Abstract
Coronavirus disease 2019 (COVID-19) predilection for angiotensin-converting enzyme 2 (ACE2) receptors allows its entrance and replication; however, they are not biochemically required for viral fusion into the cell membrane. Testicular tissue has abundant ACE2 receptors, making it a target for the COVID-19 virus. Seminal fluid parameters are measures of male fertility. Changes in semen parameters have been caused by coronavirus disease and vaccines. Some attribute that effect to direct hematogenic spread to the testis; others propose that the excessive immunological response triggered by the infection causes a deleterious effect. An unsubstantiated claim questioned whether the SARS-CoV-2 vaccine could trigger an unintentional immunological response that would impair male fertility once receiving the vaccine. Extensive research confirms the transient nature of those changes that affect sperm motility and count with full recovery post-COVID-19 infection and after vaccination. The vaccine's safety was reaffirmed; however, there are currently no recommendations for screening sperm donors. Research is warranted to guarantee the safety of couples undergoing assisted reproduction.
Keywords: COVID-19, Seminal fluid analysis, Male fertility, Vaccine, Infection
1. Introduction
The coronavirus disease of 2019 (COVID-19) is caused by an extremely contagious virus that spreads quickly into the upper respiratory tract, which is the primary way of spreading. COVID-19's most common symptoms are fever, cough, shortness of breath, muscle pain, and headache. The disease characteristics differ by patients' age, ethnic group, geographical area, and disease waves.1, 2, 3 The viral transmission to extrapulmonary organs is proposed to be systemic; many body fluids show a positive existence of the virus.4, 5, 6
The binding of the SARS-CoV-2 virus via Spike protein (protein S) to angiotensin-converting enzyme 2 (ACE-2) receptors will facilitate its entry and replication in the cell. The ACE2 appears to be a vital functional receptor for SARS-CoV-2; it accelerates viral fusion to the cell membrane; however, they are not biochemically required for viral fusion.4, 5, 6, 7
Cells that show a high level of ACE-2 expression might be directly targeted and damaged by the virus, like testicular tissues, a high-risk organ for viral infection. Spermatogonia, seminiferous duct cells, Sertoli, and Leydig cells are all targeted by SARS-CoV-2; consequently, the infection renders spermatogenesis. Noticeably, the expression of ACE-2 by the testis is age dependent. Males in their thirties had higher ACE-2 expression than males in their sixties.6 , 8
Xu et al. study declared that orchitis is one of the SARS-2002 pandemic complications. Testicular tissue destruction was detected in a postmortem study and was proposed to be mediated by the immune response. Targeting the testis during viral infection is not new; other viruses like the human immunodeficiency virus, the hepatitis-B virus, and the mumps reportedly cause viral orchitis, infertility, and even testicular tumors.9
Controversy surrounds the potential impact of COVID-19 on reproductive health, particularly in males. The propensity of the virus to attach to the ACE2 receptor on Leydig cells after crossing the blood-testis barrier was a proposed theory. Others discussed spermatogenesis impairment. Important co-factors, like mental health and unrest caused by the pandemic, should also be taken into account.7 , 10 , 11
Vaccination is the most efficient way of preventing and managing infectious illnesses. The Pfizer COVID-19 vaccine was the WHO's first vaccination authorized for emergency use in late 2020. Other vaccines were developed subsequently. Fear and uncertainty about how vaccines affect health, especially male fertility, has been named as reasons for vaccine hesitancy.12
The most popular SARS-CoV-2 vaccines are made using one of the following methods.
