Abstract
A combination of coracoid fracture and acromioclavicular dislocation is rare. Detecting further pathologies that could cause multiple superior shoulder suspensory complex disruptions is mandatory. Literature regarding these injuries and their management is lacking. We report our diagnostic and surgical strategies, and the postoperative outcomes of superior shoulder suspensory complex disruptions. We present five cases, treated from 2011 to 2016, who had >2 disruptions of the superior shoulder suspensory complex, involving at least a coracoid fracture and an acromioclavicular joint dislocation. Surgical reconstruction was performed in all cases. The patients were postoperatively followed up for a year. There were no intraoperative or postoperative complications, and bone union was achieved in all fractures. Furthermore, all patients returned to their pre-surgery activity level and jobs. Thus, we could demonstrate that in multiple superior shoulder suspensory complex disruptions involving a coracoid fracture and an acromioclavicular joint dislocation, surgical treatment leads to a good functional outcome.
Keywords: Coracoid fracture, superior shoulder suspensory complex, acromioclavicular dislocation, case report
Introduction
Injuries of the acromioclavicular (AC) joint are frequent, and commonly occur due to direct shoulder impact. 1 The patients often are young athletic adults; the incidence is 3%–12% of all shoulder injuries. 2 The incidence rises with sporting activities, up to approximately 40% in contact sports (e.g. football). 3 AC dislocation combined with a fracture of the coracoid process (CP), however, is very rare. The incidence of CP fractures is reportedly 2%–13%; 4 very few cases report an associated AC dislocation. 5 This combination results in a double disruption of the superior shoulder suspensory complex (SSSC). The SSSC includes the glenoid fossa, the clavicle, the acromion and CPs, and the AC and coracoclavicular ligaments (Figure 1). A double disruption causes construct instability. Multiple disruptions may cause nonunion due to shoulder girdle instability. 6 Literature pertaining to these injuries and their management guidelines is lacking. A review by Kose et al. 5 of 48 cases (1946–2018) found a variety of treatment options ranging from conservative management to complex surgical reconstruction and fixation. Kose et al. reported two cases; Metwaly and Edres, 7 one case; and Liau et al. 8 made a review of all 57 cases reported in the literature of concomitant fracture of the CP following AC dislocation and recommended that each case be considered individually before arriving at a treatment option. Even less case reports described at least triple disruption of the SSSC.9–13 A systematic review found 73 case reports on CP fractures with multiple disruptions of the SSSC, consisting of 42 double disruptions, 26 triple disruptions, and 5 quadruple disruptions. 14 So the difficulty in treatment lies in the knowledge of associated injuries and their influence on biomechanics. Herein, we report five more patients with the same injury pattern of multiple SSSC disruptions, including CP fracture and AC dislocation that we treated between 2011 and 2016. All patients were managed with surgical fixation of CP and repair of the associated SSSC ruptures depending on the stability. We aimed to propose a reliable treatment option of SSSC injuries with a good outcome.
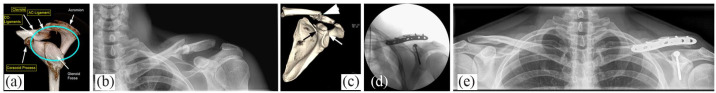
Figure 1.

The superior shoulder suspensory complex, containing the glenoid fossa, clavicle, acromioclavicular ligaments, the acromion and the coracoid processes, and the coracoclavicular ligaments.
AC: acromioclavicular; CC: coracoclavicular.
Cases
Case 1
A 30-year-old Portuguese man presented to our emergency unit 4 days after a bicycle accident. He had visited another hospital and was diagnosed to have an AC-joint subluxation and a CP fracture on shoulder radiographs (AP/Neer/axillary/AP (panorama) and stress views) (Figure 2(a) and (b)). They decided to treat him conservatively. However, he wanted a second opinion due to severe pain. Magnetic resonance imaging (MRI) was performed and he was finally diagnosed with Rockwood type III AC dislocation with a CP fracture (Figure 2(c)). We opted for a surgical approach, which was performed 10 days after the accident. With the patient under general anesthesia and in a beach-chair position, we first performed a diagnostic shoulder arthroscopy to exclude intraarticular trace injuries because of MRI-detected irregularities in the long head of the biceps. The shoulder arthroscopy showed no intraarticular injuries. Using an open approach, the CP was reduced and fixed with a 3.5-mm cannulated screw. Subsequently, the AC joint was reduced and preliminarily fixed with a K-wire. An AC-joint augmentation with a non-absorbable braided suture (Niceloop, Wright Medical Group N.V., Memphis, Tennessee, USA) was performed in (Figure 8) between the acromion and lateral clavicle for horizontal stability. For subacromial placement of the hook plate, a small incision was made posterior to the AC joint. With a template, the correct hook depth was determined. The definitive plate was appropriately placed under the acromion and secured to the clavicular shaft with three cortical screws (Figure 2(d)). The postoperative course was uneventful and the patient was discharged on the fourth postoperative day. The plate was removed 4 months postoperatively (Figure 2(e)). Six months after the accident, the patient regained full range of motion, had no pain, and could work at the construction site.
