Abstract
Deleterious variants of DYNC2H1 gene are associated with a wide spectrum of skeletal ciliopathies (SC). We used targeted parallel sequencing to analyze 25 molecularly unsolved families with different SCs. Deleterious DYNC2H1 variants were found in six sporadic patients and two monozygotic (MZ) twins. Clinical diagnoses included short rib-polydactyly type 3 in two cases, and asphyxiating thoracic dystrophy (ATD) in one case. Remarkably, clinical diagnosis fitted with EvC, mixed ATD/EvC and short rib-polydactyly/EvC phenotypes in three sporadic patients and the MZ twins. EvC/EvC-like features always occurred in compound heterozygotes sharing a previously unreported splice site change (c.6140-5A>G) or compound heterozygotes for two missense variants. These results expand the DYNC2H1 mutational repertoire and its clinical spectrum, suggesting that EvC may be occasionally caused by DYNC2H1 variants presumably acting as hypomorphic alleles.
Subject terms: Genetics research, Disease genetics
Ciliopathies are an expanding group of clinically variable and genetically heterogeneous disorders characterized by renal, liver, central nervous system, ocular and skeletal anomalies. Those with predominant skeletal involvement are grouped as skeletal ciliopathies (SCs). SCs comprise Weyers acrofacial dysostosis (WAD, MIM# 193530), Ellis-van Creveld syndrome (EvC, MIM# 225500), cranioectodermal dysplasia (CED, MIM# 218330, or Sensenbrenner syndrome), asphyxiating thoracic dystrophy (ATD, MIM# 208500; or Jeune syndrome), short rib-polydactyly type 1 (SRP1 or Saldino-Noonan type, MIM# 613091), type 2 (SRP2 or Majewski type, MIM# 263520), type 3 (SRP3 or Verma-Naumoff type, MIM# 613091), and type 4 (SRP4 or Beemer-Langer type, MIM# 269860).
To date, at least 30 genes coding for different structural cilia proteins have been implicated in SC [1, 2]. The distinct roles that these proteins have in ciliary function likely underlie some consolidated genotype-phenotype correlations and the different molecular epidemiology among SC. Most EvC cases are due to biallelic variants in EVC and EVC2 [3–5], while a few cases are caused by recessive variants in WRD35 [6], DYNC2LI1 [7], GLI1 [8] or dominant variants in PRKACA and PRKACB [9]. Among SC-associated genes, DYNC2H1 is the most commonly involved locus and DYNC2H1 deleterious variants have been found in a broad spectrum of skeletal ciliopathies ranging from the perinatally lethal SRP types 1, 2, and 3 to non-lethal-ATD cases [1, 2, 10, 11].
We used targeted parallel sequencing to analyze an extended panel of 110 ciliary genes in 26 subjects (7 prenatal and 19 postnatal cases) belonging to 25 families with clinically suspected EvC or another SC. The genes included in the panel are listed in Supplementary Table S1. In all cases, single nucleotide variants in EVC, EVC2, WDR35, DYNC2LI1, GLI1, PRKACA and PRKACB, and intragenic copy number variants (CNVs) in EVC and EVC2 had been previously excluded by Sanger sequencing, a restricted multigene panel assessed by parallel sequencing and multiplex ligation-dependent probe amplification analysis. Clinical selection criteria and description of the methods used for the molecular analyses are reported in the Supporting Information.
Sequencing identified putative deleterious variants in DYNC2H1 (NCBI Reference Sequence: NM_001377.3) in seven index cases, including six sporadic cases and a couple of monozygotic (MZ) twins. In six patients, two variants were identified, while one sporadic case showed a homozygous variant. In patients 1, 3, 6, 7 and 8 parental genotyping confirmed the occurrence of compound heterozygosity. In case 3, the homozygous splice site change, c.6140-5A>G, was absent in the father, whose paternity had been confirmed by DNA fingerprinting test (PowerPlex 16 System, Promega, Madison, WI, USA). In this patient, SNP-array analysis allowed to identify a large deletion encompassing 31 genes, including the entire DYNC2H1 as well as other 21 OMIM genes (arr[GRCh37] 11q22.1q22.3 (99715102_103351453) × 1) (Supplementary Fig. S1 and Supplementary Table S2).