-
(a)
Whole virus vaccine including inactivated or killed viruses like (ex. Sinovac's CoronaVac).And viral vector-based vaccines (ex. Astra Zeneca, Janssen/Johnson, and Johnson vaccine). These vaccines use a harmless non-replicating variant of adenovirus as a vehicle to transmit the genetic coding of the S glycoprotein antigens, inducing a targeted immune reaction. A higher incidence of systemic side effects was reported.13
-
(b)
The genetic material vaccine; mRNA-based vaccines, like Pfizer-BioNTech and Moderna. These vaccines give the genetic information needed to make the spike (S) glycoprotein antigen but not the antigens themselves; they have more local side effects.14
-
(c)
The subunit approaches where very specific parts or subunits of the SARS-CoV2 virus are used to trigger the immune system (ex. Novavax). See Table 1 for more details.
Table 1.
Most common types of COVID-19 vaccines, mode of action, and release time.
| Vaccine name | Manufacturing country | Mode of action | Time of release |
|---|---|---|---|
| Sputnik V | Russia | viral vector-based vaccines | August 2020 |
| AstraZeneca | UK/USA Oxford University/Cambridge | viral vector-based vaccines | released in 2021 |
| The Janssen/Johnson and Johnson vaccine | USA | viral vector-based vaccines | February 2021 |
| Moderna | USA | novel mRNA-based SARS-CoV-2 vaccines | released in 2020 |
| Pfizer-BioNTech | USA | novel mRNA-based SARS-CoV-2 vaccines | December 2020 |
| Sinovac's CoronaVac | China | whole virus technology(inactivated or killed virus) | December 2020 |
| Novavax | USA | Protein sub-unit vaccine | released in 2021 |
Several researchers have investigated the potential effects of COVID-19 on male fertility, hormone indicators, and sperm parameters, whether as a result of infection or vaccination. Few, however, had addressed which factor had the greatest impact on seminal fluid analysis (SFA).
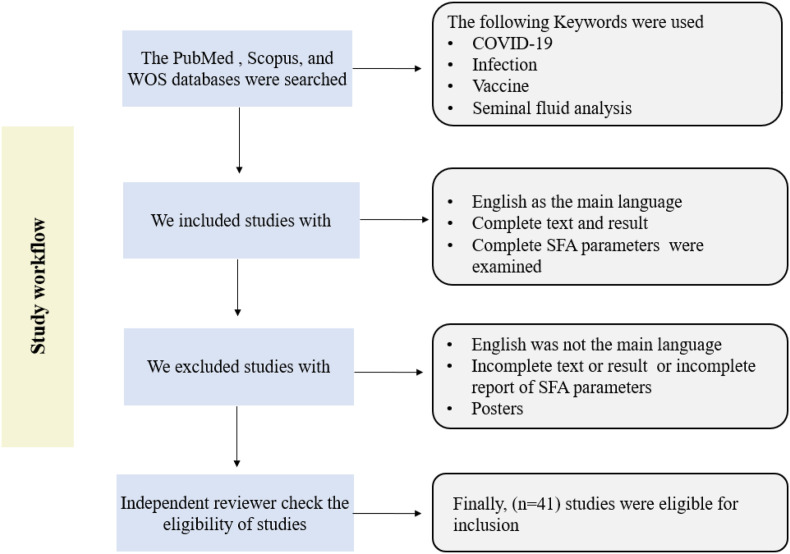
This paper aims to increase our insight into how SFA changes during infection and after vaccination, especially after global vaccination campaigns, and to examine which significantly impacts SFA and its parameters.15, 16, 17 See Fig. 1 .
Fig. 1.
Study flowchart.
