Abstract
Due to the increased prevalence of obesity and disparity experienced by youth with intellectual disabilities, efforts to synthesize existing knowledge of interventions to attenuate obesity within this marginalized population is imperative. The purpose of this investigation is to systematically analyze interventions targeting anthropometric changes in youth with intellectual disabilities. A search of Cumulative Index of Nursing and Allied Health Literature, Educational Resources Information Center, Medical Literature Analysis and Retrieval System Online, and Psychological Information Database was conducted for the time frame of January 2006 to October 2016. Data extraction resulted in a total of 10 interventions that met inclusion criteria. Included studies mainly comprised participants having mild-to-moderate intellectual disability with diverse comorbidities. Five studies indicated significant positive outcomes in at least one anthropometric measure. The majority of programs utilized physical activity targeting individual-level change as the primary intervention modality. Weaknesses of the reviewed studies and inconclusive evidence indicate the need for additional research to gauge the effectiveness of interventions to treat obesity among youth with intellectual disabilities.
Keywords: intellectual disability, youth, obesity, intervention, systematic review
Introduction
A significant number of children are overweight or obese in the United States, with rates that have doubled for children and quadrupled for adolescents during the past three decades (Ogden et al., 2014). Deleterious effects associated with this condition include increased cardiovascular risk, asthma, type-2 diabetes mellitus, musculoskeletal disorders, and psychosocial consequences such as stigma and lowered self-esteem (Gundersen et al., 2011; McCrindle, 2015; Nguyen et al., 2011; Visness et al., 2010). Onset of obesity in childhood is particularly concerning as reported measures have indicated an alarming propensity for children to maintain obese status into adulthood due to the retention of obesity-related behaviors (Craigie et al., 2011; Freedman et al., 2005).
An intellectual disability (ID) is defined as a disability with limitation in the two areas of intellectual functioning and adaptive behavior (Schalock et al., 2010). Intellectual functioning, or intelligence, refers to mental capacity and is typically measured through an intelligence quotient test, with scores less than 70 indicating intellectual functioning limitations. Adaptive behavior is comprehensive of conceptual, social, and practical skills including language and literacy, interpersonal or occupational skills, and personal care. In 2002, a report by the Surgeon General explicated disparities in health care and outcomes experienced by individuals with ID and advocated for increased research and implementation of health promotion programs within this population (US Public Health Service, 2002). Literature has indicated that adults with ID may experience increased rates of adverse health outcomes and shorter life expectancy than the general population (Haveman et al., 2010; Havercamp et al., 2004). Children with developmental disabilities, which are inclusive of ID, have an obesity prevalence equal to or higher than peers without disability (Bandini et al., 2005). Recent literature has confirmed the high prevalence of obesity among youth with ID (Rimmer et al., 2010), with rates in children as high as 37% (Must et al., 2014). Due to the propensity of overweight or obesity status in childhood to persist into adulthood and result in increased risk for chronic conditions, it is likely these same consequences and trends will result in youth with ID (Must and Strauss, 1999). Due to the increased prevalence of obesity, adverse health outcomes, and disparity experienced by youth with ID, prevention efforts to attenuate obesity and obesity-related conditions within this marginalized population is an imperative public health issue. Health promotion efforts targeting this population have implications for improved interdependent living, health status, and quality of life. Research addressing primary prevention of obesity in youth with ID is in its infancy (Must et al., 2014) necessitating efforts to synthesize existing knowledge to develop optimal recommendations for future research and practice.
Previous reviews have extensively examined the effects of interventions designed to improve anthropometric outcomes in the adult ID population and assert success in reducing weight and improving body composition through behavior modification that includes reducing energy intake, increasing energy expenditure, or fostering healthy skills (Casey and Rasmussen, 2013; Heller et al., 2011; Spanos et al., 2013). Evidence of effective interventions targeting anthropometric outcomes in youth with ID is limited due to reviews that are dated (Fox et al., 1982; Rotatori et al., 1981), do not exclusively examine interventions targeting youth with ID (Casey and Rasmussen, 2013; Rotatori et al., 1981), or only examined the effects of exercise training on body fat (Casey and Rasmussen, 2013). A more recent review by Maiäno et al. (2014) examined lifestyle interventions targeting changes in body weight and composition among youth with ID and concluded that interventions utilizing diet, physical activity (PA), and health education modalities may be beneficial for positive anthropometric change in this population. However, the authors also caution their findings as preliminary and indicative of a need for further research including the assessment of lifestyle intervention effects on secondary outcomes such as physical fitness, mental health, and maladaptive behaviors. Due to the inconclusiveness of past reviews, further examination of interventions targeting body weight and composition in youth with ID is warranted and would benefit health researchers and practitioners working with this population. Thus, the purpose of this review is to build on previous literature by examining the effectiveness of obesity interventions for youth with ID focusing on anthropometric measures (weight, body mass index (BMI), waist circumference (WC), and body fat) and secondary health-related outcomes (physical/mental health and physical/cardiovascular fitness).
Methods
Information sources and eligibility
A review of the literature utilizing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria for reporting (Moher et al., 2009) was conducted to systematically analyze interventions targeting anthropometric changes in youth with ID. Studies of interest were located utilizing keywords targeting type of disability, age group, and intervention. The search protocol utilized Boolean search logic with the string (ID OR mental retardation OR learning disability OR developmental disability OR learning disabilities) AND obesity AND (children OR adolescents OR youth OR child OR teenager) AND intervention. Indexes searched included the Cumulative Index of Nursing and Allied Health Literature (CINAHL), Educational Resources Information Center (ERIC), Medical Literature Analysis and Retrieval System Online (MEDLINE), and Psychological Information Database (PsycINFO). Searches were delimited a priori to (1) peer-reviewed articles, (2) studies published between January 2006 and October 2016, and (3) studies in the English language. Inclusion criteria for articles were (1) interventions with (2) outcome measures of changes in anthropometric measures (weight, BMI, body fat, and WC) of (3) any quantitative study design where (4) sampled participants had a mean age less than 18 years and (5) presented with an ID. Exclusion criteria were (1) study populations with a mean over the age of 18, (2) interventions using surgical, medical, or pharmacological treatments, (3) case studies, (4) lack of anthropometric outcomes, (5) studies published prior to 2006, (6) in a language other than English, and (7) review or theoretical, unpublished, or non-peer-reviewed articles.
Search strategy
The review encompassed three phases. Phase I utilized Boolean search logic to extract initial titles and abstracts from included databases. Phase II protocol consisted of list refinement through examination of title and abstract resulting in the removal of duplicates, review articles, studies of the wrong design, and articles irrelevant to the research question. In phase III, authors examined the full text of remaining articles to ensure conformity to inclusion criteria. Additionally, to further the comprehensiveness of the review, the authors performed a reference search to identify articles that may not have populated during the initial search. Information was extracted from full-text articles utilizing a data collection sheet developed using the 2011 “Cochrane Handbook for Systematic Reviews of Interventions” (Higgins and Green, 2011). One author extracted information from relevant studies while the second author reviewed extracted information. Study components extracted included author, country of origin, participants, comorbidities, study design and intervention, duration, outcome, and intervention effects.
The initial phase I search utilizing Boolean logic generated 99 articles from CINAHL , ERIC , MEDLINE , and PsycINFO . Phase II refinement through examination of study titles and abstracts resulted in the removal of duplicates , review articles , studies of the wrong design , adult populations , and articles irrelevant to the research question . Phase III author examination of the full text of remaining articles resulted in the exclusion of articles that did not target obesity , explicitly target an ID population , and did not include quantitative anthropometric outcome measures . Review of references from phase III articles resulted in the addition of one article to the inclusion total. Data extraction resulted in 10 unique studies (Figure 1) that satisfied inclusion and exclusion criteria.
Figure 1.
