, hospitalizations/emergency department [ED] visits) during the initial stages of the COVID-19 pandemic and related stay-at-home orders. Specifically, it was hypothesized that reported social activities declined during the initial stages of the COVID-19 pandemic, resulting in increased physical illness and psychological distress as a function of rurality.
Methods
Participants and procedures
Participants were enrolled as part of the Collaborative Aging Research using Technology (CART) initiative, a NIH- and VA HSRD-funded, multi-site study examining the feasibility of digital health monitoring and intervention in older adults (Beattie et al., 2020). The CART system represents an expansion on the Oregon Center for Aging & Technology (ORCATECH), a technology platform that has successfully developed algorithms to study measures of gait (Dodge et al., 2012), computer use (Kaye et al., 2014), and medication adherence (Austin et al., 2017), as examples, to monitor aging and dementia via in-home sensors. Compared with conventional neuropsychological tests, these unobtrusive in-home devices and sensors are almost unnoticeable to participants and collect data in a frequent fashion.
Inclusion criteria for the study included participants being: 62 years or older, living alone or with a cohabitant over age 18 (cohabitants were required to consent to fully participate in the study), age and education adjusted MoCA >18, and household ability to have a reliable broadband internet connection. Exclusion criteria included: patient having conditions that would limit physical participation at entry to study (e.g., wheelchair bound), any uncontrolled medical condition that would be expected to preclude completion of the study such as late stage cancers, and more than two people living in the participant’s residence (overnight visitors were acceptable), and Geriatric Depression Scale score greater than 5 (Yesavage, 1988).
The CART initiative tested innovative technology applications in four diverse, older adult populations; this report focuses on the Veteran cohort and their cohabitants. Volunteers were recruited from the Portland, Oregon Veterans Affairs (VA) Medical Center to participate in a longitudinal aging study of unobtrusive sensing technology whose protocol included completing weekly online health surveys (Beattie et al., 2020). Written informed consent was obtained from all participants (Veterans and cohabitants) consistent with the Helsinki and Portland VA intuitional guidelines. The study was approved by the Portland VA and Oregon Health & Science Institutional Review Board.
Measures
As part of the CART study protocol, all participants completed weekly online health forms (OHFs). OHFs have been used as self-report data collection tools in ORCATECH studies since 2007 (Kaye et al., 2011). Participants received weekly web-based surveys via email that asked questions about behaviors that could affect activity patterns which may be related to functional or cognitive decline. Surveys were administered on the Qualtrics Survey Platform. Research personnel contacted participants if he or she neglected to complete the survey or needed technical assistance, in order to ensure data capture and quality. Thirteen questions chosen for practical reasons included medication changes, falls, injuries, health changes, emergency room visits, blue mood, changes to living space, travel away from home, overnight visitors, need for increased assistance, loneliness, pain intensity, and pain interference. OHFs from January 6, 2020 to July 8, 2020 were analyzed for this study, in the context of a national emergency being declared in the U.S. on March 13, 2020 and Oregon Governor Kate Brown’s subsequent March 23, 2020 stay-at-home restrictions orders. Primary outcome domains in the current analysis were yes/no questions assessing mood (e.g., blue mood, loneliness), health (e.g., hospitalizations, ED visits), and social activities (e.g., overnight visitors, travel from home) variables following national emergency declaration. Blue mood was defined and questioned, “Have you felt downhearted or blue for three or more days in the past week?” (Yesavage, 1988). Loneliness questions included, “In the past week I felt lonely.” Travel from home questions included, “In the past week, have you been away from home overnight?” Overnight visitors were assessed by the question, “In the past week, have you had visitors who stayed with you in your home for a night or more?” Participants were asked weekly as part of the OHF if he or she visited the emergency room or were admitted to the hospital during the past week. Health limitations was queried as, “Has your physical health been limited more than usual this past week?” Rurality was measured by U.S. Census-based rural-urban commuting area (RUCA) score (urban = RUCA score 1–3; rural = RUCA score 4–6; small/isolated rural = RUCA score 7–10).