2. Semen production
The hypothalamus produces the gonadotrophin-releasing hormone, which causes the pituitary gland to secrete a follicular stimulating hormone (FSH) and luteinizing hormone (LH). Testosterone is produced by Leydig cells under the influence of LH. In contrast, the androgen binding protein (ABP) is secreted by Sertoli cells under the effect of FSH. ABP will concentrate testosterone to promote spermatogenesis. Testosterone will orchestrate different maturations of spermatogonia, aided by Sertoli cells. Maintaining the gap junction with other Sertoli cells to form the blood-testis barrier (BTB) represents the utmost function of Sertoli cells.18 Thus, it maintains the immunologically privileged environment in the testis, adding to its local anti-inflammatory action. The primordial sperm cells at the base of the Sertoli cell are more susceptible to external immune damage since they lack a blood-testis barrier. The finalization of sperm maturation occurs in the epididymis. Other seminal fluid contents, including seminal vesical and prostate secretion, will occur in the vas deferens.19
3. Seminal fluid changes during the infection
The first report of changed SFA in response to COVID-19 was made by Holtmann et al.20; they reported a statistically significant reduction of sperm concentrations and sperm counts, in addition to a reduced number of progressively motile sperm in comparison to healthy controls. This novel finding suggests that the virus causes short-term depression of spermatogenesis in patients with moderate symptoms. The authors excluded cases with fever to clarify the negative impact of fibril illness on the SFA; interestingly, only the total sperm motility remained meaningful. The rest of the parameters showed an insignificant reduction in response to the infection; see Table 2 .
Table 2.
Seminal fluid changes due to COVID-19 infection.
| Study | Study type Sampling frequency | Number recruited | Finding |
|---|---|---|---|
| Holtmann N et al20 | Pilotcohort study One time sampling: 32.7 days in covalence period of COVID-19 infection Acute phase of infection |
18/34 recovered males 14/34 healthy controls. 2/34 males in acute infection phase |
In patients with moderate infection, reduction of sperm concentrations, and total sperm counts, added to a reduced progressive motile sperm. |
| Enikeev D et al21 | Prospective study 2 times sampling: 1st taken at time of hospitalization for COVID-19 2nd at 12 weeks follow-up visit |
44/88 study cases and 44/88 healthy controls |
A significant reduction of sperm motility increased immotile sperms, and a low percentage of normal sperms was documented in moderate and severe cases, which was transient. |
| GuoTH et al22 | Cohort study 2 times sampling: 1st sampling 56 days following discharge 2nd sampling(84 days) |
40/90 cases 50/90 controls 22/40 had secondary sample 84 days |
1st sampling showed a meaningful reduction of sperm counts, motility, and less progressive motile sperms. 2nd sampling highlighted a significant increase in the parameters mentioned above. They confirmed that changes in SFA were transient |
| Li H et al24 | Cross-sectional cohort one time sampling: within 7 days of confirmed COVID-19 infection |
23/55 study cases; inpatients COVID-19 cases. 22/55 age-matching male healthy controls. |
Reduced sperm concentrations and oligo-azoospermia in males who already had offspring |
Enikeev et al.21 examined SFA for seropositive males during the acute infection and 12 weeks later, revealing a similar finding to Holtmann's results. The changes in SFA seen were transient, and they returned to normal levels three months later. Enikeev reported significantly higher IgA by direct mixed agglutination reaction at the time of the second sampling, which supports the role of an inflammatory response in the pathogenesis of COVID-19 in testicular injury. Twenty of the 44 patients they enrolled died as a result of the illness; autopsies revealed inflammatory reactions and viral invasion of the testis. Guo et al.22 examined the semen of a recovered patient in two settings over a time frame of 84 days. The first sampling showed a similar result to Holtmann and Enikeev's. The second sampling showed a significant increase in the parameters mentioned above. They confirmed that SFA changes were transient and that one spermatogenic cycle was likely enough to resolve them.