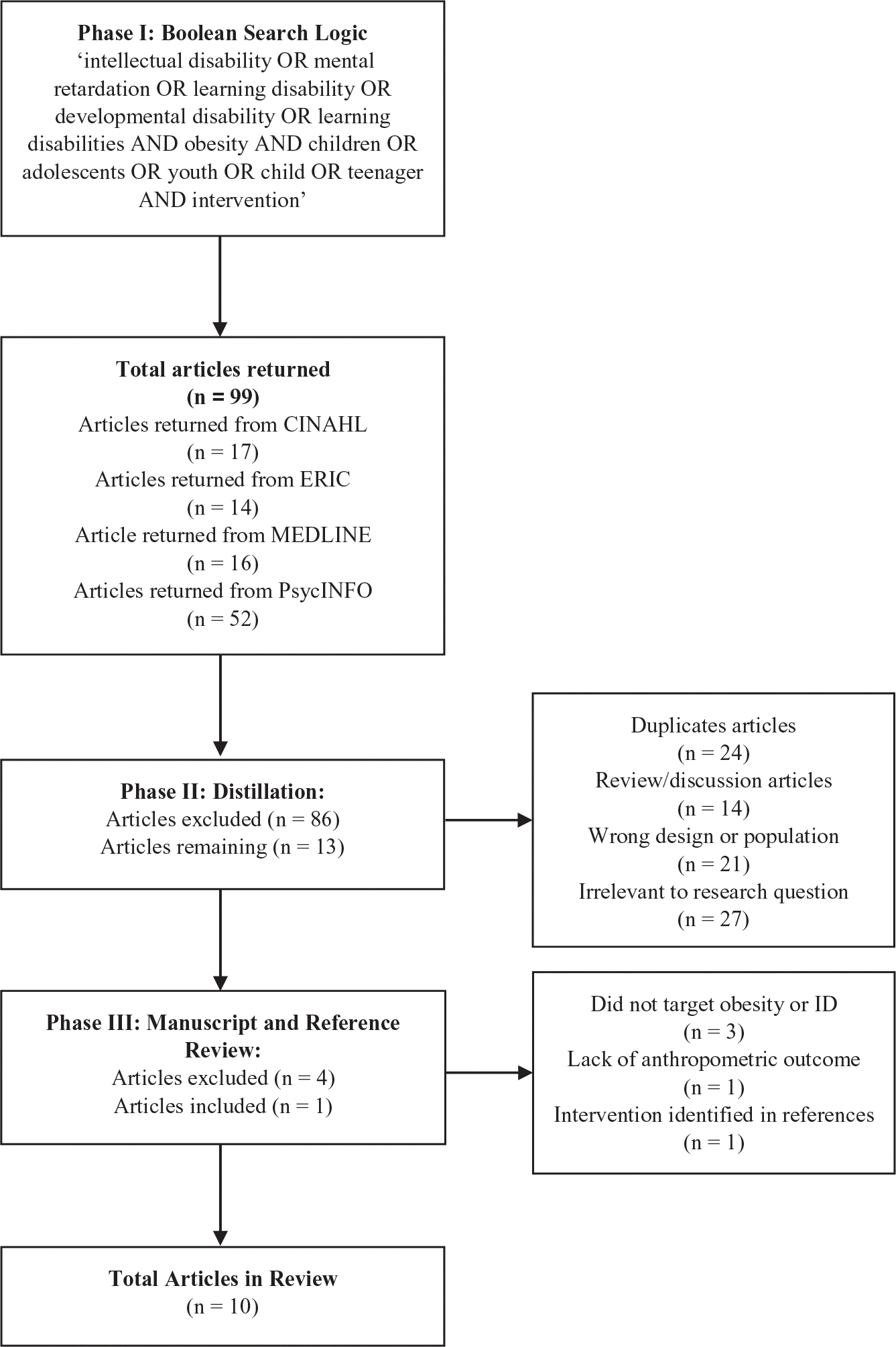
Flowchart depicting the data extraction process.
Methodological quality assessment of review studies
As suggested by the PRISMA explanation and evaluation statement (Liberati et al., 2009), a methodological quality assessment or risk of bias for each study was conducted utilizing a modified augmented Jadad scale (Sarris and Byrne, 2011). The original Jadad scale was based on the quality factors of randomization, blinding, and reported withdrawals, while the modified version also assesses methodological factors such as utilization of a control, data reporting, exclusion criteria, and intervention used to provide a quality total out of 10. Evaluation of studies was performed by one author and reviewed by the second author for agreement. Studies were not excluded on the basis of their bias scores but are presented to empirically rate study quality.
Results
Table 1 summarizes primary data extraction components for each study. Study components included author, country of origin, participants, comorbidities, study design and intervention, duration, outcome, and intervention effects. Results of the quality assessment for each included study utilizing the modified Jadad scale are presented in Figure 2 and arranged in ascending order by year of publication. The mean score for all the studies was 4.6 , median of 4.25, with scores ranging from 2 to 7.
Table 1.
Summary of obesity interventions targeting youth with intellectual disabilities conducted between January 2006 and October 2016 (n = 10).
| Author/year/country | Participants | Study design//intervention strategy/groups | Duration/intervention activities | Outcome | Intervention effects |
|---|---|---|---|---|---|
|
| |||||
|
Ordonez et al. (2006) Spain |
ntotal = 22 Age: 16.2 ± 1 years ID level: mild Comorbidity: DS (n = 22) |
Design: Pre and posttest Techniques: PA Groups: Tx |
Intervention: 12 weeks Follow-up: none Description: water and land aerobic exercise Session length: (a) 30 min (weeks: 1–2), (b) 45 min (weeks: 3–4), and (c) 60 min (weeks: 5–12) Frequency: 3 times/week |
Body weight and composition: weight and fat mass (kg and %) Health related: NM |
• Significant reduction in weight and fat mass (kg and %) from baseline |
|
Ozmen et al. (2007) Turkey |
ntotal = 30 Age: 8–15 years ID level: mild to moderate Comorbidity: NR |
Design: RCT Techniques: PA Groups: (1) Tx, PA 3 times/week (n = 16) and (2) Cnt (n = 14) |
Intervention: 10 weeks Follow-up: none Description: walking, interval training, and recreational activity Session length: 60 min Frequency: 3 times/week (Tx); None (Cnt) |
Body weight and composition: Fat mass (%) Health related: physical fitness (20-MST) |
• No change in percent body fat in Tx or Cnt from baselinelncrease in 20-MST for Tx versus Cnt |
|
Elmahgoub et al. (2009) Belgium |
ntotal 30 Age: 14–22 years ID level: mild to moderate Comorbidity: FXS (n = 16) and ASD (n = 14) |
Design: RCT Techniques: PA Groups: (1) Tx, PA 3 times/week (n = 15) and (2) Cnt (n = 15) |
Intervention: 10 weeks Follow-up: none Description: strength and endurance training Session length: 50 min Frequency of sessions: 3 times/ week |
Body weight and composition: weight, BMI, WC, and fat mass (kg) Health related: physical and cardiovascular fitness and health |
• Decrease among Tx in weight, BMI, WC, and fat mass; no change in Cnt • Increase in fat-free mass in Tx • Increase in PW, 6MWD, HG, MFR, MS- UL, MS-LL, and sit to stand in Tx • Improvement in Chi, Tri, HDL, and LDL in Tx |
|
Casey et al. (2010) Canada |
ntotal = 8 Age: 9–17 years ID level: mild to moderate Comorbidity: DS (n = 3) and ASD (n = 1) |
Design: Pre and posttest Techniques: PA Groups: Tx |
Intervention: 16 weeks Follow-up: none Description: swim and dry land training Session length: 60 min Frequency of sessions: 3 times/week |
Body weight and composition: fat mass (%) Health related: NM |
• Increase in fat mass (%) from baseline |
|
Elmahgoub et al. (2011) Belgium |
ntotal = 45 Age: 14–22 years ID level: mild to moderate Comorbidity:FXS (n = 16), FAS (n = 2), PWi (n = 2), HCP (n = 3), PDD (n = 5), SS (n = 2), and MD1 (n = 3) |
Design: Quasi Techniques: PA Groups: (1) Tx1 2 times/week (n = 15), (2) Tx2 3 times/week (n = 15), and (3) Cnt (n = 15) |
Intervention: 10 (Tx2) to 15 (Tx1) weeks Follow-up: none Description: strength and endurance training Session length: 50 min Frequency of sessions: 2 times/week (Tx2) and 3 times/ week (Tx1) |
Body weight and composition: weight, BMI, WC, and fat mass (kg) Health related: physical and cardiovascular fitness and health |