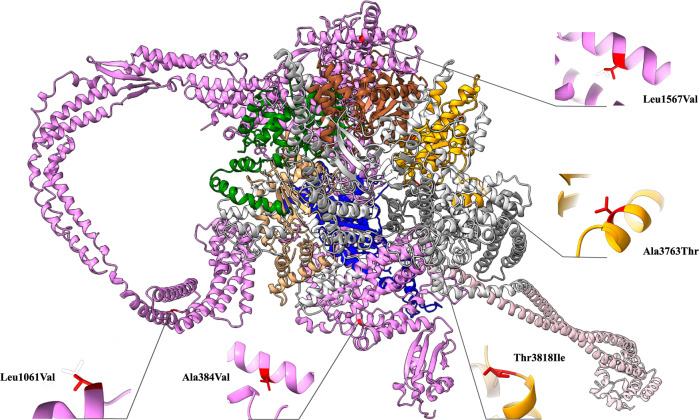
The mutation spectrum included a total of 11 DYNC2H1 variants (Table 1). Among the novel variants, two were recurrent (c.6140-5A>G [patients 1, 2, and 3] and c.9171_9174delGGAA [patients 1 and 6]). Although the DYNC2H1 variants were distributed along the entire length of the gene, missense changes affected two specific regions of the protein, the Stem and AAA + 6 domains (Fig. 1). We explored a possible structural and functional impact of these amino acid alterations in terms of protein stability by measuring their induced thermodynamic change [12]. Based on the difference in free energy value (ΔΔG = ΔGmt – ΔGwt), p.(Ala384Val), p.(Leu1567Val) and p.(Thr3818Ile) variants were classified as destabilizing and p.(Ala3763Thr) change as slightly stabilizing. Finally, a neutral impact was predicted for the p.(Leu1061Val) substitution. The free energy calculations results are summarized in Table 1, while protein stability study methods are described in the Supporting Information.
Table 1.
Molecular description, population prevalence, bioinformatics predictions, and pathogenicity classification according to the American College of Medical Genetics and Genomics-Association for Molecular Pathology (ACMG-AMP) classification of DYNC2H1 variants identified in this study.
| Patienta | Nucleotide substitutionb | RNA substitution | Protein substitution | Variant type | Protein Domain | GnomAD | CADD score | ΔΔGc | ACMG-AMP criteria met | ACMG-AMP classification | Pubmed |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | c.6140-5A>G | r.6139_6140insATAG | p.Val2048ArgfsTer9 | Splicing | AAA + 2 | Absent | / | NE | PS3_Strong, PM2_Moderate, PM3_Moderate | LP | Not reported |
| c.9171_9174delGGAA | NE | p.(Glu3058Ter) | Frameshift | MT-binding stalk | Absent | / | NE | PVS1_VeryStrong, PM2_Moderate. PM3_Moderate | P | Not reported | |
| 2 | c.12619C>T | NE | p.(Arg4207Ter) | Nonsense | ATP-ase ring (Dynein heavy) C-terminal | 0.000004193 | 56 | NE | PVS1_VeryStrong, PM2_Moderate. PM3_Moderate | P | Not reported |
| c.6140-5A>G | r.6139_6140insATAG | p.Val2048ArgfsTer9 | Splicing | AAA + 2 | Absent | / | NE | PS3_Strong, PM2_Moderate, PM3_Moderate | LP | Not reported | |
| 3 | arr[GRCh37] 11q22.1q22.3 (99715102_103351453)x1 | - | - | Whole gene deletion | - | / | / | NE | NA | P | Not reported |
| c.6140-5A>G | r.6139_6140insATAG | p.Val2048ArgfsTer9 | Splicing | AAA + 2 | Absent | / | NE | PS3_Strong, PM2_Moderate, PM3_Moderate | LP | Not reported | |
