Abstract
Purpose
Despite being one of the most common types of the peripheral vertigo encountered in clinical practice, benign paroxysmal positional vertigo (BPPV) remains underdiagnosed and undertreated, even in affluent health care systems. The publication of fully updated clinical practice guidelines significantly facilitated the diagnosis and treatment of BPPV. This study evaluates the adoption of the guidelines in our clinical setting and reviews further recommendations for quality-of-care improvement.
Methods
This retrospective cross-sectional survey included a total of 1155 adult patients diagnosed with BPPV at the biggest tertiary care center in the country during a 5-year period (2017–2021). The data for the first three years (2017–2020) and 919 patients were collected in full, and for the remaining 236 patients (2020–2021) only partially due to the disturbance in referrals caused by COVID-19 pandemic.
Results
The familiarity with and adherence to the published clinical guidelines by physicians judged by patients’ charts and our health care database were overall unsatisfactory. The adherence varied from 0 to 40.5% in our sample. The recommendations for making the diagnosis and for repositioning procedure as first-line therapy were followed in only 20–30% of cases.
Conclusion
There are large opportunities for improvement in quality of care of BPPV patients. Apart from constant and systematic education at the primary health care level, the health care system may need to adopt more advanced measures of ensuring better adherence to guidelines and subsequent reduction in medical costs.
Keywords: Benign paroxysmal positional vertigo, Clinical practice guidelines, Adherence, Vertigo
Introduction
Although benign paroxysmal positional vertigo (BPPV) was first described 100 years ago and further explained about 70 years ago, it did not become widely known until the 1990s, when Alain Semont and John Epley brought this disorder to the attention of the clinical community and introduced repositioning maneuvers as proposed treatment [1, 2]. BPPV is a form of a positional vertigo characterized by short periodic episodes of vertigo caused by changes in head position and abnormal stimulation of the cupula of one of the three semicircular canals in the inner ear, most often the posterior [3]. BPPV accounts for 17–42% of all patients with vertigo making it the most common type of peripheral vertigo encountered in everyday clinical practice [4].
The incidence of BPPV increases with age by about 38% for each decade of life and has a favorable prognosis of complete recovery since it is not associated with any underlying serious disorder [5]. In 20% of patients, BPPV goes away spontaneously within 1 month of follow-up, and in 50% after 3 months [6]. The diagnosis of the disorder is usually very simple, and it can be made based on the history of vertigo when throwing head, bending down, lying down, getting up, or when turning in bed and by an appropriate positional test (most commonly Dix–Hallpike test for the posterior canal) [7, 8]. Further testing or diagnostic procedures are not required in patients who meet the clinical criteria for the diagnosis of BPPV [9-11].
The most successful repositioning maneuver for the treatment of posterior canal BPPV is Epley, and for horizontal canal BPPV Lempert maneuver, also known as “Barbecue” [12-14]. Both maneuvers are very easy to perform and can be done as part of an exercises at home in selected patients [15]. Medical therapy is not indicated unless patients experience severe nausea or vomiting. Unfortunately, BPPV often relapses after the first episode, with a relapse rate between 15 and 50%, and the next episode usually occurs within a few months [4, 11].
Despite the fully published and updated clinical guidelines for BPPV which are freely available online, this disorder remains underdiagnosed and undertreated [11, 12]. Most of the key statements in the published guidelines are in the form of recommendations for or against the listed actions and are designed to guide the clinician’s decisions in a standardized manner, to consistently achieve best possible treatment outcome, and to lower medical costs. Recently published systematic review warned that adoption of clinical guidelines in otolaryngology is slow, incomplete and can vary widely depending on the evaluated factors (type of the evaluated recommendation, type of the clinical setting, etc.) [16]. Only a few studies were published to date on the adherence to the clinical practice guidelines for BPPV: two of them from emergency settings in Australia and one in form of the research letter from USA which dealt mostly with adherence to guidelines by specialty [17-19].