• Decrease in weight, BMI, EC, and fat mass (kg) in Tx1; nonsignificant decreases in Tx2; no change in Cnt • Increase in PW, 6MWD, HG, MFR, MS- UL, MS-LL, and sit to stand in Tx1 versus Cnt • Improvement in Chi, HDL, and LDL in Txi versus Cnt • Significant increase in MS-LL in Tx1 versus Tx2 |
|
Gonzâlez- Agüero et al. (2011) Spain |
ntotal = 26 Age: 10–19 years ID level: NM Comorbidity: DS (n = 26) |
Design: RCT Techniques: PA Groups: (1) Tx (n = 13) and (2) Cnt (n = 13) |
Intervention: 21 weeks Follow-up: none Description: conditioning and plyometric training Session length: 25 min Frequency of sessions: 2 times/week |
Body weight and composition: weight, BMI, and fat mass (kg and %) Health related: NM |
• Increase in weight, BMI, and fat mass (kg and %) from baseline in Tx |
|
Hinckson et al. (2013) New Zealand |
ntotal = 17 Age: 7–21 years ID level: mild to moderate Comorbidity: DS (n = 2), ASD (n = 7), and GDD (n = 4) |
Design: Pre and posttest Techniques: PA and health education Groups: Tx |
Intervention: 10 weeks Follow-up: 24 weeks Description: (1) PA, (2) healthy eating, and (3) motivational skills Session length: (1) 120 min and (2) and (3) 60 min Frequency of sessions: 2 times/week |
Body weight and composition: BMI and WC Health related: physical fitness and healthy lifestyle (nutrition, PA, and screen time) |
• No significant difference in BMI, WC, PF, PA, or SB from baseline to posttest and follow-up • Only 6MWD indicated a possibly positive result at follow-up • Decrease in reported consumption of chocolate and confectionary from baseline to follow-up |
|
Wallen et al. (2013) Sweden |
ntotal = 14 Age: 16.6–18.8 years ID level: mild to mod Comorbidity: DS (n = 4) |
Design: Quasi Techniques: PA, nutrition, and health education Groups: (1) Tx and (2) historical comparison |
Intervention: 2 years Follow-up: none Description: (1) daily PA, (2) nutrition policy, (3) low- cost healthy food, and (4) monthly health bulletin and annual 3-day camp to practice healthy lifestyle patterns Session length: (1) 60/30 min Frequency of sessions: (1) 60 min 3 days/week; 30 min 2 days/ week, and (4) monthly and annually |
Body weight and composition: BMI, WC, and fat mass (%) Health related: cardiovascular health and VO2max |
• No significant difference in Tx for BMI, WC, and body fat (%) from baseline • Decrease in DBP in Tx • Decrease in mean body fat (%) in Tx than historical comparison |
|
Salaun et al. (2014) France |
ntotal = 23 Age: 6–18 years ID level: mild Comorbidity: NR |
Design:Pre and posttest Techniques: PA Groups:Tx |
Intervention: 9 months Follow-up: none Description:Aerobic PA and strength training Session length: (a) 30 min (weeks 1–10), (b) 30 and 50 min (weeks 11–20), and (c) 45 and 60 min (weeks 21–30) Frequency of sessions:2 times/week |
Body weight and composition: BMI, WC, and fat mass (%) Health related: self-perception measures |
• No significant difference in Tx for BMI, WC, and body fat (%) from baseline • Decrease in Tx WC and percent fat from baseline • Decrease in body image dissatisfaction following intervention |
|
Ptomey et al. (2015) USA |
ntotal = 20 Age: 11–18 years ID level: mild to moderate Comorbidity: ASD (n = 9), DS (n = 8), and other (n = 3) |
Design: RCT Techniques: diet and health education Groups: (1) Tx (n = 10) and (2) cnt (n = 10) |
Intervention: 8 weeks Follow-up: none Description: (1) portion controlled meals with video chat education sessions and (2) education sessions and instructed to consume nutritionally balanced diet Session length: 90-min initial, 30-min subsequent Frequency of sessions: weekly |
Body weight and composition: BMI, and WC Health related:PA, energy intake, and diet quality |
• Reduction in weight in Tx; no difference between groups • Decrease in sedentary activity time, caloric intake, and empty calorie consumption in Tx • Increased reduction of energy intake in Tx as versus Cnt |
Note. NM: not mentioned; PA: physical activity; 20-MST: 20-m shuttle-run test; Cnt: control group; FXS: fragile-X syndrome; ASD: autism spectrum disorder; RCT: randomized control trial; BMI: body mass index; WC: waist circumference; PW: peak power; 6MWD: 6-min walk distance; HG: hand grip; MFR: muscle fatigue resistance; MS-UL: maximal strength upper limbs; MS-LL: maximal strength lower limbs; Tx: treatment group; Chl: total cholesterol; Tri: triglycerides; HDL: high-density lipoprotein; LDL: low-density lipoprotein; DS: down syndrome; FAS: fetal alcohol syndrome; HCP: hydrocephalus; PDD: pervasive development disorder; PWi: Prader–Willi syndrome; SS: Sotos syndrome; MD1: myotonic dystrophy 1; MWD: minute walk distance; DBP: diastolic blood pressure; GDD: global developmental delay; ID: intellectual disability; NR: not reported; PF: physical fitness; SD: sedentary behavior; kg: kilograms; η2: eta-squared.
Figure 2.