| 4 | c.11287G>A | NE | p.(Ala3763Thr) | Missense | AAA + 6 | 0.00005360 | 34 | −0.808502 | PM1_Moderate, PM2_Moderate, PP3_Supporting | VUS | Not reported |
| c.3181C>G | NE | p.(Leu1061Val) | Missense | Stem Domain | 0.0008700 | 21.5 | 0.419578 | PM2_Moderate | VUS | Not reported | |
| 5 | c.11287G>A | NE | p.(Ala3763Thr) | Missense | AAA + 6 | 0.00005360 | 34 | −0.808502 | PM1_Moderate, PM2_Moderate, PP3_Supporting | VUS | Not reported |
| c.3181C>G | NE | p.(Leu1061Val) | Missense | Stem Domain | 0.0008700 | 21.5 | 0.419578 | PM2_Moderate | VUS | Not reported | |
| 6 | c.9171_9174delGGAA | NE | p.(Glu3058Ter) | Frameshift | MT-binding stalk | Absent | / | NE | PVS1_VeryStrong, PM2_Moderate | LP | Not reported |
| c.11453C>T | NE | p.(Thr3818Ile) | Missense | AAA + 6 | Absent | 24.9 | 1.65291 | PM1_Moderate, PM2_Moderate,PM3_Moderate | LP | Not reported | |
| 7 | c.4699C>G | NE | p.(Leu1567Val) | Missense | Stem Domain | Absent | 25.2 | 1.16155 | PM2_Moderate, PM3_Moderate, PP5_Supporting | VUS | 1 |
| c.503-9C>G | r.503_621del | p.(Arg167GlyfsTer4) | Splicing | - | Absent | / | NE | PS3_Strong, PM2_Moderate | LP | Not reported | |
| 8 | c.1151C>T | NE | p.(Ala384Val) | Missense | Stem Domain | 0.0000244 | 28.3 | 1.56786 | PM2_Moderate, PM3_Moderate PP3_Supporting | VUS | 15 |
| c.6342_6345delTCTT | NE | p. (Phe2114LeufsTer11) | Frameshift | AAA + 2 | Absent | / | NE | PVS1_VeryStrong, PM2_Moderate | LP | Not reported |
ACMG-AMP American College of Medical Genetics and Genomics-Association for Molecular Pathology, CADD Combined Annotation Dependent Depletion, GnomAD Genome Aggregation Database, LP likely pathogenetic, NA not applicable, NE not evaluated, P pathogenetic, VUS variant of uncertain significance.
aDYNC2H1 mutations have been included in the LOVD database (https://databases.lovd.nl/shared/variants/DYNC2H1/unique); LOVD individual IDs: patient 1 (#0000407149), patient 2 (#0000407151), patient 3 (#0000407152), patient 4 (#0000407195), patient 5 (#0000407195), patient 6 (#0000407196), patient 7 (#0000407197); patient 8 (#0000409854).
bNCBI Reference Sequence: NM_001377.3.
cΔΔG (ΔGmt – ΔGwt) for DYNC2H1 mutant protein.
Fig. 1. 3D structure of DYNC2H1 obtained through modeling.
Functional domains were colored in violet (stem, residues 1-1650), brown (AAA + 1, residues 1651–1875), green (AAA + 2, residues 1938–2161), beige (AAA + 3, residues 2251–2505), blue (AAA + 4, residues 2617–2863), pink (stalk, residues 2881–3169), gray (AAA + 5, residues 3244–3473) and orange (AAA + 6, residues 3690–3905). Variants were mapped on the wild-type structure and highlighted in red.