Statistical Analyses
Analysis of covariance (ANOVA) and chi-square tests were used to compare continuous and categorical baseline characteristic variable across rurality groups, respectively. We compared frequency of health form reports before and during the COVID-19 pandemic using generalized estimating equations (GEE) logit models (i.e. a repeated measures analysis using a logit link function, SAS PROC GLIMMIX, (Liang & Zeger, 1986)). Multiple weekly observations from each individual were included, while within-individual correlations were considered in estimating standard errors. The time before and during the COVID-19 pandemic (March 13, 2020) was indicated by a dummy variable (0/1). Age, gender, living arrangement and rurality were included as covariates. GEE was appropriate because the repeated measures outcome variable data distribution was binary not continuous, and GEE has been shown to be an effective statistical method in similar previous data sets (Wu et al., 2022). All analyses were conducted with SAS 9.4 SAS software version 9.4; SAS Institute Inc., Cary, NC, USA).
RESULTS
The demographic information of the sample (n=100) is summarized overall and by rurality in Table 1. Mean age was 71.2 (SD 6.5), mean education was 14.7 years (SD 2.2) and the sample was 41% female. During the study period, 23% reported ever having blue mood, 21% reported loneliness, 60% reported travel away from home, and 48% reported overnight visitors. There were no differences on any baseline demographic characteristics or prevalence of weekly health form reports by rurality. A total of 2441 weeks of survey data were analyzed (911 and 1530 OHFs before and during the COVID-19 pandemic, respectively). On average, 24.4 (SD = 5.4) weeks of data were collected per participant.
Table 1.
Baseline sociodemographic characteristics of cohort by ruralitya.
| Variable | Full sample (N=100) |
Urban (N=35) |
Large rural (N=34) |
Small rural (N=31) |
|---|---|---|---|---|
| Age, M (SD) | 71.2 (6.5) | 71.3 (7.0) | 70.0 (5.4) | 72.3 (6.9) |
| Education (yrs), M (SD) | 14.7 (2.2) | 14.8 (2.3) | 15.1 (2.0) | 14.0 (2.1) |
| Female, No. (%) | 41 (41%) | 15 (43%) | 14 (41%) | 12 (39%) |
| Race, No. (%) | ||||
| White | 93 (93%) | 32 (91%) | 30 (88%) | 31 (100%) |
| Non-White | 7 (7%) | 3 (9%) | 4 (12%) | 0 (0%) |
| Single, No. (%) | 19 (19%) | 5 (14%) | 10 (29%) | 4 (13%) |
| Cognitive impairment, No. (%) | 39 (40%) | 12 (38%) | 14 (41%) | 14 (42%) |
| Geriatric Depression score, M (SD) | 1.7 (2.0) | 1.5 (2.1) | 1.5 (1.6) | 1.9 (2.3) |
| Weekly Online Health Formb, No. (%) | ||||
| Blue mood | 23 (23%) | 10 (29) | 9 (26) | 4 (13) |
| Loneliness | 21 (21%) | 9 (26) | 8 (24) | 4 (13) |
| Overnight visitors | 48 (48%) | 12 (34) | 20 (59) | 16 (52) |
| Travel away from home | 60 (60%) | 18 (51) | 26 (76) | 16 (52) |
| Hospitalization/ED visit | 26 (26%) | 11 (31) | 5 (15) | 10 (32) |
| Physical health limitations | 61 (61%) | 25 (71) | 19 (56) | 17 (55) |
Rurality based on RUCA score: Urban=1–3; Large rural=4–6; Small rural=7–10.
Prevalence of ever reporting during study time period (each participant counted only once, irrespective of number of individual reports).
Abbreviations: RUCA, Rural-urban commuting area score (U.S. Census-based)
After adjusting for age, gender, rurality and living arrangement, reports of blue mood (OR=4.4, p<.0001) and loneliness (OR=7.2, p<.0001) were significantly higher during the COVID-19 pandemic than before the COVID-19 pandemic (Table 2; Figure 1). Participants were half as likely to travel away from home following the onset of the COVID-19 pandemic as compared to before the COVID-19 pandemic (OR=0.5, p<.0001). No differences were observed before and during the COVID-19 pandemic in reports of overnight visitors (p=0.87), physical health limitations (p=0.29), or hospitalizations/ED visits (p=0.38).
Table 2.