The aim of this paper was to examine patient’s records and health database of the biggest tertiary care center in the country and to report available data on clinician’s adherence to the published guidelines key statements. The primary goal was to determine whether the clinicians who encounter patients with BPPV in the studied population follow the recommended guidelines regarding the diagnosis and adequate treatment (statements 1a and 4a in the published guideline) [11]. Our secondary goals included questions regarding timely diagnosis of BPPV, unnecessary diagnostic procedures, including imaging studies, inappropriate use of medications (statement 3a and 6), etc.
Materials and methods
This study was a cross-sectional retrospective analysis of a tertiary health care database and patients’ records. The study included a total of 1155 adults diagnosed with BPPV over a 5-year period (January 1, 2017–December 31, 2021) at the outpatient department of the biggest tertiary referral University Clinical Center in our country. The data for the first 3 years (2017–2020) and total of 919 patients were collected and reported in full, and for the remaining 236 patients (treated from January 1, 2020 to December 31, 2021) only partially due to the disturbance in referrals caused by COVID-19 pandemic.
The main data collected, if available, was the clinician’s adherence to eight Key Statements of the American Academy of Otorhinolaryngology-Head and Neck Surgery Clinical Practice Guidelines [11]. The additional data collected from the outpatient records included age, gender, time from onset of symptoms until correct diagnosis, maneuvers performed, development of a complication or need for repeated treatment, duration of instability, information on any prior diagnostic or imaging procedures, medication at the time of diagnosis, and recurrence of the disease within the first year of follow-up. The data were analyzed using methods of descriptive statistics (SPSS Inc. Version 23.0, Chicago, Illinois). Categorical variables were given as percentages and numeric are shown as means (M) and standard deviations (SD). Wald technique was used to calculate 95% confidence intervals.
Results
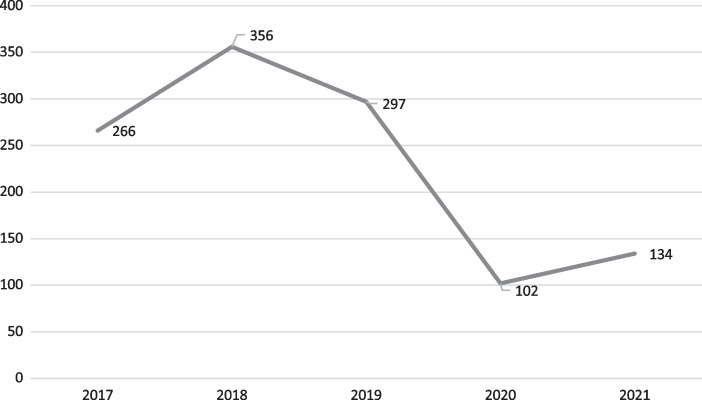
Figure 1 shows a total number of patients diagnosed with BPPV in our center by year. An obvious decrease in number of referred cases in the last 2 years by two-thirds is understandable and expected. To avoid many possible sources of biases, we decided to report fully only data from patients diagnosed in the first 3 years of the study period.
Fig. 1.
Number of patients diagnosed with BPPV in our center during examined 5-year period
The adherence to the key statements in the published guidelines varied considerably, as shown in Table 1. The data were available on five of eight key statements. In only one-third of our patients, the statement 1a was met and the diagnosis of posterior BPPV was made at the initial examination (either by performing Dix–Hallpike maneuver or the patient was referred to our department where he/she can be treated accordingly). In only one-fifth (21.8%) of the patients, the initial therapy was a canal repositioning procedure (CRP). The recommendation against radiographic imaging for patients who meet diagnostic criteria for BPPV and statement 3a was also poorly adhered to in our sample, with as many as 760 patients (82.7%) undergoing additional specialist examinations or imaging studies (multiple in some cases) before the correct diagnosis was made (most often an examination by a neurologist or physiatrist, brain CT or MRI scan, Doppler scan of the neck blood vessels, or cervical spine X-ray).
Table 1.