According to in silico splicing predictions, c.6140-5A>G and c.503-9C>G intronic variants were expected to affect proper transcript processing (Supporting Information). cDNA analysis confirmed that both variants affected splicing. Specifically, c.6140-5A>G creates a new 3´ splice acceptor site leading to an aberrantly processed transcript, which incorporates four bases of intron 38 (r.6139_6140insATAG) (Supplementary Fig. S2). This altered processing results in a frameshift and introduces of a premature termination codon [p.(Val2048ArgfsTer9)], which is predicted to lead to nonsense-mediated mRNA decay (NMD). Similarly, cDNA analysis confirmed that also c.503-9C>G affects splicing by causing the out-of-frame skipping of exon 4 (r.503_621del), the consequent introduction of a premature stop codon, and the translation of a truncated protein presumably undergoing NMD (Supplementary Fig. S3).
Demographic, radiographic and clinical data of the eight patients are shown in Table 2. Selected clinical and radiological features are illustrated in Supplementary Fig. S4. Detailed clinical descriptions of each case are reported in Supporting Information. In summary, clinical features suggested the diagnosis of EvC in two cases (patients 2 and 4/5), SRP3 in two cases (patients 6 and 7), ATD in one case (patient 1) and a mixed EvC/ATD (patient 3) or EvC/SRP3 (patient 8) phenotype in two cases.
Table 2.
Clinical features in patients with biallelic DYNC2H1 variants compared with those characterizing Ellis-van Creveld syndrome (EvC), asphyxiating thoracic dystrophy (ATD) and short-rib thoracic dysplasia type 3 (SRP3).
| Feature | 1 | 2 | 3 | 4* | 5* | 6 | 7 | 8 | ATD | EvC | SRP3 |
| Sex | F | M | M | F | F | M | F | M | |||
| Country of origin | Italy | Italy | Italy | Italy | Italy | Albany | Italy | Italy | |||
| Consanguineus parents | - | - | - | - | - | - | - | - | |||
| Age | 1 month | NA | 4 month | NA | NA | NA | NA | 1.9 years | |||
| Oral frenula | + | HLF | - | - | - | - | - | - | - | + | - |
| Dental anomalies | - | SSCT | - | HD, CT, EH | HD, CT, EH, MO | - | - | - | - | + | - |
| Dysplastic nails | - | - | STN | + | + | - | - | - | - | + | - |
| Short stature | + | + | + | + | + | + | + | - | + | + | + |
| Narrow thorax | + | + | + | + | + | + | + | + | + | + | + |
| Limb shortening | + | + | + | + | + | + | + | - | + | + | + |
| Irregular metaphyses | + | - | - | - | - | - | - | - | + | - | + |
| Vertebral anomalies | - | - | - | - | - | FVB | - | - | - | - | P |
| Pelvic abnormalities | - | - | - | - | - | SIWSLS | - | + | + | + | + |
| Hand postaxial polydactyly | B | B | B | B | B | + | + | - | Rare | + | Rare |
| Feet postaxial polydactyly | - | U | B | U | B | + | + | - | Rare | + | Rare |
| Hand brachydactyly | - | - | + | - | - | - | - | + | + | - | + |
| Hand/feet sindactyly | - | - | + | - | - | - | - | + | + | - | + |
| Cardiac defect | - | - | HLVA | pAVC, PDA | pAVC, PDA | - | - | - | TGA | + | - |
| Renal anomalies | - | - | HK, MCK | - | - | RD | HK | - | + | - | + |
| Pulmonary anomalies | PI | - | - | - | - | NA | NA | - | + | - | + |
| Gastrointestinal anomalies | - | - | - | - | - | IM | - | - | - | - | IM |
| Other anomalies | - | IH, PolyH | - | - | - | - | - | CF | |||
| Clinical diagnosis | ATD | EvC | EvC/ATD | EvC | EvC | SRPS3 | SRPS3 | EvC/SRP3 |
+, present; -, absent; *, monozygotic twins.