GEE Models of online health form data pre-post onset of COVID-19 pandemic restrictions
| Parameter | Estimate | SE | Odds ratio (95%) CI | p-value |
|---|---|---|---|---|
| Model 1: Blue mood | ||||
| Intercept | −6.60 | 3.45 | 0.06 | |
| COVID-19 pandemic (yes/no) | 1.48 | 0.33 | 4.38 (2.31 – 8.30) | <0.01* |
| Age | 0.02 | 0.05 | 1.02 (0.93 – 1.12) | 0.69 |
| Female vs. male | −0.28 | 0.64 | 0.76 (0.22 – 2.66) | 0.67 |
| Large rural | 0.00 | 0.65 | 1.00 (0.28 – 3.53) | 0.99 |
| Small rural | −0.74 | 0.74 | 0.48 (0.11 – 2.03) | 0.32 |
| Single vs. married | 0.55 | 0.72 | 1.74 (0.43 – 7.10) | 0.44 |
| Model 2: Loneliness | ||||
| Intercept | −11.09 | 4.21 | 0.01 | |
| COVID-19 pandemic (yes/no) | 1.97 | 0.38 | 7.17 (3.43 – 14.99) | <0.01* |
| Age | 0.07 | 0.06 | 1.07 (0.96 – 1.19) | 0.24 |
| Female vs. male | −0.31 | 0.85 | 0.73 (0.14 – 3.85) | 0.71 |
| Large rural | −0.30 | 0.84 | 0.74 (0.14 – 3.89) | 0.72 |
| Small rural | −0.42 | 0.90 | 0.66 (0.11 – 3.85) | 0.64 |
| Single vs. married | 2.22 | 0.85 | 9.17 (1.72 – 48.90) | <0.01* |
| Model 3: Travel away from home | ||||
| Intercept | −1.69 | 2.08 | 0.42 | |
| COVID-19 pandemic (yes/no) | −0.71 | 0.15 | 0.49 (0.37 – 0.67) | <0.01* |
| Age | −0.02 | 0.03 | 0.98 (0.93 – 1.04) | 0.53 |
| Female vs. male | 0.00 | 0.37 | 1.00 (0.48 – 2.07) | 1.00 |
| Large rural | 1.23 | 0.39 | 3.43 (1.60 – 7.34) | <0.01* |
| Small rural | 0.47 | 0.42 | 1.60 (0.71 – 3.61) | 0.26 |
| Single vs. married | 0.06 | 0.44 | 1.06 (0.44 – 2.52) | 0.90 |
p<0.05
Figure 1.
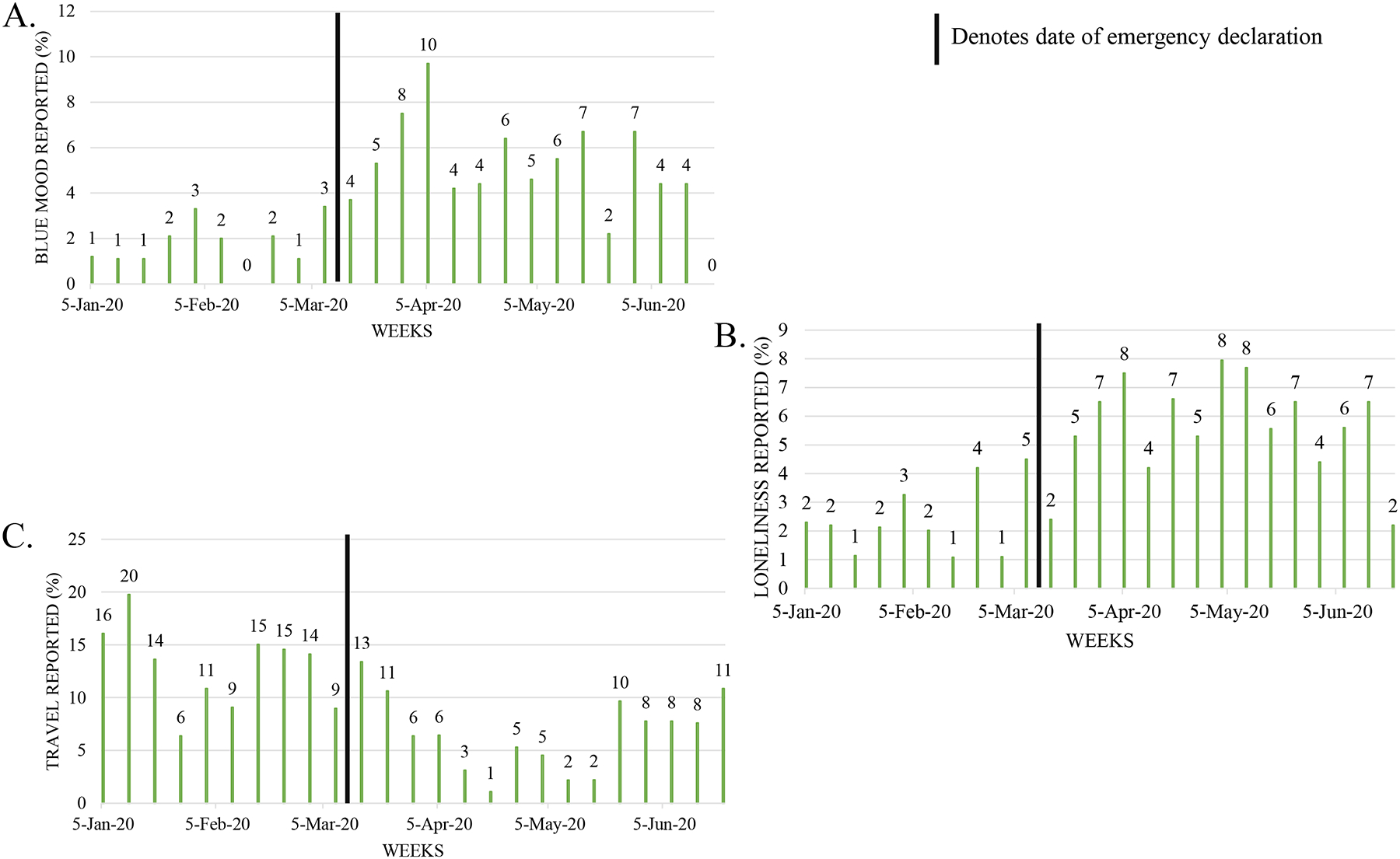
Generalized Estimating Equations Models Prevalence Rates Change Post-Emergency Declaration Compared to Pre-Declaration. (A) Reports of blue mood increased (OR=4.4); (B) Reports of loneliness increased (OR=7.2); (C) Reports of travel away from home decreased (OR=0.5).
Discussion
The current study examined the impact of the March 13, 2020 COVID-19 pandemic declaration of national emergency and Oregon Governor Kate Brown’s subsequent March 23, 2020 stay-at-home restrictions orders on weekly reported mood, social activities, and physical illness in a sample of older Veterans and their cohabitants. Overall, prevalence of blue mood and loneliness was higher during the COVID-19 pandemic in this cohort of older Veterans and their cohabitants, regardless of level of rurality. This is in alignment with recent findings in a non-Veteran cohort which reported older adults showing greater psychological distress during the pandemic, as