Adherence to AAH Guidelines Key Action Statements [11] in our sample
| Statement | Action | Strength | Adherence in % (with 95% CI) |
|---|---|---|---|
| 1a. Diagnosis of posterior semicircular canal BPPV | Clinicians should diagnose posterior semicircular canal BPPV when vertigo associated with torsional, up-beating nystagmus is provoked by Dix–Hallpike maneuver | Strong recommendation | 31.5% (27.3–35.7%) |
| 1b. Diagnosis of lateral (horizontal) semicircular canal BPPV | Clinician should perform supine roll test to assess for lateral semicircular canal BPPV if the patient has a history compatible with BPPV and the Dix–Hallpike test exhibits horizontal or no nystagmus | Recommendation | 26.1% (13.4–38.8%) |
| 3a. Radiographic testing | Clinicians should not obtain radiographic imaging in a patient who meets diagnostic criteria for BPPV | Recommendation (against) | 17.3% (14.9–19.7%) |
| 4a. Repositioning procedures as initial therapy | Clinicians should treat, or refer to clinician who can treat, patients with posterior canal BPPV with CRP | Strong recommendation | 21.8% (19.1–24.4%) |
| 4c. Observation as initial therapy | Clinicians may offer observation with follow-up as initial management | Option | 40.5% (37.3–43.6%) |
| 5. Vestibular rehabilitation | The clinician may offer vestibular rehabilitation, either self-administered or with a clinician | Option | 0% (NA) |
| 6. Medical therapy | Clinicians should not routinely treat BPPV with vestibular suppressant medications | Recommendation (against) | 24.7% (21.2–27.5%) |
BPPV benign paroxysmal positioning vertigo, CRP Canal Repositioning Procedure, CI Confidence Interval, NA not applicable
Table 2 shows the detailed demographic data on 919 patients diagnosed with BPPV included in the study. The data on time to correct diagnosis was available for 816 (89%) patients, and in our sample, it was 10 months and 28 days. The findings on the positional tests at the first examination were negative in 397 patients (43.2%), although the history and the accompanying clinical findings clearly indicated BPPV. In the majority of patients with positive result on the positional test, the findings suggested the involvement of the posterior semicircular canal (pc-BPPV) and in only 46 patients (8.9%) horizontal canal was involved (hc-BPPV). Just over one half of the patients with hc-BPPV had geotropic nystagmus, while the remaining had apogeotropic (24 and 22 patients, respectively). In three patients in whom the positional nystagmus suggested the anterior canal involvement, it was not possible to determine with certainty the side of the disorder.
Table 2.
Main demographic and clinical characteristics of patients included in the study
| Parameter | Number of patients N = 919 |
|---|---|
| Age (mean ± SD) | 54.94 ± 14.62 |
| Gender | |
| Male | 239 (26%) |
| Female | 680 (74%) |
| Average time from symptoms onset to diagnosis | 328 days (min 1 day, max 20 years) |
| Negative positional test | 397 (43.2%) |
| Positive positional test | 522 (56.8%) |
| Canal involvement (N = 522) | |
| Posterior canal | 473 (90.6%) |
| Horizontal canal | 46 (8.9%) |
| Anterior canal | 3 (0.6%) |
| Side affected | |
| Right | 287 (55%) |
| Left | 219 (45%) |
| Maneuvers performed (N = 476) | |
| Epley | 452 (95%) |
| Barbeque | 24 (5%) |
| Complications | |
| Transition or conversion | 32 (6.7%) |
SD Standard deviation, min minimum, max maximum
After the repositioning maneuver, most patients achieved complete resolution of discomfort. A relatively small percent of patients developed complications (32 patients experienced an undesirable migration of otoconial particles to another semicircular canal). The most common migration was expectedly from the posterior to the horizontal semicircular canal (10 as canalithiasis and 18 as cupulolithiasis). All patients with hc-BPPV canalithiasis were cured immediately with the Barbecue repositioning maneuver, while in the remaining patients with cupulolithiasis hc-BPPV, the symptoms resolved spontaneously during the first week from initial visit.