B bilateral, BH bilateral hydronephrosis, CF club foot, CT conical teeth, EH enamel hypoplasia, F female, FVB flattened vertebral bodies, HD hypodontia, HK hyperechogenic kidneys, HLF hypertrophic labiogingival frenulum; HLVA hypertrabeculature of left ventricle apex, IH inguinal hernia, IM intestinal malrotation, M male, MCK multicistic kidneys, MO, malocclusion, NA not available; P platyspondyly, pAVC partial atrioventricular canal, PDA, patent ductus arteriosus, PI pulmonary insufficiency PolyH polyhydramnios, RD renal dysplasia, SIWSLS small iliac wings with small lower spur, SSCT, small, sharp and conical teeth, STN short thin nails, U unilateral, TGA great vessels transposition, VC vertebral cleft.
Deleterious biallelic variants in DYNC2H1 gene have been identified in patients with ATD, SRP1, SRP2, SRP3, and very recently in three individuals with EvC showing no cardiac involvement, but multiple frenula and nail hypoplasia [13]. The present results further expand DYNC2H1-associated mutational repertoire and widen the clinical spectrum of the deleterious variants of this gene to include also EvC. The identification of potentially disease-causing DYNC2H1 variants in individuals with a presentation fitting with EvC rather than with ATD and short rib-polydactyly is not surprising within the spectrum of SCs. The current nosology of hereditary bone disorders maintains separate these conditions [14]. Such a distinction is supported by considering the overall severity, postnatal life expectancy and pattern of associated extra-skeletal features. However, the existence of a phenotypic continuum among them dates back to the observation of SRP3 and ATD in the same family [15]. In the present cohort, two index cases had a diagnosis of SRP3 before molecular testing, supporting the presence of a predominant pattern of anomalies associated with DYNC2H1 deleterious variants at the severe end of the spectrum. In addition, biallelic DYNC2H1 variants were found in a case of ATD with multiple oral frenula and favorable prognosis (patient 1). A sporadic case was considered affected by a mixed ATD/EvC phenotype featuring short stature of the short limb type, dysplastic nails, tetramelic postaxial polydactyly, and congenital heart and genitourinary anomalies (patient 3). Another sporadic case was clinically framed as a mixed SRP3/EvC phenotype because of a mild bone dysplasia with short ribs associated with partial feet syndactyly. Finally, two MZ twins showed full-blown characteristics of EvC including multiple oral frenula, dysplastic nails, short stature with short limbs, narrow thorax and polydactyly (patients 4 and 5). The present findings support the existence of a much wider phenotypic spectrum for biallelic DYNC2H1 variants extending to an attenuated skeletal phenotype strongly resembling EvC.
We identified 11 different DYNC2H1 variants, including two known as pathogenic [1, 16], and nine not previously reported. To our knowledge, this is the first description of compound heterozygosity for a whole gene deletion (WGD) including DYNC2H1. Interestingly, the novel c.6140-5A>G splice site change was found in three subjects with variable clinical features fitting with ATD (case 1), EvC (case 2), and both conditions (case 3). In two cases, c.6140-5A>G was combined with a truncating variant [p.(Glu3058Ter), p.(Arg4207Ter)], and in one case with a WGD. We speculate that the phenotypic variability of these patients, ranging from ATD to EvC, is attributable to a variable loss of DYNC2H1 function induced by the null allele, while the specific c.6140-5A>G splice change probably acts as a hypomorphic allele. Accordingly, this intronic variant has never been identified in association with SRP3, which is the most severe DYNC2H1-related SC. c.6140-5A>G was found in patients from Southern Italy, probably representing a founder effect in that population. Interestingly, the three DYNC2H1-mutated individuals with EvC phenotype recently described in Aubert-Mucca et al. [13] were also compound heterozygous for a mutant null allele and an intronic variant outside the canonical splice sites. The description of further DYNC2H1-mutated EvC cases may clarify whether or not there is an association between DYNC2H1 intronic variants and EvC. The identification of two missense changes [p.(Ala3763Thr) and p.(Leu1061Val)] in MZ twins displaying a typical EvC phenotype may suggest the existence of specific DYNC2H1 missense variants determining less severe consequences on the protein function and, thus, leading to milder phenotypes. This hypothesis seems to be consistent with protein stability computations, predicting that variants associated with SRP3 destabilize the protein [p.(Ala384Val), p.(Leu1567Val) and p.(Thr3818Ile)], while those associated with EvC are either neutral [p.(Leu1061Val)] or increase protein stability [p.(Ala3763Thr)].