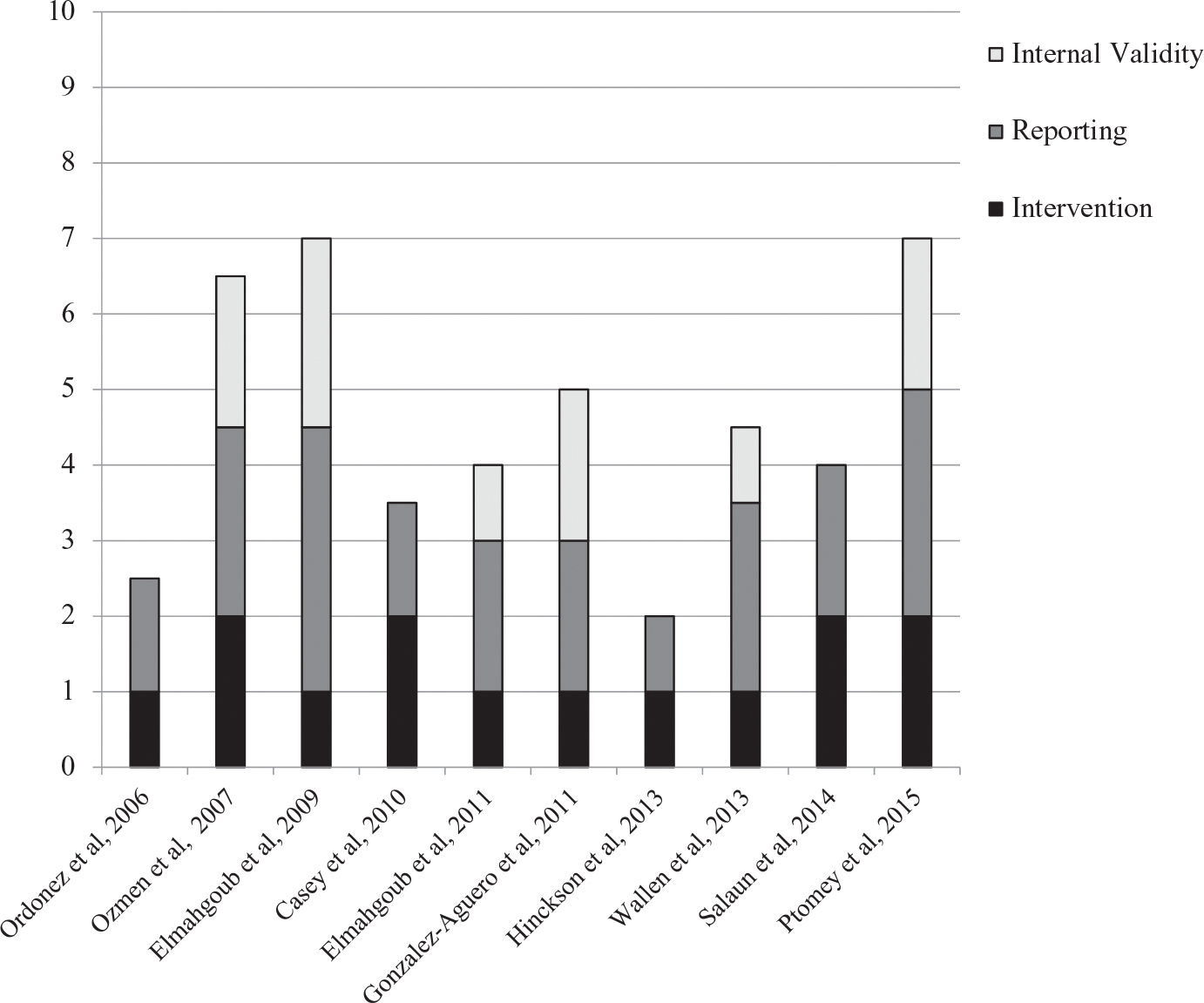
Bar chart of the methodological quality of the reviewed studies.
Ordonez et al. (2006) employed a 12-week PA program that incorporated land and aquatic exercise. A total of 22 participants with Down syndrome and a mean age of 16.2 (± 1) were included. Program dosage consisted of three sessions per week with intensity prescribed and measured by investigators on the basis of heart rate. The duration of exercise sessions scaled from weeks 1 and 2 (30 min), 3 and 4 (45 min), and 5 through 12 (60 min). Specific exercises engaged in by the participants as well as the structure of the PA sessions were not reported. The intervention utilized a pre/post evaluation protocol to measure the primary outcomes of body weight and fat mass. At posttest, intervention effects indicated a reduction in weight and fat mass, measured in kilograms (kg) and total percent, from baseline .
Ozmen et al. (2007) implemented a 10-week PA program utilizing a single-blinded randomized control trial (RCT) protocol. Participants included 30 youth with an ID level classification of mild to moderate between 8 years and 15 years. Participants were randomly assigned to treatment (Tx) and control (Cnt) arms in which the Tx participated in PA for a duration of 60 min, three times per week while the Cnt arm received no PA other than habitual exercise. The Tx participated in intervention activities with the designated protocol that included 10 min of warm-up exercises, 20 min of interval training, 25 min of recreational activity, followed by a 5-min cooldown. Interval training in the initial 4 weeks of the intervention employed four sets of three repetitions and was increased to four sets of four repetitions in weeks five to eight and four sets of five repetitions during the final 2 weeks. The primary body composition outcome measured was fat mass as a percent, with secondary health-related outcomes including a measure of fitness (20-m shuttle run). Following the intervention, analysis indicated no significant change in percent body fat in either arm from baseline; however, a significant increase in 20-m shuttle run performance was reported for Tx versus Cnt arms.
Elmahgoub et al.’s (2009) intervention employed a strength and endurance training PA program with participants selected utilizing an RCT design. Participants from a pool of 40 homogenous candidates were randomly assigned to the Tx , with a matching Cnt arm selected at random from the remaining 25 candidates. The final sample included 30 participants between 14 years and 22 years and an ID level classification of mild to moderate. The Tx arm participated in a strength and endurance program three times per week, with each session lasting 50 min. Session components included a warm-up (5 min), cycling (10 min), strength training consisting of biceps and triceps exercises (10 min), stepping (10 min), strength training of the quadriceps/hamstrings (10 min), followed by a 5-min cool down period. Aerobic training components of the programs used individually prescribed targets of 60% heart rate reserve and was increased to 70% after the completion of 10 sessions and 75% after 20 sessions. Strength exercises employed stack weight equipment for three sets of 10 repetitions between 60% and 80% of one-repetition maximum (1RM). The primary anthropometric outcome measures included weight, BMI, WC, and fat mass. Secondary health-related outcomes including indices of physical and cardiovascular fitness such as peak power, peak heart rate, peak VO2, relative peak, 6-min walk distance (6MWD), hand grip strength, muscle fatigue resistance (MFR), maximal strength for upper and maximal strength for lower limbs (MS-LL), sit to stand, total cholesterol (Chl), triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL). Results of the intervention indicated the Tx arm achieved a significant decrease in weight, BMI, WC, and fat mass from baseline, while the Cnt arm indicated no change in primary outcome measures. Significant improvements in performance and cardiovascular measures were observed in the Tx arm for peak power, 6MWD, MFR, MS-UL, MS-LL, sit to stand, Chl, triglycerides, HDL, and LDL at posttest .
Casey et al. (2010) administered a 16-week swim training program to eight participants with a mild or moderate classification between 9 years and 17 years. Program dosage consisted of three sessions per week for a duration of 60 min per session. Session PA components consisted of performing swim strokes and exercises using a flutter board device at 60–80% of participant theoretical maximum heart rate. Additionally, participants engaged in dry land training that included stroke instruction, stretching, sit-ups, aerobic tasks, or velocity training for a total of 10 min per session. A pre/post evaluation design was utilized to assess the primary anthropometric outcome measure of body fat percentage. Following the intervention, researchers reported a significant increase in fat mass from baseline.
Elmahgoub et al. (2011) expanded on their previous strength and endurance PA program by including two Tx arms in addition to a Cnt arm. A total of 45 participants with an age range of 14–22 years with mild to moderate ID were separated into a primary (Tx1) treatment , secondary (Tx2) treatment , and Cnt . The Tx1 arm participated in the program for a duration of 15 weeks with a frequency of two 50-min sessions per week, while Tx2 engaged in the program for 10 weeks and a frequency of three 50-min sessions per week. The Cnt arm received no training as a result of the program. Similar to the previous program, participants engaged in a warm-up (5 min), cycling (10 min), strength training of the biceps and triceps (10 min), stepping (10 min), strength training of the quadriceps/hamstrings (10 min), followed by a 5-min cooldown. Exercise intensity was scaled throughout the program from 60% to 75% of peak heart rate (cycling/stepping) and 60% to 80% of 1RM (upper/lower limb exercises), with maximum intensity achieved in 10 weeks for Tx2 and 15 weeks for Tx1. The primary anthropometric outcome measures included weight, BMI, WC, and fat mass. Secondary health-related outcomes including indices of physical and cardiovascular fitness such as peak power, peak heart rate, peak VO2, relative peak, 6MWD, hand grip strength, MFR, MS-UL, MS-LL, sit to stand, total cholesterol, HDL, and LDL. At posttest, the Tx1 and Tx2 arms indicated decreases in weight, BMI, WC, and fat mass; however, only the decreases in Tx1 were significant compared to the Cnt. The Cnt remained steady and did not have any significant changes in primary outcome measures. Tx1 indicated significantly improved measures of peak power, 6MWD, peak heart rate, MFR, MS-UL, MS-LL, sit to stand, Chl, HDL, and LDL as compared to the Cnt .