At the time of first sampling, the SARS-CoV-2 virus may not be the only cause for the temporary changes in sperm parameters. The emotional and mental stress of COVID-19 is inversely linked with spermatogenesis. Other possible causes; include febrile illness, medication, therapy, or the severity of COVID-19.23 , 24 Li et al. discovered decreased sperm concentrations and oligo-azoospermia in males who already had children, confirming their fertility prior to infection.24 Segars et al.'s findings were consistent, as they reported reduced sperm concentrations and motility 71–90 days after infection.25
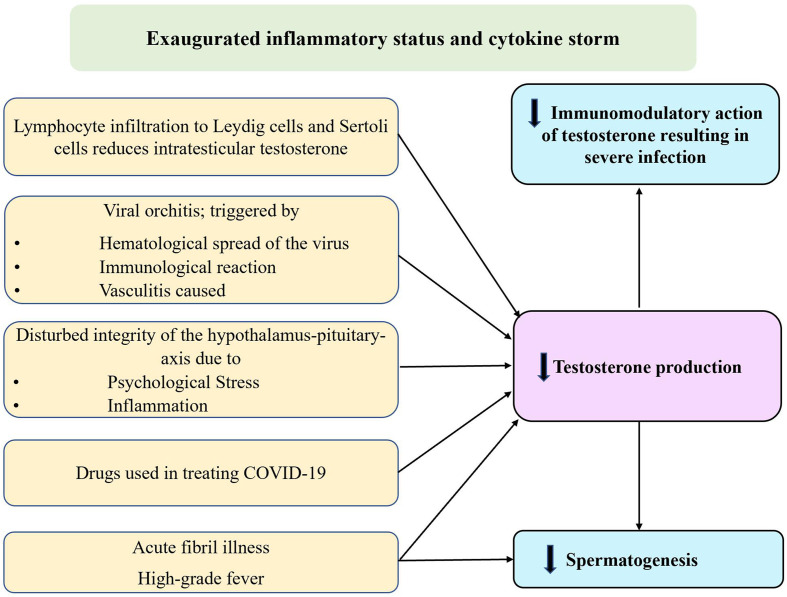
4. Causes for deterioration of SFA parameters in COVID-19 cases
Many hypotheses were suggested to explain SFA changes; see Fig. 2 . SARS-CoV2 is not the only virus that targets the testis; human papillomavirus, the influenza virus, the Zika virus, and the Epstein-Barr virus are all known to cause viral orchitis.11 It is still not clear if orchitis is caused by inflammation or an immune response, but the immune response is most likely to be the cause. The exaggerated inflammatory response initiated by the infection and cytokine storm will reduce the blood supply to the blood-testis barrier, resulting in orchitis-like syndrome, which is the most acceptable theory.26
Fig. 2.
Mechanism of testicular injury during COVID-19 infection.
The inflammatory cells and locally released cytokines by Leydig and Sertoli cells will generate reactive oxygen species (ROS) that damage sperm DNA, causing cell death and impairing SFA parameters.27 In a recently published paper, the authors confirm that only Leydig cells and not Sertoli cells are infected, which is further validated by postmortem specimens showing significant seminiferous tubular damage and decreased levels of Leydig cells.28 Inflammation, COVID-19, and stress affect the integrity of the hypothalamic-pituitary axis. The reduced testosterone production will impair spermatogenesis, and the beneficial immunomodulatory and anti-inflammatory actions will be lost.29 SARS-CoV2 is a thrombogenic virus; vasculitis is another possible factor for testicular damage triggered by segmental vasculitis. Vasculitis-caused orchitis is another proposed theory for COVID-19.30 IgG was found in the seminiferous tubule by an immunohistochemistry study on samples from deceased COVID-19 patients.31 Being a fibril illness is another important cause that triggers gonadal cell apoptosis.32 Some of the therapies used in the management were also blamed; specific antivirals and using hydroxychloroquine were reasons for reduced SFA parameters.17 , 22
5. Does seminal fluid carry the COVID-19 virus?
The evidence regarding SARS-CoV-2 presence in semen was conflicting; Li et al., Machado et al., and Gacci et al. identified SARS-CoV-2 in the semen of confirmed and recovered cases. The sample size in the studies was small.33, 34, 35
Luddi et al. show that viral replication in male gametes happens in more than one step and that viral particles can be separated at the middle of the sperm tail.28
Conversely, Ma et al., Kteily et al., and Holtmann et al.20 , 36 , 37 denied the presence of viruses in semen samples. Because of the modest number of positive samples tested and the lack of viral RNA in semen, this research shows that the presence of SARS-CoV-2 in sperm is an uncommon finding.