In conclusion, this study adds nine novel variants to the DYNC2H1 mutational repertoire and provides evidence that the associated clinical spectrum of pathogenic DYNC2H1 variants includes EvC and EvC-like phenotypes. This work also highlights the utility to add splicing and CNV analysis in the diagnostic flow-chart of SCs in order to improve the clinical effectiveness of the laboratory report.
Supplementary information
Acknowledgements
We would like to express our gratitude to the patients who made this study possible.
Author contributions
Conceptualization: FP-S, BM, MT, ADL; Formal analysis: MCD, FP, LB, TM; Funding acquisition: FP-S, LM, TM, MT, MC, ADL; Investigation: FP-S, LM, BT, VG, FC, IT, AO, EF, MCD, FP, LB, CM, DC, ADL; Project administration: FP-S, ADL; Resources: FS, DG, GM, CP, FF, NB-P, AN, AP, BM, MCD, BD, VLR-P, MC; Supervision: TM, MC, ADL; Visualization: FP-S, LM, LB, MCD, TM, ADL; Writing – original draft: FP-S, LM; Writing – review & editing: TM, BD, VLR-P, MT, MC, ADL.
Funding
This study was supported by funding from the Italian Ministry of Health (RC‐2020 and RC-2021, to ADL; RC-2018-2021 to LM and MC; 5 × 1000, to MT and TM), and the Sapienza University of Rome research grants “avvio alla ricerca 2019 (AR11916B7A1835AC)” and “avvio alla ricerca 2021 (AR12117A86EA0740)” to FP-S.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request. All variants have been added to the Leiden Open Variation Database (LOVD, https://databases.lovd.nl/shared/variants/DYNC2H1/unique).
Competing interests
The authors declare no competing interests.
Ethics approval
The study was performed in accordance with the principles set out in the 1984 Declaration of Helsinki and subsequent versions and was approved by the local institutional review board (no. 13/CE 2021). All patients signed an informed consent for the scientific use of clinical and genetic data. Written informed consent for publication of images was obtained.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41431-022-01276-7.
References
- 1.Zhang W, Taylor SP, Ennis HA, Forlenza KN, Duran I, Li B, et al. Expanding the genetic architecture and phenotypic spectrum in the skeletal ciliopathies. Hum Mutat. 2018;39:152–66. doi: 10.1002/humu.23362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hammarsjo A, Pettersson M, Chitayat D, Handa A, Anderlid B-M, Bartocci M, et al. High diagnostic yield in skeletal ciliopathies using massively parallel genome sequencing, structural variant screening and RNA analyses. J Hum Genet. 2021;66:995–1008. doi: 10.1038/s10038-021-00925-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiz-Perez VL, Ide SE, Strom TM, Lorenz B, Wilson D, Woods K, et al. Mutations in a new gene in Ellis-van Creveld syndrome and Weyers acrodental dysostosis. Nat Genet. 2000;24:283–6. doi: 10.1038/73508. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Perez VL, Tompson SW, Blair HJ, Espinoza-Valdez C, Lapunzina P, Silva E, et al. Mutations in two nonhomologous genes in a head-to-head configuration cause Ellis-van Creveld syndrome. Am J Hum Genet. 2003;72:728–32. doi: 10.1086/368063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D’Asdia MC, Torrente I, Consoli F, Ferese R, Magliozzi M, Bernardini L, et al. Novel and recurrent EVC and EVC2 mutations in Ellis-van Creveld syndrome and Weyers acrofacial dyostosis. Eur J Med Genet. 