Unfortunately, the reliable data on the recurrence rate could not be obtained with certainty; however, among the patients in our database, there were 204 cases (22.2%) of BPPV recurrence during the first year of follow-up.
Discussion
The reason to exclude data on patients diagnosed and treated during the last 2 years of the ongoing pandemic was not only due to a decrease in outpatients visits. The more worrying reasons were the quality of care, which was most likely adversely affected given multiple lockdowns and different referral patterns adopted by the government in different periods of the pandemic. Furthermore, it was reported that the highest rate of appointment cancelations during the COVID-19 pandemics was actually observed in BPPV patients. In Japan, 75% of BPPV patients reported cancelation of their visits for fear of contracting infection in hospital [20].
Increasing the awareness on low adherence to the clinical guidelines
Depending on how the health service is organized in different European countries, doctors of different specialties diagnose and treat BPPV, from general practitioners, to otorhinolaryngologists, neurologists, internal medicine specialists, to physiotherapists and each of them have different level of familiarity with published recommendations [21]. In the United States, the cost of care for patients with vertigo or dizziness shows 1.38-fold annual increase after controlling for demographic and socioeconomic factors [22]. Furthermore, it is estimated that the burden on the health system is about $2 billion per year and that only about 20% of patients with BPPV receive adequate treatment [23]. The data from our center show similar numbers. Adherence to the published recommendations is very low, varying from 0 to 40.5%. Although the key recommendations are strong and state that the diagnosis of posterior canal BPPV should be made (or the patient referred to the clinician who can make the diagnosis, statement 1a) and that the initial therapy should be a repositioning procedure (statement 4a), the average time to correct diagnosis and repositioning procedure in our sample was almost 11 months. Considering that around 50% of BPPV cases resolve spontaneously within three months, the number of patients who have never been diagnosed is most likely much higher [6]. As many as 43.2% of patients had a negative result on the positional tests at the time of the examination, which may further inflate the number of undiagnosed patients in case they achieved spontaneous resolution by that time.
Although it has been reported that the “recommendations against” has higher adherence among clinicians [16], the recommendation against radiographic imaging and for routine treatment with vestibular suppressant medication was very poorly adhered in our sample with only 17.3% of patients not getting any imaging done and 24.7% of them had not been prescribed with medical therapy. These findings are slightly worse than the previous published data on most frequent procedures and medication in patients with vertigo, both in primary care and emergency departments [17, 18, 24-26]. Although, as many as 40% of patients were initially offered observation rather than repositioning procedure in our sample, none was offered vestibular rehabilitation, although there is evidence that that it can be beneficial, especially in elderly patients [27].
Study sample features
Based on their characteristics, the patients examined in our study had similar profile with those from other published studies. Women were affected three times more often than men, which is slightly more than in other population-based studies [4, 28], although there are studies with a similar gender ratio [29]. The right side was slightly more often affected, and the most common diagnosis was pc-BPPV canalithiasis, present in 90.6% of cases. As many as 80% of patients were cured using only one repositioning maneuver, while further 13.1% of patients required two or more maneuvers. The rate of conversion when performing repositioning maneuvers was low in our sample, which is consistent with the other published studies in the literature and previously reported data from this center [30].
Recurrence rate in our sample was rather low, but it is well known that recurrence rate of BPPV during one-year follow-up can reach almost 50%, especially in the elderly population [5, 28, 30, 31]. Therefore, it is very important to explain to patients the nature of the disorder and provide detailed instructions and advice on future behavior and possible recurrence of symptoms [32].
Limitations of the study
This study has several limitations. Due to its retrospective nature, it shares the same shortcomings with all retrospective case studies, i.e., information bias, meaning that patients’ records and procedures may not accurately reflect the patients’ presentation. Due to its single-site study design, it may have limited generalizability, but it is still valuable in highlighting weaknesses in our referrals system and can help identify the reasons for nonadherence. To avoid selection bias and to make our sample more representative, we excluded from the analysis patients from the last two years.