A breach in the blood-testis-different barriers can explain the viral presence in the SFA, which allows the virus to seed to the male reproductive tract during systemic inflammation. Even though the virus is incapable of replication in the reproductive system, it persists in the testis due to the testis' unique immunity.33
Given the lack of evidence of viral transmission by blood or sexual activity, scientists deny the benefit of washing sperm, which is routinely done in human immunodeficiency virus or hepatitis B virus-positive males to protect uninfected females and cross-contaminated reproductive tissues.20 There are currently no recommendations or guidelines for screening oocyte or sperm donors for SARS-CoV-2. More research needs to be done to make sure that both preserved gametes and couples who use assisted reproduction are safe.
6. Vaccines and SFA
A vaccine is a combination of biological materials that gives active protection against a particular infectious pathogen by inducing an immune reaction to an antigen (a molecule of the pathogen). Vaccination is the most effective long-term technique for preventing and controlling infectious diseases.12 , 13 Local adverse effects were more prevalent with mRNA-based vaccinations, especially among women and younger people, compared to viral vector-based vaccines, which showed more systemic side effects.14 , 38
Unsubstantiated media reports suggest a possible link between the SARS-CoV-2 vaccination and male infertility, resulting in immunization reluctance. In addition, previous research examined the influence of the infection on SFA parameters and how it led to impaired spermatogenesis. The most widely accepted etiology was autoimmune orchitis, discovered in postmortem specimens.39, 40, 41
Theoretically, a parallel consequence may be observed after receiving the SARS-CoV-2 vaccine, which may induce a similar immune reaction. Some authors proposed that the systemic immune response that follows vaccination may be the underlying mechanism, and the overall prognosis is good. Concerns were raised regarding the coronavirus vaccination's potential effect on male fertility.16 Many works were carried out in the field (see Table 3 ), and SFA changes were monitored up to 145 days.
Table 3.
The seminal fluid changes seen following vaccination.
| The study | Type; number enrolled and vaccine type | Sampling period and frequency | Finding |
|---|---|---|---|
| Abd ZH et al12 | Prospective observational study; 60 adult men; Pfizer-BioNTech mRNA COVID-19 vaccine |
The days between the pre-vaccine semen analysis and the first vaccination dose were 100.5 ± 69. The days first and second doses were 101 ± 37 and 133 ± 39 respectivly |
A statistically significant reduction in total sperm motility and progressively motile sperm, both readings before and after vaccination were within the normal range. |
| Safrai M et al15 | Case-control study; | The time between the first vaccine and the post-vaccine sperm analysis was 71.0 days | No significant changes in SFA after vaccination among men with a normal and abnormal semen analysis. Therefore, the BNT162b2 vaccine does not seem to affect sperm parameters |
| 72 men with normal and abnormal SFA; | |||
| BNT162b2 mRNA Covid-19 vaccine, a nucleoside-modifiedRNA vaccinedeveloped by BioNTech and Pfizer | |||
| Lifshitz D et al40 | Prospective cohort study; | 1–2 months following their second dose; Time from 2nd vaccination to participation was, on average, 37 days, | A trend of lower abnormal semen parameters predominantly within the normal range |
| 75 fertile men were analyzed; | |||
| Pfizer's COVID-19 vaccine | |||
| Gonzalez DC et al41 | Prospective study; 45 were recruited Pfizer's COVID-19 vaccine: Moderna |
1st sampling was after the first vaccine dose and around 70 days after. The follow-up samples were at a median of 75 days after the second dose of the vaccine |
After 2nd vaccine dose, the sperm concentration, motility, and semen volume were significantly increased. 7/45 men had increased sperm concentration to the normozoospermic range. 1/45 men who initially was oligospermia showed no meaningful decreases in any sperm parameter |
| Gat I et al16 | Retrospective longitudinal multicenter cohort study. BNT162b2 vaccination 37- sperm donors gave 216 samples The study had four phases: 1st pre-vaccination baseline control. 2nd post-vaccination samples |
The study had four times sampling: 1st pre-vaccination; baseline control samples. 2nd post-vaccination samples; here the sampling took place 3 times •Short timed sample to show the effect of vaccine with in (15–45) days • Intermediate time sample to show the effect of vaccine with in (75–125) days •Long timed sample to show the vaccine effect over 145 days |
A selective transient increase in sperm concentration and deterioration of total motile sperm. 3 months after vaccination, followed by later recovery. Long-term impact of the BNT162b2 vaccine seems safe. |
Most of the changes seen included sperm motility and concentration; however, those were within the normal range of WHO guidelines for SFA. Furthermore, the changes triggered following the complete vaccine schedule were transient, and all parameters returned to normal in both normal fertile and sub-fertile males. The safety of the vaccine was reinforced; however, no current guidelines exist for screening sperm in couples undergoing assisted reproduction, which warrants more research.