2013;56:80–87. doi: 10.1016/j.ejmg.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Caparrós-Martín JA, De Luca A, Cartault F, Aglan M, Temtamy S, Otaify GA, et al. Specific variants in WDR35 cause a distinctive form of Ellis-van Creveld syndrome by disrupting the recruitment of the EvC complex and SMO into the cilium. Hum Mol Genet. 2015;24:4126–37. doi: 10.1093/hmg/ddv152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niceta M, Margiotti K, Digilio MC, Guida V, Bruselles A, Pizzi S, et al. Biallelic mutations in DYNC2LI1 are a rare cause of Ellis-van Creveld syndrome. Clin Genet. 2018;93:632–9. doi: 10.1111/cge.13128. [DOI] [PubMed] [Google Scholar]
- 8.Palencia-Campos A, Ullah A, Nevado J, Yıldırım R, Unal E, Ciorraga M, et al. GLI1 inactivation is associated with developmental phenotypes overlapping with Ellis-van Creveld syndrome. Hum Mol Genet. 2017;26:4556–71. doi: 10.1093/hmg/ddx335. [DOI] [PubMed] [Google Scholar]
- 9.Palencia-Campos A, Aoto PC, Machal EMF, Rivera-Barahona A, Soto-Bielicka P, Bertinetti D, et al. Germline and mosaic variants in PRKACA and PRKACB cause a multiple congenital malformation syndrome. Am J Hum Genet. 2020;107:977–88. doi: 10.1016/j.ajhg.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidts M, Arts HH, Bongers EM, Yap Z, Oud MM, Antony D, et al. Exome sequencing identifies DYNC2H1 mutations as a common cause of asphyxiating thoracic dystrophy (Jeune syndrome) without major polydactyly, renal or retinal involvement. J Med Genet. 2013;50:309–23. doi: 10.1136/jmedgenet-2012-101284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El Hokayem J, Huber C, Couve A, Baujat G, Bouvier R, Cavalcanti DP, et al. NEK1 and DYNC2H1 are both involved in short rib polydactyly Majewski type but not in Beemer Langer cases. J Med Genet. 2012;49:227–33. doi: 10.1136/jmedgenet-2011-100717. [DOI] [PubMed] [Google Scholar]
- 12.Wang Z, Moult J. SNPs, protein structure, and disease. Hum Mutat. 2001;17:263–70. [DOI] [PubMed]
- 13.Aubert-Mucca M, Huber C, Baujat G, Michot C, Zarhrate M, Bras M, et al. Ellis-Van Creveld Syndrome: clinical and molecular analysis of 50 individuals. J Med Genet. 2022:2022-108435. [DOI] [PubMed]
- 14.Mortier GR, Cohn DH, Cormier-Daire V, Hall C, Krakow D, Mundlos S, et al. Nosology and classification of genetic skeletal disorders: 2019 revision. Am J Med Genet A. 2019;179:2393–419. doi: 10.1002/ajmg.a.61366. [DOI] [PubMed] [Google Scholar]
- 15.Ho NC, Francomano CA, van Allen M. Jeune asphyxiating thoracic dystrophy and short-rib polydactyly type III (Verma-Naumoff) are variants of the same disorder. Am J Med Genet. 2000;90:310–4. doi: 10.1002/(SICI)1096-8628(20000214)90:4<310::AID-AJMG9>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 16.Mei L, Huang Y, Pan Q, Su W, Quan Y, Liang D, et al. Targeted next-generation sequencing identifies novel compound heterozygous mutations of DYNC2H1 in a fetus with short rib-polydactyly syndrome, type III. Case Reports. Clin Chim Acta. 2015;447:47–51. doi: 10.1016/j.cca.2015.05.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request. All variants have been added to the Leiden Open Variation Database (LOVD, https://databases.lovd.nl/shared/variants/DYNC2H1/unique).