What can be done about adherence?
It has been already reported that the greatest improvements in adherence to the guidelines were observed when clinical practices were intentionally standardized according to the guideline [33]. Other suggestions have been also proposed: support through electronic health records, education through interactive small group meetings, online education courses, leadership commitment, etc. [16]. Preferences of clinicians are variable and therefore, strategy should be multifaceted with both education and system plan and a lot of energy to implement changes [34]. These efforts should be primarily directed to primary care physicians and non-otolaryngologists, i.e., emergency care neurologists and doctors who treat elderly patients, as they are the ones who usually first encounter the patients with BPPV in our country. Initial step could be support through electronic health record, as it is universal throughout the whole national health care system. Suggestions and directions on how to refer these patients to doctors who can successfully preform the maneuvers could prove to be crucial, and lead to substantial improvement in quality of health care and lowering of the costs.
Conclusion
BPPV is the most common form of vertigo found in clinical practice with more than one third of patients with vertigo being affected by BPPV. Although clinical guidelines and recommendations for best treatment were published almost 15 years ago and are freely available online, timely diagnosis and adequate treatment are achieved in only one-third to one-fifth of our patients. To avoid late diagnosis, delay in treatment and costs of additional diagnostic procedures and examinations, it is necessary to constantly educate general practitioners, primary care ENT specialists, as well as neurologists about this disorder and its treatment, whether using physician championship, local leaders, or continual medical education. Authors believe that the growing awareness of low adherence rates and dissemination of clinical guidelines will help decrease the costs of health care and enable delivery of the best care to our patients.
Author contributions
BB: Made a substantial contribution to the concept and design of the paper, data collection, analysis, and interpretation, drafted the article, revised it critically for important intellectual content, and approved the final submitted version. DN, DP, and NR: Made a substantial contribution to the data collection and analysis, and approved the final submitted version. TI and AJ: Made substantial contribution to data collection, critically revised the article for important intellectual content, and approved the final submitted version.
Funding
The authors did not receive support from any organization for the submitted work.
Data availability
Data from this study are not publicly available due to legal and ethical grounds (of opening electronic health care records which could possibly compromise the privacy of research participants) but can be seen partially upon a reasonable request to the authors.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial conflicts of interest to disclose.
Ethical statement
The Institutional Review Committee of Faculty of Medicine, University of Belgrade approved this study (decision number 1-UAU-03). The formal consent would be difficult to obtain due to retrospective nature of this study and is not needed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290–293. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 2.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 3.Hanley K, O’Dowd T, Considine N. A systematic review of vertigo in primary care. Br J Gen Pract. 2001;51(469):666–671. [PMC free article] [PubMed] [Google Scholar]