compared to prior to the pandemic (Leese et al., 2021). The presence of loneliness and blue mood may reflect larger mental health concerns, as pandemic related loneliness has been associated with increased depressive symptoms, anxiety, worry, and concerns about general health (Kotwal et al., 2021). The cohort did not report a decline in physical health or an increase in hospitalizations/ED visits during the initial stages of the COVID-19 pandemic. It is possible that these medical outcomes are delayed, and continued longitudinal monitoring may show an increase in medical needs, but these factors did not appear to contribute to the findings of participants’ report of increased blue mood and loneliness.
The finding of increased blue mood and loneliness is consistent with stress process models, in which persistent stress and uncertainty related to the pandemic potentially contribute to psychological distress (Shattuck et al., 2022). Recent research indicates that older adults have experienced less pandemic-related stress and depressive symptoms as compared to younger adults despite being at higher risk for severe illness. This finding is presumably related to older adults general emotional resiliency and having less disruption in daily life due to having different social roles (i.e. retirement) than younger adults (Feliciano et al., 2022; Kotwal et al., 2021). It is also possible that increased computer usage may have mitigated the severity of blue mood in older adults, as research indicates increased computer usage in older adults during the pandemic, and that internet use decreases the probability of depression in older adults by 33%, particularly in those who are isolated (Cotten et al., 2014; Leese et al., 2021).
No changes were observed between pre- and post-pandemic declaration of national emergency for reports of overnight visitors. This result is seemingly in contrast to the finding of increased feelings of loneliness. One possible explanation is that the social impact of the pandemic is not easily attenuated by overnight visitors, as loneliness reflects a subjective experience. This finding is similar to recent published research which failed to find a relationship between anxiety symptoms and social contact during the pandemic, yet inconsistent with theoretical stress process models that posit increased social connectedness serves as a protective factor for mental health during times of adversity (Charles & Carstensen, 2010; Shattuck et al., 2022).