González-Agüero et al. (2011) implemented a 21-week conditioning and plyometric PA program with an RCT design. A total of 26 participants between 10 years and 19 years at baseline were recruited from schools and institutions and randomly assigned to the Tx and Cnt arms. Participants in the Tx arm received the program at a frequency of two times per week for a duration of 25 min per session, while the Cnt received no training. Each session consisted of a 5-min warmup and cooldown as well as 10–15 min of prescribed exercise. The training consisted primarily of exercise circuits comprising jumps, wall press-ups, elastic fitness bands, and adapted medicine balls. Participants were separated into four intensity groups based on capacity and could increase to higher groups after showing adequate facility. All participants followed the same exercise schedule of one set of 10 repetitions (weeks 1–5), two sets of 10 repetitions (weeks 6–10), two sets of 15 repetitions (weeks 11–15), and two sets of 20 repetitions (weeks 16–21). Primary anthropometric outcome measures included weight, BMI, and fat mass in kilograms and percent. At posttest, Tx results indicated an increase in fat mass , weight, and BMI.
Hinckson et al. (2013) implemented a 10-week PA, healthy eating, and motivational skills program. Program participants included 17 youth with mild to moderate ID between 7 years and 21 years. The program consisted of 18 PA sessions, 10 nutrition, and eight motivational segments distributed over the 10-week period at a frequency of twice per week. Sessions included a 1 h family PA component followed by an active session with youth while parents attended a nutrition or motivation segment for an additional hour. Nutrition and motivation segments encompassed topics including food portion size and labeling, eating out, supermarket tours, modeling, triggers, goal-setting, and incentives. A pre–post evaluation design was utilized to assess primary anthropometric outcomes of WC and BMI as well as health-related measures of physical fitness (6-min walk test) and lifestyle (nutrition, PA, and screen time) from baseline and 24 weeks post program. At posttest and 24-week follow-up, no significant differences were found for BMI, WC, physical fitness, PA, or screen time as a result of program participation. At 24-week follow-up, a possibly positive result was observed in 6-min walk test among participants, while parents also reported participants consuming less confectionary and chocolates per week.
Wallen et al. (2013) assessed the effects of a 2-year, multicomponent school-based intervention that incorporated PA, nutrition, health education, and policy. Participants were 14 first-year upper secondary school students with a mean age of 17.8 years and an ID classification from mild to moderate. The Tx group was compared to a historical comparison of fourth-year students with ID who had participated in a previous study. A primary component of the intervention was a school-adopted health policy which incorporated restrictions on less nutritious food and beverage options as well as school meals meeting specific cost and nutrition standards, and the hiring of a dedicated health educator. Additional intervention components included daily PA for 60-min, 3 days a week, and 30-min for the remaining 2 days. School lunches were served on a uniquely designed plate which was divided into three distinct sections that corresponded to a specific food group to assist students in choosing appropriately nutritious options. Health education components of the intervention included a monthly health bulletin and an annual 3–4 day camp to develop healthy lifestyle patterns. The primary anthropometric outcomes measured included BMI, WC, and fat mass. Additional health-related outcomes included indices of cardiovascular health and aerobic capacity such as systolic blood pressure (SBP), diastolic blood pressure (DBP), Chl, Tri, and VO2max. Following the 2-year period, there was a positive trend in body fat from baseline but no significant differences at the group level were observed for any anthropometric variable. When compared to the historical comparison, a significant decrease in mean body fat percent and BMI was observed. Results of secondary outcomes indicated positive trends in cardiometabolic variables (SBP, DBP, Tri, and Chl) but only DBP was significant at the group level in Tx arm.
Salaun et al. (2014) implemented a 9-month PA program utilizing a combination of aerobic and strength training exercises. A total of 23 participants between 6 years and 18 years with an ID classification of mild were included in the study. The implementation duration totaled 30 weeks with a session frequency of twice per week. The first 10 weeks of the program included two, 30-min continuous aerobic sessions to a prescribed intensity of 30–40% VO2max. In weeks 11–20, participants continued with a singular aerobic session for a duration of 30 min in addition to a prolonged session of 50 min with an increased intensity of 35–45% VO2max. Weeks 21–30 increased the initial session length to 45 min with a second weekly session of 1 h with an intensity goal of achieving shortness of breath in participants. Primary anthropometric outcome measures included BMI, WC, and percent fat mass. Health-related outcomes include measurements of physical self-perception such as positive illusory bias of sport competence, obesity awareness, and body image perception. Following the intervention, decreases were observed for anthropometric outcomes from baseline; however, only WC and percent body fat were significant. Similarly, positive effects were observed for health-related outcomes, but only body image dissatisfaction was significant from baseline to posttest .
Ptomey et al. (2015) implemented an 8-week technology-based diet and education program with an RCT design. A total of 20 participants between 11 years and 18 years with mild to moderate ID classification were randomly separated in Tx and Cnt arms. Participants in the Tx arm received prepackaged portion-controlled meals (PCMs) that contained portioned, low-calorie, high-nutritional value meals for consumption as well as shake beverages. Consumption of noncaloric beverage was permitted and participants were instructed to consume two PCMs and two shakes per day. Participants in the Cnt arm received nutrition education and were instructed to consume a nutritionally balanced diet. All participants were given a tablet computer in which they logged food and beverage consumption as well as PA. Additionally, participants and parents engaged in weekly 30-min sessions with a registered dietitian nutritionist (RDN) over video chat. Sessions addressed lifestyle modifications and topics including social support, self-monitoring, PA, and self-efficacy. Additionally, the RDN reviewed the previous week’s data and assisted with goal-setting while providing additional support. The primary anthropometric measures assessed were weight, BMI, and WC. Additional health-related measures include PA, energy intake, and diet quality. At posttest, there was an improvement in BMI and WC as well as a significant reduction in weight for the Tx arm. No significant differences were observed when comparing anthropometric outcomes between Tx and Cnt arms. Results of health-related outcomes indicated a positive increase in PA , decrease in caloric intake , and decrease in empty calorie consumption from baseline in the Tx arm. The decrease in caloric intake in the Tx arm was significantly lower than the Cnt .
Intervention design
All studies meeting inclusion criteria utilized some form of quantitative design including four RCT (Elmahgoub et al., 2009; González-Agüero et al., 2011; Ozmen et al., 2007; Ptomey et al., 2015), two quasi-experimental (Elmahgoub et al., 2011; Wallén et al., 2013), and four pre/post (Casey et al., 2010; Hinckson et al., 2013; Ordonez et al., 2006; Salaun et al., 2014) designs. Additionally, the majority of reviewed studies included health-related outcome measures in addition to anthropometric or body composition measures (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Hinckson et al., 2013; Ozmen et al., 2007; Ptomey et al., 2015; Salaun et al., 2014; Wallén et al., 2013). Of the 10 included studies, 9 provided ID level classifications of intervention participants with ID levels of mild or moderate (Casey et al., 2010; Elmahgoub et al., 2009; Elmahgoub et al., 2011; Hinckson et al., 2013; Ordonez et al., 2006; Ozmen et al., 2007; Ptomey et al., 2015; Salaun et al., 2014; Wallén et al., 2013). Additionally, none of the reviewed articles explicitly stated utilization of a health behavior or education theoretical framework.