- 4.Messina A, Casani AP, Manfrin M, Guidetti G. Italian survey on benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. 2017;37(4):328–335. doi: 10.14639/0392-100X-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Zaag-Loonen HJ, van Leeuwen RB, Bruintjes TD, van Munster BC. Prevalence of unrecognized benign paroxysmal positional vertigo in older patients. Eur Arch Oto-Rhino-Laryngology. 2015;272(6):1521–1524. doi: 10.1007/s00405-014-3409-4. [DOI] [PubMed] [Google Scholar]
- 6.Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987;37(3):371–378. doi: 10.1212/WNL.37.3.371. [DOI] [PubMed] [Google Scholar]
- 7.Yao Q, Wang H, Song Q, Shi H, Yu D. Use of the Bárány Society criteria to diagnose benign paroxysmal positional vertigo. J Vestib Res. 2018;28(5–6):379–384. doi: 10.3233/VES-190648. [DOI] [PubMed] [Google Scholar]
- 8.Nuti D, Zee DS, Mandalà M. Benign paroxysmal positional vertigo: what we do and do not know. Semin Neurol. 2020 doi: 10.1055/s-0039-3402733. [DOI] [PubMed] [Google Scholar]
- 9.Von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3–4):105–117. doi: 10.3233/VES-150553. [DOI] [PubMed] [Google Scholar]
- 10.Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, Chalian AA, Desmond AL, Earll JM, Fife TD, Fuller DC, Judge JO, Mann NR, Rosenfeld RM, Schuring LT, Steiner RW, Whitney SL, Haidari J. American Academy of Otolaryngology-Head and Neck Surgery Foundation Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139(5 Suppl 4):47–81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K, Hollingsworth DB, Roberts R, Seidman MD, Steiner RW, Do BT, Voelker CC, Waguespack RW, Corrigan MD. Clinical practice guideline: benign paroxysmal positional vertigo (update) Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 12.Mandalàà M, Salerni L, Nuti D. Benign positional paroxysmal vertigo treatment: a practical update. Curr Treat Options Neurol. 2019;21(12):66. doi: 10.1007/s11940-019-0606-x. [DOI] [PubMed] [Google Scholar]
- 13.Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD003162.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burton MJ, Eby TL, Rosenfeld RM. Extracts from the Cochrane Library: modifications of the Epley (canalith repositioning) maneuver for posterior canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2012;147(3):407–411. doi: 10.1177/0194599812457134. [DOI] [PubMed] [Google Scholar]
- 15.Piromchai P, Eamudomkarn N, Srirompotong S, Ratanaanekchai T, Yimtae K. The efficacy of a home treatment program combined with office-based canalith repositioning procedure for benign paroxysmal positional vertigo—a randomized controlled trial. Otol Neurotol. 2019;40(7):951–956. doi: 10.1097/MAO.0000000000002310. [DOI] [PubMed] [Google Scholar]
- 16.Ryan MA, Leu GR, Boss EF, Raynor EM, Walsh JM. Adherence to American Academy of Otolaryngology-head and neck surgery clinical practice guidelines: a systematic review. Otolaryngol Head Neck Surg. 2020;163(4):626–644. doi: 10.1177/0194599820922155. [DOI] [PubMed] [Google Scholar]
- 17.Neely P, Patel H, Wellings T. Benign paroxysmal positional vertigo in the emergency department: an observational study of an Australian regional hospital's acute clinical practice. Emerg Med Australas. 2021;33(6):1082–1087. doi: 10.1111/1742-6723.13810. [DOI] [PubMed] [Google Scholar]
- 18.Lloyd M, Mackintosh A, Grant C, McManus F, Kelly AM, Karunajeewa H, Tang CY. Evidence-based management of patients with vertigo, dizziness, and imbalance at an Australian metropolitan health service: an observational study of clinical practice. Physiother Theory Pract. 2020;36(7):818–825. doi: 10.1080/09593985.2018.1511020. [DOI] [PubMed] [Google Scholar]
- 19.Dunlap PM, Khoja SS, Whitney SL, Freburger JK. Assessment of physician adherence to guidelines for the diagnosis and treatment of benign paroxysmal positional vertigo in ambulatory care settings. JAMA Otolaryngol Head Neck Surg. 2018;144(9):845–846. doi: 10.1001/jamaoto.2018.1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ueda K, Ota I, Yamanaka T, Kitahara T. The impact of the COVID-19 pandemic on follow-ups for vertigo/dizziness outpatients. Ear Nose Throat J. 2021;100(2_suppl):163S–168S. doi: 10.1177/0145561320980186. [DOI] [PubMed] [Google Scholar]