Taken together, findings suggest older Veterans and their cohabitants experienced loneliness and blue mood during, at minimum, the early stages of the pandemic irrespective of the amount of social contact or urban-rural setting. While research indicates that older adults increased their computer usage during the pandemic, this has not necessarily translated into increased socializing or improved mood (Kotwal et al., 2021; Leese et al., 2021; Stone & Veksler, 2022). Of interest, recent research indicates a subgroup of older adults continue to have increasing loneliness over the course of the pandemic despite relaxation of stay-at-home orders (Kotwal et al., 2021), associated with difficulty with emotional coping and a lack familiarity with technology. As such, simply encouraging video-mediated socializing in older adults who are unfamiliar with technology is likely not sufficient to curb loneliness. Instead, promoting technology literacy may be an important step for increasing the efficacy of technology-mediated care, and for decreasing feelings of loneliness in older adults (Gould & Hantke, 2020). This may be of particular importance among the Veteran population, as COVID-19 pandemic related feelings of loneliness have been shown to compound the effects of depression and PTSD on alcohol use (Fitzke et al., 2021). Recent studies have indicated possible risk factors for pandemic-related loneliness among Veterans. Specifically, a diagnosis of a psychiatric disorder prior to the pandemic, unpartnered marital status, and the presence of pandemic-related social restrictions have all been associated with increased loneliness during the pandemic (Na et al., 2022). Monitoring older Veterans at elevated risk for loneliness via weekly surveys and unobtrusive monitoring (e.g. computer usage) may assist in determining which older Veterans require additional resources.
There are several limitations of the current findings. The sample included a cohort of Veterans and cohabitants in rural and urban settings of limited racial diversity. Thus, due to sample size of non-White participants, we were unable to report on specific racial/ethnic identities beyond aggregated all non-White groups. It is unclear how well these results generalize to non-Veteran populations, although results appear consistent with extant research (Luchetti et al., 2020). Further longitudinal monitoring is necessary to determine the future, long-term impact of the pandemic and related isolation on health.
This study informs the need for greater mental health services for at-risk older Veterans and their cohabitants, both rural and urban, in the context of COVID-19-related loneliness and blue mood. Further, more timely real-world monitoring of these variables may help to identify those at greater risk for blue mood and loneliness, allowing for the facilitation of appropriate interventions.
Clinical Implications.
Feelings of loneliness and blue mood increased during the initial stages of the pandemic, regardless of number of social interactions or rural setting.
Ongoing assessment of mood during the pandemic may help to detect those at greatest risk before prominent symptoms arise.
Funding:
This research was supported by the Collaborative Aging-in-place Research using Technology (CART) initiative through the Office of the Director, National Institutes of Health (OD), National Center for Advancing Translational Sciences (NCATS), National Institute of Biomedical Imaging and Bioengineering (NIBIB), National Institute of Nursing Research (NINR), National Institute on Aging (NIA), National Institute of Neurological Disorders and Stroke (NINDS), National Cancer Institute NCI) and the Veterans Administration HSR&D (Veterans Administration grant IIR 17-144; COVID-19 Rapid Response Supplement); the Oregon Roybal Center for Translational Research on Aging (NIA P30 AG024978); the Oregon Clinical Translational Research Institute CTSA award (UL1TR002369); and the National Institutes of Health (U2 CAG054397, P30 AG024978, P30 AG008017, RF1 AG22018, P30 AG10161, R01 AG051628, K01 AG059839).
Disclosure/Conflict of Interest:
HD works as a consultant for Biogen and is supported by the following federal grants: NIH R01AG051628, R01AG056102, R01AG069782, P30AG066518, R01AG072449, P30 AG008017, P30AG024978, U2CAG054397, R01AG056712, R01AG0380651, P30 AG053760, U01NS100611, U2CAG057441, U01NS106670, R01AG054484, RF1AG072449. The remaining authors report no conflicts with any product mentioned or concept discussed in this article.
Footnotes
All cited articles in this manuscript contain human and/or animal work approved by institutional review boards (IRBs) prior to publication.
Data Statement:
This data was presented at the 2020 conference of the Gerontological Society of America (GSA).