Figure 2.
(a–e) Case 1: Triple disruption of the SSSC: (a) the acromioclavicular and coracoclavicular ligaments tear and a CP fracture. (b) In the panorama view, we can see a widening of the AC joint and (c) in the MRI, a CP fracture and coracoclavicular ligaments rupture. (d) Intraoperative fluoroscopy showing the CP fixation with a cannulated screw and the AC-joint fixation with a nice-loop and a hook plate. (e) The panorama view after 6 months shows good reduction of the AC-joint after removal of the hook plate.
SSSC: superior shoulder suspensory complex; CP: coracoid process; AC: acromioclavicular.
Figure 8.

Active range of motion 1 year after surgery. Flexion, abduction, and external rotation were measured in degrees. For internal rotation, the highest vertebral level that the thumb can reach is recorded.
IR: internal rotation; ER: external rotation.
Case 2
A 25-year-old German student injured his left shoulder in a ski accident. He initially presented to a nearby emergency department where radiography was performed; no fractures were detected. Back home, he presented to another doctor due to constant pain. He was transferred to our hospital on suspicion of a lateral clavicle fracture. Other radiograph views were obtained, and we found a CP fracture in addition to an extremely lateral clavicle fracture and AC-joint disruption (Figure 3(a) and (b)). The injuries were confirmed using a computed tomography (CT) scan that showed no additional shoulder lesions (Figure 3(c)). Surgery was performed 13 days after trauma. With the patient under general anesthesia and in a beach-chair position, a diagnostic shoulder arthroscopy was performed which showed an intact rotator cuff, long head of biceps tendon, and labrum. Two cannulated screws were arthroscopically inserted into the CP. After fixation of the CP also the AC-joint was reduced. To avoid stress on the CP osteosynthesis, the AC-joint was transfixed with two K-wires (Figure 3(d)). The patient was discharged from hospital on the fourth postoperative day. The K-wires were removed 1 month postoperatively (Figure 3(e)).
Figure 3.
(a–e) Case 2: Quadruple disruption of the SSSC: (a) AC and CC ligaments, clavicle, and CP. (b, c) In the radiograph and the initial CT, we can see the lateral clavicle and CP fracture. (d) Postoperative radiographs after fixation of the CP and the AC joint and (e) 6 months postoperatively after removal of the k-wires show good reduction.
SSSC: superior shoulder suspensory complex; CP: coracoid process; AC: acromioclavicular; CC: coracoclavicular.
Case 3
A 32-year-old Swiss firefighter suffered a ski fall. He was diagnosed with a left-sided clavicle fracture at a nearby clinic. The patient presented to our hospital for surgical management. We additionally detected a CP fracture near the base extending to the upper part of the glenoid cavity and a Rockwood type II AC-joint dislocation (Figure 4(a)–(c)). With the patient under general anesthesia and in a beach-chair position, a diagnostic arthroscopy was performed 3 days after injury. The fracture could be visualized in the upper third of the glenoid with a dislocation of 3 mm. An open fixation of the CP was performed under arthroscopic control with a 4.5 mm cannulated screw. Subsequently, open reduction and internal fixation of the clavicle fracture was performed with an isolated 2.0 mm bicortical screw and an eight-hole plate (Figure 4(d) and (e)). The AC-joint dislocation was not addressed surgically. The patient was discharged on the fifth postoperative day.
Figure 4.
(a–e) Case 3: (a) Quadruple disruption of the SSSC. (b) The first radiograph showed the midshaft clavicle fracture. (c) In the following CT-scan, a CP fracture was detected additionally. (d) The intraoperative fluoroscopy shows the plate fixation of the clavicle and the screw fixation of the CP. (e) The 6-month follow-up shows good reduction with fracture union.