7. Conclusion and future perspective
Hundreds of tests were swiftly produced, created, and certified for COVID-19 diagnostic assays. Using Artificial intelligent -based techniques and Deep Learning experts' active collaboration with healthcare experts would ideally allow more accurate and sensitive ways for earlier diagnosis and severity evaluation. Newer approaches have the advantage of the ease in modification and sensitivity to tiny antigens.42 , 43
The SFA changes that follow the COVID-19 infection and vaccine are reversible. Vaccines are safe and do not impact male fertility, even in subfertile cases.
There are still uncertainties regarding the effect of the infection on preserved gametes, the effect of seminal fluid mediators, and immune parameters relevant to viruses—all these warrant further work.
Author's contribution
WN conceived, designed the study, and drafted the manuscript, DAS analyzed data; both authors approved the final version of the manuscript.
Ethics approval
Not applicable.
Consent for publication
All authors consent for publication.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
To our university, Mustansiriyha for continuous support.
References
- 1.Tolu L.B., Feyissa G.T., Jeldu W.G. Guidelines and best practice recommendations on reproductive health services provision amid COVID-19 pandemic: scoping review. BMC Publ Health. 2021;21(1):276. doi: 10.1186/s12889-021-10346-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roozbeh N., Amirian A., Abdi F., et al. A systematic review on use of medicinal plants for male infertility treatment. J Fam Reprod Health. 2021;15(2):74–81. doi: 10.18502/jfrh.v15i2.6447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farhan F.S., Nori W., Al Kadir I.T.A., et al. Can fetal heart lie? Intrapartum CTG changes in COVID-19 mothers. J Obstet Gynaecol India. 2022;24:1–6. doi: 10.1007/s13224-022-01663-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crook H., Raza S., Nowell J., et al. Long covid-mechanisms, risk factors, and management. BMJ. 2021;374 doi: 10.1136/bmj.n1648. [DOI] [PubMed] [Google Scholar]
- 5.Nori W., Hamed R.M., Roomi A.B., et al. Alpha-1antitrypsin in pre-eclampsia; from a clinical perspective. J Pakistan Med Assoc. 2021;71(12):S53–S56. (Suppl 8) [PubMed] [Google Scholar]
- 6.Thakur V., Ratho R.K., Kumar P., et al. Multi-organ involvement in COVID-19: beyond pulmonary manifestations. J Clin Med. 2021;10(3):446. doi: 10.3390/jcm10030446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edenfield R.C., Easley C.A., 4th Implications of testicular ACE2 and the renin-angiotensin system for SARS-CoV-2 on testis function. Nat Rev Urol. 2022;19(2):116–127. doi: 10.1038/s41585-021-00542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malki M.I. COVID-19 and male infertility: an overview of the disease. Medicine (Baltim) 2022;101(27) doi: 10.1097/MD.0000000000029401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu J., Qi L., Chi X., et al. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol Reprod. 2006;74(2):410–416. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khalili M.A., Leisegang K., Majzoub A., et al. Male fertility and the COVID-19 pandemic: systematic review of the literature. World J Mens Health. 2020;38(4):506–520. doi: 10.5534/wjmh.200134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Desai A.D., Lavelle M., Boursiquot B.C., et al. Long-term complications of COVID-19. Am J Physiol Cell Physiol. 2022;322(1):C1–C11. doi: 10.1152/ajpcell.00375.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abd Z.H., Muter S.A., Saeed R.A.M., et al. Effects of Covid-19 vaccination on different semen parameters. Basic Clin Androl. 