Intervention implementation
Of the reviewed studies, seven interventions (Casey et al., 2010; Elmahgoub et al., 2009; Elmahgoub et al., 2011; González-Agüero et al., 2011; Ordonez et al., 2006; Ozmen et al., 2007; Salaun et al., 2014) incorporated PA as the singular strategy for obesity prevention and targeted the participants with ID as the sole agents of change. Less commonly utilized strategies included health education (Hinckson et al., 2013; Ptomey et al., 2015; Wallén et al., 2013) and nutrition (Ptomey et al., 2015; Wallén et al., 2013) components and the inclusion of interpersonal or community-level targets of changes such as families (Hinckson et al., 2013; Ptomey et al., 2015) or the school environment (Wallén et al., 2013). The combined total of the 10 studies was 235 participants across groups ranging from 8 to 45 participants. Intervention duration ranged from 8 weeks to 2 years. Study durations included five interventions lasting 8–12 weeks (Elmahgoub et al., 2009; Hinckson et al., 2013; Ordonez et al., 2006; Ozmen et al., 2007; Ptomey et al., 2015), three interventions lasting 3 to 6 months (Casey et al., 2010; Elmahgoub et al., 2011; González-Agüero et al., 2011), one intervention lasting 9 months (Salaun et al., 2014), and one intervention lasting 2 years (Wallén et al., 2013). Of the reviewed interventions, seven indicated some element of process evaluation (Casey et al., 2010; Elmahgoub et al., 2009; González-Agüero et al., 2011; Hinckson et al., 2013; Ordonez et al., 2006; Ozmen et al., 2007; Ptomey et al., 2015). Fidelity to delivery protocols was minimal within these studies, primarily monitoring exercise intensity (Casey et al., 2010; Elmahgoub et al., 2009; Ordonez et al., 2006; Ozmen et al., 2007), participant component adherence through logs (Ptomey et al., 2015), participant attendance (González-Agüero et al., 2011), program quality through parental feedback (Hinckson et al., 2013), and monitoring of study protocol (Casey et al., 2010). Only one reviewed intervention incorporated a technology component to enhance participant learning (Ptomey et al., 2015).
Intervention evaluation
Interventions assessed body composition measures utilizing similar anthropometric outcomes. Primary anthropometric outcome measures included BMI (Elmahgoub et al., 2009; Elmahgoub et al., 2011; González-Agüero et al., 2011; Hinckson et al., 2013; Ptomey et al., 2015; Salaun et al., 2014; Wallén et al., 2013), fat mass (Casey et al., 2010; Elmahgoub et al., 2009; Elmahgoub et al., 2011; González-Agüero et al., 2011; Ordonez et al., 2006; Ozmen et al., 2007; Salaun et al., 2014; Wallén et al., 2013), weight (Elmahgoub et al., 2011; Elmahgoub et al., 2009; González-Agüero et al., 2011; Ordonez et al., 2006; Ptomey et al., 2015), and WC (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Hinckson et al., 2013; Ptomey et al., 2015; Salaun et al., 2014; Wallén et al., 2013). Studies with health-related outcome measures assessed physical or cardiovascular health and fitness (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Hinckson et al., 2013; Ozmen et al., 2007; Wallén et al., 2013), PA (Ptomey et al., 2015), nutrition or dietary measures (Hinckson et al., 2013; Ptomey et al., 2015), and self-perception measures (Salaun et al., 2014). Of all the included articles, only one included a follow-up evaluation, which took place 24 weeks after the cessation of the intervention (Hinckson et al., 2013). Article review indicated that five studies reported significant, positive changes in at least one anthropometric outcome variable (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Ordonez et al., 2006; Ptomey et al., 2015; Salaun et al., 2014), whereas five reported negative or insignificant changes (Casey et al., 2010; González-Agüero et al., 2011; Hinckson et al., 2013; Ozmen et al., 2007; Wallén et al., 2013). Of reviewed studies, only one included medication in participant characteristics (Hinckson et al., 2013) or included ID classification as a covariate during data analysis (Ptomey et al., 2015).
Discussion
The purpose of this investigation was to systematically analyze interventions targeting anthropometric changes in youth with ID conducted between 2006 and 2016. Examination of these interventions included assessing the effectiveness to promote positive change in body weight and composition as well as in secondary health-related outcomes. Overall, findings from this review indicate that interventions aimed at youth with ID have the propensity to foster positive anthropometric change by reducing fat mass (Elmahgoub et al., 2011; Ordonez et al., 2006; Salaun et al., 2014), BMI (Elmahgoub et al., 2009; Elmahgoub et al., 2011), WC (Elmahgoub et al., 2009; Salaun et al., 2014), and weight (Elmahgoub et al., 2009; Ordonez et al., 2006; Ptomey et al., 2015). Positive improvements to these anthropometric outcomes through behavior and lifestyle interventions is consistent with previous literature reviews of adult populations with ID as well as youth without an ID (Heller et al., 2011; Oude et al., 2009; Spanos et al., 2013).
This review indicated that the majority of interventions designed to improve anthropometric outcomes in youth with ID primarily utilize PA exclusively and are moderately effective in facilitating positive changes in fat mass (Elmahgoub et al., 2011; Ordonez et al., 2006; Salaun et al., 2014), BMI (Elmahgoub et al., 2009; Elmahgoub et al., 2011), WC (Elmahgoub et al., 2009; Salaun et al., 2014), and weight (Elmahgoub et al., 2009; Ordonez et al., 2006). Conversely, two of these interventions indicated no change in BMI (González-Agüero et al., 2011; Ozmen et al., 2007), weight (González-Agüero et al., 2011), and fat mass (González-Agüero et al., 2011). Of the multicomponent interventions, results were mixed as one demonstrated positive changes to weight (Ptomey et al., 2015) while the other two found no change in BMI, fat mass, and WC (Hinckson et al., 2013; Wallén et al., 2013) in Tx arms. These findings are inconsistent with previous literature that found a combination of strategies are more effective for sustainable change among youth with and without an ID (Must et al., 2014; Oude et al., 2009). According to clinical guidelines for obesity interventions, strategies incorporating PA, dietary techniques, and behavioral strategies are necessary for sustainable change and are recommended over PA alone (Must et al., 2014).
Seven of the studies included in this review examined a secondary health-related outcome. Results from the interventions indicate promising improvements to indices of physical fitness and activity (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Hinckson et al., 2013; Ozmen et al., 2007; Ptomey et al., 2015), cardiovascular health (Elmahgoub et al., 2009; Elmahgoub et al., 2011; Wallén et al., 2013), dietary habits (Hinckson et al., 2013; Ptomey et al., 2015), as well as self-perception (Salaun et al., 2014). Inclusion of these health-related outcomes in evaluation design is important as these variables can be considered antecedents to anthropometric change. In the current review, five studies indicated a lack of positive change in anthropometric outcomes and observed positive health-related outcomes (Hinckson et al., 2013; Ozmen et al., 2007; Wallén et al., 2013) or did not evaluate health-related outcomes (Casey et al., 2010; González-Agüero et al., 2011). As changes in anthropometric variables occur over time, the inability to account for health-related variables may lead researchers and practitioners to falsely conclude the ineffectiveness of an intervention if solely evaluating changes to body weight and composition.
While some of the results indicated in this review are promising, inconsistency and heterogeneity in outcome measures and study design limit conclusions regarding the effectiveness of these interventions to promote sustainable health-related outcomes among youth with ID. Cautious interpretation of these results is warranted due to limitations of the review itself as well as in the intervention design, implementation, and evaluation of the reviewed studies. While it appeared saturation was achieved for this review, only selected databases were included in the protocol resulting in the possibility that other search engines may have populated additional articles. This review was also limited to studies from 2006 to 2016 published in the English language, thus studies preceding and published after were not included. Finally, a singular reviewer extracted information from included articles; future work could be strengthened through multiple reviewers.
As illustrated in Figure 2, findings of this review indicate studies exhibited a low to moderate methodological quality as assessed through the modified Jadad scale with scores less than 5 on a 10-point scale for internal validity, reporting, and intervention quality (Casey et al., 2010; Elmahgoub et al., 2011; González-Agüero et al., 2011; Hinckson et al., 2013; Ordonez et al., 2006; Salaun et al., 2014; Wallén et al., 2013). Interventions with higher Jadad scale scores were mainly attributed to a research protocol that incorporated an RCT design or pretest and posttest with a control group (Elmahgoub et al., 2009; Ozmen et al., 2007; Ptomey et al., 2015). Studies utilizing an RCT design provide more robust evidence due to the ability to more adequately control for internal and external validity, whereas the utilization of less robust designs provides weaker program evidence due to an inability to account for casual evidence resulting from the intervention. However, prevalent and frequently cited obstacles in the incorporation of RCT protocols in participants with ID (Hassiotis and Sturmey, 2010; Oliver et al., 2002) have lead researchers to question the practicality and feasibility of this design in the ID population.