References
- Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, Bouaziz B, Brach M, Schmicker M, Bentlage E, How D, Ahmed M, Aloui A, Hammouda O, Paineiras-Domingos LL, Braakman-Jansen A, Wrede C, Bastoni S, Pernambuco CS, … Consortium, E.-C. (2020). Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PLoS One, 15(11), e0240204. 10.1371/journal.pone.0240204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin J, Klein K, Mattek N, & Kaye J (2017). Variability in medication taking is associated with cognitive performance in nondemented older adults. Alzheimers Dement (Amst), 6, 210–213. 10.1016/j.dadm.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beattie Z, Miller LM, Almirola C, Au-Yeung WM, Bernard H, Cosgrove KE, Dodge HH, Gamboa CJ, Golonka O, Gothard S, Harbison S, Irish S, Kornfeld J, Lee J, Marcoe J, Mattek NC, Quinn C, Reynolds C, Riley T, … Kaye J (2020). The Collaborative Aging Research Using Technology Initiative: An Open, Sharable, Technology-Agnostic Platform for the Research Community. Digit Biomark, 4(Suppl 1), 100–118. 10.1159/000512208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, & Thisted RA (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging, 25(2), 453–463. 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST, & Carstensen LL (2010). Social and emotional aging. Annu Rev Psychol, 61, 383–409. 10.1146/annurev.psych.093008.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten SR, Ford G, Ford S, & Hale TM (2014). Internet use and depression among retired older adults in the United States: a longitudinal analysis. J Gerontol B Psychol Sci Soc Sci, 69(5), 763–771. 10.1093/geronb/gbu018 [DOI] [PubMed] [Google Scholar]
- Dennis D, Radnitz C, & Wheaton MG (2021). A Perfect Storm? Health Anxiety, Contamination Fears, and COVID-19: Lessons Learned from Past Pandemics and Current Challenges. Int J Cogn Ther, 1–17. 10.1007/s41811-021-00109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge HH, Mattek NC, Austin D, Hayes TL, & Kaye JA (2012). In-home walking speeds and variability trajectories associated with mild cognitive impairment. Neurology, 78(24), 1946–1952. 10.1212/WNL.0b013e318259e1de [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feliciano L, Johanson KA, Okun ML, & Walden A (2022). Impacts of the Coronavirus Pandemic on the Emotional and Physical Health of Older Adults Compared with Younger Cohorts. Clin Gerontol, 45(1), 45–57. 10.1080/07317115.2021.1966561 [DOI] [PubMed] [Google Scholar]
- Fitzke RE, Wang J, Davis JP, & Pedersen ER (2021). Substance use, depression, and loneliness among American veterans during the COVID-19 pandemic. Am J Addict, 30(6), 552–559. 10.1111/ajad.13211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould CE, & Hantke NC (2020). Promoting Technology and Virtual Visits to Improve Older Adult Mental Health in the Face of COVID-19. Am J Geriatr Psychiatry, 28(8), 889–890. 10.1016/j.jagp.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoogendijk EO, Smit AP, van Dam C, Schuster NA, de Breij S, Holwerda TJ, Huisman M, Dent E, & Andrew MK (2020). Frailty Combined with Loneliness or Social Isolation: An Elevated Risk for Mortality in Later Life. J Am Geriatr Soc, 68(11), 2587–2593. 10.1111/jgs.16716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katerndahl DA, & Parchman M (2002). The ability of the stress process model to explain mental health outcomes. Compr Psychiatry, 43(5), 351–360. 10.1053/comp.2002.34626 [DOI] [PubMed] [Google Scholar]
- Kaye J, Mattek N, Dodge HH, Campbell I, Hayes T, Austin D, Hatt W, Wild K, Jimison H, & Pavel M (2014). Unobtrusive measurement of daily computer use to detect mild cognitive impairment. Alzheimers Dement, 10(1), 10–17. 10.1016/j.jalz.2013.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye JA, Maxwell SA, Mattek N, Hayes TL, Dodge H, Pavel M, Jimison HB, Wild K, Boise L, & Zitzelberger TA (2011). Intelligent Systems For Assessing Aging Changes: home-based, unobtrusive, and continuous assessment of aging. J Gerontol B Psychol Sci Soc Sci, 66 Suppl 1, i180–190. 10.1093/geronb/gbq095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Holt-Lunstad J, Newmark RL, Cenzer I, Smith AK, Covinsky KE, Escueta DP, Lee JM, & Perissinotto CM (2021). Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID-19 Shelter-in-Place Orders. J Am Geriatr Soc, 69(1), 20–29. 