- 21.Male AJ, Ramdharry GM, Grant R, Davies RA, Beith ID. A survey of current management of Benign Paroxysmal Positional Vertigo (BPPV) by physiotherapists’ interested in vestibular rehabilitation in the UK. Physiother (United Kingdom) 2019;105(3):307–314. doi: 10.1016/j.physio.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Ruthberg JS, Rasendran C, Kocharyan A, Mowry SE, Otteson TD. The economic burden of vertigo and dizziness in the United States. J Vestib Res. 2021;31(2):81–90. doi: 10.3233/VES-201531. [DOI] [PubMed] [Google Scholar]
- 23.You P, Instrum R, Parnes L. Benign paroxysmal positional vertigo. Laryngoscope Investig Otolaryngol. 2018;4(1):116–123. doi: 10.1002/lio2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grill E, Strupp M, Müller M, Jahn K. Health services utilization of patients with vertigo in primary care: a retrospective cohort study. J Neurol. 2014;261(8):1492–1498. doi: 10.1007/s00415-014-7367-y. [DOI] [PubMed] [Google Scholar]
- 25.Ahsan SF, Syamal MN, Yaremchuk K, Peterson E, Seidman M. The costs and utility of imaging in evaluating dizzy patients in the emergency room. Laryngoscope. 2013;123(9):2250–2253. doi: 10.1002/lary.23798. [DOI] [PubMed] [Google Scholar]
- 26.Saber Tehrani AS, Coughlan D, Hsieh YH, Mantokoudis G, Korley FK, Kerber KA, Frick KD, Newman-Toker DE. Rising annual costs of dizziness presentations to U.S. emergency departments. Acad Emerg Med. 2013;20(7):689–696. doi: 10.1111/acem.12168. [DOI] [PubMed] [Google Scholar]
- 27.Bressi F, Vella P, Casale M, Moffa A, Sabatino L, Lopez MA, Carinci F, Papalia R, Salvinelli F, Sterzi S. Vestibular rehabilitation in benign paroxysmal positional vertigo: reality or fiction? Int J Immunopathol Pharmacol. 2017;30(2):113–122. doi: 10.1177/0394632017709917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu CT, Zhao XQ, Ju Y, Wang Y, Chen MM, Cui Y. Clinical characteristics and risk factors for the recurrence of benign paroxysmal positional vertigo. Front Neurol. 2019;10:1190. doi: 10.3389/fneur.2019.01190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim SK, Hong SM, Park IS, Choi HG. Association between migraine and benign paroxysmal positional vertigo among adults in South Korea. JAMA Otolaryngol Head Neck Surg. 2019;145(4):307–312. doi: 10.1001/jamaoto.2018.4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Babic BB, Jesic SD, Milovanovic JD, Arsovic NA. Unintentional conversion of benign paroxysmal positional vertigo caused by repositioning procedures for canalithiasis: transitional BPPV. Eur Arch Oto-Rhino-Laryngol. 2014;271(5):967–973. doi: 10.1007/s00405-013-2494-0. [DOI] [PubMed] [Google Scholar]
- 31.Nahm H, Han K, Shin JE, Kim CH. Benign paroxysmal positional vertigo in the elderly: a single-center experience. Otol Neurotol. 2019;40(10):1359–1362. doi: 10.1097/MAO.0000000000002385. [DOI] [PubMed] [Google Scholar]
- 32.Kong TH, Song MH, Shim DB. Recurrence rate and risk factors of recurrence in benign paroxysmal positional vertigo: a single-center long-term prospective study with a large cohort. Ear Hear. 2022;43(1):234–241. doi: 10.1097/AUD.0000000000001093. [DOI] [PubMed] [Google Scholar]
- 33.Milder EA, Rizzi MD, Morales KH, Ross RK, Lautenbach E, Gerber JS. Impact of a new practice guideline on antibiotic use with pediatric tonsillectomy. JAMA Otolaryngol Head Neck Surg. 2015;141(5):410–416. doi: 10.1001/jamaoto.2015.95. [DOI] [PubMed] [Google Scholar]
- 34.Ishii LE. Closing the clinical gap: translating best practice knowledge to performance with guidelines implementation. Otolaryngol Head Neck Surg. 2013;148(6):898–901. doi: 10.1177/0194599813481203. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from this study are not publicly available due to legal and ethical grounds (of opening electronic health care records which could possibly compromise the privacy of research participants) but can be seen partially upon a reasonable request to the authors.