SSSC: superior shoulder suspensory complex; CP: coracoid process; AC: acromioclavicular.
Case 4
A 39-year-old Swiss electrician presented to the emergency room a day after a bicycle accident with left shoulder pain. Radiographs of his shoulder (clavicle AP/tangential and shoulder AP/Neer/axial/panorama with and without weight views) revealed a CP fracture and an associated Rockwood type III AC-joint dislocation (Figure 5(a)–(c)). A CT scan did not reveal any further injuries (Figure 5(d)). The surgery was performed 5 days after the accident. With the patient under general anesthesia and in a beach-chair position, open fixation of the CP fracture with a cannulated screw, and AC-joint fixation with a hook plate, similar to that in Case 1, were performed. In addition, the AC ligaments were repaired using a suture anchor and fixation with a hook plate, the suture anchors were passed through the AC ligaments and tied with multiple knots (Figure 5(e) and (f)). On the third postoperative day, the patient was discharged. The hook plate was removed 5 months after surgery (Figure 5(g)).
Figure 5.
(a–g) Case 4: (a) Triple disruption of the SSSC is shown in the graphic. (b, c) The first radiographs and (d) the following CT show the CP fracture. (e) Intraoperative fluoroscopy showed good reduction of the CP fracture and the AC joint. (f) A CT performed 5 months postoperative, showed good consolidation of the CP. (g) A panorama view 1-year after surgery showed an AC-joint symmetric to the contralateral side.
SSSC: superior shoulder suspensory complex; CP: coracoid process; AC: acromioclavicular.
Case 5
A 52-year-old Portuguese gardener was brought to our hospital by an ambulance, after he fell onto a wet street because of a scooter accident. He complained of left shoulder and knee pain. Radiographic examination of the knee revealed a complex injury with a proximal tibial fracture, a bony avulsion of the anterior crucial ligament and medial collateral ligament, a complex tear of the medial meniscus, and a nondisplaced proximal fibular fracture. The left shoulder showed a Rockwood type IV AC-joint dislocation and CP fracture (Figure 6(a)–(c)). The knee injury was tackled 6 days after the accident. Three days later, with the patient under general anesthesia and in a beach-chair position, open reduction and fixation of the AC joint with a hook plate and fixation of the CP with a cannulated screw were performed (Figure 6(d)). The patient was discharged 11 days after the shoulder surgery. The shoulder was immobilized for 4 weeks. Thereafter, functional physiotherapy without weight-bearing was initiated and continued for 12 weeks. The rehabilitation process was difficult because of the combined injuries; 5 months postoperatively, the hook plate was removed (Figure 6(e)). The patient had persistent left shoulder pain and restricted range of motion; an intraarticular steroid injection was given and physiotherapy was continued for the postoperative capsulitis. At the 1-year follow-up, the shoulder pain had reduced, but restriction of shoulder movements persisted. In the MRI, the fracture was consolidated (Figure 6(f)).
Figure 6.
(a–f) Case 5: (a) Triple disruption of the SSSC shown in the graphic, (b) could be detected on a panorama view by the widening of the AC joint. (c) The CP fracture was diagnosed on CT. (d) After screw fixation of the CP and transfixion of the AC-joint with a hook plate, anatomical reduction was confirmed with a panorama view. (e) After removal of the hook plate the AC joints were symmetric. (f) Because of capsulitis an MRI was performed 2 years postoperatively that showed good alignment of the CP.
SSSC: superior shoulder suspensory complex; CP: coracoid process; AC: acromioclavicular.
Results
The mean patient age at the time of surgery was 36.6 years (range 25–52 years). In all five cases, we had at least a double disruption of the SSSC. Double disruptions lead to instability and require operative treatment.15–17 In all five cases, CP fracture occurred, which was surgically treated with reduction and fixation. The mean time between accident and surgery was 7.4 days (range 3–13 days). A cannulated screw was used for CP fixation in all cases. This was done via arthroscopy, arthroscopy-assisted, or the open method. This depended on the surgeon’s experience and the secondary injuries to be addressed. There were no differences in the postoperative course among the surgical methods. All patients had an associated AC-joint dislocation. AC-joint dislocation of Cases 1, 4, and 5 were treated with a hook plate. The plates were removed after 4–5 months. In Case 2, the AC joint had been transfixed with K-wires, which were removed 1 month postoperatively. In Case 3, there was an additional mid-third clavicle fracture. The fracture was reduced and fixed with an eight-holed plate on the superior surface.