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krendl AC, & Perry BL (2021). The Impact of Sheltering in Place During the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being. J Gerontol B Psychol Sci Soc Sci, 76(2), e53–e58. 10.1093/geronb/gbaa110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrasseur A, Fortin-Bedard N, Lettre J, Raymond E, Bussieres EL, Lapierre N, Faieta J, Vincent C, Duchesne L, Ouellet MC, Gagnon E, Tourigny A, Lamontagne ME, & Routhier F (2021). Impact of the COVID-19 Pandemic on Older Adults: Rapid Review. JMIR Aging, 4(2), e26474. 10.2196/26474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leese MI, Bernstein JPK, Dorociak KE, Mattek N, Wu CY, Beattie Z, Dodge HH, Kaye J, & Hughes AM (2021). Older Adults’ Daily Activity and Mood Changes Detected During the COVID-19 Pandemic Using Remote Unobtrusive Monitoring Technologies. Innov Aging, 5(4), igab032. 10.1093/geroni/igab032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K-Y, & Zeger SL (1986). Longitudinal data analysis using generalized linear models. Biometrika, 73(1), 13–22. 10.1093/biomet/73.1.13 [DOI] [Google Scholar]
- Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, & Sutin AR (2020). The trajectory of loneliness in response to COVID-19. Am Psychol, 75(7), 897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menec VH, Newall NE, Mackenzie CS, Shooshtari S, & Nowicki S (2020). Examining social isolation and loneliness in combination in relation to social support and psychological distress using Canadian Longitudinal Study of Aging (CLSA) data. PLoS One, 15(3), e0230673. 10.1371/journal.pone.0230673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry R, Rosansky J, McGuire J, McDermott C, Jarvik L, & Group UC (2001). Social isolation predicts re-hospitalization in a group of older American veterans enrolled in the UPBEAT Program. Unified Psychogeriatric Biopsychosocial Evaluation and Treatment. Int J Geriatr Psychiatry, 16(10), 950–959. 10.1002/gps.447 [DOI] [PubMed] [Google Scholar]
- Na PJ, Straus E, Jack T, Norman SB, Southwick SM, & Pietrzak RH (2022). Loneliness in U.S. military veterans during the COVID-19 pandemic: A nationally representative, prospective cohort study. J Psychiatr Res, 151, 546–553. 10.1016/j.jpsychires.2022.05.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine. (2020). In Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. The National Academic Press. 10.17226/25663 [DOI] [PubMed] [Google Scholar]
- Perissinotto C, Holt-Lunstad J, Periyakoil VS, & Covinsky K (2019). A Practical Approach to Assessing and Mitigating Loneliness and Isolation in Older Adults. J Am Geriatr Soc, 67(4), 657–662. 10.1111/jgs.15746 [DOI] [PubMed] [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, & Covinsky KE (2012). Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med, 172(14), 1078–1083. 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shattuck SM, Kaba D, Zhou AN, & Polenick CA (2022). Social Contact, Emotional Support, and Anxiety during the COVID-19 Pandemic among Older Adults with Chronic Conditions. Clin Gerontol, 45(1), 36–44. 10.1080/07317115.2021.1957051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone LB, & Veksler AE (2022). Stop talking about it already! Co-ruminating and social media focused on COVID-19 was associated with heightened state anxiety, depressive symptoms, and perceived changes in health anxiety during Spring 2020. BMC Psychol, 10(1), 22. 10.1186/s40359-022-00734-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson G, Hill M, & Kiernan MD (2018). Loneliness and social isolation of military veterans: systematic narrative review. Occup Med (Lond), 68(9), 600–609. 10.1093/occmed/kqy160 [DOI] [PubMed] [Google Scholar]
- Wu CY, Mattek N, Wild K, Miller LM, Kaye JA, Silbert LC, & Dodge HH (2022). Can changes in social contact (frequency and mode) mitigate low mood before and during the COVID-19 pandemic? The I-CONECT project. J Am Geriatr Soc, 70(3), 669–676. 10.1111/jgs.17607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA (1988). Geriatric Depression Scale. Psychopharmacol Bull, 24(4), 709–711. https://www.ncbi.nlm.nih.gov/pubmed/3249773 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This data was presented at the 2020 conference of the Gerontological Society of America (GSA).