2022;32(1):13. doi: 10.1186/s12610-022-00163-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klugar M., Riad A., Mekhemar M., et al. Side effects of mRNA-based and viral vector-based COVID-19 vaccines among German healthcare workers. Biology. 2021;10(8):752. doi: 10.3390/biology10080752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hogerwerf L., Post P.M., Bom B., et al. Proximity to livestock farms and COVID-19 in The Netherlands, 2020-2021. Int J Hyg Environ Health. 2022;245 doi: 10.1016/j.ijheh.2022.114022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safrai M., Herzberg S., Imbar T., et al. The BNT162b2 mRNA Covid-19 vaccine does not impair sperm parameters. Reprod Biomed Online. 2022;44(4):685–688. doi: 10.1016/j.rbmo.2022.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gat I., Kedem A., Dviri M., et al. Covid-19 vaccination BNT162b2 temporarily impairs semen concentration and total motile count among semen donors. Andrology. 2022;10(6):1016–1022. doi: 10.1111/andr.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shen Q., Li J., Zhang Z., et al. COVID-19: systemic pathology and its implications for therapy. Int J Biol Sci. 2022;18(1):386–408. doi: 10.7150/ijbs.65911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zirkin B.R., Papadopoulos V. Leydig cells: formation, function, and regulation. Biol Reprod. 2018;99(1):101–111. doi: 10.1093/biolre/ioy059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardeland R. Melatonin and the programming of stem cells. Int J Mol Sci. 2022 10;23(4):1971. doi: 10.3390/ijms23041971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holtmann N., Edimiris P., Andree M., et al. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil Steril. 2020;114(2):233–238. doi: 10.1016/j.fertnstert.2020.05.028.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Enikeev D., Taratkin M., Morozov A., et al. Prospective two-arm study of the testicular function in patients with COVID-19. Andrology. 2022;10(6):1047–1056. doi: 10.1111/andr.13159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo T.H., Sang M.Y., Bai S., et al. Semen parameters in men recovered from COVID-19. Asian J Androl. 2021;23(5):479–483. doi: 10.4103/aja.aja_31_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nordkap L., Jensen T.K., Hansen Å.M., et al. Psychological stress and testicular function: a cross-sectional study of 1,215 Danish men. Fertil Steril. 2016;105(1):174–187. doi: 10.1016/j.fertnstert.2015.09.016. e1-2. [DOI] [PubMed] [Google Scholar]
- 24.Li H., Xiao X., Zhang J., et al. Impaired spermatogenesis in COVID-19 patients. EClinicalMedicine. 2020 Nov;28 doi: 10.1016/j.eclinm.2020.100604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Segars J., Katler Q., McQueen D.B., et al. American society for reproductive medicine coronavirus/COVID-19 task force. Prior and novel coronaviruses, coronavirus disease 2019 (COVID-19), and human reproduction: what is known? Fertil Steril. 2020;113(6):1140–1149. doi: 10.1016/j.fertnstert.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tariq J., Chatterjee T., Andreoli L., et al. COVID-19 and fertility-at the crossroads of autoimmunity and thrombosis. Rheumatol Int. 2021;41(11):1885–1894. doi: 10.1007/s00296-021-04977-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen Q., Xiao X., Aierken A., et al. The ACE2 expression in Sertoli cells and germ cells may cause male reproductive disorder after SARS-CoV-2 infection. J Cell Mol Med. 2020;24(16):9472–9477. doi: 10.1111/jcmm.15541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luddi A., Luongo F.P., Dragoni F., et al. Cellular and molecular mechanisms of in vivo and in vitro SARS-CoV-2 infection: a lesson from human sperm. Cells. 