All patients were immobilized after surgery for 3 weeks with an arm sling or a Gilchrist bandage. Physiotherapy without weight-bearing and a restricted range of motion for abduction/flexion of 90° was started from the fourth week. Full range of motion was allowed after 6 weeks. For the patients with a hook plate, weight-bearing was not allowed until plate removal.
The follow-up for all patients was exactly 12 months. The Constant-Score was measured after 3, 6, and 12 months (Figure 7). The 100-points scale of the score is divided into 4 subscales: pain (15 points), activities of daily living (20 points), strength (25 points), and range of motion of the shoulder (40 points). The higher the score, the better the function of the shoulder. 18 The mean score 1 year after surgery was 94.8/100. There was no acute complication. In the fifth case, a posttraumatic capsulitis occurred, which was treated with physiotherapy and a glenohumeral steroid injection, resulting in a prolonged postoperative course.
Figure 7.

The Constant Score was measured 3, 6, and 12 months after surgery. The mean score after 1 year was 94.8/100.
In all the patients, bone union was achieved. At the end of the follow-up period one patient had persistent reduced range of motion (Figure 8). Four out of the five patients were symptom-free 6 months after surgery. The patient with the capsulitis was pain-free after 1 year. All patients returned to their pre-surgery activity levels.
Discussion
Coracoid fractures are rare, and it is difficult to make a diagnosis through physical examination alone. A radiographic examination is indispensable in revealing the injury. Nevertheless, this fracture is frequently overlooked.19,20 Therefore, a CT or MRI study is required before performing a planned AC-joint stabilization with a coracoclavicular type tight-rope or with other similar devices.
Once a coracoid fracture is detected, additional injuries must be looked for. A three-dimensional CT or MRI will help identify the possible presence of double disruptions. Goss introduced the concept of the SSSC and forewarned that a double disruption could lead to an unstable shoulder and requires surgical treatment. 21 Operative management is indicated in nonunion, displacement of the CP fracture of more than 1 cm, or multiple disruptions of the SSSC. 22 If CP fracture occurs with an AC-joint dislocation, it is possible to address CP alone or with fixation of the AC joint. 6 All our cases had a double disruption of the SSSC. The CP can be stabilized with cannulated screws. To appropriately reduce and realign the CP fragment, preoperative CT- or MRI-scans are helpful. The AC-joint dislocation can be addressed through vertical fixation of the CP and the coracoclavicular ligaments with cannulated screws. Alternatively, horizontal stabilization of AC-joint dislocation can be achieved with a hook plate. In the case of coracoid fractures, AC-joint stabilization with a new, modern, claviculocoracoidal device is not recommendable or advisable.
A stable fixation can be achieved by these methods, but hook plate removal must be performed within 3–4 months. Transarticular wires (AC joint) have been described by other authors; however, this technique carries the risk of hardware migration and breakage. 7 At the moment, there is no surgical consensus on the optimum treatment strategy. The best treatment should be individualized considering age, associated injuries, and biomechanics. 23 In all our patients, bone union was achieved, and all of them returned to their pre-surgery activity levels.
Conclusion
In conclusion, surgical management of multiple SSSC disruptions with a CP fracture and an AC-joint dislocation produces good outcomes. The surgical techniques described in this article are a safe, but challenging way to treat multiple SSSC disruptions.
Footnotes
Consent for publication: Written informed consent was obtained from all the patients for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Institutional Review Board and/or ethical approval was not required as this piece of work was deemed to be an audit of clinical practice. Patient consent was obtained for use of radiographic imaging in the study.