The majority of interventions primarily targeted the individual with an ID as the sole agent of change. The adoption of ecological, multilevel frameworks could prove beneficial in improving obesity prevention programs in individuals with ID as the approach can expand intervention components to better facilitate sustainable change (McLeroy et al., 1988). Within the context of family factors, parents play a key role to influence and facilitate dietary habits, reduce sedentary behavior, and promote healthier lifestyles (Must et al., 2014). Only two studies in this review integrated parental involvement to better foster behavior change, with results indicating improvements in PA (Ptomey et al., 2015) and nutritional habits (Hinckson et al., 2013; Ptomey et al., 2015). A singular study in this review employed a school-based intervention (Wallén et al., 2013) even though schools have been identified as a focal point for obesity prevention by the Institute of Medicine (2012) and have been evidenced as one of the most effective settings for obesity prevention (Wang et al., 2015). Multilevel approaches have been asserted as an effective strategy to improve obesity-related outcomes in youth with ID (Must et al., 2014), so future interventions should seek to leverage interpersonal and community influences such as school-based interventions that include family or home components.
None of the reviewed articles explicitly stated the utilization of a theoretical framework guiding intervention design. Previous research of obesity interventions in youth has indicated the need for interventions to include appropriate theoretical underpinnings of behavior change (Al and Nagy, 2011; Campbell et al., 2001). The incorporation of theoretical frameworks into obesity prevention interventions can assist to guide researchers in the design and evaluation of interventions to more adequately assess outcomes as a result of measuring antecedents of behavior (Glanz et al., 2008). Incorporating diverse theoretical frameworks into interventions will allow for the determination of their utility in changing behavior (Hackman and Knowlden, 2014) and has the capacity to improve research relating to individuals with ID and obesity prevention. Through the incorporation of theories and models, researchers can further explain behavior and develop strategies to increase behavior change (Glanz et al., 2008). Not only should future research incorporate health behavior or social theories and models, it is necessary that interventionists appropriately operationalize employed theories in order to effectively assess change in construct variables from baseline (Knowlden and Sharma, 2012).
The accuracy and sustainability of outcomes may be limited due to shortcomings in program implementation and evaluation. Most of the interventions in this review targeting anthropometric change in youth with ID were implemented for a short duration weeks; weeks). Interventions with short program durations may not be sufficient enough to facilitate meaningful or sustainable change to antecedents or actual behavior through the utilization of effective strategies (Spanos et al., 2013). Within this review, results of the intervention by Elmahgoub et al. (2011) provide support to duration as a key variable as improved outcomes were observed in the Tx arm with a longer program duration even though total sessions were equivalent between groups. The addition of a control group in interventions with longer program durations is also necessary to examine program effects. The 2-year intervention by Wallén et al. (2013) did not result in significant decreases in primary measures of body weight and composition but indicated that these values were significantly lower than a historical control group. This may provide evidence that the intervention was successful in attenuating the rate of obesity that may be traditionally observed during that period.
While some interventions did include individual components of process evaluation related to fidelity, failure to more comprehensively evaluate program fidelity components may limit the attribution of nonsignificant intervention outcomes due to ineffective program components as opposed to inadequate delivery. Additionally, based on the findings of this review, it is unclear whether positive changes attributed to these interventions are sustainable and long lasting. Only one of the studies reviewed included a follow-up evaluation (24 weeks) after the cessation of the intervention and the results indicated no change in anthropometric outcomes (Hinckson et al., 2013). Increased interventions with long-term outcome evaluation are needed to gauge long-term program effects. Previous literature has asserted weight loss attenuates and rebounds at 12 months (Oude et al., 2009), necessitating outcome evaluation at least 24 months from baseline (Knowlden and Sharma, 2012). Including increased follow-up periods may further explicate program capacity to elicit sustainable change.
While most articles included BMI as an anthropometric outcome measure, three studies did not include this measurement (Casey et al., 2010; Ordonez et al., 2006; Ozmen et al., 2007). Omission of a standardized outcome measure reduces clarity regarding program efficacy and should be considered. Further standardization of anthropometric outcome measures can allow for increased assessment of intervention effectiveness through meta-analysis. Additionally, there was a lack of evaluation design to analyze program effectiveness between ID level categories. Assessing the effectiveness of program components between ID level classifications can allow for further tailoring of interventions to a more specific subset of individuals with ID. Intervention evaluations also neglected to assess potential differences between age categories which could result in a failure to detect significant positive program effects between these groups. Consistent with previous literature, evaluation efforts should seek to elucidate potential differences between developmental age periods and ID level classification (Maïano et al., 2014), as well as certain medications. Certain pharmaceuticals, such as some atypical antipsychotics, are commonly prescribed in the treatment of autism spectrum disorder (ASD) and have been associated with significant weight gain and development of metabolic syndrome (Almandil et al., 2013; Beduin and de Haan, 2010). ASD was a common comorbidity attributed to participants in the included studies, and failure to account for medications that induce weight gain may mask program effects if not accounted for.
In conclusion, findings from this review elucidate that past interventions designed to improve anthropometric and health-related outcomes in youth with ID demonstrate promising but inconclusive evidence of successful change. The relatively small number of studies located via this review indicates a need for further interventions focusing on obesity prevention in youth with ID. As the evidence base grows, more distinct patterns and mechanisms of change can be identified to improve health outcomes in individuals with ID. It is recommended that future interventions directed towards changing body weight and composition among youth with ID strive to incorporate multilevel and multicomponent approaches that are guided by a theoretical framework. Additionally, future interventions should include longer treatment periods to ensure adequate time for behavioral and anthropometric change, comprehensive fidelity measures to limit the attribution of nonsignificant intervention outcomes due to ineffective program components as opposed to inadequate delivery, and increased follow-up periods post intervention to assess sustainability of any program effects. Evaluation designs should differentiate program effects associated with ID classification, age group, and medication while also including health-related outcomes to determine program effects on potential antecedents to anthropometric change.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- AlMarzooqi MA and Nagy MC (2011) Childhood obesity intervention programs: a systematic review. Life Science Journal 8: 45–60. [Google Scholar]
- Almandil NB, Liu Y, Murray ML, et al. (2013) Weight gain and other metabolic adverse effects associated with atypical antipsychotic treatment of children and adolescents: a systematic review and meta-analysis. Pediatric Drugs 15: 139–150. [DOI] [PubMed] [Google Scholar]
- Bandini LG, Curtin C, Hamad C, et al. (2005) Prevalence of overweight in children with developmental disorders in the continuous national health and nutrition examination survey (NHANES) 1999–2002. The Journal of Pediatrics 146: 738–743. [DOI] [PubMed] [Google Scholar]
- Beduin AS and de Haan L (2010) Off-label second generation antipsychotics for impulse regulation disorders: a review. Psychopharmacology Bulletin 43: 45–81. [PubMed] [Google Scholar]
- Campbell K, Waters E, O’meara S, et al. (2001) Interventions for preventing obesity in childhood. A systematic review. Obesity Reviews 2: 149–157. [DOI] [PubMed] [Google Scholar]