2022;11(17):2631. doi: 10.3390/cells11172631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.He Y., Wang J., Ren J., et al. Effect of COVID-19 on male reproductive system - a systematic review. Front Endocrinol. 2021;12 doi: 10.3389/fendo.2021.677701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parrón D., Gartzia A., Iturregui A.M., et al. SARS-CoV-2-Associated obliterative arteritis causing massive testicular infarction. Clin Pract. 2021;11(2):246–249. doi: 10.3390/clinpract11020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van der Kuyl A.C., Berkhout B. Viruses in the reproductive tract: on their way to the germ line? Virus Res. 2020;286 doi: 10.1016/j.virusres.2020.198101. [DOI] [PubMed] [Google Scholar]
- 32.Abdelhamid M.H., Fellah A.A., Elmarghani A., et al. An assessment of men's semen alterations in SARS-CoV-2: is fever the principal concern? Reprod Sci. 2022 Feb 22:1–9. doi: 10.1007/s43032-022-00889-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li D., Jin M., Bao P., et al. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Machado B., Barcelos Barra G., Scherzer N., et al. Presence of SARS-CoV-2 RNA in semen-cohort study in the United States COVID-19 positive patients. Infect Dis Rep. 2021;13(1):96–101. doi: 10.3390/idr13010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gacci M., Coppi M., Baldi E., et al. Semen impairment and occurrence of SARS-CoV-2 virus in semen after recovery from COVID-19. Hum Reprod. 2021;36(6):1520–1529. doi: 10.1093/humrep/deab026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma L., Xie W., Li D., et al. Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients. J Med Virol. 2021;93(1):456–462. doi: 10.1002/jmv.26259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kteily K., Pening D., Diaz Vidal P., et al. Risk of contamination of semen, vaginal secretions, follicular fluid and ovarian medulla with SARS-CoV-2 in patients undergoing ART. Hum Reprod. 2022;37(2):235–241. doi: 10.1093/humrep/deab255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nori W., Akram W. Effect of gender on the reliability of COVID-19 rapid antigen test among elderly. World J Clin Cases. 2022;10(29):10820–10822. doi: 10.12998/wjcc.v10.i29.10820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abbasi J. Widespread misinformation about infertility continues to create COVID-19 vaccine hesitancy. JAMA. 2022;327(11):1013–1015. doi: 10.1001/jama.2022.2404. [DOI] [PubMed] [Google Scholar]
- 40.Lifshitz D., Haas J., Lebovitz O., et al. Does mRNA SARS-CoV-2 vaccine detrimentally affect male fertility, as reflected by semen analysis? Reprod Biomed Online. 2022;44(1):145–149. doi: 10.1016/j.rbmo.2021.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gonzalez D.C., Nassau D.E., Khodamoradi K., et al. Sperm parameters before and after COVID-19 mRNA vaccination. JAMA. 2021;326(3):273–274. doi: 10.1001/jama.2021.9976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vandenberg O., Martiny D., Rochas O., et al. Considerations for diagnostic COVID-19 tests. Nat Rev Microbiol. 2021;19:171–183. doi: 10.1038/s41579-020-00461-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chavda V.P., Valu D.D., Parikh P.K., et al. Conventional and novel diagnostic tools for the diagnosis of emerging SARS-CoV-2 variants. Vaccines. 2023;11(2):374. doi: 10.3390/vaccines11020374. [DOI] [PMC free article] [PubMed] [Google Scholar]