ORCID iD: Philipp Tuor  https://orcid.org/0000-0003-4412-8877
https://orcid.org/0000-0003-4412-8877
References
- 1.Chillemi C, Franceschini V, Dei Giudici L, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int 2013; 2013: 171609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Enad JG, Gaines RJ, White SM, et al. Arthroscopic superior labrum anterior-posterior repair in military patients. J Shoulder Elbow Surg 2007; 16(3): 300–305. [DOI] [PubMed] [Google Scholar]
- 3.Willimon SC, Gaskill TR, Millett PJ. Acromioclavicular joint injuries: anatomy, diagnosis, and treatment. Phys Sportsmed 2011; 39(1): 116–122. [DOI] [PubMed] [Google Scholar]
- 4.Knapik DM, Gillespie RJ, Salata MJ, et al. Prevalence and impact of glenoid augmentation in American football athletes participating in the National Football League Scouting Combine. Orthop J Sports Med 2017; 5(8): 7722945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kose O, Canbora K, Guler F, et al. Acromioclavicular dislocation associated with coracoid process fracture: report of two cases and review of the literature. Case Rep Orthop 2015; 2015: 858969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Passaplan C, Beeler S, Bouaicha S, et al. Arthroscopic management of a coracoid fracture associated with acromioclavicular dislocation: technical note. Arthrosc Tech 2020; 9(11): e1767–e1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metwaly RG, Edres K. Biplanar fixation of acromio-clavicular joint dislocation associated with coracoid process fracture: case report. Trauma Case Rep 2018; 15: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liau GZQ, Phua SKA, Li T, et al. Concomitant fracture of the coracoid process following acromioclavicular joint dislocation. Ann Acad Med Singap 2021; 50(5): 438–440. [PubMed] [Google Scholar]
- 9.Lecoq C, Marck G, Curvale G, et al. Triple fracture du complexe suspenseur superieur de l’epaule: presentation d’un cas [Triple fracture of the superior shoulder suspensory complex]. Acta Orthop Belg 2001; 67(1): 68–72. [PubMed] [Google Scholar]
- 10.Badam VK, Harsha TSS, Sankineani SR, et al. Triple disruption of the superior shoulder suspensory complex—a case report. J Orthop Case Rep 2019; 9(3): 39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krtička M, Petráš M. Ipsilaterální zlomenina processus coracoideus a akromionu lopatky v kombinaci se zlomeninou laterální části klavikuly, terapeutická možnost řešení [Ipsilateral fractures of the coracoid and acromion process of the scapula combined with the distal clavicle end fracture, treatment options]. Acta Chir Orthop Traumatol Cech 2019; 86(4): 299–303. [PubMed] [Google Scholar]
- 12.Mulawka B, Jacobson AR, Schroder LK, et al. Triple and quadruple disruptions of the superior shoulder suspensory complex. J Orthop Trauma 2015; 29(6): 264–270. [DOI] [PubMed] [Google Scholar]
- 13.Tamimi Mariño I, Martin Rodríguez I, Mora Villadeamigo J. Triple rotura del complejo suspensorio del hombro [Triple fracture of the shoulder suspensory complex]. Rev Esp Cir Ortop Traumatol 2013; 57(5): 371–374. [DOI] [PubMed] [Google Scholar]
- 14.Van Doesburg PG, El Saddy S, Alta TD, et al. Treatment of coracoid process fractures: a systematic review. Arch Orthop Trauma Surg 2021; 141(7): 1091–1100. [DOI] [PubMed] [Google Scholar]
- 15.Kim SH, Chung SW, Kim SH, et al. Triple disruption of the superior shoulder suspensory complex. Int J Shoulder Surg 2012; 6(2): 67–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma 1993; 7(2): 99–106. [DOI] [PubMed] [Google Scholar]
- 17.Oh W, Jeon IH, Kyung S, et al. The treatment of double disruption of the superior shoulder suspensory complex. Int Orthop 2002; 26(3): 145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987; 214: 160–164. [PubMed] [Google Scholar]
- 19.Ogawa K, Matsumura N, Ikegami H. Coracoid fractures: therapeutic strategy and surgical outcomes. J Trauma Acute Care Surg 2012; 72(2): E20–E26. [PubMed] [Google Scholar]
- 20.Ogawa K, Ikegami H, Takeda T, et al. Defining impairment and treatment of subacute and chronic fractures of the coracoid process. J Trauma 2009; 67(5): 1040–1045. [DOI] [PubMed] [Google Scholar]
- 21.Tucker A, Donnelly K, Murphy L, et al. Percutaneous arthroscopic-assisted glenoid fixation: a novel surgical technique. J Orthop Case Rep 2018; 8(4): 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Westphal T, Lippisch R, Jürgens J, et al. Gleichzeitige Frakturen von Acromion und Korakoid: seltene Variante der doppelten Unterbrechung des superior shoulder suspensory complex [Simultaneous fracture of the acromion and coracoid process: rare variant of double disruption of the superior shoulder suspensory complex]. Unfallchirurg 2018; 121: 968–975. [DOI] [PubMed] [Google Scholar]
- 23.Wu K, Wu XM, Zha XL, et al. Anatomic restoration of triple disruption of the superior shoulder suspensory complex: a case report and review of the literature. Orthop Surg 2020; 12(5): 1526–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]