- Casey AF and Rasmussen R (2013) Reduction measures and percent body fat in individuals with intellectual disabilities: a scoping review. Disability & Health Journal 6: 2–7. [DOI] [PubMed] [Google Scholar]
- Casey AF, Rasmussen R, Mackenzie SJ, et al. (2010) Dual-energy X-ray absorptiometry to measure the influence of a 16-week community-based swim training program on body fat in children and adolescents with intellectual disabilities. Archives of Physical Medicine & Rehabilitation 91: 1064–1069. [DOI] [PubMed] [Google Scholar]
- Craigie AM, Lake AA, Kelly SA, et al. (2011) Tracking of obesity-related behaviours from childhood to adulthood: a systematic review. Maturitas 70: 266–284. [DOI] [PubMed] [Google Scholar]
- Elmahgoub SM, Lambers S, Stegen S, et al. (2009) The influence of combined exercise training on indices of obesity, physical fitness and lipid profile in overweight and obese adolescents with mental retardation. European Journal of Pediatrics 168: 1327–1333. [DOI] [PubMed] [Google Scholar]
- Elmahgoub SS, Calders P, Lambers S, et al. (2011) The effect of combined exercise training in adolescents who are overweight or obese with intellectual disability: the role of training frequency. Journal of Strength & Conditioning Research 25: 2274–2282. [DOI] [PubMed] [Google Scholar]
- Fox R, Switzky H, Rotatori AF, et al. (1982) Successful weight loss techniques with mentally retarded children and youth. Exceptional Children 49: 238–244. [Google Scholar]
- Freedman DS, Khan LK, Serdula MK, et al. (2005) The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics 115: 22–27. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, and Viswanath K (2008) Health Behavior and Health Education: Theory, Research, and Practice. Hoboken: John Wiley & Sons. [Google Scholar]
- González-Agüero A, Vicente-Rodríguez G, Gómez-Cabello A, et al. (2011) A combined training intervention programme increases lean mass in youths with Down syndrome. Research in Developmental Disabilities 32: 2383–2388. [DOI] [PubMed] [Google Scholar]
- Gundersen C, Mahatmya D, Garasky S, et al. (2011) Linking psychosocial stressors and childhood obesity. Obesity Reviews 12: e54–e63. [DOI] [PubMed] [Google Scholar]
- Hackman CL and Knowlden AP (2014) Theory of reasoned action and theory of planned behavior-based dietary interventions in adolescents and young adults: a systematic review. Adolescent Health, Medicine and Therapeutics 5: 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassiotis A and Sturmey P (2010) Randomised controlled trials in intellectual disabilities and challenging behaviours–current practice and future challenges. European Psychiatric Review 3: 39–42. [Google Scholar]
- Haveman M, Heller T, Lee L, et al. (2010) Major health risks in aging persons with intellectual disabilities: an overview of recent studies. Journal of Policy and Practice in Intellectual Disabilities 7: 59–69. [Google Scholar]
- Havercamp SM, Scandlin D, and Roth M (2004) Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Reports 119: 418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller T, McCubbin JA, Drim C, et al. (2011) Physical activity and nutrition health promotion interventions: what is working for people with intellectual disabilities. Intellectual & Developmental Disabilities 49: 26–36. [DOI] [PubMed] [Google Scholar]
- Higgins JP and Green S (eds) (2011) Cochrane Handbook for Systematic Reviews of Interventions, Vol. 4. Hoboken: John Wiley & Sons. [Google Scholar]
- Hinckson EA, Dickinson A, Water T, et al. (2013) Physical activity, dietary habits and overall health in overweight and obese children and youth with intellectual disability or autism. Research in Developmental Disabilities 34: 1170–1178. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2012) Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington: National Academies Press. [Google Scholar]
- Knowlden A and Sharma M (2012) Systematic review of family and home-based interventions targeting paediatric overweight and obesity. Obesity Reviews 13: 499–508. [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maïano C, Normand CL, Aimé A, et al. (2014) Lifestyle interventions targeting changes in body weight and composition among youth with an intellectual disability: a systematic review. Research in Developmental Disabilities 35: 1914–1926. [DOI] [PubMed] [Google Scholar]
- McCrindle BW (2015) Cardiovascular consequences of childhood obesity. Canadian Journal of Cardiology 31: 124–130. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, et al. (1988) An ecological perspective on health promotion programs. Health Education & Behavior 15: 351–377. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151: 264–269. [DOI] [PubMed] [Google Scholar]
- Must A, Curtin C, Hubbard K, et al. (2014) Obesity prevention for children with developmental disabilities. Current Obesity Reports 3: 156–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A and Strauss RS (1999) Risks and consequences of childhood and adolescent obesity. International Journal of Obesity & Related Metabolic Disorders 23: S2–S11. [DOI] [PubMed] [Google Scholar]
- Nguyen NT, Nguyen XMT, Lane J, et al. (2011) Relationship between obesity and diabetes in a US adult population: findings from the national health and nutrition examination survey, 1999–2006. Obesity Surgery 21: 351–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, et al. (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311: 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver PC, Piachaud J, Done A, et al. (2002) Difficulties in conducting a randomized controlled trial of health service interventions in intellectual disability: implications for evidence-based practice. Journal of Intellectual Disability Research 46: 340–345. [DOI] [PubMed] [Google Scholar]
- Ordonez FJ, Rosety M, and Rosety RM (2006) Influence of 12-week exercise training on fat mass percentage in adolescents with Down syndrome. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research 12: CR416–CR419. [PubMed] [Google Scholar]
- Oude LH, Baur L, Jansen H, et al. (2009) Interventions for treating obesity in children. Cochrane Database of Systematic Reviews 1: CD001872. [DOI] [PubMed] [Google Scholar]
- Ozmen T, Ryildirim N, Yuktasir B, et al. (2007) Effects of school-based cardiovascular-fitness training in children with mental retardation. Pediatric Exercise Science 19: 171–178. [DOI] [PubMed] [Google Scholar]
- Ptomey LT, Sullivan DK, Lee J, et al. (2015) The use of technology for delivering a weight loss program for adolescents with intellectual and developmental disabilities. Journal of the Academy of Nutrition & Dietetics 115: 112–118. [DOI] [PubMed] [Google Scholar]
- Rimmer J, Yamaki K, Lowry B, et al. (2010) Obesity and obesity-related secondary conditions in adolescents with intellectual/developmental disabilities. Journal of Intellectual Disability Research 54: 787–794. [DOI] [PubMed] [Google Scholar]
- Rotatori A, Switzky HN, and Fox R (1981) Behavioral weight reduction procedures for obese mentally retarded individuals: a review. Mental Retardation 19: 157–161. [PubMed] [Google Scholar]
- Salaun L, Reynes E, and Berthouze-Aranda SE (2014) Adapted physical activity programme and self-perception in obese adolescents with intellectual disability: between morphological awareness and positive illusory bias. Journal of Applied Research in Intellectual Disabilities 27: 112–124. [DOI] [PubMed] [Google Scholar]
- Sarris J and Byrne GJ (2011) A systematic review of insomnia and complementary medicine. Sleep Medicine Reviews 15: 99–106. [DOI] [PubMed] [Google Scholar]
- Schalock RL, Borthwick-Duffy SA, Bradley VJ, et al. (2010) Intellectual Disability: Definition, Classification, and Systems of Supports. Washington: American Association on Intellectual and Developmental Disabilities. [DOI] [PubMed] [Google Scholar]
- Spanos D, Melville CA, and Hankey CR (2013) Weight management interventions in adults with intellectual disabilities and obesity: a systematic review of the evidence. Nutrition Journal 12: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Public Health Service (2002) Closing the gap: A national blueprint for improving the health of individuals with mental retardation. Report of the surgeon general’s conference on health disparities and mental retardation. Washington, DC: US Department of Health and Human Services. [PubMed] [Google Scholar]
- Visness CM, London SJ, Daniels JL, et al. (2010) Association of childhood obesity with atopic and nonatopic asthma: results from the national health and nutrition examination survey 1999–2006. Journal of Asthma 47: 822–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallén EF, Müllersdorf M, Christensson K, et al. (2013) A school-based intervention associated with improvements in cardiometabolic risk profiles in young people with intellectual disabilities. Journal of Intellectual Disabilities 17: 38–50. [DOI] [PubMed] [Google Scholar]
- Wang Y, Cai L, Wu Y, et al. (2015) What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obesity Reviews 16: 547–565. [DOI] [PMC free article] [PubMed] [Google Scholar]


